Abstract
Naoxintong Capsule (NXT), a Chinese medicine, has been widely used for the treatment of cardiovascular diseases in clinic. The present study was designed to clarify the effects of NXT on haemorheology, blood coagulation, hepatic function, antioxidant capacity and inflammatory responses in a rat model of blood stasis syndrome. Rats were placed in ice-cold water for 5 min during the time interval of two adrenaline injections to induce blood circulation disorders after intragastric administration of 10 consecutive days. Blood was collected from abdominal aorta to determine whole blood viscosity (WBV), plasma viscosity (PV), activated partial thromboplastin time (APTT), prothrombin time (PT), fibrinogen (FIB), total antioxidant capacity (T-AOC), superoxide dismutase (SOD), malonaldehyde (MDA), alanine transaminase (ALT), aspartate transaminase (AST), interleukin-1β (IL-1β), interleukin-6 (IL-6), platelet activating factor (PAF). The results showed that NXT could significantly decrease the WBV, PV, FIB and prolong the APTT and PT. Meanwhile, NXT significantly decreased the serum contents of MDA, IL-1β, IL-6, ALT, AST and PAF, while elevating T-AOC and SOD levels. These results indicate that NXT could improve coagulation function, enhance antioxidant capacity and suppress inflammation, which might partly account for its mechanisms of action in preventing and treating cardiovascular diseases.
Introduction
Cardiovascular diseases (CVD) have become the major killer of the public health worldwide, including coronary heart disease, hypertension, stroke and heart failure [Citation1]. Blood circulation disorders are described as blood stasis in traditional Chinese medicine (TCM) theory, characterized as a slowing or pooling of the blood due to disruption of heart Qi, which is often understood in terms of hematological disorders such as hemorrhage, congestion, thrombosis, local ischemia, and tissue changes [Citation2]. Blood stasis is accompanied by coagulation abnormalities, inflammation and free radical accumulation, which in turn further promote the occurrence of blood stasis [Citation3]. Reports have suggested that blood stasis is an important underlying pathology of many disease processes [Citation4] and is often found in the course of diseases such as CVD [Citation5–7].
The blood stasis model, which was obtained by placing rats in ice-cold water during the time interval between two injections of adrenaline, has been widely used [Citation8–10]. As an acute-stress, the injection of adrenaline could cause striction of peripheral vessels, enhancement of myocardial contraction, as well as haemorheological disorders such as blood hypercoagulability and a rise of blood coagulation activity [Citation11, Citation12]. Besides, the effect of adrenaline will be enhanced via the exposure to ice-cold water because of increasing the cardiac afterload and myocardial oxygen consumption.
Traditional Chinese medicines have long been used in the prevention and treatment of CVD due to positive performance and few adverse effects [Citation13, Citation14]. Buyang Huanwu Decoction (BHD), a classic formula for activating blood circulation and removing stasis, has been recognized as a treatment for CVD in clinical practices. [Citation15, Citation16]. Naoxintong Capsule (NXT), developed from BHD, consists of 16 kinds of herbs: Astragalus membranaceus, Paeonia lactiflora, Salvia miltiorrhiza, Angelica sinensis, Ligusticum chuanxiong, Prunus persica, Achyranthes bidentata, Morus alba, Pheretima aspergillum, Hirudo nipponica, Spatholobus suberectus, Cinnamomum cassia, Carthamus tinctorius, Boswellia carterii, Commiphora myrrha and Buthus martensii. Early in 1993, NXT was approved by the China Food and Drug Administration (CFDA) (State Medical License No. Z20025001). For more than 20 years, NXT has played an important role in treating patients with CVD with good clinical performance [Citation17, Citation18]. Many studies have demonstrated that NXT has the characteristics of multi-component interaction with multiple targets in treating CVD. For instance, NXT protected proatherogenic animals against atherosclerosis with the improvement of serum lipid profiles, reduction of inducible nitric oxide synthase expression in lesions and inhibition of dendritic cell maturation [Citation19, Citation20]. In our previous studies, the material basis of NXT was investigated and 59 active constituents were identified [Citation21]. However, little research has been done on the systematic functions of NXT, especially with regard to the mechanisms against CVD. It is known that maintaining good blood circulation, good antioxidant functioning and balanced inflammatory cytokine networks are necessary for fighting against CVD. Therefore, in this study, we investigated the effect of NXT on haemorheology, blood coagulation, antioxidant capacity and inflammatory responses in rats with blood circulation disorders, with BHD and aspirin serving as positive control. These results provided valuable insight on revealing the mechanisms underlying the activity of NXT against CVD.
