Abstract
The treatment of choice for distal femur malignancies in skeletally immature patients remains controversial. As the mainstream treatment, limb-salvage treatment has been recently investigated, but its application in children remains challenging. Specifically, the procedure causes potential limb-length discrepancy from the continued normal growth of the contralateral lower extremity. We designed a new type of noninvasive prosthesis that is extendable within the body. To evaluate our prosthesis’ reliability and extensibility, in vitro and in vivo (animal) experiments were conducted. The in vitro experiment was used to verify the lengthening performance of the prosthesis. In the in vivo experiment, to determine the extension length and internal structure condition, the prosthesis was implanted into the rear femoral limb of a sheep under fluoroscopic guidance. Expansion was achieved with the aid of an external electromagnetic field, and the experiments proved the extensibility and noninvasiveness of our prosthesis. However, many problems need to be resolved.
Introduction
Osteosarcoma is one of the most common bone malignant tumors, and it affects the bone and soft tissues that can produce bone and bone type mesenchymal cells. Due to its pathological characteristics, osteosarcoma eventually results in tissue sarcoma and the tumor osteogenesis phenomenon [Citation1]. According to previous research, typical osteosarcoma accounts for 0.2% of all tumors, and its annual incidence is approximately 3% per million people [Citation2]. In primary malignant bone tumors, the incidence of distal femur and proximal tibia osteosarcoma is the highest, and these osteosarcoma types most frequently occur in adolescents and children [Citation3]. People with these osteosarcoma types are prone to lung metastasis, which results in the deterioration of the whole body, leading to a high fatality rate. A previous study reported that approximately 80% of osteosarcoma occurs in the limbs, particularly in the distal femur, proximal tibia and proximal humerus [Citation4]. With the development of limb-salvage technology—in addition to neoadjuvant chemotherapy—patients with osteosarcoma no longer have to undergo amputation, and their limbs can be salvaged. Survival rates have also significantly improved. Furthermore, a previous study discovered that skeletal sarcomas rarely invade the nerves and vasculature directly. Thus, excision surgery only included the involved bone and adjacent affected muscle, leaving a neurovascular-intact limb that can be reconstructed in several ways [Citation5].
Limb salvage is now regarded as the mainstream of limb osteosarcoma surgical treatment. In principle, the same patient survival rate can be obtained for amputation and limb salvage. A study found that limb-salvage surgery combined with preoperative and postoperative chemotherapy can cure 60%–70% of the patients with osteosarcoma. The overall limb-salvage rate was above 90%, and approximately 78% of patients recovered well after operation [Citation6]. In children, malignant bone tumors cover a large proportion of the bone and often occur in the long bones or (at or near) the joints (typically of the shoulder, hip and knee)[Citation7]. Removal of the tumor often requires removal of some portion of the joint or the entire joint. Unfortunately, resection often includes the epiphysis. Thus, the continuation of normal contralateral limb growth may lead topotentially significant limb-length discrepancy. The unequal length of limbs not only considerably affects gait and function but also might cause pelvic tilt, scoliosis and joint damage due to abnormal stress and other complications [Citation4]. Once developed, an extendable prosthesis is a possible solution to this problem. Its functions include provision of strong support to the limb and limb extension so that the shorter limb’s growth keeps pace with the growth of the healthy counterpart. Thus, many designs have been proposed for prostheses that can be easily expanded either without surgery or through a minor surgical procedure [Citation8].
Most of these designs either have mechanical disadvantages or require major surgery for the lengthening procedure. Combination prosthesis (e.g. modular endoprosthesis) is one of the earliest types of extendable prosthesis and has been replacing longer prosthetic components for achieving limb extension [Citation9]. However, such prostheses require major trauma surgery and results in limited limb growth in addition to other complications. Subsequent research of structurally different microtrauma prostheses has also only focused on structural design rather than component replacement. The flaws in these prosthesis designs have caused a higher incidence of postoperative complication due to the need for second replacement extension surgery.
