ABSTRACT
The aim of this study was to explore the cost-effectiveness of short protocols including different types of gonadotropins for controlled ovarian hyperstimulation (COH) for in vitro fertilization (IVF). A retrospective, observational study of the real-life practice in a specialized IVF gynaecology clinic in 2009–2013 was carried out. All women on short COH protocols were recruited into three groups: COH including recombinant follicle stimulating hormone (rFSH) and urinary-FSH (urFSH) (n = 173); including urFSH alone (n = 289); and including rFSH alone (n = 212). The cost-effectiveness of the COH protocols was explored in two different case scenarios for possible outcomes. The first case scenario took into consideration a successful live birth, and the second one, the women to achieve pregnancy with live birth. Decision modelling was done using the TreeAge 2014 Software. According to the results in the first case scenario, the rFSH plus urFSH COH approach showed the highest weighted probability (p = 0.38) of live birth, but the urFSH alternative was cost-effective. The results in the second case scenario demonstrated that the urFSH protocol was again the cost-effective alternative. These results suggest that the strategy with urFSH should be preferred in both cases, but rFSH could also be considered as a cost-effective alternative for successful live birth and achieving pregnancy and delivery, since the incremental cost-effectiveness ratio in comparison with the urFSH protocol is below the gross domestic product per capita. The combined approach of rFSH and urFSH was shown not to be cost-effective in both explored scenarios.
Introduction
Ovarian stimulation is the critical part of the medication management of in vitro fertilization (IVF) therapy.[Citation1] A variety of efficacious controlled ovarian hyperstimulation (COH) regimens are used, but their cost-effectiveness needs to be further explored in terms of individualized management of successful pregnancy and delivery. Development of biotechnologically derived recombinant products also contributes to the success of IVF.[Citation2–6]
A cost-effectiveness study on the higher efficacy of follitropin-beta, a new recombinant follicle stimulating hormone (rFSH), versus urinary-FSH (urFSH), found that the incremental cost-effectiveness ratio (ICER) varies from 19.2 to 26.0 million Italian lire (11 300 $US and 15 400 $US) depending on the setting and the type of treatment.[Citation7] The cost-effectiveness and economic aspects of the IVF methods have been explored after transfer of one or two embryos.[Citation8,Citation9] Comparative analysis in terms of cost-effectiveness has been performed on rFSH versus urFSH by using modelling techniques [Citation10,Citation11], as well as on three gonadotropin treatments: with rFSH, highly purified urFSH and human menopausal gonadotropins (hMGT), by also exploring the possibility for IVF failure.[Citation12]
This study was based on the recommendations by Garceau et al. [Citation13] that the cost-effectiveness of different interventions should be considered when making decisions about treatment, especially in health-care settings with limited budgets. The aim of the study was to explore the cost-effectiveness of three short COH protocols including different types of gonadotropins for IVF. The first one is a combination of rFSH (follitropin-alfa or follitropin-beta) and urFSH (highly purified human FSH/ highly purified hMGTs), the second one is with urFSH only and the third one is with rFSH only. The study was performed from the point of view of the IVF clinic for a period of five years. It addressed the question of which of the studied COH approaches is cost-effective resulting in (1) live-born children and (2) women with pregnancies and live birth.
Subjects and methods
Study cohort and design
A retrospective, observational study of the real-life practice in a specialized IVF gynaecology clinic in 2009–2013 was carried out. Information was collected about the short protocol COH approaches used in the clinic for all patients admitted during the period. All women with short protocols of COH (n = 674) out of all 685 admitted women were recruited into three groups according to the type of follicular stimulating hormone (FSH) included in the short COH protocols as follows (): COH including rFSH and urFSH (n = 173), COH including urFSH alone (n = 289) and COH including rFSH alone (n = 212). All patients gave their informed consent. The study complied with the ethical guidelines of the Medical University of Sofia.
Table 1. Description of the studied COH protocols.
All other medicines included in the protocols were also systematized. A record was kept of the number of live-born children and women with live birth. Due to multiple pregnancies, in some cases the numbers differ (). Within the framework of the chosen setting, an attempt was made to identify which of the adopted practices gave better results.
Table 2. Characteristics of the study cohort.