Materials and methods
Ethical statement
All experimental procedures were carried out according to the National Institutes of Health guide for the care and use of laboratory animals and were approved by the Animal Care and Use Committee of the School of Life Sciences of Sun Yat-sen University (Permission No. 2016022014). Any harm to rats was minimized during the experimental process by taking appropriate measures.
Animals
Forty-nine male sprague-dawley rats, specific pathogen free (SPF), weighing 180-220 g, were obtained from Guangdong Medical Experimental Animal Center (Certification No. SCXK-(Yue) 2013-0002, Quality Qualification Certificate No. 44007200028430) and raised in the SPF houses of Ocean and Traditional Chinese Medicine Laboratory of Sun Yat-sen University (License No. SCXK-(Yue) 2014-0020). The temperature of the SPF houses was 20-23 °C and the relative humidity was 50-65%. Rats were fed by standard pellet feed and kept under a 12-h dark-light cycle. The experiments began after the rats adapted to the new environment for one week.
Preparation of drugs
NXT capsules (State Medical License No. Z20025001, composed of Astragalus membranaceus, Paeonia lactiflora, Salvia miltiorrhiza, Angelica sinensis, Ligusticum chuanxiong, Prunus persica, Achyranthes bidentata, Morus alba, Pheretima aspergillum, Hirudo nipponica, Spatholobus suberectus, Cinnamomum cassia, Carthamus tinctorius, Boswellia carterii, Commiphora myrrha and Buthus martensii) were provided by Shanxi Buchang Phamaceutical Co.Ltd. NXT capsules were flayed, triturated, quantified and then were dissolved with normal saline to 200 mg/mL. Aspirin was purchased from Bayer HealthCare Co.Ltd. (State medical permission No. H20130192, Batch No. BJ24230). Adrenaline was purchased from Sichuan Hengtong Animal Pharmacy Co. Ltd. (State medical permission No. 220381220, Batch No. 20150801). Aspirin was triturated, quantified and then dissolved with normal saline to 10 mg/mL. Adrenaline was diluted with normal saline to 0.4 mg/mL before use.
Based on the original prescription from Yi Lin Gai Cuo, BHD consists of seven medicinal components, including Astragalus membranaceus, Angelica sinensis, Ligusticum chuanxiong, Paeonia lactiflora, Pheretima aspergillum, Prunus persica and Carthamus tinctorius. The components were mixed in order with the ratio of 120:6:3:4.5:3:3:3 (dry weight). All of the herbal components were GAP grade and purchased from Guangzhou Zhongshuntang Co, Ltd. These crude drugs were soaked in distilled water and boiled twice, for 30 min each time [Citation22]. The drug solution was filtered through a mesh, then the filtrates were combined and concentrated to 3.0 g/mL (equivalent to the dry weight of crude drugs). The combined filtrates were collected and stored at 4 °C until use.
Experimental instruments and reagents
Ultra-low temperature freezer (Haier, BCD-568W); 1/100000 Electronic analytical balance (Sartorius, Germany, BP211D); Refrigerated centrifuge (Eppendorf, 5430 R); Full-automatic blood coagulation analyzer (Sysmex, CA-510); Full-automatic self-cleaning haemorheology analyzer (Beijing Precil, LBY-N6B); Full-automatic biochemical analyzer (COBAS INTEGRA 800).
Experimental model
Rats were randomly divided into seven groups, including normal group, model group, NXT-L (500 mg/kg/d) group [Citation23], NXT-M (1000 mg/kg/d) group, NXT-H (2000 mg/kg/d) group, BHD (6420 mg/kg/d) group [Citation22], aspirin (100 mg/kg/d) group [Citation6], with seven animals in each group. Drugs were administered intragastrically once a day for 10 consecutive days, while the normal group and model group received the same volume of normal saline. Thirty minutes after the tenth drug administration, the rats in the normal group were subcutaneously injected with normal saline, while the other rats were subcutaneously injected with adrenaline (0.8 mg/kg). After a period of 2 h, the rats except those in the normal group, were kept in ice-cold water (0-4 °C) for 5 min, and then re-injected with adrenaline subcutaneously (0.8 mg/kg) 2 h later [Citation8]. After the re-injection, all the rats were fasted for 12 h before given the last drug administration.
