ABSTRACT
Dental implants have been used for the last 20 years. With the latest modern developments, however, minimally invasive protocols and immediate implants are currently used. The aim of this study was to evaluate the primary stability of a new implant design. Thirty immediate implants were placed and they all achieved successful osseointegration. Primary stability was reached with all the implants after the first apical threads. Within the limitations of the present study, the immediate implant approach seems to be a predictable treatment option, especially in conjunction with a specifically designed implant system.
Introduction
Dental implants are consolidated treatments for replacing missing teeth, allowing restoration of chewing function, speech and aesthetics. Implants are inserted into the jawbones to support a dental prosthesis and are retained because of the intimacy of bone growth on to their surface. Such direct structural and functional connection between living bone and implant surface, termed osseointegration, has surely been one of the most significant scientific breakthroughs in dentistry over the past 30 years.[Citation1]
Before placing dental implants, teeth are removed and the extraction sockets are left to heal for several months. After tooth extraction, however, alveolar ridge resorption may be observed, which leads to reduced bone volume and an average loss of buccal contour. This has an undesirable effect on implant positioning, since the achieved restoration may not be optimal.[Citation2–4] The problem is particularly undesirable at the anterior maxilla and aesthetic areas.[Citation5]
This problem could be avoided by early implant placement into the extraction sockets.[Citation2,Citation3] The great majority of patients (and clinicians as well) are in favour of shortening the treatment time between tooth extraction and implant placement, or even better in having the implants inserted during the same session as the teeth are extracted (immediate implants).[Citation2]
The placement of implants into fresh extraction sockets was introduced in the late 1970s and has been further developed (for review, see [Citation6–8]). Several recent papers have presented clear clinical guidelines for patient selection and/or for achieving an optimal outcome.[Citation7]
The approach of immediate post-extraction implant placement is often preferred because the result is favourable from an aesthetic point of view; the procedure shortens the treatment and surgical time and allows for preservation of the socket walls. A potential disadvantage with immediate implants could be the mismatch between the implant surface and the socket wall; therefore, gaps may be present after implantation since dental roots do not have a regular circular diameter shape. It is also possible that one or more bony socket walls are either partly resorbed due to the disease processes or damaged as a result of the tooth extraction procedure.[Citation2]
These potential problems have been tackled in different ways. As reviewed,[Citation2] manufacturers have designed specific systems for immediate implantation including fixtures having various tapered shapes and different diameters for use with sockets of varying dimensions.
In some cases, it is recommended to use immediate-delayed implants, in which the soft-tissue is allowed to start healing for about two or three weeks prior to implant placement. Another option is to choose among a range of methods for augmentation/regeneration of the bone between the extraction sockets and the surface of the implant, e.g. autologous bone grafting, guided bone regeneration using resorbable or non-resorbable barriers, bone substitutes, and different bone-promoting materials.[Citation6,Citation9,Citation10]
In order to achieve successful osseointegration, epithelial tissue exclusion and blood clot stabilization have been indicated as critical factors. To achieve these goals, it has been suggested to apply a barrier membrane. However, immediate implant placement into fresh extraction sockets, both with or without a membrane, has not been shown to prevent bone resorption that may amount to more than 50% at the buccal side and 30% at the palatal side. Most of the resorption occurs over the first three months following extraction.
The aim of this study was to evaluate the primary stability of single implants placed in fresh extraction sockets, using a new implant design, with tapered morphology.
Subjects and methods
Study design
This study was a clinical trial. Edentulous areas were restored in 30 patients. Each patient provided only one implant site. At the screening, the operator freely selected one implant site to be included in the trial. The trial had a three-year post-loading duration. For each implant, the primary stability as well as bone level changes and the aesthetic result were evaluated by a single blinded and independent assessor.
The principles outlined in the Declaration of Helsinki on clinical research involving human subjects were adhered to.
Inclusion criteria
Any patient requiring at least one single immediate post-extractive implant, being at least 18 years old and able to sign an informed consent was enrolled, with the presence of the two adjacent teeth or at least other implants, but not near to edentulous ridges. The patients were grouped into (1) non-smokers; (2) light smokers (≤10 cigarettes/day) and (3) heavy smokers (≥11 cigarettes/day), according to what they declared.
