ABSTRACT
Achievement of optimal glycaemic control in children and adolescents with type 1 diabetes depends on the knowledge of the patients and their parents about the control of the disease and the family support. The aim of this study was to investigate the importance of the social standard of the families determined by the employment of the parents and their educational qualification on the control of diabetes. Two consecutive national multi-centre cross-sectional studies of patients with type 1 diabetes, aged 0–19 years, for HbA1c were conducted in 2012 and in 2014. The first study included 829 patients (422 boys, 407 girls), and the second - 498 patients; 281 patients participated in both studies. The patients whose parents are with primary education showed the highest level of HbA1c in both studies: 9.73% ± 2.38% and 9.27% ± 1.54% in the first, and the second study, respectively. The patients whose parents have university education achieved the best control: HbA1c is 8.45% ± 1.76% and 7.84% ± 1.24%, respectively. The cohorts of diabetic patients whose parents have secondary (p = 0.035) and university education (p < 0.001) showed significant reduction of HbA1c in the second study compared to the first one. The patients in families with unemployed parents or families in which only the mother is employed showed the highest levels of HbA1c. Our results underline the importance of the educational qualification and the social standard of the family for the proper control of this chronic disease.
Introduction
Type 1 diabetes mellitus is one of the most common endocrine diseases of childhood and adolescence caused by insulin deficiency. This chronic disease requires intensive and challenging self-management. This includes multiple insulin injections daily, frequent and accurate monitoring of blood glucose, and adjustment of the insulin dose to the carbohydrate intake and/or physical activity [Citation1–3]. The regular investigation of HbA1c with a standardized method and the analysis of the factors influencing the control of diabetes are important steps for its improvement [Citation4,Citation5]. The long-term maintenance of optimal glycaemic control (HbA1 < 7.5%) is obligatory for prevention of the chronic diabetic complications [Citation6,Citation7]. Achievement of the desired glycaemic control during childhood depends to a large extent on the family support and the parents’ knowledge about the management and control of diabetes [Citation8,Citation9]. Interaction between the parents and their children is generally agreed to be a major factor in the glycaemic management [Citation10,Citation11].
The role of the social factors that hinder the achievement of optimal glycaemic control has been investigated and discussed [Citation8]. Social determinants/issues have been defined as factors in the social environment. These include: socioeconomic status, housing and transportation, accessibility of health care resources, social support, education, unemployment, job security and disability [Citation9]. These factors would appear to be obvious determinants of health. The reports of the relationship between glycaemic control and social determinants are controversial, but most researchers identify association between them [Citation10,Citation12].
The aim of our study was to investigate the importance of the social standard of the families determined by the employment of the parents and their educational qualification on the control of diabetes.
Materials and methods
Study design
Two consecutive national multi-centre cross-sectional studies of glycated haemoglobin (HbA1c) in patients with type 1 diabetes mellitus aged 0–19 years were conducted in 2012 (1 February 2012–30 August 2012) and 2014 (15 January 2014–15 September 2014) in 11 paediatric endocrine practices in Bulgaria. The two studies included all the patients who visited the offices of their paediatric endocrinologist for the above-mentioned defined periods and agreed to participate. An exclusion criterion was disease duration of less than three months.
A special self-report questionnaire was filled in by the families, including data about the educational qualification of the parents and employment as well as the age of diagnosis of diabetes, insulin regimen, dosages of bolus and basal insulin and the type of insulin preparations used.
A special web page was developed for the project. The data concerning the patients and their parents (age, sex, employment and education of the parents) were coded and entered by the physicians. The educational qualification was defined as follows: 1 – primary or lower; 2 – secondary; 3 – university. For the definition of employment, the parents were divided into the following four groups: 1 – both parents work; 2 – only the father works; 3 – only the mother works; 4 – both parents are unemployed.
Cohort of patients
The first study, included 829 patients (422 boys and 407 girls), aged 11.9 ± 4.2 years, and the second study, 498 ones (261 boys and 237 girls), aged 11.6 years ± 4.1 years; 281 patients participated in both studies. The cohort of patients included in the two studies represents about 60% of children and adolescents with type 1 diabetes mellitus aged 0–19 years in Bulgaria.
There are several reasons for the incomplete overlap of the cohort of patients included in the two studies. First, during the period of two years, there were some newly diagnosed patients. Second, some patients left the cohort because they reached the age of 19 years and were no longer monitored by the paediatric endocrinologists or because their families emigrated in the period between the two studies. Third, some of the outpatient offices in the countryside rural areas included a smaller number of patients in the second survey, due to organizational issues (difficulties in the distribution of the kits and timely delivery of samples).