Complications from repeated operation can be avoided by implanting a noninvasive extendable prosthesis. This prosthesis’ working principle is supported by two primary (internal and external) mechanisms. The internal power pushes an internal component for the extension effect, and the external power is an external resource that provides energy to the internal components. The prosthesis is composed of a compressed cobalt–chromium spring inside a titanium tube; the compression of the spring is maintained by a polyethylene locking mechanism (). The cobalt–chromium spring stores energy from the compression and is insulated by a ceramic ring. One tube is connected to the stem of the implant, and the second tube constitutes the hinge component of the hinge prosthesis. The uninvolved side of the joint is minimally resurfaced with a press-fit stem to preserve the function of the noninvolved growth plate.
Figure 1. (a) Internal structure of the prosthesis. (b) Prosthesis placed in the center of the magnetic generator. (c) Prosthesis before and after extension.
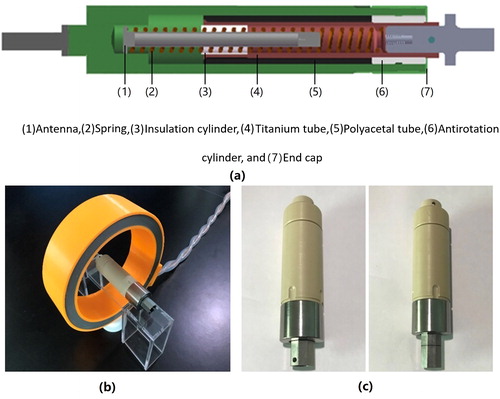
Expansion is achieved through exposure to an external electromagnetic field around the extremity. The intensity of the magnetic field is approximately 6000 A/m at 100 kHz frequency range for a 20-second duration. It is known that this intensity is much lower than MRI scan (1 Tesla machine = 8 × 1011 A/m), which reflects no harm to the human being. The electromagnetic field generates an electrical current within the flange of the spring housing tube and is focused on the receiving antennae within the implant. Due to the eddy effects produced, the heated element at the end of the titanium tube softens the surrounding polyacetal locking mechanism, which allows for spring expansion. Subsequently, the spring expansion pushes the two tubes apart, minimizing the difference in the overall length of the two limbs. Under fluoroscopic guidance, the electromagnetic field is applied until the desired amount of lengthening is achieved. Once the electromagnetic field disappears, the polyecetal tube cools and locks the spring in a new position while becoming solid.
To verify the reasonable extension of the prosthesis when implanted into the body, in vitro and in vivo animal experiments were conducted. This paper reports the experimental results and discusses the design and potential applications of our prosthesis.
Materials and methods
In vitro experiment
The maximum theoretical extension length is the length of the polyacetal tube (at 68 mm). The in vitro experiment was conducted to investigate the effect of prosthesis lengthening within the generated external electromagnetic field and to obtain the actual maximum extension length (in meters) and extension rate (in seconds). The experiment also verified whether the housing was at an acceptable temperature. In our previous experiments, the prosthesis began lengthening upon the generation of the magnetic field, but the extension time had to be limited to 5 s to prevent overheating.
Five prostheses were selected for the in vitro experiment, with each placed at the center of the generator for efficient extension (). The ambient temperature was set as 23 ± 1 °C, and humidity was maintained within 10%–50%. A series of basic operations was started by launching the magnetic generator for heating the polyacetal tube and producing the subsequent forward motion of the titanium tube. With the extension duration maintained at approximately 5 s, the extension length and maximum housing temperature were recorded. After a cooling stage of 15 min, the steps were repeated until maximum extension.
Ethics statement
The source of the sample was approved by the Animal Ethics Committee of Shanghai Anzhu Medical Technology Co. Ltd. Our experimental procedure complied with animal test criteria, which included minimizing stimulation intensity, eliminating the pain felt by the test animal and conducting humane euthanasia when the animal felt pain intensely; excessive harm to the animal was strictly prohibited. To ensure compliance, the experiment was conducted under third-party supervision.
In vivo experiment
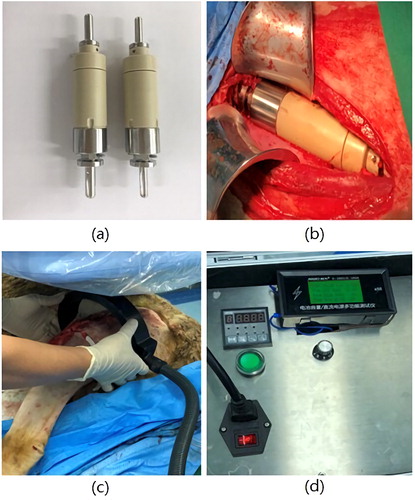
Because the length of a sheep’s limb is similar to that of a human limb, a sheep was selected as the subject for the in vivo experiment (). The weight of the adult sheep in our experiment was 45 kg. The animal was required to undergo physical examination and a set of auxiliary diagnostic tests before the experiment could proceed.