Pre-operative radiographs were taken and the principal clinical investigator was free to choose the most appropriate examination according to the clinical case (intra-oral, panoramic, computed tomography scans, etc.).
Exclusion criteria
Patients with the following characteristics were excluded: general contraindications to implant surgery, immunosuppressed or immunocompromised status, irradiation in the head and/or neck, uncontrolled diabetes, pregnancy or lactation, poor oral hygiene and motivation, addiction to alcohol or drugs, psychiatric problems, acute infections (abscess) in the site intended for implant placement, necessity to lift the maxillary sinus; patients not able to commit to a three-year follow-up, patients treated or under treatment with intravenous amino-bisphosphonates and patients with partial absence of the buccal bone, as it may compromise the aesthetic outcome of implant placement.
All the patients were drawn from Genoa University, Laser and Restorative Center, and prior to the enrolment, participants were asked to sign an informed consent form to document that they understand the scope of the study (including procedures, follow-up evaluations and any potential risks involved); they were allowed an opportunity to ask questions pertaining to this study and were apprised of treatment alternatives. The study was open to qualifying patients without regard to sex or race.
After determining that a patient was qualified for the study, and informed consent was obtained, a thorough oral examination was performed to assess the health status, identify oral pathologies that require treatment prior to implant therapy and analyse available bone over vital structures and adjacent to remaining natural teeth. Other medical tests and/or consultation with the patient's physician were sometimes indicated by the presence of compromised medical conditions.
Comprehensive hard- and soft-tissue examinations were also performed in order to rule out undiagnosed malignancies or dysplastic oral, head and neck lesions. Investigators attempted to identify inflammatory disease, unfavourable and excessive occlusal forces and other pathologies that could threaten the long-term survival of the dental implant restoration. Malocclusion, severe caries, periapical lesions and periodontal disease were identified and eliminated, as well as unacceptable occlusion from tipped or overerupted teeth. The remaining dentition was checked for evidence of enamel wear, chipping and faceting as indicators of destructive parafunctional habits. The temporomandibular joints were also evaluated for deviations in function, joint sounds and/or pain.
After a patient had been diagnosed medically, dentally, psychologically, functionally and anatomically to be a good candidate for dental implant therapy and was committed to pursuing treatment and follow-up as a study participant, a complete diagnostic work-up was undertaken.
Implant selection was predicted on the location and anatomic morphology of the proposed implant receptor site and its contiguous structures. Therefore, radiographic examinations were performed to assist with treatment planning and were used as a screening tool to assess the patient's overall dental health. Intra-oral or panoramic radiographs were used to verify that no contraindicated abnormalities are present (i.e. root tips, cysts, anatomic anomalies, etc.) and to identify the locations of the mandibular canal, maxillary sinus cavities, nasal cavity, as well as adjacent dentition relative to the proposed implant site.
Implant placement
Prophylactic therapy
Amoxicillin 2 g, 1 hour prior to the intervention. Patients allergic to penicillin were prescribed clindamycin 600 mg, 1 hour prior to the intervention. Mouth rinse with chlorhexidine 0.2% for 1 minute was done prior to the intervention.
Local anaesthesia
Local infiltration with articaine (with adrenaline 1:100.000) was used.
Tooth extraction
Tooth extractions were performed as atraumatically as possible, attempting to preserve the buccal alveolar bone. Extraction sockets were carefully cleaned from any remains of granulation tissue.
Implant type
BT SAFE Bone Level Implant (BTK, Vicenza, Italy) with internal connection, composed of titanium on the surface. The operators were free to choose implant lengths (8.5, 10, 11.5, 13 and 15 mm) and diameters (4 or 5 mm), according to the clinical indications and their preferences ().
Table 1. Distribution of implants used in this study according to diameter and position.
Implant installation technique
Drills with increasing diameters (2, 2.8, 3.5 mm and when needed 4.3 mm) were used to prepare the implant site as suggested by the manufacturer. The choice of the implant diameter and length was recorded. Implants were placed crestally; however, in aesthetic areas, the operator could place the head of the implant slightly subcrestally, about 1–2 mm below the most apical bone peak, and slightly palatally. The implant insertion torque was also assessed with a manual wrench and reported as ≥20 or <20 N cm.