The choice of stimulation short protocol was made primarily based on (1) the individual characteristics of the patient (age, habitat, ovarian reserve, BMI (body mass index), presence of polycystic ovary syndrome (PCOS),[Citation14] ovarian response to stimulation during a previous cycle (if available)); (2) price of medicines; and (3) experience and preferences of the physician leading the stimulation. In the observed clinic, only one team of physicians was responsible for ovarian stimulation and, therefore, there were considered to be no differences in the experience. Every woman in the study was assigned to a particular COH protocol group based on the above-mentioned criteria and the real-life choice of the physician.
Modelling
To explore the cost-effectiveness of the studied COH approaches, two scenarios were designed. The decision tree model was built using TreeAge 2014 software. The first step was to create the model framework for the two scenarios. The model was used to analyse the three COH approaches as compared with therapeutic alternatives and expected results.
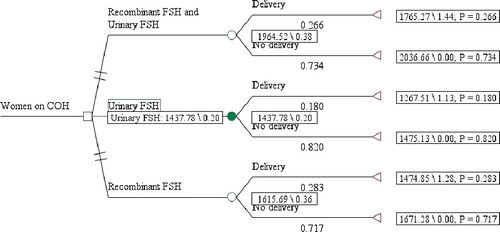
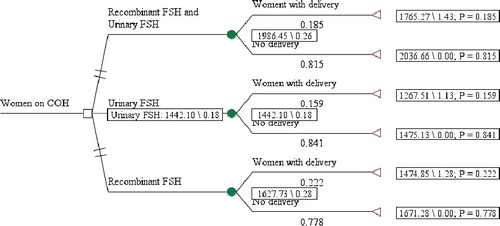
The first case scenario was designed to take into consideration only the criterion successful child delivery (number of live-born children). For each COH alternative, two possible chance node outcomes were considered, i.e. delivery (live birth) or no delivery. The second case scenario was created to explore the cost-effectiveness of the three COH approaches in regard to conceiving and delivering (live birth). In this scenario, the chance nodes were women with delivery (live birth) and no delivery ().
Data analysis
The average cost and standard deviation (SD) of the three COH approaches in the model were calculated for each chance node: group on rFSH and urFSH with delivery (live birth) and no delivery; group with urFSH with delivery (live birth) and no delivery; group with rFSH with delivery (live birth) and no delivery, for the first case scenario on the basis of the real-life data in the clinic for a five-year period. Information about the prices of all medicines included in the COH protocols for each woman was gathered from the positive drug list at the 2014 price level in the local currency (exchange rate 1 BGN = 0.95 Euro).[Citation15] After defining the groups, the average cost per protocol was calculated ().
Table 3. Cost of COH protocols.
In the first case scenario, probabilities were derived considering the live-born children in the clinic in each of the compared alternatives. In the second case scenario, the probability of a woman conceiving and delivering was considered instead. Only live births were considered in both scenarios.
The results are presented as number of live-born children for each alternative. ICER was calculated using the classical formula [Citation16] and the cost-effectiveness plate was built.
Results and discussion
Various types of COH protocols have been developed for the purposes of assisted reproductive technologies, but two of them are seen as the ‘gold standard’: a long protocol with gonadotropin-releasing hormone agonist (GnRH agonist) and a short protocol with (gonadotropin-releasing hormone antagonist (GnRH antagonist). With the emergence of GnRH antagonists in the last century, the short antagonist protocol is gaining popularity, as it has a few advantages over the long protocol with a GnRH agonist. The advantages are that it is a short, simple and convenient method of stimulation which is well tolerated by the patient; it gives the possibility to reduce the dose of gonadotropins and to minimize the risk of side effects; there is decreased risk of ovarian hyperstimulation syndrome (OHSS); the method provides patient comfort and better clinical results of IVF cycles, which are comparable with those achievable via long protocols with a GnRH agonist.[Citation17–19] In this study, three short COH protocols were analysed from the point of view of cost-effectiveness, since the results could differ depending on the medicines used for COH. The first one is a combination of rFSH (follitropin-alfa or follitropin-beta) and urFSH (highly purified human FSH/highly purified human menopausal gonadotropins), the second one is with urFSH only and the third one is with rFSH only.
Short COH protocols
The three short COH protocols as alternative approaches are presented in . The choice of the COH protocol and the combination of medicines depends on the individual characteristics of each patient: age, habitat, ovarian reserve, BMI, presence of PCOS,[Citation14] and ovarian response to stimulation during a previous cycle (if data were available). The three groups in this study were defined based on the groups of medicines included in the short COH protocols: recombinant gonadotropins, urinary gonadotropins or a combination of both. The possible sub-combinations of medicines within these three groups that were used in the stimulation protocols are also given in
Different combinations were applied in each group for patients with poor ovarian response. The characteristics of the compared groups of women are given in . The majority of women received urFSH, which is the least costly COH approach, but with the lowest probability of live birth and of women conceiving and delivering (live birth). On the other hand, this approach led to a relatively high share of pregnancies (28.3%). The highest probability of child delivery and of women conceiving and delivering was observed in the group on rFSH.
