ABSTRACT
Objectives
Evaluation of the effect of deep neuromuscular blockade (DNMB) with low abdominal insufflation pressure (AIP) during laparoscopic colectomy on serum levels of inflammatory cytokines and on wound and shoulder-tip pain (STP) scores.
Patients & Methods
NMB was provided as rocuronium 0.6 mg/Kg initial dose and 0.15 mg/kg as maintenance dose according to the required depth of blockade and was reversed by sugammadex 4 mg/kg. AIP was provided at 10 and 14 mm Hg for Group-D and Group-C, respectively. Blood samples were collected for ELISA estimation of cytokines’ serum levels.
Results
The doses of intraoperative (IO) fentanyl (p = 0.026) and postoperative (PO) morphine, and 24-h cumulative pain score were significantly lower (p = 0.025) in Group-D. The measured cytokines’ serum levels increased progressively during surgery with significantly lower percentage of increase in Group-D (p = 0.0022; 0.0043; <0.001 for IL-1β, IL-6 and TNF-α, respectively). The percentage of increase in immediate PO serum cytokines’ levels was negatively related to the depth of NMB, while it showed positive correlation with the total dose of IO fentanyl, post-anesthetic care unit (PACU) pain scores, 24-h cumulative pain score and STP scores. Statistical analyses defined DNMB and serum IL-6 levels as significant predictor for cumulative pain scores.
Conclusion
The use of DNMB with low AIP significantly ameliorated the impact of surgery on immune milieu, reduced IO consumption of narcotic and reduced PO pain.
1. Introduction
Pain syndromes are mostly attributed to the perverse stir of the primary sensory neurons in the dorsal root ganglia secondary to the interaction between proinflammatory nociceptive cytokines and the satellite glial cells [Citation1].
Surgical stress can induce inflammatory responses and reduce the function of the immune system in a parallel fashion to the severity of surgical trauma with negative effects on postoperative (PO) pain sensation, resumption of physiological organ functions and wound healing [Citation2].
Laparoscopic surgery (LS) paved its way to be a popular procedure for short-timed surgeries but during the last decade it was tired and became a feasible procedure for major surgeries [Citation3]. Abdominal insufflation to create feasible surgical field is one of the cornerstones of LS but has multiple physiological impacts especially for ventilation and intraoperative (IO) cardiopulmonary compensatory mechanisms [Citation4]. One of the main drawbacks of pneumoperitoneum is the accumulation of air under the diaphragm with subsequent phrenic nerve irritation which is responsible for induction of PO shoulder-tip pain (STP) that may extend for weeks after surgery [Citation5].
Expanded surgical field to allow improved quality of surgical conditions is essential prerequisite for LS, and this was found to proportionate with the depth of neuromuscular blockade (NMB) [Citation6]. Deep NMB (DNMB) for LS provides better surgical workspace conditions and may allow reduction of abdominal insufflation pressure (AIP) [Citation7].
Surgery-induced temporal changes in the immune system might be modulated by anesthetic manipulations as regional blocks and epidural anesthesia [Citation8]. However, whether DNMB affects surgical immune stress, perioperative pain and PO outcomes or not is still unclear [Citation7].
2. Study hypothesis
Laparoscopic surgery under DNMB with reduction of AIP may impact the release of nociceptive cytokines secondary to surgical trauma with subsequent reduction of both IO and PO pain scores.
3. Objectives
Objectives are evaluation of the effect of DNMB with low AIP during laparoscopic colectomy on the extent of change in levels of proinflammatory cytokines and consumption of IO and PO analgesia as a judge for pain severity.
4. Design
Prospective interventional randomized multicenter comparative study.
5. Setting
Anesthesia, pain & ICU Department in conjunction with Medical Biochemistry Department, Faculty of Medicine, Menoufia and Cairo Universities.
6. Sample size
The null hypothesis of the current study was the detection of significant difference in serum levels of the studied cytokines between patients who received DNMB with low AIP and patients who received conventional NMB and AIP. Previously, Kim et al. [Citation9] and Koo et al. [Citation10] evaluated the effect of NMB on levels inflammatory cytokines during laparoscopic gastrectomy for 96 and 46 patients, respectively, who were randomized two groups according to the depth of blockade. Using the G*Power (Version 3.1.9.2) computer system for sample size calculation [Citation11] and considering the effect size of 0.20, the required sample size was calculated, using F-test model, with the use of α error factor of 5% and a power of 80%, sample size of 40 patients per group would assure the reliability of the null hypothesis.
7. Ethical data
The study protocol was approved by the departmental committee, and then the case collection was started. The protocol was discussed freely with patients before surgery and patients who accepted to participate in the study signed written fully informed consent before enrolment in the study. After complete case collection, the final approval by the Local Ethical Committee, Menoufia University, was obtained.