Table 1. Details of experimental sample.
To induce anesthesia, the intramuscular injection of hydrochloric acid serazine hydrochloride was performed preoperatively. The anesthesiologist maintained the induction of anesthesia during the test. After the induction of anesthesia, a bright oral tracheal intubation device was connected to a respirator machine and was controlled by a professional technician. The sheep’s breathing rate was approximately 20 times/min, and the tidal volume was 10 mL/kg (adjusted based on a blood gas analysis). The sheep was placed supinely on the operation table using bandage fixation, and a monitoring wire was subsequently connected to measure physiological parameters for the maintenance of anesthesia.
We then proceeded with our proposed prosthesis procedure. To implant the prosthesis, the intercept was set at around 155 mm from the rear femoral limb bone of the sheep (). The prosthesis was implanted into the cutting location of the rear femoral limb, and it was ensured that the prosthesis was fastened to the limb (). A known-diameter metal sphere was placed near the prosthesis as a reference measure. After suturing, a brim convex shape was observed based on X-ray images, and the shape was marked on the rear femoral limb. The external electrical magnetic generator was around in the rear femoral limb (), confirming that the marked position was at the center of the generator. The generator was set to power-off at approximately 20 s after power-on (). The X-ray film recorded the current state of the prosthesis based on the marked reference point. The first extension ended in cool-down time. After approximately 20 min, the second extension was conducted following the aforementioned steps. The total extension experiment was repeated three times until the prosthesis could not be extended.
Results and discussion
In vitro results
According to the in vitro results, the mean total extension length of the five selected prostheses was 61.9 mm (62.1, 60.4, 61.7, 62.2 and 63.6 mm), which is different from the theoretical value of 68 mm. The reason was that the prosthesis requires the locking mechanism to support the whole structure, and a part of the titanium tube must be fitted with the polyacetal tube to prevent the mechanism from failing. The appearance of the polyacetal tube did not change with extension, even at the maximum length, and the titanium tube was locked in place by the polyacetal tube.
The relationship between the mean value extension length and extension rate for extension was conducted 12 times and is presented in . Each extension value was measured from the five prostheses. As displayed in , the relationship between the mean rate and extension time was decreasing and approximately linear. The mean rate decreased from 0.9 to 0.1 mm/s, and we concluded that extension rate decreased as the extension length increased.
Figure 3. (a) Variation of the extension rate with extension time for five prostheses, *p < 0.05. (b) Variation of maximum temperature with extension time for one prosthesis. (c) Mean temperature after each extension for five prostheses, *p < 0.05.
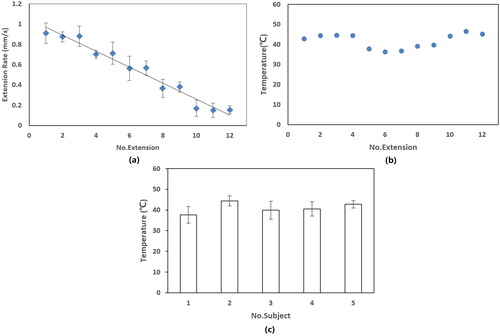
The relationship between the mean values and temperature of the housing surface for the five prostheses is presented in . The mean total temperature was approximately 41 °C, and the minimum and maximum mean temperatures were 37.7 °C and 44.4 °C, respectively. These results indicate that the maximum temperature was maintained within an acceptable range, and that temperature increases were not too rapid. The surface temperature of the housing continued to increase until it reached its maximum value, after which the magnetic generator powered off. This process could be sustained for approximately 2–3 min.
In vivo results
X-ray images enabled a comparison of the extension results before and after the implantation surgery (). The images revealed that the internal titanium component was implanted in the rear femoral limb and the nonmetallic component (the housing, antirotation cylinder and polyacetal tube) was not. In our proposed procedure, the prosthesis was extended only three times due to the limited length of the rear femoral limb. A total lengthening of 9 mm was obtained according to the X-ray images. With an invariable current of 2.5 A and magnetic generation time of 20 s, the extension lengths were 2, 4 and 3 mm for the three expansion procedures, with a mean extension length of 3 mm per extension time. Combining the X-ray images, the rear femoral limb was revealed to be lengthened by 9 mm.
