ABSTRACT
Glass carbomer cement is a new dental material developed from the traditional glass ionomer cements. It has better mechanical and chemical features when compared to the conventional glass ionomer cements. The purpose of this in silico investigation was to examine the influence of glass carbomer and composite resin materials with class I cavity design on stresses happening in the inlay. Finite-element analysis and three-dimensional modelling were used to examine the stress in the glass carbomer and hybrid composite inlays resulting from a 300-N point load on occlusal surfaces. Two different inlay materials, glass carbomer cement and hybrid composite resin, were evaluated. The maximum von Misses stress values in the composite resin inlays were significantly lower than those in the glass carbomer inlays. The results from this study showed that the resistance of the glass carbomer against the forces was higher than that of the composite resin inlays. The stresses were concentrated mostly at similar regions. The obtained results suggest that glass carbomer may be recommended as a preferred filler restorative material in teeth with much structure loss.
Introduction
Ideally, the restorative filling material should be able to replace the enamel and dentin, and also not damage the tissues in the mouth. However, a material like this does not exist yet [Citation1]. The purpose filling is to prevent the formation of caries by eliminating all microorganisms, and to ensure normal dentin formation on the pulp after removing all the demineralized dentin [Citation2]. Glass polyalkenoate or glass ionomer cements (GPCs/GICs) have made some advancement towards this goal [Citation1].
GICs have been applied in common clinical uses such as liner, base, adhesive and restorative materials [Citation3]. GICs have been defended as a restorative material on account of their chemical adhesion to tooth structures and continuous in vivo fluoride release. In addition, GICs have cariostatic and biocompatible properties [Citation4,Citation5]. Due to their antibacterial effects and remineralizing ability, conventional GICs have been well accepted in cases of high caries risk activity [Citation5,Citation6]. However, conventional GICs have drawbacks like handling and working difficulties, sensitivity to wetness and fragility [Citation7]. Consequently, a new GIC-based material has been developed, glass carbomer cement (GCC), which is claimed to have better mechanical–chemical properties. GCC is a fluor/hydroxy apatite-containing GCC with nano-sized particles [Citation8]. GCCs are significantly superior to conventional GICs in terms of mechanical–chemical properties (remineralisation effect, strength, resistance to shear, wear and acid attacks) with the application of heat with a LED curing light unit [Citation9].
Since the success of dental restorations depends on the stress and the physical and mechanical features of the materials used, restorative materials, as a rule, are evaluated under compressive loading to determine their fatigue limit [Citation10,Citation11]. As a result of continuous developments of dental materials and restorative techniques, finite-element analysis (FEA) has been widely used in many dental biomechanical studies to assess the impact of dental materials and their effect on stress distribution. FEA is accepted as an effective method to evaluate the biomechanical properties of dental restorative materials and systems. As new dental restorative materials are compared to determine their ability to withstand the masticatory forces, the results can be of significant importance in clinical practice [Citation12].
The model resulting from three-dimensional (3D) FEA analysis is divided mathematically into a number of separate subregions, or ‘elements,’ connected at separate points called ‘nodes.’ Some of these nodes have fixed displacements, and others have prescribed loads [Citation13]. A physical effect in one element which applies force or displacement is transmitted to the other elements by the nodes, allowing the determination of stress/strain values for the particular system under examination. Definition of the new term is required. The von Mises stress or equivalent tensile stress is a combination of all the stresses (normal stress in all directions, and all three shear stresses). The performance of most ductile materials such as restorative materials can be predicted using von Misses stress. In addition, this stress has to be considered when evaluating the appropriate dental material to use, as well as the hard tissue damage that may happen [Citation14]. Due to this, it is possible to detect whether or not it is likely for permanent deformation or breakage to occur in the material [Citation15].
The aim of the present study was to analyse the biomechanical performance glass carbomer and hybrid composite resin inlays, under a 300-N point load applied to the occlusal surface of the first molar. The adhesion properties and von Misses stress values in the enamel, dentin, glass carbomer and composite resin materials were simulated using 3D FEA.