8. Patients
All patients assigned for laparoscopic colectomy were clinically evaluated to assure the absence of exclusion criteria. The collected patients’ constitutional data included age, gender, weight, and height for calculation of body mass index (BMI) according to the equation BMI (kg/m2) = weight (kg)/height (m2). Patients were graded as underweight, average weight, obese grades I-III according to the WHO guidelines. The presence of additional comorbidities was inquired for, and ASA grade, baseline heart rate (HR) and mean arterial pressure (MAP) were determined, and routine lab investigations were performed.
9. Exclusion criteria
The presence of myasthenia graves, neuromuscular disorders, immune-compromising disorders, maintenance on immunosuppressive drugs, autoimmune disorders, previous open abdominal surgery with scar that may hinder abdominal insufflation, ASA grade III or IV, obesity grade II and III, and refusal of study participation are the exclusion criteria.
10. Inclusion criteria
Patients prepared for laparoscopic colectomy, free of exclusion criteria and signed the written consents were enrolled in the study.
11. Randomization & grouping
Patients were randomly distributed between two study groups according to the depth of NMB using a computer system (Excel program; 2007) by applying 1:1 randomization process with dropping of even numbers. The study groups are Group-C, which included patients who received conventional NMB (CNMB) and AIP up to 14 mm Hg and Group-D which included patients who received DNMB and low AIP up to 10 mm Hg.
12. Neuromuscular blockade procedure
NMB procedure was conveyed as previously described by Barrio et al. [Citation12]; all patients received rocuronium as an initial dose of 0.6 mg/Kg, while maintenance dose of 0.15 mg/Kg was adjusted according to the desired depth as follows:
Patients of Group-C received the initial dose of rocuronium and when two responses appeared in the Train of Four stimulation (TOF), the maintenance dose of rocuronium was given.
For patients of Group-D, after receiving the initial rocuronium dose, and when two post-tetanic contractions (PTCs) appeared, the maintenance dose was injected.
13. Anesthetic technique
Preoperative HR and MAP measures were determined, preoperative blood samples were obtained, and patients received intravenous (IV) midazolam in a dose of 0.05 mg/kg up to 2.5 mg as premedication. On admission to the operative room, patients were pre-oxygenated; anesthesia was induced by propofol 1.5–2.5 mg/kg and IV rocuronium bromide 0.6 mg/Kg, and after about 3 min trachea was intubated. Anesthesia was maintained with 50% air in oxygen and an end-tidal concentration of 2–3% sevoflurane. Maintenance dose of rocuronium was provided as 0.15 mg/kg according to the group. Ventilation was controlled and minute ventilation was adjusted to maintain end-tidal CO2 at 35 ± 5 mm Hg. Then, intraoperative fentanyl was given as 1–2 µg/kg/min to maintain non-invasive HR within a range of ± 20% of the preoperative values, and MAP measures are in the range of 65–100 mm Hg. NMB was reversed at the end of surgery by IV injection of sugammadex 4 mg/kg and after resolution of NMB, trachea was extubated and patients were maintained on supplemental O2 until awake in the PACU. When patient is ready for PACU discharge, he was admitted to the intermediate care unit (IMCU) for 24 h and was discharged to surgical ward after assessment of the recovery status.
14. IO monitoring
– The frequency of failure of low IAP to provide satisfactory surgical field visibility (SFV) and shift to conventional AIP was recorded.
– Non-invasive measures of HR and MAP were recorded after intubation, 5 min before and after insufflation, after CO2 desufflation and extubation.
– The total dose of IO fentanyl required to control manipulation-induced pain for patients of both groups was registered.
– Surgical feasibility was evaluated according to the surgical field visibility that was presented as frequency and mean score for each group. SFV was scored on a 5-point Likert scale with higher scores that indicated very good SFV.
– Operative time and blood loss were recorded and presented as mean value.
– Duration of PO curarization was determined as time-lapsed from the start of sugammadex injection to the recovery of the TOFR to 0.9.
– Time lapsed till readiness for theater discharge and PACU transfer was also registered.
15. PACU monitoring
– Patients were evaluated for PO sedation using Ramsey Sedation Score (RSS) [Citation13]; immediately at PACU admission and every 30 min until achieving RSS of 2
–Patients were observed for development of PO pain that was assessed immediately at PACU admission and 1 h later and after transfer to the IMCU using 11-point (0-10) numeric pain scale (NRS) score with 0 indicates no pain and 10 indicates the worst intolerable pain [Citation14].
–Postoperative nausea and vomiting (PONV) was observed during PACU and IMCU stay. PONV, if occurred, was rated using a 4-point score for nausea (0-3) and 3-point score (0-2) vomiting scores [Citation15], and IV ondansetron 8 mg was given for patients who had nausea (score 3) or vomiting (score 1).
–Patients were evaluated for PACU discharge using the modified Aldrete score that ranges between 0 and 12, and patient was discharged at score of ≥9 [Citation16].