Educational training for parents
Between the first and the second study, additional structured training was conducted for the patients, their families and medical staff in different regions of the country with regard to the control of the disease: insulin therapy, diet, carbohydrate counting and meal boluses, the use of a correction factor for hyperglycaemia, treatment of hypoglycaemia, acute and chronic complications of diabetes.
HbA1c examination
The examination of HbA1c was performed in a certified Central Laboratory using a standardized high-performance liquid chromatography (HPLC) method (Bio-Rad). A single capillary blood sample was taken in the offices of endocrinologists, coded and stored according to the requirements and shipped weekly to the Central Laboratory. The results for HbA1c were entered by the lab technician in the study web-page. Every participating physician had access to the results of his/her patients only.
Ethics approval
The study was approved by the Ethics Committee of the Medical University of Sofia, Bulgaria in 2011. Informed consent was obtained from the parents or legal guardians of children, according to the local regulations.
Statistical analysis
The results were entered and processed with statistical package SPSS for Windows, Version 16.0. Differences were considered to be statistically significant at p < 0.05. Descriptive statistics was used for presentation of data by summarizing statistical characteristics: average values, standard deviations (±SD), minimum and maximum values and more. Chi-square test or Fisher's exact test were applied for verification of the hypothesis of a link between two categorical variables. The non-parametric test of Kolmogorov–Smirnov was applied for checking the distribution of the statistical sample for normality. Differences in the mean values between groups were analysed using Student's t-test and Mann–Whitney U test.
Results and discussion
Descriptive statistics
There was no significant difference in the duration of diabetes between the two consecutive studies: 4.32 ± 3.54 years for the first study and 4.52 ± 3.38 years for the second one (p = 0.089). The distribution of the participants in the two studies ( and ) did not differ by gender (p = 0.595) and age (p = 0.258).
Table 1. Gender distribution of participants in the two studies.
Table 2. Average age of the girls and the boys in total in the two studies.
This is the first study in Bulgaria to analyse the influence of some social factors on the level of HbA1c among patients with type 1 diabetes aged 0–19 years. After the first evaluation in 2012, in which the HbA1c median level of 8.93% ± 1.98% was found rather unsatisfying, additional training for the patients and their parents was conducted the following years. In 2014, we performed a second study and found a significantly lower level of HbA1c (8.42% ± 1.69%) compared to that in 2012 (p < 0.001) [Citation13]. Below, we analyse and discuss the impact of some of the examined social factors on the glycaemic control in children and adolescents with type 1 of diabetes mellitus.
Impact of parents’ education
In both studies, we collected information about the educational qualification of the mothers and the fathers of the patients. The percentage of parents with primary, secondary or university education is shown in and ). In the subsequent analyses, if there was a difference in the educational level of the parents, we chose the education of the mother as an indicator of the educational qualification in the family. The results showed that there were no significant differences in the distribution of the fathers across the three levels of education between the two studies ().
Table 3. Distribution of the fathers according to their educational level.
Table 4. Distribution of the mothers according to their educational level.
The analysis of the mothers’ level of education showed that there were significantly more mothers with primary education in the first study (p = 0.015) compared to the second one (). The percentage of mothers with university education was significantly higher in the second study than in the first one (). A reason for this could be the fact that part of the patients from the rural part of the country – an area with an overall lower level of education among the general population – were not able to participate in the second study due to technical/logistic obstacles mentioned above. Another explanation might be unwillingness of some families to participate specifically in the second study; however, it is unfortunately not possible to collect evidence for this particular hypothesis. Additionally, there are new patients in the second study, which may also account for the differences in the family educational status between the cohorts in the two studies.
The analysis of the dependence of the control of diabetes and the educational qualification of the parents showed that the children of parents with a lower educational level had the highest level of HbA1c in both studies (). In the first study, the children of parents with elementary education or lower, showed a mean HbA1c level of 9.73% ± 2.38%, which is significantly higher than that of the patients whose parents have secondary (9.07% ± 1.92%; 75.60 ± 20.99 mmol/mol; p = 0.002) or university education (8.45% ± 1.76%; 69.0 ± 19.3 mmol/mol; p < 0.001). The patients from families with secondary education had significant (p = 0.035) reduction of HbA1c in the second study, down to 8.77% ± 1.9% (72.45 ± 20.77 mmol/mol). The children of parents with university degrees achieved the best control in both studies: in the first study, their mean HbA1c level was 8.45% ± 1.76% (69.0 ± 19.30 mmol/mol) and in the second one, 7.84% ± 1.24% (62.19 ± 13.69 mmol/mol).