Materials and methods
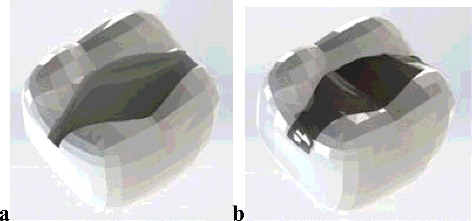
In this in silico study, stress analysis was performed on the first molar teeth, using stress analysis software (ANSYS Rel.6.0, ANSYS Inc., Houston, TX, USA). The FEA model consisted of dental restorations, enamel and dentin. The mandibular molar tooth was selected as the model based on the anatomical measurements suggested by Wheeler (see [Citation16]). A computer model of the mandibular molar was generated. An additional inlay-shaped volume, having a 3.5 mm cavity depth and 2.5 mm isthmus width, was created using the FEA software preprocessor. The cavity preparation was created by deleting the inlay volume. A tooth model with an inlay-prepared cavity with rounded corners was obtained ((a)). Inlays with a 0.1-mm bonding layer were overlapped on the models in a similar way. The inlays were bonded to the tooth structure with a bonding system.
Two restoration materials used were GCC (Glass Fill, Glass Carbomer Products, Leiden, Netherlands) and hybrid composite resin (Estenia, Kuraray Medical Inc, Tokyo, Japan). lists the elasticity modules and Poisson's ratios of enamel, dentin, GCC and hybrid composite resin [Citation17].
Table 1. Poisson ratio and elasticity modulus values of the materials used in the study.
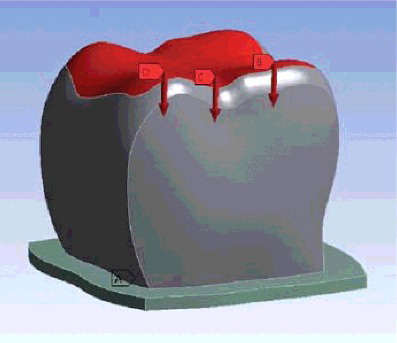
A permanent right lower first molar tooth was modelled as a three layered structure consisting of enamel, dentin and filling material. Two different materials were used as fillings for class I cavities ((b)). Different restorative materials and the hard tissues of the tooth were loaded under a force of 300 N applied vertically (). The 300-N load was spread over three areas of the tooth. In total, two models were prepared and evaluated. Maximum and minimum stresses were calculated for each model separately.
Figure 2. Vertical loading force of 250 N (a). Mesial loading of 300/3 N (b). Central loading of 300/3 N (c). Distal loading of 300/3 N (d).
The analysis was performed using an Intel Pentium D CPU 3.00 GHz processor, with a 250 GB hard disk and 3.00 GB of RAM. The computer was equipped with the Windows XP Professional operation system (version 2002 with Service Pack 3). FEA and 3D modelling were performed using a laser scanner (Next Engine, Inc., Santa Monica, CA), 3D modelling software (Rhinoceros 4.0, McNeel North America, Seattle, WA, USA) and the stress analysis software (ANSYS Rel.6.0, ANSYS Inc., Houston, TX, USA).
Results and discussion
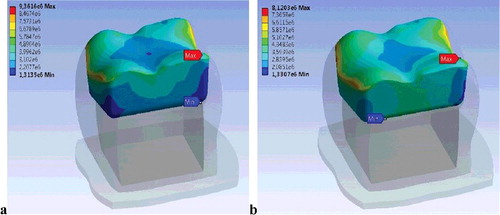
In this study, the maximum and minimum stress values for enamel, dentin and dental fillings for teeth restored with different materials were compared under vertical occlusal forces in two models. indicates the stress values in the inlay materials for GCC and hybrid composite resin. The maximum von Mises stress value in the GCC inlay was determined to be 9361 MPa and that in the hybrid composite inlay, 8120 MPa (). Also, the locations of maximum von Mises stress values for both inlay materials were determined on similar areas. This indicates that the structure of GCC inlays is more resistant to hybrid composite inlays. Due to the fact that the values obtained by FEA are variances that occur as a result of non-mathematical calculations, careful review and analysis of the stress distributions were carried out instead of performing statistical analysis.
Table 2. Maximum and minimum von Misses stress values after force application (MPa).