16. IMCU monitoring
Patients were admitted to the IMCU for the first 24-h PO before ward transfer for monitoring of
– PO pain scores were assessed at 2, 3 and 4 h and 4 h till 24 h using the NRS pain score. Routine PO analgesia was provided on admission to IMCU as ketorolac tromethamine (2 mg diluted to 20 ml with normal saline 0.9%) in a dose of 5 ml direct IV.
– Duration of PO analgesia, which was determined as the time elapsed from PACU discharge till having NRS score of ≥ 4 and requesting PO rescue analgesia.
– Rescue analgesia was provided for patient who had pain score of ≥ 4 despite of ketorolac injection as morphine 5 mg that was diluted to 10 ml using normal saline 0.9% and injected IV as 2 ml doses till pain resolution. The frequency of patients who required PO morphine injection, times of requirement and the received dose of morphine was recorded.
– The duration till 1st ambulation, the occurrence and severity of PONV attacks were determined.
– Recovery was assessed before IMCU discharge using the Quality of recovery score 40 (QoR40) questionnaire that was specially designed to measure patient’s health status after surgery and anesthesia [Citation17]. The QoR40 is a 5-domain patient-rated questionnaire consisting of 40 items (Appendix I), which are scored using a 5-point Likert scale with score of 1 indicated not present for positive items and present at all of the time for negative items and the reverse for score of 5. The individual scores were added to yield a total score ranging between 40 and 200 points [Citation18].
17. Ward monitoring and hospital discharge
During ward stay, the following items were recorded
–The shoulder-tip pain was assessed within 14 days after surgery by the use of the numeric pain scale as the pain referred to the tip of shoulder [Citation19] and expressed as both frequency of patients complained of such pain and its severity was presented as the mean value of pain score.
–Duration of hospital stay.
–At time of hospital discharge, patients were asked to record the frequency and severity of STP till the end of 2 weeks after surgery and feedback these data on the first PO follow-up visit.
–Surgeons’ satisfaction by the provided protocol was evaluated as 1 if field visibility was very dissatisfactory; 2 if dissatisfactory; 3 if good; 4 if satisfactory and 5 if it was very satisfactory.
18. Blood sampling & investigations
Four blood samples were collected preoperatively, at 1 h IO after induction of anesthesia, immediate and 48 h postoperatively. Blood samples were aseptically collected from the antecubital vein in a clean tube, allowed to clot and centrifuged at 2000 rpm for separation of serum that was collected in clean numbered Eppendorf tubes and stored at −20°C till being ELISA assayed for estimation of serum levels of interleukin (IL)-1β, IL-6, tumor necrosis factor (TNF)-α according to the manufacturer instructions and results were read using a 96-well microplate ELISA reader (Dynatech, MR 7000). Serum levels of the studied cytokines were measured using Abcam ELISA kit (Abcam Inc., San Francisco, USA) for Human IL-1β [Citation20], IL-6 [Citation21] and TNF-α [Citation22]; catalog no. ab214025; ab178013 & ab179886, respectively.
19. Statistical analyses
The obtained results were analyzed using IBM® SPSS® Statistics (Version 22, 2015; Armonk, USA). Comparisons of inter-group data were conveyed by one-way ANOVA test and paired t-test for intra-group comparisons. The extent of change in serum cytokines was calculated as the difference between levels measured in any sample minus the preoperative level and the result was divided by the preoperative level and multiplied by 100 to get the percentage of change. Pearson’s correlation analysis was used to assess the relation between the percentage of change in cytokines’ levels and perioperative data. The receiver operating characteristic (ROC) curve was conducted to evaluate the predictability of the percentage of change in serum cytokines’ levels estimated in samples obtained immediately and 48 h after surgery and the application of DNMB and the cumulative pain score during 24 h after surgery and the severity of STP during hospital stay. The results of the ROC analysis were presented as the area under the curve (AUC) and its significance was verified versus the area under the reference line (AUC = 0.5). The significance of these predictors was verified using the univariate regression analysis and the multivariate regression analysis to define the best predictor for oncoming 24-h cumulative pain score. The optimum cut-off point for significance of a result is p = 0.05.
20. Study outcomes
The primary outcome is the extent of change in serum levels of the studied cytokines in relation to preoperative levels. The secondary outcomes included evaluation of the correlation between the extent of change in cytokines’ levels estimated immediately PO and depth of NMB, IO fentanyl, operative time and NRS wound pain scores determined at PACU admission and 1 h later and between the extent of change in cytokines’ levels estimated at 48 h and cumulative 24 h NRS pain and STP scores. Also, defining the predictors for oncoming high cumulative NRS pain score among the studied cytokines and the use of DNMB.
