Abstract
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality worldwide. It is also associated with significant concomitant diseases which affect the disease progression course, and contribute to the exacerbation of health status and overall mortality rate. The aim of this study was to identify the most frequent Cardio-vascular disease (CVD) comorbidities among patients with COPD in Bulgaria and their effect on the hospitalization rate, hospital stay duration and health status. A retrospective national observational study was conducted among a statistically representative cohort of 426 patients in Bulgaria. Demographic data, smoking, clinical data for COPD severity and co-morbidity were collected. Health status was assessed through the specific COPD assessment test (CAT). CVD co-morbidity was evaluated by type, considering the GOLD guidelines and number. More than 80% of the patients reported two and more CVD co-morbidities and all of them reported more than two exacerbations and more than two hospitalizations over the last year. The most frequently reported CVD co-morbidity was hypertension, which was present in 88% of the men and in 89% of the women. The data showed a positive correlation between the cardiovascular risk and the progression of the disease. Hypertension, ischemic heart disease and heart failure prevailed in the observed population. With the advancement of COPD, the number of CVDs diseases per patient and CAT score, average hospitalization rate and hospital stay increased.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality worldwide and its burden is estimated to increase due to continuous exposure to COPD risk factors: tobacco smoking, biomass fuel exposure, air pollution and aging of population [Citation1,Citation2].
COPD patients also experience significant concomitant diseases which impact the disease progression and contribute to the overall morbidity and mortality [Citation1]. Cardio-vascular diseases (CVDs) are one of the most significant and important co-morbidities in these patients [Citation3–5] with common pathogenic mechanisms: systemic inflammation, oxidative stress, extracellular matrix destruction, etc. [Citation6] mostly due to personal behaviour risk factors: tobacco smoking and sedentary lifestyle. Large studies have also shown that airflow limitation is an independent risk factor for CVD proving that COPD has significant systemic consequences [Citation7,Citation8].
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) the five most common CVDs that should always be considered in these patients are arterial hypertension, ischemic heart disease, chronic congestive heart failure, rhythm disorders and peripheral vascular disease (PVD) [Citation1]. Patients with COPD should periodically be monitored for symptoms of ischemic heart disease, especially in more severe stages, as the risk of myocardial impairment during an acute exacerbation is increased in patients manifesting both diseases [Citation9]. The annual incidence rate of heart failure in patients with COPD is 3–4% and is a significant and independent mortality factor [Citation10]. Undiagnosed heart failure can accompany acute exacerbation [Citation11]. Cardiac arrhythmias are another common co-morbidity to COPD, with atrial fibrillation having the most direct impact on FEV1 values [Citation12]. The COSYCONET study showed that the prevalence of PVD among patients with COPD is higher than in the general population (8.8%), regardless of disease severity [Citation13]. Arterial hypertension is the most common CVD in COPD patients. A great number of studies have shown that diastolic dysfunction may lead to exercise intolerance and mimic acute exacerbation which may provoke the need for hospitalization [Citation14]. The GOLD document recommends regular blood pressure control in patients with both COPD and hypertension [Citation1].
Bulgaria ranks third in Europe in terms of CVD-related mortality, after Belarus and Ukraine, with an annual mortality rate at 888.7/100,000, and first among the Central and Eastern European Countries. The major risk factors are smoking and increased sodium consumption. Bulgaria is the European country with the highest annual mortality for COPD: 110.2/100,000, which is almost 2.5 times higher than the annual COPD mortality in Central Europe: 42.9/100,000. Tobacco smoke and air pollution are the most prominent risk factors in Bulgaria [Citation15].
Data from the Institute for Health Metrics and Evaluation show that CVD and COPD were in the top six reasons for disability and premature death in Bulgaria for 2016 [Citation15]. Studies, conducted in Bulgaria among COPD patients, show that they are with increased risk of CVDs [Citation16–18].
These data prompted us to investigate the most frequent cardio-vascular type of co-morbidities (according to GOLD 2019) in COPD patients in Bulgaria and their impact on the health status. In our opinion, identifying the type of CVDs in these patients could improve the complex monitoring, optimize their pharmacotherapy and reduce the mortality.
Subjects and methods
Ethics statement
All patients recruited in this study were informed about the study design and its aim, and signed informed consent forms. The study was approved by the Bulgarian National Science Fund.