Collection of blood samples and detection of biochemical indexes
Rats were anesthetized with 10% chloral hydrate (3.5 mL/kg) one hour after the last drug administration and blood was drawn from the abdominal aorta. One part of the blood was collected into plastic tubes with 3.2% sodium citrate (citrate/blood: 1/9, v/v) for the whole blood viscosity (WBV), plasma viscosity (PV), activated partial thromboplastin time (APTT), prothrombin time (PT) and fibrinogen (FIB) measurements. LBY-N6B was used to detect WBV at 5 s−1, 30 s−1, 50 s−1, 150 s−1, and 200 s−1 and PV at 120 s−1 shear rates. APTT, PT and FIB were examined by full-automatic blood coagulation analyzer (Sysmex, CA-510). Plasma was separated from blood by centrifugation at 3820 r/min for 15 min. One part of the blood was used to detect the total antioxidant capacity (T-AOC), superoxide dismutase (SOD), malonaldehyde (MDA), alanine transaminase (ALT), aspartate transaminase (AST), interleukin-1β (IL-1β), interleukin-6 (IL-6), platelet activating factor (PAF). Serum was separated from blood by centrifugation at 2000 g for 15 min. All the above serum biochemical indices were measured and quantified by kits (Nanjing Jiancheng Bio-engineering Institute, Nanjing, China) according to the manufacturer’s instructions.
Statistical analysis
Data were presented as mean values with standard deviation (±SD). One-way analysis of variance (ANOVA), Student’s t-test and Dunnett’s multiple comparisons were used to compare the results among groups. Statistical analysis was carried out with SPSS (Version: 21.0). Differences were considered statistically significant at p < 0.05 or p < 0.01.
Results and discussion
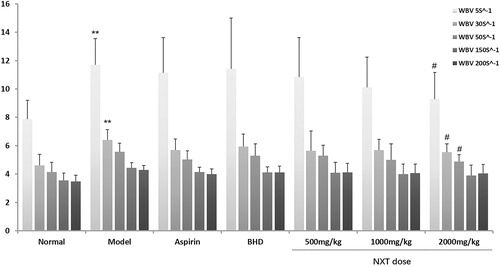
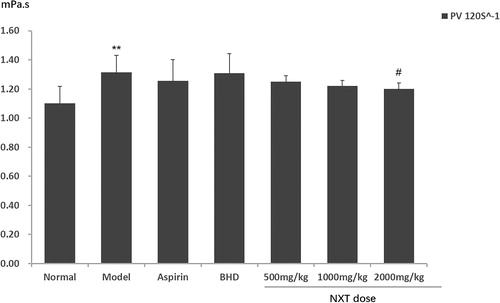
Effect of treatments on WBV and PV
For the diagnosis of CVD and evaluation of the drugs in promoting blood circulation, haemorheological parameters are commonly detected in clinic. As an essential observed index in hemorheology, WBV is the reflection of intrinsic resistance of blood to flow in vessels and increased blood viscosity is associated with cardiovascular events [Citation24]. In this study, WBV significantly increased at all shear rates in the model group (p < 0.01), suggesting that blood stasis appeared in the model rats. After administration, aspirin and BHD had no significant effects on WBV. The high dose of NXT caused statistical decrease in WBV at low shear rates (p < 0.05) (). Since WBV at low shear rates reflected red blood cell aggregation [Citation25], the results indicated that NXT had significant effect on the suppression of red blood cell aggregation. The apparent viscosity of blood is determined not only by RBCs but also by PV, which mainly depends on the type and concentration of proteins in plasma [Citation8]. Our results showed that PV was significantly decreased in the high dose of the NXT group (p < 0.05) (), indicating that the regulation on the plasma proteins might be one way that NXT works in decreasing the blood viscosity. The results were consistent with the clinical experimental results of Li et al. [Citation26], who demonstrated that NXT could significantly affect haemorheological parameters, including a decrease in WBV and PV.