Figure 4. (a, b) Prespective images after implantation. (c, d) Prespective images of prosthesis extension.
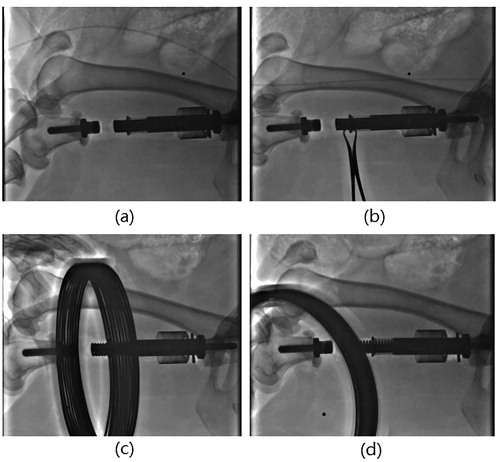
For further investigation, follow-up fluoroscopic guidance was used to determine whether the prosthesis displaced in no other direction when implanted into the rear limb (). According to , the adjacent bone (near the prosthesis) was not affected by the extension and retained its original position after implantation surgery (). Thus, consistent with our expectations, there was no trauma on the rear femoral limb.
To identify any internal component deformation, the technicians disassembled the prosthesis that was extracted from the rear femoral limb. All components were intact and undamaged. The extension of the prosthesis was based on the shifted titanium tube that was locked in a new position by the polyecetal tube. However, large quantities of blood were found in the prosthesis during the dismantling process. This was due to the poor sealing performance of the prosthesis, resulting in blood flow into the prosthesis.
The previous report mentioned that the incidence of osteosarcoma in all populations is around 4–5 per one million. It is higher in adolescents to 8–11 per one million population per year at the age of 15–19 years [Citation10,Citation11]. Overall, osteosarcoma has a moderate incidence rate, with 10–26 per million new cases worldwide each year [Citation12,Citation13].
Over the past 25 years, with the development of medical and health care technology, limb salvage has received increasing attention. These advances in bone tumor management have given surgeons and patients more treatment options instead of limb ablation. Limb salvage has replaced amputation as the treatment of choice for patients with malignant bone tumors of the extremities. In previous research, the overall survival of children after limb salvage was 94% at 24 months and 76% at 72 months, with a local recurrence rate of 9.4% [Citation14,Citation15].
Osteosarcomas are common around the knee joint, especially the distal femur. Reconstruction of the distal femur and proximal tibia after tumor resection is an important weight-bearing bone [Citation16]. With the application of modern effective treatment methods, limb salvage surgery has become the first choice for the treatment of osteosarcoma. There are several options for reconstruction of the distal femur and proximal tibia after tumor resection, including megaprosthesis, extracorporeally irradiated autograft and metallic plus bone cement. In developed countries, megaprosthesis is used widely because of their accessibility and convenience.
Megaprosthesis is the preferred method to repair the function and obtain the patient satisfaction [Citation15,Citation17,Citation18]. The advantage of knee reconstruction is that the patient can bear the weight immediately, maintain the flexibility of the joint and resume movement as soon as possible. The functional results after megaprosthes is reconstruction were generally good to excellent daily living activities [Citation19–21].
However, in children, limb salvage is associated with the problem of limb-length discrepancy resulting from the continued normal growth of the contralateral lower extremity [Citation22]. To address these problems, we designed a noninvasive extendable prosthesis that can be used to adjust the limb length according to the growth of the contralateral limb. The entire procedure drives the extension until the electromagnetic source is powered off. The extension procedure permits frequent extension, at smaller increments, with minimal discomfort.
To verify the feasibility of our noninvasive extendable prosthesis, we performed in vitro and in vivo (animal) experiments. In the in vitro experiment, the results revealed that the extension rates were variable due to the decreasing tendency of the spring potential; thus, any determination of the precise length through the control of the fixed extension time was invalidated. The maximum surface temperature was captured simultaneously after each extension, with 44 °C as the recorded average maximum temperature, which is within an acceptable range. In practice, adults can withstand this maximum temperature but children may not. This temperature may also cause redness and swelling of the skin.