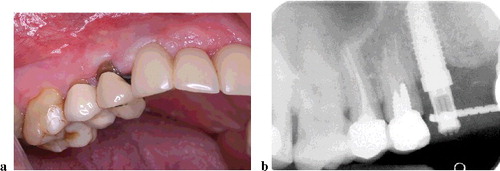
Clinical pictures of the vestibular and occlusal aspects were taken and the horizontal gap between the bone and the implant was measured intra-surgically and reported in millimetres. Implants were left to heal unloaded for 3–4 months (–).
Post-surgical instructions and follow-up
Patients were instructed according to the following protocol:
ibuprophen 400 mg to take only in case of pain;
chlorhexidine mouthwash 0.2% for 1 minute twice a day for 2 weeks;
post-operative antibiotics: amoxicillin 1 g twice a day for six days. For patients allergic to penicillin, clindamycin was prescribed 300 mg twice a day for six days.
Check-ups
The check-up schedule was at one week and one month after the implant placement.
Three/four months after placement
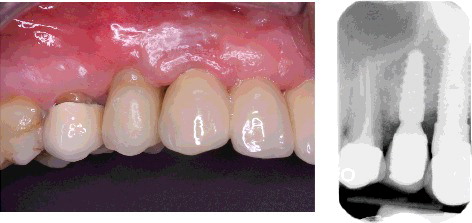
After abutment connection, implants were manually tested for stability. An impression with the pick-up impression copings was made with a polyether material in order to deliver a provisional crown in acrylic resin which was fixed on the analogue with a temporary cylinder and a titanium screw. After this procedure, the final crown in metal ceramic or metal acrylic was placed both cemented and screw-retained.
One and three years after loading
Crowns were manually tested for stability. During the follow-up period, patients were recalled every six months for professional cleaning.
Results and discussion
Thirty implants were placed and no major complications or implant failures occurred during the follow-up period. Almost all the implants achieved the primary stability (>25 N cm) after the insertion of the apical treads (). Single crowns, either cemented or screw-retained, were delivered after the usual healing period and the stability of the implants was manually tested, without any breakdown ().
Table 2. Number of implants which reached the primary stability with the mechanical handpiece and implants which needed the manual wrench. Long-time stability.
Figure 4. Case tooth #12, where implant primary stability was achieved with the mechanical handpiece only. Atraumatic extraction (a), implant placement and time of primary stability (b and c).

Primary stability is a requirement for osseointegration. However, controlled values of the insertion torque are needed in order to not increase bone remodelling around the implants and possibly lead to a resorption of most coronal threads.[Citation11] In post-extraction sites, the anatomy itself is not favourable for faster achievement of primary stability and osseointegration.[Citation2–4] In this case, many factors can be taken into account to speed up the process and make it successful: bone density and quality,[Citation5] implant morphology and design, implant surface.[Citation12,Citation13]
The implant system used in this specific trial (BT SAFE Bone Level Implants) has a specific implant body design with a quite accentuated morphology, which enables faster insertion, in conjunction with a double-thread design to direct the drilled bone immediately in contact with the surface of the implant.
Insertion torque values need to be discussed because in all cases they were higher than 25 N cm, but always less than 50 N cm (manually tested with a dynamometric wrench). The 50 N cm value is an important reference point according to recent evidence reported by Barone et al.,[Citation11] who observed that implants inserted with high-insertion torque (≥50 N cm) in healed bone ridges showed more peri-implant bone remodelling and buccal soft-tissue recession than implants inserted with a regular-IT (<50 N cm).
In all cases where the marginal gap between the implant and the buccal bone wall was higher than 2 mm, a bovine inorganic bone substitute was placed, which, according to the published evidence, shows greater benefit in bone level maintenance and aesthetic scores.[Citation6,Citation8,Citation9,Citation14,Citation15]
The implant body material is titanium grade 4 and the surface is of controlled micro-roughness obtained through a double-acid etching process. As reported by the manufacturer,[Citation16] morphologic analysis by scanning electron microscopy shows that this roughness of the treatment surface favours initial osteoblastic anchoring and, therefore, the interaction with the bone tissue. As a result, this makes the osseointegration time shorter.