Effect of treatments on blood coagulation
Blood coagulation plays an essential role in the development of CVD. In general, blood stasis is associated with an abnormal clotting function. PT, APTT and FIB are three parameters widely used for blood clotting function test. PT reflects the overall efficiency of extrinsic coagulation pathway, and a prolonged PT indicates a deficiency in coagulation factors V, VII and X or the presence of inhibitors of coagulation. APTT is used to evaluate the intrinsic clotting pathway, and a prolonged APTT represents a deficiency in factors VIII, IX, XI, XII and Von Willebrand’s factor. In short, a prolonged PT or APPT indicates a deficiency in coagulation factors or the presence of inhibitors of coagulation [Citation27]. In this study, the three doses of NXT significantly prolonged PT (p < 0.05, p < 0.05, p < 0.01) and the intermediate- and high-dose of NXT significantly prolonged APTT (p < 0.01), while BHD showed no significant effects (). The results indicated that NXT might have stronger effect on the suppression of both intrinsic and extrinsic blood coagulation activity than BHD. Plasma Fbg is an important component of the coagulation cascade, as well as a major determinant of blood viscosity and blood flow. High FIB levels are associated with atherosclerosis and thrombotic complications [Citation28, Citation29]. In the present study, the FIB coagulation time was measured. The shorter the coagulation time was observed, the higher the FIB level was. As shown in , compared with the model group, a longer FIB coagulation time was observed in the aspirin group (p < 0.05), intermediate- and high-dose NXT group (p < 0.01). In other words, both aspirin and NXT significantly decreased the FIB level. These results indicated that NXT had positive effects on the regulation of blood coagulation activity.
Figure 3. Effects of NXT on prothrombin time (PT), activated partial thromboplastin time (APTT) and fibrinogen (FIB) in the rat blood stasis model.
Note: Data are presented as means ± SD (n = 7). *P < 0.05, **P < 0.01 compared with the normal group, #P < 0.05, ##P < 0.01 compared with the model group.

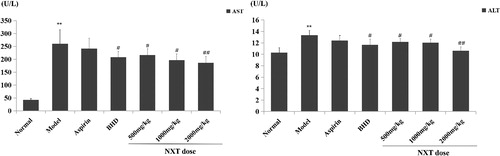
Effect of treatments on liver function
Liver function is closely related to CVD because lipid metabolism and kinds of clotting factor’s generation take place in the liver. Blood stasis can reduce the blood flow of the liver, further inhibit pathogen clearance, and result in hepatic inflammation aggravation or fibrosis-related injury [Citation30]. Hence, the drugs that activate blood circulation to remove blood stasis are often useful to protect liver. ALT and AST are commonly used indices and their levels in the serum will increase rapidly once the liver cells undergo degeneration and necrosis. In the model group, ALT and AST significantly increased compared to the normal group (p < 0.01, p < 0.01) (), which suggested that the model rats exhibited liver damage. After drug treatment, BHD and NXT produced significant decrease in the AST and ALT levels (p < 0.05, p < 0.01), while aspirin had no effects. This result indicated that BHD and NXT could inhibit the liver injury caused by blood stasis. This result is partly consistent with Yang et al.’s report that NXT could ameliorate atorvastatin-induced hepatic inflammation [Citation31], indicating that NXT possessed a liver protection function.