Figure 1. Comparison between the mean level of HbA1c among the children and adolescents with type 1 diabetes according to the educational level of their parents (indicator is the mother's qualification) in both studies.
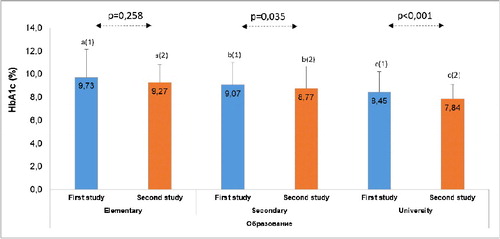
The children of parents with secondary and university education showed statistically significant reduction of the HbA1c levels in the second study compared to the first one (). The level of HbA1c was not significantly reduced in the children whose parents have elementary education.
One explanation for these results is that the additional education helped for the significant improvement in the glycaemic control for patients whose parents have a higher level of education, secondary and university. Better results may also be due to the fact that, in the second study, the cohort of patients included more mothers with university education. In Bulgaria, the mother traditionally plays a major role in the treatment of diabetes and adherence to the dietary regime of the children. Other authors have also reported that the children of mothers with higher education and experience are able to achieve better glycaemic control [Citation14,Citation15]. Conversely, Gallegos-Macias et al. [Citation16] found that a lower family socioeconomic status, but not the educational attainment of parents, was associated with significantly higher HbA1c levels, regardless of ethnicity.
The entry of new technologies in the life of our patients for monitoring and treatment of diabetes, such as insulin pumps and sensors, helped a lot for achievement of glycaemic control [Citation17–19]. Currently, diabetes management requires good knowledge and more resources that highly educated people are more likely to be in possession of. Diabetes teams therefore face challenges in fitting treatment plans for every family. Diabetes affects all strata of society, and support and interventions need to be adjusted for the inherent factors related to the families’ psychosocial and socio-demographic background [Citation8].
Impact of the social status of parents determined by their employment
The parents were equally distributed among the four groups according to their employment in both studies (). The patients in families with both unemployed parents as well as in those in which only the mother is employed, had the highest levels of HbA1c in the two studies (), respectively, for the first study: 10.28% ± 2.99% (89.13 ± 32.65 mmol/mol) and 9.45% ± 1.99% (79.8 ± 21.78 mmol/mol), and for the second one – 9.19% ± 1.39% (76.9 ± 14.74 mmol/mol) and 9.82% ± 1.97% (83.79 ± 21.57 mmol/mol).
Table 5. Distribution of parents according to their social status in both studies.
Figure 2. Comparison of the mean HbA1c in the two consecutive studies among the groups of patients according to the social status of their parents.
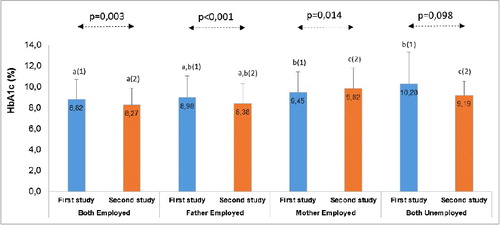
Children and adolescents with diabetes from families in which both parents are employed achieved the best control in both studies (). The mean HbA1c level in the first study was 8.82% ± 1.88% (72.98 ± 20.53 mmol/mol), whereas, in the second one, it was significantly reduced to 8.27% ± 1.59% (66.97 ± 17.40 mmol/mol), (p = 0.003).
The second study showed reduction in the level of HbA1c (), with the exception of the families with both unemployed parents and those with the mothers employed only. The patients with both parents or only the father employed showed the lowest level of HbA1c. There was no significant difference between the level of HbA1c, respectively – 8.82% ± 1.88% (72.98 ± 20.53 mmol/mol) and 8.98% ± 2.07% (75.93 ± 20.59 mmol/mol) for the first study. There was relevant reduction in the mean HbA1c in the second study: HbA1c decreased to 8.27% ± 1.59% (66.97 ± 17.40 mmol/mol; p = 0.003) and 8.38% ± 1.88% (68.0 ± 20.59 mmol/mol; p < 0.001), respectively, for the patients with both employed parents and with fathers employed only ().