Although the number of cases in this study was relatively small, the results suggest that the implant system and the new implant design are promising because of a more aggressive insertion in the bone. The threads achieve faster implant installation and the coronal design is meant to totally preserve the cortical part.
Conclusions
Within the limitations of the present study, the immediate implants approach seems to be a predictable treatment option, especially in conjunction with a specifically designed implant system. However, further studies, especially controlled clinical trials, are needed in order to support this conclusion.
Acknowledgments
The study was conducted with the support of Biotec Company BTK – the smile system.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Weinstein T. Immediate implant placement into dentoalveolar sockets in conjunction with plasma rich in growth factor [dissertation]. Milan (Italy): The University of Milan; 2011–2012. Available from: http://hdl.handle.net/2434/173986.
- Esposito M, Grusovin MG, Polyzos IP, et al. Interventions for replacing missing teeth: dental implants in fresh extraction sockets (immediate, immediate-delayed and delayed implants). Eur J Oral Implantol. 2010;3(3): 189–205. Review.2.
- Gher ME, Quintero G, Assad D, et al. Bone grafting and guided bone regeneration for immediate dental implants in humans. J Periodontol. 1994;65:881–891.
- Prosper L, Gherlone EF, Redaelli S, et al. Four-year follow-up of larger-diameter implants placed in fresh extraction sockets using a resorbable membrane or a resorbable alloplastic material. Int J Oral Maxillofac Implant. 2003;18:856–864.
- Wang R, Eppell SJ, Nguyen C, et al. Relative contribution of trabecular and cortical bone to primary implant stability: an in vitro model study. J Oral Implantol. Forthcoming 2015. Available from: http://dx.doi.org/10.1563/aaid-joi-D-14-00322 Epub ahead of print.
- Chen ST, Darby IB, Adams GG, et al. A prospective clinical study of bone augmentation techniques at immediate implants. Clin Oral Implant Res. 2005;16:176–184.
- Quirynen M, Van Assche N, Botticelli D, et al. How does the timing of implant placement to extraction affect outcome? Int J Oral Maxillofac Implants. 2007;22 Suppl:203–223. Review. Erratum in: Int J Oral Maxillofac Implants. 2008;23(1):56
- Khzam N, Arora H, Kim P, et al. Systematic review of soft tissue alterations and esthetic outcomes following immediate implant placement and restoration of single implants in the anterior maxilla. J Periodontol. 2015;86(12):1321–1330. doi:10.1902/jop.2015.150287. Epub 2015 Aug 27.
- Cornelini R, Cangini F, Martuscelli G, et al. Deproteinized bovine bone and biodegradable barrier membranes to support healing following immediate placement of transmucosal implants: a short-term controlled clinical trial. Int J Periodont Restor Dent. 2004;24:555–563.
- Fiorellini JP, Howell TH, Cochran D, et al. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol. 2005;76:605–613.
- Barone A, Alfonsi F, Derchi G, et al. The effect of insertion torque on the clinical outcome of single implants: a randomized clinical trial. Clin Implant Dent Relat Res. Forthcoming 2015. doi:10.1111/cid.12337. Epub ahead of print.
- Sennerby L, Pagliani L, Petersson A, et al. Two different implant designs and impact of related drilling protocols on primary stability in different bone densities: an in vitro comparison study. Int J Oral Maxillofac Implants. 2015;30(3):564–568.
- Lee SY, Kim SJ, An HW, et al. The effect of the thread depth on the mechanical properties of the dental implant. J Adv Prosthodont. 2015;7(2):115–121.
- De Angelis N, Felice P, Pellegrino G, et al. Guided bone regeneration with and without a bone substitute at single post-extractive implants: 1-year post-loading results from a pragmatic multicentre randomised controlled trial. Eur J Oral Implantol. 2011;4(4):313–325.
- Chen ST, Darby IB, Reynolds EC. A prospective clinical study of non-submerged immediate implants: clinical outcomes and esthetic results. Clin Oral Implant Res. 2007;18:552–562.
- BTK. Dental implants. Complete choice guide [Internet]. 16th April 2013. Available from: http://www.bioteconline.com/public/mat/allegati/prodotti_file_id38_en.pdf