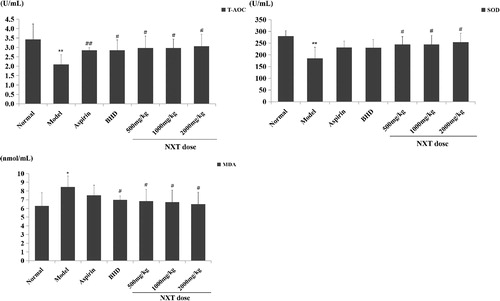
Effect of treatments on oxidative stress
Blood stasis is a complex pathological system accompanied by free radical accumulation [Citation3]. Under pathological conditions, excessive reactive oxygen species (ROS) may promote the growth and migration of inflammatory cells and vascular smooth muscle cells. Meanwhile, it promotes the formation of atherosclerotic plaques, which result in increased risk for the development of CVD. In this study, the influence of NXT on oxidative stress in rats was evaluated by T-AOC, SOD and MDA at the pharmacodynamics level. The level of T-AOC reflects the ability of the body’s antioxidant defense system to resist oxidative damage. SOD is a key enzyme which protects the body from superoxide radicals. The level of MDA, an end-product of lipid peroxidation, reflects the degree of lipid peroxidation injury and indirectly reflects the extent of cellular damage [Citation32]. In the present study, the level of MDA in the model group was significantly higher than that in the control group (p < 0.05), while the levels of T-AOC and SOD in the model group were significantly lower than those in the control group (p < 0.01, p < 0.01), indicating that oxidative damage occurred in the model rats. After administration, the three doses of NXT significantly reduced the content of MDA and increased the activity of SOD and the level of T-AOC (p < 0.05) (). The results are in line with Zhang et al. [Citation33], who showed that NXT exhibited strong protective effects on H9c2 cardiomyoblasts from H2O2-induced oxidative injury by increasing T-AOC, T-SOD levels and decreasing the level of MDA. Our data showed that NXT in vivo also was associated with stimulated antioxidant activities such that it can significantly alleviate the oxidative damage.
Effect of treatments on inflammation
Inflammation is involved in all stages of the cardiovascular disease and has suggested new targets in preventing cardiovascular disease. Evidence has indicated that the substances formed in the process of blood stasis can cause inflammation [Citation34]. Inflammatory mediators and cytokines could promote plaque formation and further lead to atherosclerosis. IL-1β can promote the expression of endothelial leukocyte adhesion molecule and stimulate the migration of inflammatory cells into the lesion site [Citation35]. IL-6 in the vessel wall can activate autocrine and paracrine secretion of monocytes contributing to the deposition of fibrinogen, thus result in the increased blood viscosity, platelet number and activity [Citation36]. As shown in , the contents of IL-1β and IL-6 significantly increased in the model group compared with the control group (p < 0.01), suggesting that the model rats had excessive inflammation. Aspirin and BHD showed significant effects on decreasing IL-1β and IL-6 levels (p < 0.05, p < 0.01). In the groups with the three doses of NXT, the IL-1β and IL-6 levels were significant lower compared with the model group (p < 0.05, p < 0.01) (), indicating that administration of NXT was associated with inhibition of inflammation. This may be one of the mechanisms of anti-CVD of NXT.
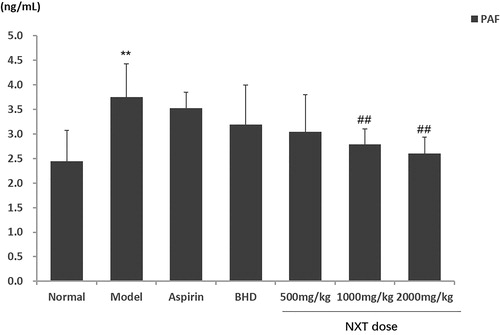
Effect of treatments on PAF
PAF is an endogenous phospholipid participating in a wide range of pathophysiological conditions of cardiovascular disease [Citation37]. Recently, an increasing number of studies have proved that PAF is closely associated with diseases with blood stasis syndrome [Citation38]. It has been found that PAF can promote platelet aggregation, increase capillary permeability, stimulate the production of inflammatory mediators and vasoactive substances, and further lead to the damage to tissues [Citation39]. At present, little research has been done on the effect of NXT on PAF. In this study, the level of PAF significantly increased in the model group compared with the normal group (p < 0.01), suggesting that platelet aggregation might increase. As shown in , the intermediate- and high-dose of NXT led to a significant reduction of PAF level (p < 0.01), while BHD and aspirin showed no effects. This result could contribute to understanding the mechanism of the anti-thrombotic action of NXT. The aspirin group showed no significant difference compared with the model group, probably because aspirin inhibits platelet aggregation by inactivating cyclooxygenase rather than reducing PAF.
Figure 7. Effects of NXT on platelet activating factor (PAF) in the rat blood stasis model.
Note: Data are presented as means ± SD (n = 7). **P < 0.01 compared with the normal group, ##P < 0.01 compared with the model group.