21. Results
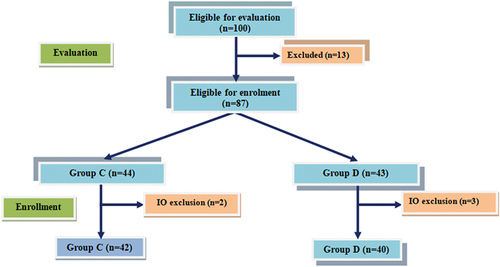
Preoperative evaluation excluded 13 patients; four patients for having previous laparotomy scar that may hinder abdominal insufflation, another four patients were obese of grades II and III, two patients had autoimmune disorders; two cardiac patients and one patient had myasthenia graves. Eighty-seven patients were enrolled in the study groups; Group-C included 44 patients and Group-D included 43 patients. Three patients were excluded intraoperatively; two of Group-C and one of Group-D, because of the presence of thick adhesion that failed to be safely resected by laparoscope. Another two patients of Group-D were excluded because of inconvenience of resection under low pressure that was increased to 14 mm Hg and the laparoscopic procedure was completed successfully. The laparoscopic procedure was completed successfully under the assigned conditions for 42 patients in Group-C and 40 patients in Group-D (). The enrolment data of patients of both groups as illustrated in show insignificant differences.
Table 1. Enrolment data of patients of both groups.
Estimated HR measures during operation and MAP measures showed insignificant differences between both groups except at 5 min after insufflation when MAP was significantly (p = 0.0006) lower in Group-D than Group-C ().
Table 2. HR and MAP measures of patients of both groups recorded throughout operation.
Operative time was significantly (p = 0.048) longer while significantly (p = 0.045) higher frequency of patients had operative time of 180–240 min among Group-D than Group-C. However, the mean dose of IO fentanyl consumed by patients of Group-D was significantly (0.026) lower than patients of Group-C ().
Table 3. IO and PACU data of patients of both groups.
The frequency of patients had high SFV score and its mean value was insignificantly lower among patients of Group-D. Moreover, mean volume of IO blood loss, time till NMB recovery and time till readiness for PACU transfer showed insignificant differences between both groups. Patients’ distribution according to RSS showed insignificant difference between both groups at time of PACU admission and at 30 min after admission. At 60 min after PACU admission, 44 patients were awake, cooperative, oriented and tranquil (RSS of 2) and 38 patients were awake but responds to commands only (RSS of 3) with significantly (p = 0.044) higher frequency of patients had RSS of 2 among Group-D than Group-C. Pain scores at PACU admission and 60-min thereafter were significantly (p = 0.0001 & 0.0022, respectively) lower in patients of Group-D than patients of Group-C. No patient had PONV during PACU stay, and at time of PACU discharge, 15 patients (18.3%), 11 of Group-C (26.1%) and four of Group-D (10%) had Aldrete score of <9 with insignificant difference between both groups as regards distribution and total Aldrete score ().
Duration of PO analgesia determined by the time elapsed between end of surgery and administration of the first dose of morphine was longer in Group-D with significant (p = 0.0041) difference in comparison with that in Group-C. Moreover, significantly higher number of patients of Group-D required morphine postoperatively and the received dose was significantly lower than patients of Group-C (p = 0.0213 & 0.0137, respectively) as shown in .
Table 4. IM-CU data.
During the IMCU stay, pain scores of patients of both groups showed insignificant differences till 8 h PO. Then, pain scores of patients of Group-D were significantly lower at 12, 16, and 20 h PO (p = 0.022; 0.0015 & 0.036, respectively) than in Group-C. The mean value of cumulative NRS score during IMCU stay was significantly (p = 0.025) lower and the duration till 1st ambulation was significantly (p = 0.019) shorter in favor of Group-D. During IMCU stay, 22 patients had nausea and 7 patients developed one vomiting attack. The frequency of patients according to incidence of PONV was insignificantly lower, while mean nausea score was significantly (p = 0.019) lower in Group-D than Group-C. Eighteen patients received ondansetron; 7 for vomiting and 11 patients for severe nausea with significantly lower requests for ondansetron in Group-D. Total and differential scores for items of QoR40 score were higher for patients of Group-D with significant differences in comparison with that of patients of Group-C except for item evaluating patient support that was insignificantly higher. Further, scores of all negative items were significantly higher for patients of Group-D than those of Group-C ().
The frequency of patients of Group-D who complained of STP during hospital stay was significantly (p = 0.040) lower in comparison with Group-C (30% vs. 52.5%) with significantly (p = 0.018) lower NRS pain score. After hospital discharge, the frequency of patients who complained of STP was insignificantly lower in Group-D than Group-C (3% vs. 20%) with insignificantly lower pain score. Duration of PO hospital stay was significantly (p = 0.023) shorter for patients of Group-D than patients of Group-C. Surgeons’ satisfaction score and distribution among satisfaction grades showed insignificant differences between both modalities of NMB and insufflation pressures ().
Table 5. Ward monitoring and hospital discharge data of patients of both groups.