Study design and patients’ characteristics
A retrospective observational study was conducted among statistically representative cohort of 426 patients with pulmonary functional tests (PFT) (spirometry, FEV1/FVC ≤ 70%) proven COPD in the five main regions in Bulgaria – North-Western, North-Eastern, South-West, South-East Bulgaria and Sofia-town. A sample size of 405 COPD Bulgarian patients considered nationally representative was calculated using the 5% standard error and the confidence level of 99% [Citation14]. The country was divided into four regions – North-western, South-western, North-eastern, South-eastern. The capital Sofia was added as a separate region because of the size of its population. Between three and five towns were chosen from every region and the number of citizens enrolled in the study for each region was calculated according to population data from the National Statistics Institute (NSI). Thus the target number of COPD patients for North-western region was 30, for South-western – 29, for North-eastern – 77, for South-eastern – 89 and for Sofia – 180. The pulmonologists were then asked to choose every fifth COPD patient from their registries as a form of random sampling. The final number of enrolled COPD patients was as follows: for the North-western region – 38, for the South-western one – 58, for the North-eastern one – 76, for the South-eastern one – 111, and for Sofia – 143. Every fifth enrolled patient was asked to participate and sign an informed consent form. Demographic data (age, gender), smoking and occupational status and clinical data for COPD duration, severity, pharmacotherapy, hospitalizations and co-morbidity were collected. COPD status was assessed through spirometry and assigned to the respective groups A, B, C and D, according to GOLD classification for that period. Health status was assessed through the specific CAT. CVD co-morbidity was evaluated by type, considering GOLD and their number.
Statistical analysis
Descriptive statistics and chi-squared test of independence for categorical variables were performed. Patients were separated into four groups according to the severity of COPD 2019 and based on pulmonary function tests (PFT results) (mild, moderate, severe and very severe), and GOLD classification (A – low risk and less symptoms, B – low risk and more symptoms, C – high risk and less symptoms and D – high risk and more symptoms); in two gender groups (male and female); two CAT score groups (<10 and >10); three groups with cardiovascular diseases (1; 2 and more than 2 CVDs). Statistical analysis was done using MedCalc v. 16.4.3.
Results and discussion
Demographic characteristics
Out of 426 patients included in the observational study 296 were men and 130 women. The average age in the cohort was 66 ± 9.09 years. The majority of the patients reported a history of smoking with mean pack-years of 38.16 ().
Table 1. Demographic characteristics.
Clinical characteristics and CVD co-morbidities
GOLD ABCD tool was used to assess the severity of COPD. The majority of the patients at the time of recruitment were at GOLD B (35%) and GOLD D (43%). The mean number of exacerbations for the last year was 2, irrespective of gender, with at least one of them leading to an ER visit or hospitalization. More than 80% of the patients in the sample reported concomitant cardio-vascular morbidity, additionally over 80% had 2 or more comorbidities ().
Table 2. Clinical characteristics.
The most frequently reported CVD co-morbidity was hypertension, which was present in 223 (88%) of the men with COPD and in 95 (89%) of the women in the observed cohort. Heart failure and ischemic heart disease were observed in 39% and 33% of the females, respectively. Arrhythmias were reported in 6% of the COPD patients, irrespective of gender. None of the women were diagnosed with PVD.
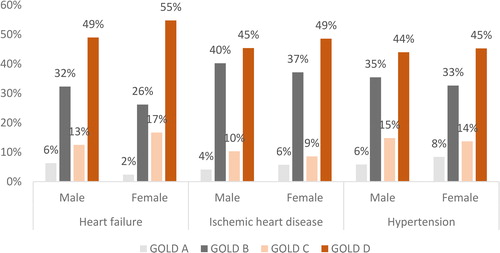
Further sub-group analysis investigated the three most frequently reported CVD-comorbidities: hypertension, heart failure and ischemic heart disease, according to COPD severity ().
Hospitalizations rate
In the observed cohort of patients, those diagnosed with GOLD C and D COPD had the highest average number of exacerbations for the last year (n = 2, SD 1.6 and n = 3, SD 1.6, respectively) and the longest duration of hospital stay: 5 and 10 days on average, respectively ().
Table 3. Hospitalization rate and average hospital stay according to GOLD ABCD.
Health status
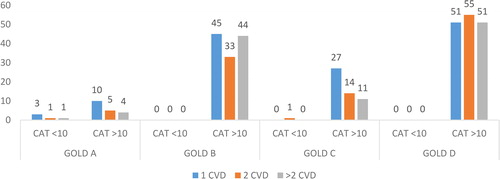
The evaluation of the health status of the patients with CAT showed that with the increase of the severity of the disease according to the GOLD ABCD assessment tool and the increase in the number of concomitant CVDs, the number of patients with CAT score above 10 also increases. This indicated deterioration in the health status ().