In the present study, based on “cold pathogen” and “fury” in the etiology of qi-stagnation and blood stasis syndrome in TCM theory, ice-water bath and adrenaline were used to copy the classical rat model of blood stasis [Citation3, Citation40]. Previous studies have proved that this model showed abnormalities in blood rheology and coagulation function, which can reproduce the blood stasis syndrome [Citation5, Citation40]. The present study found that the blood stasis rats were abnormal in oxidative stress, inflammatory response, liver function and platelet aggregation. Recently, an increasing number of studies demonstrates the effect enhancement of NXT when it combined with aspirin and clopidogrel [Citation41, Citation42], while its effective characteristics are seldom studied. Our study showed that NXT had significant effects in improving many aspects of pathological indices in vivo, including hemorheology, coagulation function, inflammation, liver function and oxidative stress. Aspirin, one of antiplatelet agents, is widely used in preventing cardiovascular thrombotic diseases in clinic and thus it was selected as a positive control. BHD is a classic formula for activating blood circulation and removing stasis. And, NXT is developed from BHD, whereas few studies focus on the therapeutic difference between these two Chinese medicines, thus BHD was selected as another positive control. The present study showed that the effect of NXT on the coagulation function and inflammation was as good as that of aspirin. NXT was superior to aspirin in oxidative stress improvement and in reducing PAF. In addition, the data showed that NXT was more effective than BHD in decreasing the blood viscosity, improving the coagulation function and reducing PAF. NXT and BHD had similar effects in the improvement of liver function, inflammation and oxidative stress. In general, NXT, BHD and aspirin all had respective advantages in rats with blood stasis syndrome.
Thousands of years of clinical practice in TCM have accumulated a number of formulas that exhibit reliable efficacy and safety in vivo [Citation43]. NXT is a complex prescription for patients with coronary heart disease and stroke caused by obstruction of blood stasis and is used under the guidance of TCM theory [Citation44, Citation45]. It should be pointed out that the pharmacological mechanism and targets of NXT are not clear yet because its composition is too complex. However, the present study makes contribution to evaluating the pharmacodynamic effects of NXT in rats with blood stasis, providing a foundation for further research, especially the follow-up studies on the mechanism. What is more, the study may provide scientific experimental evidence for the clinical application of NXT.
Conclusions
In conclusion, this study expounds the pharmacodynamic profile of NXT on rats with blood stasis syndrome from several systems. The findings demonstrate that NXT can perform good effects on improving blood coagulation, suppressing inflammatory response and enhancing the antioxidant capacity. The prevention and treatment of CVD by NXT might partly be related to the above pharmacodynamics effects.
Data availability statement
The data that support the findings of this study are available from the corresponding author, H.L., upon reasonable request.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Luepker RV, Lakshminarayan K, Detels R, et al. Oxford textbook of public health. Vol. the practice of public health. Oxford: Oxford University Press; 2009. (Cardiovascular and cerebrovascular diseases).
- Dan B, Clavey S, Stoger E, et al. Materia medica: chinese herbal medicine. Seattle (WA): Eastland Press; 2004.
- Bi C, Li PL, Liao Y, et al. Pharmacodynamic effects of Dan-hong injection in rats with blood stasis syndrome. Biomed Pharmacother. 2019;118(2019):109187.
- Zhao X, Zhang Y, Meng X, et al. Effect of a traditional Chinese medicine preparation Xindi soft capsule on rat model of acute blood stasis: a urinary metabonomics study based on liquid chromatography-mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2008;873(2):151–158.
- Liu H, Zhang WJ, Long CF, et al. Protective effects of traditional Chinese herbal formula Compound Xueshuantong Capsule (CXC) on rats with blood circulation disorders. Biotechnol Biotechnol Equip. 2017;31(4):1–9.
- Liu H, Peng YY, Liang FY, et al. Protective effects of traditional Chinese medicine formula NaoShuanTong Capsule on haemorheology and cerebral energy metabolism disorders in rats with blood stasis. Biotechnol Biotechnol Equip. 2014;28(1):140–146.
- Wang J, Chu FY, Li J, et al. Study on syndrome element characteristics and its correlation with coronary angiography in 324 patients with coronary heart disease. Chin J Integr Med. 2008;14(4):274–280.
