Abstract
Targeted therapy with tyrosine kinase inhibitors (TKIs) was introduced for the suppression of BCR-ABL fusion protein in chronic myelogenic leukemia (CML) more than 50 years ago. The introduction of TKI was an elegant way to gain control over the disease and opened a horizon to the development of new and safer drugs to better manage the disease progression in CML patients. Although Imatinib (the first TKI) was highly effective for the treatment of CML, the lack of response in some patients and the development of resistance led to the introduction of a second-generation TKI, like Nilotinib (Tasigna®). This study aimed to show the molecular response to Nilotinib after a long-term monitoring of CML patients. We analyzed the molecular response rate of twenty-seven CML patients admitted to the Hematology Ward. All of them were subjected to multiple control measurements of Philadelphia chromosome once in at least three months’ period between January 2017 and March 2020. All patients showed a remarkable decrease in the level of the fusion gene’s expression. The highest drop in the expression level was detected after the first dose admission. Some of the patients even reached an expression of BCR-ABL below the detection limit and it was maintained stably low during further examinations. In our patients with CML, Nilotinib resulted in prolonged and deep molecular response. The expression level of BCR-ABL fusion gene showed a substantial decrease immediately after Nilotinib treatment, revealed as early as the third month of therapy.
Introduction
Imatinib resistance is present in approximately 50% of patients with chronic myelogenic leukemia (CML), which could be due to mutations in BCR-ABL kinase domain [Citation1–3]. Currently, about one third of patients with CML in chronic phase experience an unsatisfactory therapeutic effect with Imatinib [Citation4, Citation5]. The main disadvantages of Imatinib treatment of CML – the occurrence of resistance and lack of response in some patients – were meant to be overcome with the introduction of a second-generation tyrosine kinase inhibitor (TKI).
Nilotinib (Tasigna®) was approved in 2007 for Philadelphia positive (Ph+) CML cases as a more potent and highly effective TKI revealing better effects as a first-line treatment of CML [Citation6]. The long-term aim of targeted treatment is to maintain/stabilize the disease in the chronic phase before it progresses to the accelerated phase and blast crisis which will eventually lead to a critical decrease in the survival time of only several months [Citation7]. That is why Nilotinib is applied generally in adults who are CML resistant and/or intolerant to Imatinib therapy [Citation8]. According to reported data, it is 20–30 times more potent [Citation9] and generally well tolerated with manageable adverse events [Citation10]. However, Nilotinib is associated with a reduction in some biochemical parameters, such as magnesium and phosphate, and elevation in serum lipase, glucose and bilirubin [Citation11]. Approximately half of patients on second-line TKI therapy will have incomplete suppression of the Ph + clone in the bone marrow, usually without evidence of overt disease progression [Citation2]. That is why it is so important to monitor those patients at regular time intervals. Eghtedar et al. [Citation12] reported that, after a median follow-up of 23 months, 21% of all treated with nilotinib (117 individuals) discontinued therapy. The most common reasons for that were toxicity; resistance in chronic phase; transformation to blast crisis [Citation12]. Nevertheless, a significant number of patients who discontinue initial therapy with second-generation TKIs (dasatinib, nilotinib) because of personal preferences or toxicity are already in chronic phase and most probably have a favorable outcome. Very few of the patients discontinue because of resistance and for those SCT or another TKI is offered as a treatment option [Citation12, Citation13].
Our aim in this study was to evaluate the molecular response of patients in chronic phase of CML while representing/evaluating the results of their molecular genetic tests performed at the Clinic of Hematology, University Hospital “St.Ivan Rilski” (Sofia, Bulgaria) for the period from January 2017 to March 2020.
Subjects and methods
Ethics statement
All patients signed a written informed consent form to participate in the study.