For the in vivo experiment, we selected a sheep as the experimental subject. The prosthesis was implanted into the rear femoral limb of the sheep. Under fluoroscopic guidance, the extension experiment was repeated only three times due to the limited length of the sheep’s limb. The total lengthening was 9 mm, with an average length of 3 mm per 20 s (duration of the electromagnetic field). Outcome images after prosthesis implantation showed the position of prosthesis after each extension, and the support condition of the prosthesis was fixed in the rear limb. Combining the images and values for the extension, we concluded that the implanted noninvasive extendable prosthesis is indeed extendable. Thus, both in vitro and in vivo results verified that the prosthesis can lengthen in the body.
The prosthesis has its limitations for a long-term survival. Postoperative infection is a major complication of limb salvage for osteosarcoma. High dose chemotherapy leads to a serious decline in leukocytes and platelets, weakened anti-infection ability, and prone to postoperative infection owing to the interference of patients’ health status. The infection rate has reportedly reached 30% [Citation23]. Peri-prosthesis infection occurs easily after the construction of the prosthesis. This prosthesis is composed of a variety of metal material, such as titanium alloy, cobalt-chromium alloy and ferrite. Thus, looking for new type material alternative is an ongoing concern. At the 16th international limb salvage conference (ISOLS), the researchers have reported that the application of silver-plated material in prosthesis revision, tibial prosthesis, radiotherapy and other operations with high infection risk achieved good preventive effect. Also, they reported that an iodine - plated titanium alloy material can be used to prevent infection and immunosuppression also produced satisfactory results [Citation24]. Other researchers have used antibiotic-coated prosthesis to treat osteosarcoma patients and control infections. They also confirmed that chitosan-methotrexate-titanium substrate could not only inhibit the adhesion and proliferation of giant cell tumor cells and promote the apoptosis of tumor cells, but also prevent bacterial adhesion, thus forming bacterial biofilms and protecting cells from infection. The material could solve the problem of infection after tumor prosthesis surgery, but need further experiments conducted in animals in vivo.
Regarding the internal components of the prosthesis, the extendable mechanism mainly relies on the elastic potential of the spring, and load bearing is dependent on the locking between the titanium and polyacetal tubes. Thus, this prosthesis may not be able to address walking or standing problems for patients, and mechanical failure may occur after long-term usage. The next limitation of the prosthesis is that its poor sealing performance can cause infection. Blood and other tissue fluids that permeate into the prosthesis will heat up when the prosthesis extends. The reintroduction of the heated fluid into the body may cause complications. The final limitation is the irregular extension rates. This prosthesis is not capable of retraction at a certain length; thus, precise extension requires more than just fluoroscopic guidance, determining the appropriate extension length in 1 s is a possible solution.
Conclusions
Our study indicated that in pediatric patients, our noninvasive extendable prosthesis can be a reliable option for treating bone sarcoma of the lower extremity. Both in vitro and in vivo results verified that the prosthesis can lengthen in the body. Meantime, the potential problem still need out attention in the future. To eliminate complications from postoperative infection, we will consider to replace the original material of end cap with iodine - plated titanium alloy and conduct further experiments in animals and in vitro. Also, the numerical simulation and dynamic force test will be applied to this prosthesis for exploring out the supporting performance.
Acknowledgements
The authors would like to acknowledge Scientific research project of Shanghai Science and Technology Commission (Serial No. 15441903000).
Disclosure statement
We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted. Dr. Zhaohua Chang is the Chairman, Executive Director and Chief Executive Officer of GMC of MicroPort.
Additional information
Funding
References
- Marcove RC, Miké V, Hajek JV, et al. Osteogenic sarcoma under the age of twenty-one: a review of one hundred and forty-five operative cases. JBJS. 1970;52(3):411–423.
- Ferrari S, Mercuri M, Bacci G, et al. Comment on “Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant Cooperative Osteosarcoma Study Group protocols. JCO. 2004;17(3):131–137.
- Kenan S, Bloom N, Lewis MM. Limb-sparing surgery in skeletally immature patients with osteosarcoma. The use of an expandable prosthesis. Clin Orthop Relat Res. 1991;270(270):223.