- Li HX, Han SY, Wang XW, et al. Effect of the carthamins yellow from Carthamus tinctorius L. on hemorheological disorders of blood stasis in rats. Food Chem Toxicol. 2009;47(8):1797–1802.
- Liu P, Shu-Lan SU, Zhou W, et al. Evaluating Effects of Xiangfu Siwu Decoction and Siwu Decoction on Hemorheological Indexes and Ovarian Function in Rat Model of Acute Blood Stasis. Chin J Integr Med. 2010;16(8):124–127.
- Wang S, Liu Y. Activating blood circulation to dissipate blood stasis effect and anti-hypoxia effect of Salviae Miltiorrhizae Liguspyragine Hydrochloride and Glucose injection. Mod J Integr Tradit Chin West Med. 2014;23:358–362.
- Zhang JH, Huang XL, Huang HB, et al. Effects of compound Xueshuantong dripping-pill on the hemorrheology in blood stasis rats and the clotting-time of mice. Chin Pharm J. 2004;39(5):350–352.
- Thrall G, Lip GYH. Haemoconcentration and the hypercoagulable state associated with mental stress. Thromb Res. 2005;115(3):171–173.
- He Y, Wan H, Du Y, et al. Protective effect of Danhong injection on cerebral ischemia-reperfusion injury in rats. J Ethnopharmacol. 2012;144(2):387–394.
- Wang PR, Wang JS, Zhang C, et al. Huang-Lian-Jie-Du-Decotion induced protective autophagy against the injury of cerebral ischemia/reperfusion via MAPK-mTOR signaling pathway. J Ethnopharmacol. 2013;149(1):270–280.
- Li JH, Liu AJ, Li HQ, et al. Buyang huanwu decoction for healthcare: evidence-based theoretical interpretations of treating different diseases with the same method and target of vascularity. Evid Based Complement Alternat Med. 2014;2014:506783.
- Guo Q, Zhong M, Mao X, et al. A systems biology perspective on the molecular mechanisms underlying the therapeutic effects of Buyang Huanwu Decoction on ischemic stroke. Rejuvenation Res. 2015;18(4):313–325.
- Wan J, Song J, Xu Y. Clinical effect of Naoxintong Capsule on treatment of lipid and carotid atherosclerosis plaques in patients with cerebral infarction. World Chin Med. 2012;7(4):299–301.
- Zheng Y, Zhang Y, Li C, et al. Antithrombotic treatment with Naoxintong Capsule for the patients underg oing percutaneous coronary intervention: a clinical research on 27 cases. J Tradit Chin Med. 2012;53(4):299–303.
- Zhao J, Zhu H, Wang S, et al. Naoxintong protects against atherosclerosis through lipid-lowering and inhibiting maturation of dendritic cells in LDL receptor knockout mice fed a high-fat diet. Curr Pharm Des. 2013; 19(33):5891–5896.
- Zhong XN, Wang HH, Lu ZQ, et al. Effects of Naoxintong on atherosclerosis and inducible nitric oxide synthase expression in atherosclerotic rabbit. Chinese Med J. 2013; 126(6):1166–1170.
- Zhang WJ, Su WW, Li PB, et al. Naoxintong Capsule inhibits the development of cardiovascular pathological changes in Bama Minipig through improving gut microbiota. Front Pharmacol. 2019;10(10):1128.
- Zhang H, Wang WR, Lin R, et al. Buyang Huanwu decoction ameliorates coronary heart disease with Qi deficiency and blood stasis syndrome by reducing CRP and CD40 in rats. J Ethnopharmacol. 2010;130(1):98–102.
- Wang QY, Guo H, Zhao BC, et al. Effects of Naoxintong Capsule on permeability of the blood brain barrier in focal cerebral ischemia—reperfusion in rats. Chin J Clin Pharmacol. 2016;32(10):890–893.
- Song SH, Kim JH, Lee JH, et al. Elevated blood viscosity is associated with cerebral small vessel disease in patients with acute ischemic stroke. BMC Neurol. 2017;17(1):20.
- Wen Z, Yao W, Xie L, et al. Influence of neuraminidase on the characteristics of microrheology of red blood cells. Clin Hemorheol Microcirc. 2000;23(1):51–57.