GCC was developed within the last few years as a new glass-ionomer-based restorative material, similar to the clinical application of GIC. The manufacturer claims that GCC leads to superior product characteristics owing to the specially developed additives, including nano-fluoride-/hydroxyapatite particles, which provide extremely low solubility, superior flexural strength, compression strength and high durability [Citation3,Citation9,Citation18].
GCC may be used as an alternative fissure sealant material in children; particularly in children with incompletely erupted teeth and where wetness control is not easy [Citation19]. Following one-year clinical evaluation, GCC showed a similar maintenance rate when compared with a resin-based material [Citation20]. This study showed that the GCC structure shows the same strength as hybrid composite inlays. In addition, GCC is resistant to moisture and easy to implement.
Atraumatic restorative treatment for cavities restored with the newly developed GCC was not significantly more fracture resistant than comparable restorations that use the conventional glass ionomer Fuji IX [Citation21]. In addition, GCC, with fluor/hydroxyapatite protects against secondary caries in teeth [Citation8]. Besides these advantages, this study demonstrated the resistance of GCC compared to composite. As a result of the FEA, it was determined that GCC is more resistant to chewing forces than hybrid composites.
The present use of composite resin restorative materials has revealed that they have toxic and local immunological effects. During the polymerization process, composite resins shrink by about 2%–5% by volume [Citation22]. This may cause gap formation between the restorative material and the wall of the tooth cavity [Citation23,Citation24], allowing penetration of bacteria and bacterial toxins through the dentin towards the dental pulp. This can lead to inflammatory reactions. It can cause pulpal necrosis and subsequently apical periodontitis [Citation25]. In GCC restoration, shrinkage does not occur during the polymerization process.
Direct composite restorations (DCRs) are made in one treatment session with little cost. However, DCR can have polymerization shrinkage if the mass to be polymerized is large (layer thickness above about 2 mm). Polymerization shrinkage may lead to significant marginal defects and fracture of restorations. However, indirect composite restorations (ICRs), such as composite resin inlays or onlays, have shown reduced polymerization shrinkage and higher resistance to wear than DCR, especially in occlusal contact areas [Citation26–29]. The improved properties of ICR are associated with a higher degree of conversion obtained by the use of different polymerization procedures that involve activation by heat between 90 and 140 °C and/or vacuum or nitrogen atmosphere [Citation30]. In addition, ICR shows less bacterial adhesion than DCR [Citation23].
In clinical situations, it is extremely difficult to calculate stresses generated within and around the restorative material. Therefore, stress analysis using FEA is often regarded as an ideal approach to evaluate stresses in the restorations under simulated clinical conditions [Citation15,Citation31]. The stress between the restorative material and the tooth structure was also analysed using FEA in this study.
The modulus of elasticity describes the relative rigidity of the solid materials within their elastic limit; in other words, it is a measure of the ability of a material to resist changes in length when under lengthwise tension or compression. The modulus of elasticity determines the suitability of materials. The use of low-modulus restorative materials in dentistry has been shown to facilitate stress distribution. Thus, integrity of structure for the tooth and the restoration is provided [Citation31,Citation32]. In this study, it was thought that GCC is resistant to stress resulting from chewing force.
Barone et al. [Citation33] investigated the clinical performance of composite inlays over a three-year period. They found that composite inlays had a very high success rate (97.4%). Another clinical study examined the clinical performance of 108 direct and indirect resin composite inlays over a five-year period. Under controlled clinical conditions, indirect composite resin inlays and direct composite resin restorations exhibited an annual failure rate of 2.5% and 1.6%, respectively, after five years [Citation34]. Mendonça et al. [Citation35] compared the direct and indirect composite inlay techniques and observed little difference in the clinical performance of direct and indirect composite inlays in posterior teeth after one year.
Indirect composite inlays have better physical properties such as easier polishing, water resistance, rigidity, control of proximal contours, marginal adaptation and polymerization shrinkage. In contrast, direct composite inlays require one appointment. It is not necessary to use impression materials and dies. They have lesser technique sensitivity, require less time to place and are cheaper compared to indirect restorations. These advantages are more useful on paediatric patients [Citation33,Citation35]. This study used an indirect composite inlay material because of its advantages. In addition, GCC is useful in paediatric patients due to the fact that it has less technique sensitivity and takes less time and effort to place in the dental cavity.