The results from the cost analysis showed that the cost of COH was the highest in the group of women treated with a combination of rFSH and urFSH (), which is not surprising, given the higher cost of combination therapy. The approach that uses rFSH ranked second in terms of costs, and the urFSH protocol ranked third.
The average cost of COH in the case of undelivered women was shown to be higher. This could probably be due to poor ovarian response in these women, since women with poor ovarian response require more medicines and longer time for stimulation, which naturally incurs higher costs.
First case scenario (number of live-born children)
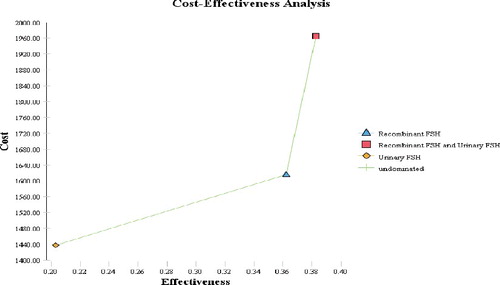
The basic decision tree for the first case scenario showed that the alternative COH approach which includes rFSH and urFSH is with the highest weighted probability (p = 0.38) of live birth. When the costs were added to the analysis and the cost-effectiveness was calculated, the obtained results indicated that the alternative with urFSH should be the preferred one from the viewpoint of the number of delivered live-born children ().
The urFSH alternative was shown to be the cost-effective choice from the perspective of live-born children ().
The ICER for the rFSH alternative could also be considered as acceptable from the point of view of the gynaecology clinic (). It falls far below the accepted threshold for the gross domestic product (GDP) per capita.[Citation20]
Table 4. ICER table in the first case scenario.
Second case scenario (number of women to conceive and give live birth)
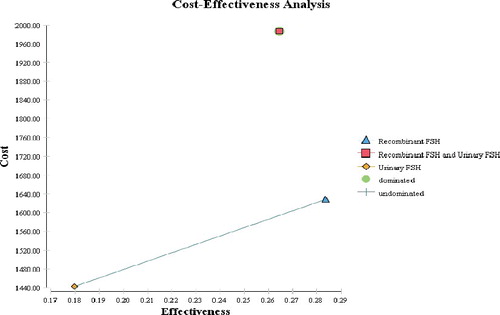
In the second case scenario, we observed that the alternative COH approach including rFSH is with the highest weighted probability (p = 0.28) of women conceiving and delivering (one or more) live-born child. When the analysis was extended to take into consideration the costs and the cost-effectiveness of the alternatives, again the urFSH stood out as the choice to be preferred from the point of view of women conceiving and delivering a live-born child ().
The urFSH protocol was shown to be the least costly alternative but with the lowest weighted probability of success for a woman to conceive and successfully give birth in this case scenario ().
The ICER for the rFSH approach in the second case scenario is also below the recommended threshold of GDP per capita and can be considered a cost-effective alternative (). In this scenario, the alternative with rFSH and urFSH is dominated by the rFSH alternative because the combination has higher cost and lower probability of success. Thus, the alternative with rFSH and urFSH is not likely to be recommended from the point of view of the IVF clinic ().
Table 5. ICER table in the second case scenario.