The measured serum levels of the studied cytokines showed progressive elevation during surgery with significant differences between levels measured at 1 h IO in comparison with preoperative levels and between levels measured immediate PO compared to levels measured at 1 h IO. Preoperative levels of serum cytokines showed insignificant difference between both groups. However, serum levels estimated at 1-h IO and immediately PO were significantly lower in samples of patients of Group-D than samples of patients of Group-C. Moreover, the percentage of increase in serum levels of the three cytokines in relation to preoperative levels was significantly lower in samples of patients of Group-D than in samples of patients of Group-C. At 48-h PO, serum levels of the three cytokines were significantly decreased in comparison with levels measured immediately PO. Moreover, serum levels of the three cytokines measured in samples of patients of Group-D were significantly lower levels than Group-C with significantly lower extent of increase in relation to preoperative levels ().
Table 6. Serum levels of the measured cytokines in samples of patients of both groups.
p value indicates the significance of difference between both groups; P1 value indicates the significance between levels estimated at 1-h IO versus preoperative levels; P2 value indicates the significance between levels estimated immediately PO compared to that estimated at 1-h IO; P3 value indicates the significance between levels estimated 48 h PO versus levels estimated immediately PO.
The percentage of increase in serum levels of the studied cytokines in samples obtained immediately PO in relation to preoperative levels was negatively related to the depth of NMB. On the other side, the total dose of fentanyl consumed during surgery, operative time and NRS pain scores determined at PACU admission and 1 h later showed positive correlation with the percentage of increase in serum levels of the studied cytokines in samples obtained immediately PO in relation to preoperative levels. Moreover, the cumulative pain score determined at 24 h PO and scores of the severity of STP determined for complaining patients during hospital stay showed positive significant correlation with the percentage of increase in serum levels of the studied cytokines in samples obtained 48 h PO.
Evaluation of the predictors for the possibility of getting high cumulative NRS pain scores at the end of 24-h PO using the ROC curve analysis defined DNMB as negative predictor, while high percentage of increase in serum IL-6 levels in samples obtained immediately PO in relation to preoperative levels as a positive significant predictor for oncoming high cumulative NRS pain scores, while high percentages of increase in serum levels of IL-1β and TNF-α in samples obtained immediately PO are positive insignificant predictors (). Univariate regression analysis assured these findings, but multivariate regression analysis defined the use of DNMB as a negative significant predictor and excluded high percentage of change in serum levels of IL-6 as predictor for getting high 24-h cumulative pain scores ().
Figure 2. The ROC of the evaluated variates as predictors for the possibility of getting high 24-h cumulative NRS pain score.
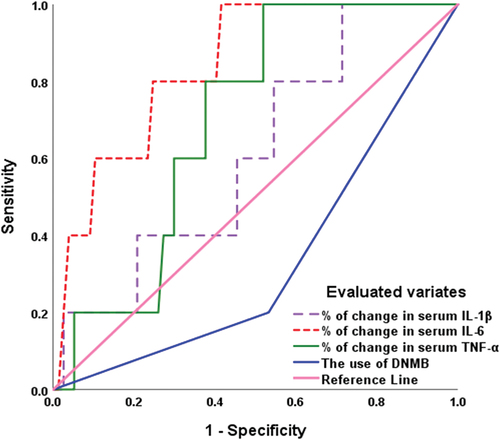
Table 7. statistical analyses of the extent of change in serum levels of the studied cytokines estimated immediately PO and 48 h PO in relation to preoperative levels.
22. Discussion
The measured serum cytokines’ levels showed significant progressive increase during surgery in comparison with their preoperative levels. This result indicated that surgery per se is an inflammatory condition and seriously impacted the body immune milieu. These findings supported the earlier studies evaluated the impact of surgical procedures on immune system [Citation23–27]. Also, Dobson et al. [Citation28] found that laparotomy led to a surgical-induced hyper-inflammation with immune activation and neuroendocrine stress. Trials were conducted to lessen the proinflammatory effect of surgery, and laparoscopic surgery was supposed by multiple studies to have less impact on immune milieu; Faisal et al. [Citation29] using immunohistochemistry detected significantly higher number of cells stained for inflammatory cytokines in specimens of patients had open surgery than LS. Recently, Erginel et al. [Citation30] reported that laparoscopic appendectomy is associated with a shorter operative time and hospital stay and smaller inflammatory response due to surgical stress than open appendectomy. Moreover, Cheng et al. [Citation31] found total laparoscopic distal gastrectomy had minimal impact on the inflammatory response than laparoscopic-assisted or open distal gastrectomy. A systemic review for studies comparing laparoscopic versus open surgery detected that LS showed more favorable outcomes with lower inflammation and less immunosuppression as indicated by higher innate and adaptive cell counts, higher natural killer cell activity, and higher expression rates of major histocompatibility complex-II cell surface receptor [Citation32].