In accordance with other reports [Citation14,Citation16,Citation20,Citation21], we found that the patients in families with low family income (unemployed parents) have the highest levels of HbA1c. The poor financial capacity of the families leads to restrictions on the number of blood glucose measurements and to inability to provide proper nutrition. Many studies have demonstrated that more frequent monitoring of blood glucose leads to better glycaemic control [Citation1,Citation8]. In our second study, when both parents are employed or only the father is, the patients showed significantly lower HbA1c levels compared to the first study. We may speculate that this is a result of both the ability for these families to buy more tests for blood glucose monitoring, in addition to those provided by the health insurance system, as well as the advantage from the additional training.
Another research discusses the possibility that African American children in particular suffer from poorer metabolic control due to lower family income, which precludes the purchase of proper health insurance and care [Citation22]. In addition, the authors suggest that there may be modifiable parameters within specific racial groups that predict glycaemic control. In Bulgaria, this is not likely the case, as the health insurance covers 1100 tests for blood glucose annually for any patient under the age of 18 years. The same goes for the insulin preparations, which are prescribed monthly by the general practitioner free of charge.
Other authors, however, do not find significant association between glycaemic control and the parents’ employment status or marital status [Citation14]. On the other hand, the Hvidore Study Group on Childhood Diabetes demonstrated a positive association between parents’ experience of well-being and glycaemic control among children with diabetes [Citation23]. Psychosocial issues appear to be common among diabetic patients worldwide and they affect diabetes self-care [Citation20]. For example, many patients have poor psychological well-being and a few ones report receiving psychological treatment [Citation20]. Therefore, professional and prompt psychological support can motivate families to achieve better results in terms of glycaemic control. It is clear that the psychosocial support for young people with diabetes must be not only continuous, but also age-appropriate as they move through the transition from childhood to adolescence [Citation24].
The Hvidore Study Group, in another large study involving 2062 adolescents and 1994 parents, found that family demographic factors associated with metabolic outcomes include: parents living together, paternal employment status, parents perceived to be over-involved in diabetes care and adolescent–parent disagreement on responsibility for diabetes care practices [Citation25]. Sullivan-Bolyai et al. [Citation15] described how social support enhances mothers’ abilities to cope with the demanding daily treatment tasks related to diabetes treatment in a child. Unfortunately, in Bulgaria, only families living in big cities may rely on optimal psychological support. Therefore, only the combined efforts and care of the family for the diabetic child and those of the diabetic team (including a psychologist and a social worker) can lead to improved control and prognosis of the disease [Citation26–29].
Conclusions
This study provides evidence for the impact of some social factors on the glycaemic control among Bulgarian children and adolescents with type 1 diabetes by analysis of the level of HbA1c. Achieving and maintaining optimal control of diabetes is mostly difficult in children and adolescents from families with low educational and social status. Our results underline the importance of the educational qualification and the social standard of the family for the proper control of this chronic disease. Further research is needed with a larger number of patients and better organization in more distant centres. Continuous education, adequate and on-time psychological and social support for the patients from economically disadvantaged families could improve the metabolic control and outcome of diabetes.
Acknowledgements
We thank the families for their participation.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Rewers MJ, Pillay K, de Beaufort C, et al. Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes. 2014;15(Suppl. 20):102–114.
- Enander R, Gundevall C, Stromgren A, et al. Carbohydrate counting with a bolus calculator improves post-prandial blood glucose levels in children and adolescents with type 1 diabetes using insulin pumps. Pediatr Diabetes. 2012;13:545–551.
- Cameron FJ, de Beaufort C, Anstoot H-J, et al. Lessons from the Hvidoere International Study Group on childhood diabetes: be dogmatic about outcome and flexible in approach. Pediatr Diabetes. 2013;14:473–480.
- Hoelzel W, Miedema K. Report of the ADA/EAS/IDF Working Group of the HbA1c Assay, London, UK. Diabetologia. 2014;47:R53–R54.
- Weykamp C. HbA: a review of analytical and clinical aspects. Ann Lab Med. 2013;33(6):393–400.
- Steffes MW, Chavers BM, Molitch ME, et al. Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the Epidemiology of Diabetes Interventions and Complications (EDIC) study. JAMA. 2003;290(16):2159–2167.
- Donaghue K, Fung A, Hing S, et al. The effect of prepubertal diabetes duration on diabetes. Microvascular complications in early and late adolescence. Diabetes Care. 1997;20(1):77–80.