Menne-Happ and Ilie [Citation9] report that heat treatment and gloss application do not influence the mechanical properties of GCP. Subramaniam et al. [Citation19] are of the opinion that glass carbomer is less soluble than a conventional glass ionomer at different pH values. Chen et al. [Citation8] studied the performance of glass carbomer in a randomized controlled trial and reported that more dentin carious lesions were observed in the glass carbomer sealant group than in other groups [Citation8]. In a clinical trial, Gorseta et al. [Citation20] observed that glass carbomer displayed a comparable retention to composite resin after 12 months. Glass carbomer is considered healthy for children, as it contains fluorhydroxyapatite but does not contain bisphenol-A [Citation20,Citation36]. This accumulating evidence strongly suggests that glass carbomer will be a preferred restorative material in the future.
Conclusions
Within the limitations of this study, glass carbomer could be suggested as the more preferable inlay restoration material because its structure holds the stress inside, i.e. less stress is transferred through the tooth structure. The glass carbomer inlay was shown to be especially applicable when the supportive tooth structure is weak. However, these in silico findings should be tested over a longer period in vivo.
Acknowledgments
The authors thank Dr Emre Ari (Dicle University, Department of Mechanical Engineering) for his helpful advice on FEA.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Zainuddin N, Karpukhina N, Law RV, et al. Characterisation of a remineralising glass carbomer® ionomer cement by MAS-NMR spectroscopy. Dent Mater. 2012;28(10):1051–1058.
- Ngo HC, Mount G, Mc Intyre J, et al. Chemical exchange between glass-ionomer restorations and residual carious dentine in permanent molars: an in vivo study. J Dent. 2006;34(8):608–613.
- Gorseta K, Borzabadi-Farahani A, Moshaverinia A, et al. Effect of different thermo-light polymerization on flexural strength of two glass ionomer cements and a glass carbomer cement. J Prosthet Dent. 2017;118(1):102–107.
- Kotsanos N1, Topitsoglou V, Tatsi C, et al. The early fluoride release pattern of an aged glass ionomer treated with fluoride. Eur J Prosthodont Restor Dent. 2007;15:135–141.
- Davidovich E, Weiss E, Fuks AB, et al. Surface antibacterial properties of glass ionomer cements used in atraumatic restorative treatment. J Am Dent Assoc. 2007;138:1347–1352.
- Rutar J, McAllan L, Tyas MJ. Three-year clinical performance of glass ionomer cement in primary molars. Int J Paediatr Dent. 2002;12:146–147.
- Dionysopoulos P, Kotsanos N, Pataridou A. Fluoride release and uptake by four new fluoride releasing restorative materials. J Oral Rehabil. 2003;30:866–872.
- Chen X, Du MQ, Fan MW, et al. Caries-preventive effect of sealants produced with altered glass-ionomer materials, after 2 years. Dent Mater. 2012;28:554–560.
- Menne-Happ U, Ilie N. Effect of gloss and heat on the mechanical behaviour of a glass carbomer cement. J Dent. 2013;41(3):223–230.
- Shor A, Nicholls JI, Phillips KM, et al. Fatigue load of teeth restored with bonded direct composite and indirect ceramic inlays in MOD class II cavity preparations. Int J Prosthodont. 2003;16:64–69.
- Ausiello P, Rengo S, Davidson CL, et al. Stress distributions in adhesively cemented ceramic and resin-composite Class II inlay restorations: a 3D-FEA study. Dent Mater. 2004;20:862–872.
- Yamanel K, Caglar A, Gülsahi K, et al. Effects of different ceramic and composite materials on stress distribution in inlay and onlay cavities: 3-D finite element analysis. Dent Mater J. 2009;28(6):661–670.
- Roylance D. Finite Element Analysis. Cambridge, MA: Massachusetts Institute of Technology; 2001. Available from: https://ocw.mit.edu/courses/materials-science-and-engineering/3-11-mechanics-of-materials-fall-1999/modules/MIT3_11F99_fea.pdf
- Guven S, Akdogan M, Oz C, et al. Three-dimensional finite-element analysis of two ceramic inlay restorations with different cavity designs. Biotechnol Biotechnol Equip. 2015;29(3):579–585.