Deep NMB showed a notable lessening effect on surgery-induced proinflammatory response as manifested by the significantly lower measured levels of the studied cytokines with DNMB than CNMB with significantly lower extent of change in measured levels between the IO and PO samples and preoperative samples. In line with these findings, Oh et al. [Citation33] detected significantly smaller changes in IL-6 with DNMB than CNMB and suggested that inflammation related to perioperative complications was inversely related to the depth of NMB. In support of this suggestion, the current study detected negative significant correlation between the extent of change in serum cytokines’ levels and the use of DNMB. Also, Kim et al. [Citation34] found DNMB with low AIP significantly suppressed the increase in IL-6 levels after pneumoperitoneum and attributed this to the detected significant improvement of the respiratory mechanics in comparison with CNMB with high AIP. Thereafter, Albers et al. [Citation35] found low AIP was associated with reduced inflammation markers and circulating damage-associated molecular patterns (DAMPs), with less impaired early PO ex-vivo cytokine production capacity. Similarly, Zhang et al. [Citation36] using DNBM detected significantly lower TNF-α and IL-6 levels than in patients received CNMB at 24-h PO.
On contrary to the obtained results and these literature, Koo et al. [Citation10] detected insignificant differences in levels of IL-6, TNF-α, IL-1β and C-reactive protein between DNMB and CNMB despite of detecting significant differences in surgical conditions, in favor of DNMB, that may influence the extent of tissue injury and release of related mediators and attributed the insignificant difference to the variance between patients’ response to trauma and to the time lag between insult and reaching the peak concentrations of these mediators.
Operative data including IO hemodynamic measures, field visibility, IO blood loss and recovery time showed insignificant differences between both groups. These findings go in hand with Raval et al. [Citation37] who reported no differences between DNMB and CNMB in terms of PACU recovery or the length of hospital stay. Also, Zhang et al. [Citation36] detected insignificant differences between DNMB and CNMB in terms of the operation time, pneumoperitoneum time, and blood loss, extubation time after surgery, PACU stay and TOF%
The obtained results showed significantly lower IO and PO analgesia consumption by patients who received DNMB with reduction of wound pain and STP. Notably, statistical analyses showed a positive significant correlation between the doses of IO fentanyl, operative time and PACU pain scores with the extent of increase in serum cytokines’ levels immediately PO in relation to preoperative levels and the cumulative 24-h PO pain scores and STP during hospital stay were positively correlated with the extent of change in cytokines’ levels in samples obtained at 48-h PO. On the reverse, the extent of change in cytokines’ levels was inversely related to the use of DNMB. Thus, the use of DNMB might brock this vicious cycle of increased inflammatory mediators and increased pain scores and consumption of analgesia. Moreover, ROC curve analysis defined low extent of change in serum IL-6 level and the use of DNMB as predictors for minimal cumulative 24-h pain scores, but multivariate regression analysis defined the provision of DNMB as the determinant factor for low pain scores.
In line with these findings, Raval et al. [Citation37] out of a systemic review found DNMB was associated with a reduction in PO pain scores in PACU and provided minor savings on resource utilization in comparison with CNMB. Additionally, Zhang et al. [Citation36] found patients who received DNMB exhibited significantly lower pain score at 24 and 48 h after surgery and decreased scores of STP than patients of CNMB group. Also, Albers et al. [Citation35] reported significantly lower pain scores with low than conventional AIP.
In trial to explore the pathogenesis of the impact of NMB on surgical pain, previous studies detected an association between surgical tissue injury with a PO state of immune misbalance and immunosuppression of circulating innate immune cells due to the release of DAMPs [Citation38–40]. Subsequent studies found DNMB would reduce tissue tension especially at the incisional sites and consequently reduce tissue damage and the subsequent release of DAMPs and its related immune misbalance and PO pain [Citation10,Citation41].
In support of the better PO course of patients received DNMB and low AIP, Oh et al. [Citation33] detected insignificantly lower frequency of PO delirium but found the amount of PO bleeding until PO day 2 was significantly lower in patients received DNMB than CNMB. Also, Albers et al. [Citation35] documented that the use of low AIP during laparoscopic colorectal surgery is safe, improves the quality of PO recovery with significant reduction of the 30-day PO infectious complications.
23. Conclusions
The use of DNMB with low AIP significantly ameliorated the impact of surgery on immune milieu, reduced IO consumption of narcotic and reduced PO pain during PACU and MICU stay. DNMB and AIP improved pain scores mostly through reduction of release of inflammatory nociceptive cytokines.
24. Recommendation
Wider scale studies were warranted to establish the obtained results. Evaluation of the effect of DNMB on outcomes of LS under epidural anesthesia, which is commonly used, is required.