Chi-squared analysis
Comparing different groups of variables, we found only two significant positive relationships (p < 0.05). Age was positively related to COPD severity (χ2=22.907, p = 0.0064) and COPD severity was positively related to the number of cardiovascular comorbidities (χ2=11.384, p = 0.0772). Moderate relationships were found between the number of cardio-vascular co-morbidities and the duration of hospital stay (χ2=22.692, p = 0.0069).
Cardio-vascular diseases are one of the most frequently reported co-morbidities in patients with COPD and contribute to the overall disability and mortality [Citation19]. Among them arterial hypertension is one of the most common comorbidities, affecting 40–60% of COPD patients [Citation6]. The mechanisms by which COPD may be a risk factor for CVD are not fully understood, but it is considered that airflow limitation and particularly hyperinflation affect cardiac function, and that inflammatory mediators in circulation may initiate or worsen comorbidities such as ischemic heart disease and heart failure [Citation20,Citation21]. These were also the most frequent comorbidities present in our sample, which adds support to the above-mentioned considerations. In our sample the percentage of respondents with two or more concomitant diseases was very high – 80%, which is similar to the results of another study where 73% were suffering from one or more comorbid conditions [Citation22]. An analysis in Greece also revealed that around 82% of patients with COPD report at least one concomitant disease and that the most common disease among the cohort was hypertension (55.3%) [Citation23].
A meta-analysis reported that the crude prevalence of CVD ranged from 28% to 70%, mostly due to differences in studied populations and CVD definitions [Citation24]. A Serbian survey also reports that the most prevalent co-morbidities among patients with COPD are hypertension (54.5%) and dyslipidaemia (26.5%), which is similar to our results [Citation25]. We observed a range from 2% for peripheral vascular to 82% for hypertension. It could also be due to the fact that COPD and CVD share a number of risk factors, including smoking and aging.
Our study confirms previously published data that with the advancement of COPD, the comorbidities increase to more than two and present a possible future risk for more health complications. These data are similar to the results of other studies. A prospective study conducted in Greece among 609 patients shows that the presence of cardiovascular diseases is related to higher risk of exacerbations and hospitalizations, especially in patients experiencing more symptoms (GOLD B and GOLD D) [Citation26].
A regional study [Citation27] among 3751 patients with COPD in the Pleven region in Bulgaria showed a statistically significant correlation between the age of the patients and the prevalence of CVDs (r = 0.38, p = 0.0001). Patients with COPD also showed increased cardiovascular risk compared to the general population with OR = 1.2 for arterial hypertension and 1.9 for heart failure.
Another Bulgarian study showed that COPD patients suffering from severe exacerbations are at great cardiovascular risk most probably due to the high prevalence of arterial hypertension [Citation18]. These studies, however, are only of a regional character.
Recent studies among patients with COPD evaluated tobacco smoke and arterial stiffness and day-and night blood pressure as parameters for detection of early atherosclerosis in COPD. The results show that in patients with COPD compared with healthy controls day-and night blood pressure and arterial stiffness parameters were elevated showing signs of earlier atherosclerosis and higher cardiovascular risk [Citation28]. Tobacco smoke among patients with COPD is proved to be a risk factor for elevated aortic pulse wave velocity (aPWV) which has positive correlation with tumorigenicity 2, a marker for major cardiovascular risk [Citation29].
It is expected that the multi-morbidity will impact health status [Citation30]. The results of studies support the use of the CAT as a simple tool to assist in the identification of patients at increased risk of exacerbations [Citation31]. Worsening of CAT score in patients with CVD is used as a marker for increasing risk of diseases progression [Citation26]. Patients with COPD and high CAT scores should be actively treated for their cardiovascular comorbidities, to reduce CV exacerbations and mortality [Citation32]. Our study also showed that all patients with more than two exacerbations for the last year and more than two hospitalizations had also CV co-morbidities which also influence the duration of hospital stay. More than 50% also had type 2 diabetes. These patients, apart from COPD pharmacotherapy, take at least three other additional medications for the treatment of their co-morbidities. This puts the patients into increased risk of drug-related problems like drug–drug interactions or adverse drug reactions. Polypharmacy is a prevalent issue in Europe, particularly among elderly individuals >65 years, which necessitates that these patients are monitored closely.