- Akhtar K, Turnbull T, Simmons D. Influences of social issues on type 1 diabetes self-management: are we doing enough? Pract. Diabetes. 2016;33(9):307–312.
- Mikkonen J, Raphael D. Social determinants of health: the Canadian facts. Toronto: York University School of Health Policy and Management; 2010.
- Zysberg L, Lang T. Supporting parents of children with type 1 diabetes mellitus: a literature review. Patient Intel. 2015;7:21–31.
- Smith L, Kugler B, Lewin A, et al. Executive functioning, parenting stress, and family factors as predictors of diabetes management in pediatric patients with type 1 diabetes using intensive regimens. Child Health Care. 2014;43(3):234–252.
- Hassan K, Robert Loar R, Anderson B, et al. The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. J Pediatr. 2006;149(4):526–531.
- Archinkova M, Konstantinova M, Savova R, et al. Glycemic control in type 1 diabetes mellitus among Bulgarian children and adolescents: the results from the first and the second national examination of HbA1c. Biotechnol Biotechnol Equip. 2017;31(6):1198–1203.
- Haugstvedt A, Wentzel-Larsen T, Rokne B, et al. Psychosocial family factors and glycemic control among children aged 1–15 years with type 1 diabetes: a population-based survey. BMC Pediatr. 2011 [cited 2017 Apr 27];11:118. DOI:10.1186/1471-2431-11-118
- Sullivan-Bolyai S, Deatrick J, Gruppuso P, et al. Mothers' experiences raising young children with type 1 diabetes. J Spec Pediatr Nurs. 2002;7:93–103.
- Gallegos-Macias A, Macias R, Kaufman E, et al. Relationship between glycemic control, ethnicity and socioeconomic status in Hispanic and white non-Hispanic youths with type 1 diabetes mellitus. Pediatr Diabetes. 2003;4(1):19–23.
- Battelino T, Longet I, Olsen B, et al. The use and efficacy of continuous glucose monitoring in type 1 diabetes treated with insulin pump therapy: a randomized controlled trial. Diabetologia. 2012;55(12):3155–3162.
- Sherr J, Hermann J, Campbell F, et al. Use of insulin pump therapy in children and adolescents with type 1 diabetes and its impact on metabolic control: comparison of results from three large, transatlantic paediatric registries. Diabetologia. 2016;59:87–91.
- Phillip M, Danne T, Battelino T, et al. Use of insulin pump therapy in the pediatric age-group. consensus statement from the ESPE, the LWPES and ISPAD, endorsed by ADA and EASD. Diabetes Care. 2007;30:1653–1662.
- Peyrot M, Rubin R, Lauritzen T, et al. Psychosocial problems and barriers to improved diabetes management: results of the cross-national diabetes attitudes, wishes and needs (DAWN) study. Diabet Med. 2005;22(10):1379–1385.
- Hatherly K, Smith L, Overland J, et al. Glycemic control and type 1 diabetes: the differential impact of model of care and income. Pediatr Diabetes. 2011;12:115–119.
- Willi S, Miller K, DiMeglio L, et al. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135:424–434.
- Hoey H. Psychosocial factors are associated with metabolic control in adolescents: research from the Hvidøre Study Group on childhood diabetes. Pediatr Diabetes. 2009;10(Suppl. 13):9–14.
- Anderson B. Psychosocial care for young people with diabetes. Pediatr Diabetes. 2009;10(Suppl. 13):3–8.
- Cameron F, Skinner T, de Beaufort C, et al. Hvidore Study Group on Childhood Diabetes. Are family factors universally related to metabolic outcomes in adolescents with Type 1 diabetes? Diabetes Med. 2008;25(4):463–468.
- Simmons D, Hartnell S, Watts J, et al. Effectiveness of a multidisciplinary team approach to the prevention of readmission from acute glycaemic events. Diabetes Med. 2015;32:1361–1367.
- Jack L, Jack N, Hayes S. Social determinants of health in minority populations: a call for multidisciplinary approaches to eliminate diabetes-related health disparities. Diabetes Spect. 2012;25(1):9–13.
- American Diabetes Association. Promoting health and reducing disparities in populations. Diabetes Care. 2017;40(Suppl. 1):S6–S10.
- Wrosch C, Scheier M. Personality and quality of life: the importance of optimism and goal adjustment. Qual Life Res. 2003;12(Suppl. 1):59–72.