Availability of data and material
Data are available when requited.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Estivill-Torrús G, Martínez-Padilla A, Sánchez-Salido L, et al. The dorsal root ganglion as a target for neurorestoration in neuropathic pain the dorsal root ganglion as a target for neurorestoration in neuropathic pain. Neural Regen Res. 2024 Feb;19(2):296–301. doi: 10.4103/1673-5374.374655
- Lantos J, Németh T, Barta Z. Pathophysiological advantages of spontaneous ventilation front surg. [2022 Mar 14];9:822560. doi: 10.3389/fsurg.2022.822560
- Jolly S, Kundu N, Rathnayake S. A case of mistaken identity: bile duct masquerading as gallbladder. J Surg Case Rep. [2023 Jan 19];2023(1):rjad001. doi: 10.1093/jscr/rjad001
- Smith RB, Biller E, Hu C. Impact of pneumoperitoneum pressure during laparoscopic hysterectomy: A randomized controlled trial.Eur. J Obstet Gynecol Reprod Biol. 2023 Jan;280:73–77. doi: 10.1016/j.ejogrb.2022.11.011
- Ortenzi M, MontorFi G, Sartori A. Low-pressure versus standard-pressure pneumoperitoneum in laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2022 Oct;36(10):7092–7113. doi: 10.1007/s00464-022-09201-1
- Lowen D, Hodgson R, Tacey M. Does deep neuromuscular blockade provide improved outcomes in low pressure laparoscopic colorectal surgery? A single blinded randomized pilot study. ANZ J Surg. 2022 Jun;92(6):1447–1453. doi: 10.1111/ans.17458
- Liu S, He B, Deng L. Does deep neuromuscular blockade provide improved perioperative outcomes in adult patients? A systematic review and meta-analysis of randomized controlled trials. PLOS ONE. [2023 Mar 9];18(3):e0282790. doi: 10.1371/journal.pone.0282790
- Balsevicius L, Urbano P, Hasselager R. Effect of anterior quadratus lumborum block with ropivacaine on the immune response after laparoscopic surgery in colon cancer: a substudy of a randomized clinical trial. Reg Anesth Pain Med. 2023 Nov;9:rapm-2023–104896. doi: 10.1136/rapm-2023-104896
- Kim HJ, Lee KY, Kim MH. Effects of deep vs moderate neuromuscular block on the quality of recovery after robotic gastrectomy. Acta Anaesthesiol Scand. 2019 Mar;63(3):306–313. doi: 10.1111/aas.13271
- Koo B, Oh A, Ryu J. Effects of deep neuromuscular blockade on the stress response during laparoscopic gastrectomy randomized controlled trials. Sci Rep. [2019 Aug 27];9(1):12411. doi: 10.1038/s41598-019-48919-2
- Faul F, Erdfelder E, Lang AG. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi: 10.3758/BF03193146
- Barrio J, Errando C, Miguel G. Effect of depth of neuromuscular blockade on the abdominal space during pneumoperitoneum establishment in laparoscopic surgery. J Clin Anesth. 2016 Nov Z;34:197–203. doi: 10.1016/j.jclinane.2016.04.017
- Sessler CN, Grap MJ, Ramsay MAE. Evaluating and monitoring analgesia and sedation in the intensive care unit. Crit Care. 2008;12(Suppl 3):S2. doi: 10.1186/cc6148
- Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. doi: 10.1111/j.1365-2702.2005.01121.x
- Watcha MF, White PF. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology. 1992;77(1):162–184. doi: 10.1097/00000542-199207000-00023
- Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995 Feb;7(1):89–91. doi: 10.1016/0952-8180(94)00001-k
- Myles PS, Weitkamp B, Jones K. Validity and reliability of a postoperative quality of recovery score: the QoR-40. Br J Anaesth. 2000;84(1):11–15. doi: 10.1093/oxfordjournals.bja.a013366
- Shida D, Wakamatsu K, Tanaka Y. The postoperative patient-reported quality of recovery in colorectal cancer patients under enhanced recovery after surgery using QoR-40. BMC Cancer. 2015;15:799. doi: 10.1186/s12885-015-1799-3
- Madsen MV, Istre O, Staehr-Rye A. Postoperative shoulder pain after laparoscopic hysterectomy with deep neuromuscular blockade and low-pressure pneumoperitoneum: a randomised controlled trial. Eur J Anaesthesiol. 2016 May;33(5):341–347. doi: 10.1097/EJA.0000000000000360
- Dinarello CA. ELISA kits based on monoclonal antibodies do not measure total IL-1β synthesis. J Immunol Methods. 1992;148(1–2):255–259. doi: 10.1016/0022-1759(92)90179-W
- Gaines-Das RE, Poole S. The international standard for interleukin-6—evaluation in an international collaborative study. J Immunol Methods. 1993;160(2):147–153. doi: 10.1016/0022-1759(93)90172-4
- Coughlan MT, Oliva K, Georgiou HM. Glucose-induced release of tumor necrosis factor-alpha from human placental and adipose tissues in gestational diabetes mellitus. Diabet Med. 2001;18(11):921–927. doi: 10.1046/j.1464-5491.2001.00614.x
- Wang HJ, Ding YC. A analysis of ELISA on the time-related expression of IL-2 and TNF-alpha during the healing process of the wound in rat skin. Fa Yi Xue Za Zhi. 2003;19(1):10–12.