Our study is the first study performed on a national level with real-world data and the results are considered as statistically relevant for the total COPD population in Bulgaria. As a limitation, however, we can consider that the patients self-reported the incidence of their CVDs, and no cardiologic clinical variable was obtained to determine the severity. The patients also had other co-morbidities that might further influence the cardio-vascular risk, i.e. more than 50% of the patients reported at least one endocrine disorder with type 2 diabetes being the most frequently reported. Some patients might not be aware that they have CVD. Identifying the type of CVDs could improve the complex monitoring of these patients, optimize their pharmacotherapy and reduce mortality. Further studies should be carried out among the Bulgarian population with COPD in order to investigate the mortality risk after myocardial infarction in comparison with non-COPD patients, which is in the focus of recently conducted international studies [Citation33]. Moreover, the economic burden of COPD therapy [Citation34], the burden associated with CVD in patients with COPD, the cost for treatment of these concomitant diseases and the burden of possible drug-related problems is another valuable area for future researches in Bulgaria [Citation35].
In this respect, a multidisciplinary approach which also includes the expertise of pharmacists in terms of preventing drug-related problems would be valuable to reduce the rate of ER visits or hospitalizations [Citation36]. This is now more important than ever, especially in the current situation of global COVID-19 pandemic, because it is already proven that patients with COPD and cardiovascular diseases are put at increased COVID-associated mortality risk [Citation37]. Further analysis is also needed to evaluate the possible role of the pharmacists in hospital and community settings in the process of pharmacotherapy monitoring and reducing the risk of drug-related problems.
Conclusions
Patients with COPD present more cardiovascular comorbidities than the general population. The number of CVD comorbidities increases with disease progression due to the overlapping nature of the risk factors associated with both diseases. Hypertension, ischemic heart disease and heart failure prevail in the observed population. With the progression of COPD, the number of cardio-vascular co-morbidities per patient increases. We observed also an increase in the CAT score, pointing out to the deterioration in the health status and an increase in the hospitalization rate and duration of hospital stay.
Acknowledgements
This work is part of a project assessing the risk and the adherence to therapy and their impact on the cost of pharmacotherapy and health status of patients with COPD in Bulgaria.
Disclosure statement
The authors do not have any conflict of interests to declare.
Additional information
Funding
References
- GOLD 2019. [cited 2019 May]. Available from: http://goldcopd.org/wp-content/uploads/2017/11/GOLD-2010-v6.0-FINAL-revised-20-Nov_WMS.pdf.
- Antoniu SA. Reducing mortality for chronic obstructive pulmonary disease: role of statins and angiotensin-covering enzyme inhibitors. Exp Rev Parmacoecon Outcomes Res. 2009;9(6):523–525.
- Soriano JB, Visick GT, Muellerova H, et al. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128(4):2099–2107.
- Fabbri LM, Luppi F, Beghe B, et al. Complex chronic comorbidities of COPD. Eur Respir J. 2008;31(1):204–212.
- Trinkmann F, Saur J, Borggrefe M, et al. Cardiovascular comorbidities in chronic obstructive pulmonary disease (COPD)-current considerations for clinical practice. JCM. 2019;8(1):69.
- Dalal AA, Shah M, Lunacsek O, et al. Clinical and economic burden of patients diagnosed with COPD with comorbid cardiovascular disease. Respir Med. 2011;105(10):1516–1522.
- Maclay JD, McAllister DA, Macnee W. Cardiovascular risk in chronic obstructive pulmonary disease. Respirology. 2007;12(5):634–641.
- Osmanliev D. COPD – Cardiovascular comorbidity and safety of beta 2 agonists with focus on the indacaterol. Thoracic Med. 2013;5(3):10–20.
- Hoiseth AD, Neukamm A, Karlsson BD, et al. Elevated high-sensitivity cardiac troponin T is associated with increased mortality after acute exacerbation of chronic obstructive pulmonary disease. Thorax. 2011; 66(9):775–781.
- Finkelstein J, Cha E, Scharf SM. Chronic obstructive pulmonary disease as an independent risk factor for cardiovascular morbidity. Int J Chron Obstruct Pulmon Dis. 2009;4:337–349.
- MacDonald MI, Shafuddin E, King PT, et al. Cardiac dysfunction during exacerbations of chronic obstructive pulmonary disease. Lancet Respir Med. 2016;4(2):138–148.
- Buch P, Friberg J, Scharlin H, et al. Reduced lung function and risk of atrial fibrillation in the Copenhagen City Heart Study. Eur Respir J. 2003;21(6):1012–1016.
- Houben-Wilke S, Jorres RA, Bals R, et al. Peripheral artery disease and its clinical relevance in patients with COPD in the COSYCONET Study. Am J Respir Crit Care Med. 2017;195(2):189–197.