- Bahrami B, Shahrbaf S, Mirzakouchaki B, et al. Effect of surface treatment on stress distribution in immediately loaded dental implants – a 3D finite element analysis. Dent Mater. 2014;30(4):89–97.
- Ash MM, Nelson N. Wheeler's dental anatomy, physiology, and occlusion. 8th ed. Philadelphia (PA): Saunders; 2002. p. 297–306.
- Yokoyama D, Shinya A, Gomi H, et al. Effects of mechanical properties of adhesive resin cements on stress distribution in fiber-reinforced composite adhesive fixed partial dentures. Dent Mater J. 2012;31(2):189–196.
- Goldman AS, Chen X, Fan M, et al. Cost-effectiveness, in a randomized trial, of glass-ionomer-based and resin sealant materials after 4 yr. Eur J Oral Sci. 2016;124:472–479.
- Subramaniam P, Girish BKL, Jayasurya S. Evaluation of solubility and microleakage of glass carbomer sealant. J Clin Pediatr Dent. 2015;39(5):429–434.
- Gorseta K, Glavina D, Borzabadi-Farahani A, et al. One year clinical evaluation of a glass carbomer fissure sealant: a preliminary study. Eur J Prosthodont Restor Dent. 2014;22(2):67–71.
- Koenraads H, Van der Kroon G, Frencken JE. Compressive strength of two newly developed glass ionomer materials for use with the atraumatic restorative treatment (ART) approach in class II cavities. Dent Mater. 2009;25(4):551–556.
- Kleverlaan CJ, Feilzer AJ. Polymerization shrinkage and contraction stress of dental resin composites. Dent Mater. 2005;21(12):1150–1157.
- Derchi G, Vano M, Barone A, et al. Bacterial adhesion on direct and indirect dental restorative composite resins: an in vitro study on a natural biofilm. J Prosthet Dent. 2017;117(5):669–676.
- Lopes GC, Baratieri LN, Monteiro S Jr, et al. Effect of posterior resin composite placement technique on the resin-dentin interface formed in vivo. Quintessence Int. 2004;35:156–161.
- Dawson VS, Amjad S, Fransson H. Endodontic complications in teeth with vital pulps restored with composite resins: a systematic review. Int Endod J. 2015;48:627–638.
- Scheibenbogen-Fuchsbrunner A, Manhart J, Kremers L, et al. Two-year clinical evaluation of direct and indirect composite restorations in posterior teeth. J Prosthet Dent 1999;82:391–397.
- Alvanforoush N, Palamara J, Wong RH, et al. A Comparison between published clinical success of direct resin composite restorations in vital posterior teeth in 1995–2005 and 2006–2016 periods. Aust Dent J. 2017;62(2):132–145.
- Van Dijken JWV. Direct resin composite inlays/onlays: an 11 year follow-up. J Dent. 2000;28:299–306.
- Barabanti N, Preti A, Vano M, et al. Indirect composite restorations luted with two different procedures: a ten years follow up clinical trial. J Clin Exp Dent. 2015;7(1):54–59.
- Tezvergil-Mutluay A, Lassila LVJ, Vallittu PK. Degree of conversion of dual cure luting resins light-polymerized through various materials. Acta Odontol Scand. 2007;65:201–215.
- Dauvillier BS. Visco-elastic parameters of dental restorative materials during setting. J Dent Res. 2000;79:818–823.
- Srirekha A, Bashetty K. A comparative analysis of restorative materials used in abfraction lesions in tooth with and without occlusal restoration: three-dimensional finite element analysis. J Conserv Dent. 2013;16(2):157–161.
- Barone A, Derchi G, Rossi A, et al. Longitudinal clinical evaluation of bonded composite inlays: a 3-year study. Quintessence Int. 2008;39(1):65–71.
- Cetin AR, Unlu N, Cobanoglu N. A five-year clinical evaluation of direct nanofilled and indirect composite resin restorations in posterior teeth. Oper Dent. 2013;38(2):31–41.
- Mendonça JS, Neto RG, Santiago SL, et al. Direct resin composite restorations versus indirect composite inlays: one-year results. J Contemp Dent Pract. 2010;11(3):25–32.
- Eng DS, Lee JM, Gebremariam A, et al. Bisphenol A and chronic disease risk factors in US children. Pediatrics. 2013;132(3):637–645.