- Bai R, Wan L, Shi M. The time-dependent expressions of IL-1beta, COX-2, MCP-1 mRNA in skin wounds of rabbits. Forensic Sci Int. 2008;175(2–3):193–197. doi: 10.1016/j.forsciint.2007.07.006
- Takamiya M, Fujita S, Saigusa K. Simultaneous detection of eight cytokines in human dermal wounds with a multiplex bead-based immunoassay for wound age estimation. Int J Legal Med. 2008;122(2):143–148. doi: 10.1007/s00414-007-0183-5
- Takamiya M, Biwasaka H, Saigusa K. Wound age estimation by simultaneous detection of 9 cytokines in human dermal wounds with a multiplex bead-based immunoassay: an estimative method using outsourced examinations. Leg Med (Tokyo). 2009;11(4):186–190. doi: 10.1016/j.legalmed.2009.03.010
- Varadhan K, Constantin-Teodosiu D, Constantin D. Inflammation-mediated muscle metabolic dysregulation local and remote to the site of major abdominal surgery. Clin Nutr. 2018 Dec;37(6 Pt A):2178–2185. doi: 10.1016/j.clnu.2017.10.020
- Dobson G, Morris J, Biros E. Major surgery leads to a proinflammatory phenotype: Differential gene expression following a laparotomy. Ann Med Surg. [2021 Oct 21];71:102970. doi: 10.1016/j.amsu.2021.102970
- Faisal M, Schäfer C, Myrelid P. Effects of analgesic and surgical modality on immune response in colorectal cancer surgery. Surg Oncol. 2021 Sep;38:101602. doi: 10.1016/j.suronc.2021.101602
- Erginel B, Karadeniz M, Yuksel S. Can serum soluble urokinase plasminogen activator receptor be an effective biomarker in comparing the inflammatory response between laparoscopic and open appendectomy? Wideochir Inne Tech Maloinwazyjne. 2023 Jun;18(2):351–357. doi: 10.5114/wiitm.2023.128681
- Cheng X, Wang C, Liu Y. Effects of different radical distal gastrectomy on postoperative inflammatory response and nutritional status in patients with gastric cancer. Front Surg. [2023 Mar 15];10:1112473. doi: 10.3389/fsurg.2023.1112473
- Bohne A, Grundler E, Knüttel H. Influence of laparoscopic surgery on cellular immunity in colorectal cancer: a systematic review and meta-analysis. Cancers (Basel). [2023 Jun 28];15(13):3381. doi: 10.3390/cancers15133381
- Oh C, Lim H, Jeon H. Effect of deep neuromuscular blockade on serum cytokines and postoperative delirium in elderly patients undergoing total hip replacement: A prospective single-blind randomised controlled trial. Eur J Anaesthesiol. [2021 Mar 1];38(Suppl 1):S58–S66. doi: 10.1097/EJA.0000000000001414
- Kim J, Min S, Ha E. Effects of deep neuromuscular block with low-pressure pneumoperitoneum on respiratory mechanics and biotrauma in a steep Trendelenburg position. Sci Rep. [2021 Jan 21];11(1):1935. doi: 10.1038/s41598-021-81582-0
- Albers K, Polat F, Helder L. Recover study collaborators quality of recovery and innate immune homeostasis in patients undergoing low-pressure versus standard-pressure pneumoperitoneum during laparoscopic colorectal surgery (RECOVER): a randomized controlled trial. Ann Surg. [2022 Dec 1];276(6):e664–e673. doi: 10.1097/SLA.0000000000005491
- Zhang Y, Li Y, Huang W. Utilization of deep neuromuscular blockade combined with reduced abdominal pressure in laparoscopic radical gastrectomy for gastric cancer: an academic perspective. World J Gastrointest Surg. [2023 Jul 27];15(7):1405–1415. doi: 10.4240/wjgs.v15.i7.405
- Raval A, Deshpande S, Rabar S. Does deep neuromuscular blockade during laparoscopy procedures change patient, surgical, and healthcare resource outcomes? A systematic review and meta-analysis of randomized controlled trials. PLoS One. [2020 Apr 16];15(4):e0231452. doi: 10.1371/journal.pone.0231452
- Máca J, Burša F, Ševčík P. Alarmins and clinical outcomes after major abdominal surgery-A prospective study. J Invest Surg. 2017 Jun;30(3):152–161. doi: 10.1080/08941939.2016.1231855
- Leijte G, Custers H, Gerretsen J. Increased Plasma levels of danger-associated molecular patterns are associated with immune suppression and postoperative infections in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Front Immunol. [2018 Apr 5];9:663. doi: 10.3389/fimmu.2018.00663
- Vourc’h M, Roquilly A, Asehnoune K. Trauma-induced damage-associated molecular patterns-mediated remote organ injury and immunosuppression in the acutely Ill patient. Front Immunol. [2018 Jun 15];9:1330. doi: 10.3389/fimmu.2018.01330
- Bijkerk V, Visser J, Jacobs L. Deep versus moderate neuromuscular blockade during total hip arthroplasty to improve postoperative quality of recovery and immune function: protocol for a randomised controlled study. BMJ Open. 2023;13(8):e073537. doi: 10.1136/bmjopen-2023-073537