- Lopez-Sanchez M, Munoz-Esquerre M, Huertas D, et al. High prevalence of left ventricle diastolic dysfunction in severe COPD associated with a low exercise capacity: a cross-sectional study. PLoS One. 2013;8(6):e68034.
- Institute for Health Metrics and Evaluation: Bulgaria. [cited Jan 2018]. Available from: http://www.healthdata.org/bulgaria.
- Kamusheva M, Dimitrova M, van Boven JFM, et al. Clinical characteristics, treatment patterns, and socio-economic burden of COPD in Bulgaria. J Med Econ. 2017;20(5):503–509.
- Mekov E, Slavova Y, Tsakova A, et al. Cardiovascular risk assessment in COPD patients with severe exacerbation. Eur Respirat J. 2016;48:PA1134.
- Pavlov P, Ivanov Y, Glogovska P, et al. Cardiovascular comorbidity and mortality in patients with chronic obstructive pulmonary disease. Eur Respirat J. 2012;40:P986.
- Ni Y, Shi J, Wan H. Use of cardioselective β-blockers in patients with chronic obstructive pulmonary disease: a meta-analysis of randomized, placebo-controlled, blinded trials. J Int Med Res. 2012;40(6):2051–2065.
- O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease—2007update. Can Respir J. 2007;14(Suppl. B):5B–32B.
- Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018;27(149):180057.
- van Manen JG, Bindels PJ, IJzermans CJ, et al. Prevalence of comorbidity in patients with a chronic airway obstruction and controls over the age of 40. J Clin Epidemiol. 2001;54(3):287–293.
- Mitsiki E, Bania E, Varounis C, et al. Characteristics of prevalent and new COPD cases in Greece: the GOLDEN study. Int J Chron Obstruct Pulmon Dis. 2015;10:1371–1382.
- Müllerova H, Agusti A, Erqou S, et al. Cardiovascular comorbidity in COPD: systematic literature review. Chest. 2013;144(4):1163–1178.
- Nagorni-Obradovic L, Vukovic D. The prevalence of COPD co-morbidities in Serbia: results of a national survey. NPJ Prim Care Respir Med. 2014;24:12020–14008.
- Papaioannou AI, Bartziokas K, Loukides S, et al. Cardiovascular comorbidities in hospitalised COPD patients: a determinant of future risk? Eur Respir J. 2015;46(3):846–849.
- Ivanov Y, Nikolaev I, Nemeth I. Real-life evaluation of COPD treatment in a Bulgarian population: a 1-year prospective, observational, noninterventional study. Int J Chron Obstruct Pulmon Dis. 2018;13:653–663.
- Bocskei RM, Benczur B, Bikov A, et al. Cardiovascular risk detection in COPD. Eur Respir J. 2019;54:PA5016.
- Soumagne T, Roche N, Guillien A, et al. Cardiovascular risk in COPD: Deciphering the contribution of tobacco smoking. Chest. 2020;157(4):834–845.
- Hutchinson AF, Graco M, Rasekaba TM, et al. Relationship between health-related quality of life, comorbidities and acute health care utilisation, in adults with chronic conditions. Health Qual Life Outcomes. 2015;13:69.
- Lee SD, Huang MS, Kang J, et al. Investigators of the Predictive Ability of CAT in Acute Exacerbations of COPD (PACE) Study. The COPD assessment test (CAT) assists prediction of COPD exacerbations in high-risk patients. Respirat Med. 2014;108(4):600–608.
- Fragoso E, André S, Boleo-Tomé JP, et al. Understanding COPD: a vision on phenotypes, comorbidities and treatment approach. Rev Port Pneumol (2006). 2016;22(2):101–111.
- Quint J. The Relationship between COPD and cardiovascular disease. Tanaffos. 2017; 16(Suppl 1):S16–S17.
- Bayar B, Kutkan NU, Yilmaz ES, et al. Cost evaluation of inhaler therapies used in respiratory diseases: 1998-2015 period in Turkey. Value Health Reg Issues. 2017;13:31–38.
- Morgan AD, Zakeri R, Quint JK. Defining the relationship between COPD and CVD: what are the implications for clinical practice. Ther Adv Respir Dis. 2018;12:1753465817750524
- Juanes A, Garin N, Mangues MA, et al. Impact of a pharmaceutical care programme for patients with chronic disease initiated at the emergency department on drug-related negative outcomes: a randomised controlled trial. Eur J Hosp Pharm. 2018;25(5):274–280.
- Wang B, Li R, Lu Z, et al. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging. 2020; 12(7):6049–6057.