Comparative analysis
In a variety of healthcare settings, short protocols are connected with decreased overall cost of treatment. Based on the data accumulated on a global scale and our clinics’ experience, we suggest the short protocol with a GnRH antagonist as more appropriate and this can explain the majority of patients treated with short protocols. This experience is also in line with the results from randomized clinical trials, which have shown that the short protocol with a GnRH antagonist is the first choice in IVF programmes, with fewer complications, reduced risk of OHSS and sufficient success.[Citation17,Citation21]
In all types of stimulation protocols, ovarian stimulation is performed with gonadotropins (FSH products: urinary, recombinant or a combination of both). In recent years, many studies and debates have been conducted on the effectiveness of rFSH compared to urFSH. A study in 2001 reported a greater percentage of clinical pregnancies when using urFSH as compared to rFSH.[Citation18] Based on the contrasting data published in the following years, 10 years later, the same authors reported their key Cochrane study comparing the effectiveness of rFSH to that of three types of urFSH.[Citation19] The results showed no difference in the performance of different FSH products in terms of clinical pregnancies, live births and safety, both in fresh and frozen IVF cycles.[Citation22,Citation23]
Regarding the questions addressed in our study, the results suggest that the urFSH strategy should be preferred as the most cost-effective alternative in both case scenarios because the cost per unit of result is lower. The rFSH alternatives could also be considered cost-effective in terms of the number of delivered live-born children as well as in terms of the number of women with successful conception and delivery because the ICER is below the GDP per capita threshold recommended by health economists.[Citation16] The rFSH and urFSH combination approach was shown not to be cost-effective in both explored scenarios from the point of view of the clinic.
Short stimulation protocols including only urFSH are applied mainly in patients of advanced maternal age (over 35 years) and those with reduced ovarian reserve (FSH levels less than 15 mIU/mL, anti-Müllerian hormone levels under 0.8–1 ng/mL and 2–3 antral follicles in each ovary). The practice of applying short protocols in women aged over 35 years has been recommended in several studies.[Citation24–26] The higher biological activity of urinary products is necessary in extreme cases, when stronger stimulation is required, i.e. in patients of advanced maternal age and those with reduced ovarian reserve. The price of urinary products is also important in these cases and high doses of FSH are needed to achieve satisfactory results.
The frequent choice of urFSH as a COH strategy could be explained by the individual patients’ characteristics (age over 35 years, reduced ovarian reserve) as well as by the lowest average cost of this alternative in comparison with the other two approaches. These results confirm the conclusions of other authors [Citation27,Citation28] that, in choosing the COH strategy, it is necessary to individualize the approaches considering a variety of factors, and not only the cost of COH.
Our study, however, has some limitations: it was only focused on COH medication therapy and did not explore other factors, such as physicians’ experience, different settings among the clinical centres, etc. The reasoning behind the choice of factors to be analysed was based on the aim to optimize the future choices for COH by also considering the probability of successful pregnancy and delivery. Although our study was a retrospective analysis, the results would aid future therapeutic decisions in cases of doubt as to which strategy would most likely be successful or cost-effective.
Conclusions
The results from this study indicated that the strategy with urFSH should be further preferred in both case scenarios (live-born children or women who conceive and give live birth). rFSH could also be considered as a cost-effective alternative in both these case scenarios because the ICER in comparison with urFSH is below the GDP per capita. The combination approach of rFSH and urFSH was shown not to be cost-effective in both explored scenarios from the point of view of the clinic. Although the conclusions are valid only for the particular clinic observed in our study, they could also be used in making therapeutic decisions by any other IVF clinic with similar therapeutic practices.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Murat A, Bocca S, Mirkin S, et al. Controlled ovarian hyperstimulation protocols for in vitro fertilization: two decades of experience after the birth of Elizabeth Carr. Fertil Steril. 2005;3:555–569.
- Jones GS, Garcia JE, Rosenwaks Z. The role of pituitary gonadotropins in follicular stimulation and oocyte maturation in the human. J Clin Endocrinol Metab. 1984;59:178–180.
- Scott RT, Toner JP, Muasher SJ, et al. Follicle-stimulating hormone levels on cycle day 3 are predictive of in vitro fertilization outcome. Fertil Steril. 1989;51:651–654.
- Jain T, Soules MR, Collins JA. Comparison of basal follicle-stimulating hormone versus the clomiphene citrate challenge test for ovarian reserve screening. Fertil Steril. 2004;82:180–185.
- Hugues JN. Ovarian stimulation for assisted reproductive technologies. In: Vayena E, Rowe PJ, Griffin PD, editors. Current practices and controversies in assisted reproduction. Geneva: World Health Organization; 2002. p. 102–125.
- Jones GS, Acosta AA, Garcia JE, et al. The effect of follicle-stimulating hormone without additional luteinizing hormone on follicular stimulation and oocyte development in normal ovulatory women. Fertil Steril. 1985;43:696–702.
- Mantovani LG, Belisari A, Szucs TD. Pharmaco-economic aspects of in-vitro fertilization in Italy. Hum Reprod. 1999;14:953–958.
- Wølner-Hanssen P, Rydhstroem H. Cost-effectiveness analysis of in-vitro fertilization: estimated costs per successful pregnancy after transfer of one or two embryos. Hum Reprod. 1998;13:88–94.