- Li XC, Zhao DM, Xiang AL. Effects of Naoxintong Capsules on hemorheology and coagulation function in patients with acute cerebral infarction. China Pharm. 2014;28(1):2623–2625.
- Chan KC, Yin MC, Chao WJ. Effect of diallyl trisulfide-rich garlic oil on blood coagulation and plasma activity of anticoagulation factors in rats. Food Chem Toxicol. 2007;45(3):502–507.
- Ahmed M, Chowdhury NA, Sofdar G, et al. High fibrinogen level is an independent predictor of presence and severity of coronary artery disease. Cardiovasc J. 2014;7(1):4–10.
- de Moerloose P, Boehlen F, Neerman-Arbez M. Neerman-Arbez M. Fibrinogen and the risk of thrombosis. Semin Thromb Hemost. 2010;36(1):7–17.
- Lieming XU. Resolving blood stasis to improve liver microcirculation and treat chronic liver diseases. J. Clin. Hepatol. 2013; 29(4):257–263.
- Yang X, Li Y, Sun L. NaoXinTong enhances atorvastatin-induced plaque stability while ameliorating atorvastatin-induced hepatic inflammation. J Cardiovasc Pharm. 2016; 69(1):55–64.
- Parameshwaran K, Irwin MH, Steliou K, et al. D-Galactose effectiveness in modeling aging and therapeutic antioxidant treatment in mice. Rejuvenation Res. 2010;13(6):729–735.
- Zhang F, Huang B, Zhao Y, et al. BNC Protects H9c2 cardiomyoblasts from H 2 O 2 -induced oxidative injury through ERK1/2 signaling pathway . Evid Based Complement Alternat Med. 2013;2013:802784 [2013 Sep 09];
- Ma XJ, Yin HJ, Chen KJ. Research progress of correlation between blood-stasis syndrome and inflammation. Chin J Integrated Tradit Western Med. 2007; 27(7):669–672.
- Zhu H, Lin X, Zheng P, et al. Inflammatory cytokine levels in patients with periodontitis and/or coronary heart disease. Int J Clin Exp Pathol. 2015; 8(2):2214–2220.
- Yudkin JS, Kumari M, Humphries SE, et al. Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis. 2000; 148(2):209–214.
- Palur Ramakrishnan AV, Varghese TP, Vanapalli S, et al. Platelet activating factor: a potential biomarker in acute coronary syndrome? Cardiovasc Ther. 2017;35(1):64–70.
- Luo LJ, Zhu MZ, Wang H, et al. Research on correlation between sublingual venae characteristic of blood stasis syndrome and serum PAF and vegf expressions in patients with ischemic stroke. Liaoning J Tradit Chin Med. 2018; 45(2):248–251.
- Paraskevi D, Tzortzis N, Elizabeth F, et al. Platelet activating factor in heart failure: potential role in disease progression and novel target for therapy. Curr Heart Fail Rep. 2013; 10(2):122–129.
- Li P, Su W, Yun S, et al. Toward a scientific understanding of the effectiveness, material basis and prescription compatibility of a Chinese herbal formula Dan-hong injection. Sci Rep. 2017;7:46266.
- Chen DK, Zhang HQ, Zhang JH. Intervening effect of Naoxintong on anti-platelet treatment with aspirin. Chin J Integr Med. 2008;28(9):843–846.
- Chen H, Wu XY, Wu HX, et al. A randomized controlled trial of adjunctive Bunchang Naoxintong Capsule versus maintenance dose clopidogrel in patients with CYP2C19*2 polymorphism. Chin J Integr Med. 2014;20(12):894–902.
- Zhao J, Nagle DG, Zhou YD, et al. Network Pharmacology in the study of TCM formulae. In: Zhang WD, editor. Systems biology and its application in TCM formulas research. Vol. 4. New York: Academic Press; 2018. p. 69–95.
- Liang QE, Cai YF, Chen RX, et al. The effect of Naoxintong Capsule in the treatment of patients with cerebral infarction and carotid atherosclerosis: a systematic review and meta-analysis of randomized trials. Evid Based Complement Alternat Med. 2018;2018:1–9.
- Liu LT. Chinese Experts Consensus on Clinical Application of Naoxintong Capsule [脑心通胶囊]. Chin J Integr Med. 2018;24(3):232–236.