- Tang X, Guo W, Yang R, et al. Limb salvage surgery for osteosarcoma around the knee in children and adolescent patients. Zhonghua Wai Ke Za Zhi. 2007;45(10):669–672.
- Rougraff BT, Simon MA, Kneisl JS, et al. Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. A long-term oncological, functional, and quality-of-life study. JBJS. 1994;76(5):649–656.
- Chauhan A, Joshi GR, Chopra BK, et al. Limb Salvage surgery in bone tumors: a retrospective study of 50 cases in a single center. Indian J Surg Oncol. 2013;4(3):248–254.
- Arkader A, Viola DCM, Morris CD, et al. Coaxial extendible knee equalizes limb length in children with osteogenic sarcoma. Clin Orthop Relat Res. 2007;459(459):60–65.
- Zhang C, Zeng B, Zhu K, et al. Limb salvage for malignant bone tumours of distal tibia with dual ipsilateral vascularized autogenous fibular graft in a trapezoid-shaped array with ankle arthrodesis and preserving subtalar joint. Foot & Ankle Surgery. 2017;25(3):278-285.
- Henderson ER, O'Connor MI, Ruggieri P, et al. Classification of failure of limb salvage after reconstructive surgery for bone tumours: a modified system Including biological and expandable reconstructions. Bone Joint J. 2014;96-B(11):1436–1440.
- Kamal AF, Widyawarman H, Husodo K, et al. Clinical outcome and survival of osteosarcoma patients in Cipto Mangunkusumo Hospital: limb salvage surgery versus amputation. Acta Medica Indonesiana. 2016;48(3):175–183.
- Ando K, Heymann MF, Stresing V, et al. Current therapeutic strategies and novel approaches in osteosarcoma. Cancers (Basel)). 2013;5(2):591–616.
- Ottaviani G, Jaffe N. The epidemiology of osteosarcoma. Cancer Treat Res. 2009;152:3–13.
- Xin S, Wei G. Prognostic factors in osteosarcoma: a study level meta-analysis and systematic review of current practice. J Bone Oncol. 2020;21:100281. DOI. 10.1016/j.jbo.2020.100281.
- Pesenti S, Peltier E, Pomero V, et al. Knee function after limb salvage surgery for malignant bone tumor: comparison of megaprosthesis and distal femur allograft with epiphysis sparing. Int Orthop (Sicot)). 2018;42(2):427–436.
- Fauzi KA, Astuti P, Yogi P. Megaprosthesis limb salvage surgery: outcome and challenges in treating advanced bone tumour cases in vast archipelago in Indonesia. A case series. Int J Surg Open. 2018;11:30–36.
- Muratori F, Mondanelli N, Prifti X, et al. Total femur prosthesis in oncological and not oncological series. Survival and failures. J Orthop. 2020;17:215–220.
- Sharil AR, Nawaz AH, Azman MN, et al. Early functional outcome of resection and endoprosthesis replacement for primary tumor around the knee. Malays Orthop J. 2013;7(1):30–35.
- Kamal AF, Rubiansyah P. Clinical outcome of various limb salvage surgeries in osteosarcoma around knee: megaprosthesis, extracorporeal irradiation and resection arthrodesis. Ann Med Surg (Lond)). 2019;42:14–18.
- Kim W, Han I, Lee JS, et al. Postmetastasis survival in high-grade extremity osteosarcoma: a retrospective analysis of prognostic factors in 126 patients. J Surg Oncol. 2018;117(6):1223–1231.
- Gautam D, Malhotra R. Megaprosthesis versus allograft prosthesis composite for massive skeletal defects. J Clin Orthop Trauma. 2018;9(1):63–80.
- Henrichs M-P, Liem D, Gosheger G, et al. Megaprosthetic replacement of the distal humerus: still a challenge in limb salvage. J Shoulder Elbow Surg. 2019;28(5):908–914.
- Forni C, Gaudenzi N, Zoli M, et al. Living with rotationplasty-quality of life in rotationplasty patients from childhood to adulthood. J Surg Oncol. 2012;105(4):331–336.
- Jeys LM. Periprosthetic infection in patients treated for an orthopaedic oncological condition. J Bone and Joint Surg (American). 2005;87(4):842.
- Yang Y, Han L, He Z, et al. Advances in limb salvage treatment of osteosarcoma. J Bone Oncol. 2018;10:36–40.