- Gerris J, De Sutter P, De Neubourg D, et al. A real-life prospective health economic study of elective single embryo transfer versus two-embryo transfer in first IVF/ICSI cycles. Hum Reprod. 2004;19:917–923.
- Daya S., Ledger W., Auray J, et al. Cost-effectiveness modelling of recombinant FSH versus urinary FSH in assisted reproduction techniques in the UK. Hum Reprod. 2001;16:2563–2569.
- Briggs A., Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13:397–409.
- Sykes D, Out HR, Palmer SJ, et al. The cost-effectiveness of in vitro fertilization in the United Kingdom: a comparison of three gonadotropin treatment. Hum Reprod. 2001;16:2557–2562.
- Garceau L, Henderson J, Davis LJ, et al. Economic implications of assisted reproductive techniques: a systematic review. Hum Reprod. 2002;17:3090–3109.
- Tandulwadkar SR, Lodha PA, Mangeshikar NT. Obstetric complications in women with IVF conceived pregnancies and polycystic ovarian syndrome. J Hum Reprod Sci. 2014;7:13–18.
- National Council on Pricing and Reimbursement. Positive drug list [Internet]. Sofia: National Council on Pricing and Reimbursement; c2014 [cited 2014 Jun 15]. Available from: www.ncpr.bg.
- Drummond M, Stoddart G, Torrance G. Methods for the evaluation of health care programmes. 2nd ed. New York: Oxford University Press; 1998.
- Ghumman S. Step by step ovulation induction. 2nd ed. New Delhi: Jaypee Brothers Medical Publishers; 2014.
- Al-Inany H, Aboulghar M. Gonadotrophin-releasing hormone antagonists for assisted conception. Cochrane Database Syst Rev [Internet]. 2001 [cited 2016 Feb 25];4:CD001750. Available from: http://dx.doi.org/10.1002/14651858.CD001750.
- Al-Inany HG, Youssef MA, Aboulghar M, et al. Gonadotrophin-releasing hormone antagonists for assisted reproductive technology. Cochrane Database Syst Rev [Internet]. 2011 [cited 2015 Nov 10];5:CD001750. Available from: http://dx.doi.org/10.1002/14651858.CD001750.pub3.
- World Health Organization. Cost effectiveness and strategic planning (WHO-CHOICE) [Internet]. Geneva:World Health Organization; c2016 [cited 2015 Feb 20]. Available from: http://www.who.int/choice/costs/CER_thresholds/en/.
- Xavier P, Gamboa C, Caleo L, et al. A randomized study GnRH antagonist (cetrorelix) versus agonist (buserelin) for controlled ovarian stimulation: effect on safety and efficacy. Eur J Obstet Gynecol Reprod Biol. 2005;120:185–189.
- van Wely M, Westergaard LG, van der Veen F, et al. Effectiveness of human menopausal gonadotrophin versus recombinant follicle-stimulating hormone for controlled ovarian hyperstimulation in assisted reproductive cycles: a meta-analysis. Fertil Steril. 2003;80:1086–1093.
- van Wely M, Kwan I, Burt AL, et al. Recombinant versus urinary gonadotropin for ovarian stimulation in assisted reproductive technology cycles. Hum Reprod Update. 2012;18:111.
- Pacchiarotti A, Sbracia M, Frega A, et al. Urinary hMG (Meropur) versus recombinant FSH plus recombinant LH (Perfoveris) in IVF: a multicentre, prospective, randomized controlled trial. Fertil Steril. 2010;94:2467–2469.
- Aboulghar MA, Mansour RT, Serour GA, et al. In vitro fertilization in a spontaneous cycle: a successful simple protocol. J Obstet Gynaecol. 1995;21:337–340.
- Selman H, Pacchiarotti A, El-Danasouri I. Ovarian stimulation protocols based on follicle-stimulating hormone glycosylation pattern: impact on oocyte quality and clinical outcome. Fertil Steril. 2010;94:1782–1786.
- Mantovani L, Belisari A, Szucs T. Pharmaco-economic aspects of in vitro fertilization in Italy. Hum Reprod. 1999;14:953–958.
- Polinder S, Heijnen E, Macklon N, et al. Cost-effectiveness of a mild compared with a standard strategy for IVF: a randomized comparison using cumulative term live birth as the primary endpoint. Hum Reprod. 2014;23:316–323.