Selection of patients
Altogether 27 CML patients were selected for genetic analysis. Their therapeutic regimes included treatment with Nilotinib (second-generation TKI) at a dose of 600 mg daily as a first-line therapy. All monitored patients were in chronic phase of CML, which had been confirmed previously (upon their first admission to the Clinic of Hematology). Their molecular tests were subsequently repeated to monitor the level of the BCR-ABL transcript and estimate their molecular-genetic progress. Results with at least two following measurements of the fusion gene for a total period of four months were included for statistical analysis. Five patients met these minimum criteria, the other twenty-two patients underwent molecular genetic tests between three and six times for an average period of 15.5 months (7–32 months) (). Patients in acute phase of CML; with only one molecular-genetic measurement and/or a total monitoring period of less than four months were not considered in this study.
Table 1. Number of molecular-genetics monitoring tests and total monitoring period for the patients included in the study.
Molecular-genetic analysis
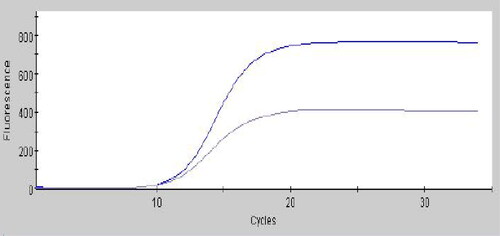
For all patients the molecular response was assayed based on the expression level of BCR-ABL mRNA in peripheral blood samples taken in K2 EDTA collection tubes. The test was carried out upon admission of each patient at the Clinic of Hematology and subsequently, at least at three months’ intervals as a control monitoring test. Quantitative results were first normalized against a reference gene such as ABL [Citation14]. The level of mRNA transcripts of ABL were used as an endogenous control. The test was performed automatically by Cepheid GeneXpert® platform (RNA isolation and quantification are performed in the GeneExpert cassette) and the result was given as a %BCR-ABL/ABL (IS) as previously described [Citation15, Citation16]. The efficiency value of each test is embedded in the barcode of the Xpert BCR-ABL Ultra cartridge and the scaling factor is lot-specific (). The difference between the BCR-ABL Ct and ABL Ct (ΔCt) represents the ratio of the two populations of mRNAs and ultimately the fraction of neoplastic cells present [Citation17].
Results
Fifteen of our patients with CML (55.6%) reached MMR (Major Molecular Response) (BCR-ABL<0.1%) upon their second molecular test. MR4.0 (Molecular Response) (<0.01%) was achieved in 16 patients (59.3%) at the average time of nine months following treatment. MR4.5 (<0.0032%) was estimated only in patients who were tested at least three times following initial diagnosis (22 patients). In 14 patients (63.6%) altogether MR4.5 was achieved at approximately 9.5 months after the initiation of Nilotinib treatment.
Estimating the general distribution of the BCR-ABL expression percentage, neither of the monitored individuals (except one) had reversed to values higher than the results from the previous molecular test (). Thirteen individuals reached a negative value of the fusion gene expression (48.1%).
Table 2. Expression levels of BCR-ABL mRNA (given in %IS) of all 27 patients per month for the whole monitoring period January, 2017 to March, 2020.
Generally, the expression level substantially dropped down after the first application of the drug. The level of BCR-ABL transcripts showed a decrease immediately after Nilotinib treatment, revealed at the third month’s visit of the patient.
Discussion
The diagnosis of CML is traditionally made either by standard karyotyping techniques or fluorescence in situ hybridization (FISH). As a Ph chromosome cannot be detected in approximately 5% of cases, we used real-time polymerase chain reaction to detect the BCR-ABL gene [Citation2]. It is a more sensitive alternative and provides a quantification of the relative amount of BCR-ABL mRNA in the peripheral blood [Citation2]. The results for each individual patient are expressed as a ratio of BCR-ABL transcript copies to control gene copies and could be possibly converted to an international standard unit [Citation18]. Regular measurement of the BCR-ABL transcript levels could be potentially used for frequent monitoring of CML patients even if it may not fully overlap with the patient’s response to treatment [Citation19]. Therefore, we used BCR-ABL mRNA transcript levels expressed in %(IS) as a marker for molecular response in patients. We accepted the complete absence of transcripts (negative result) for a CMR (Complete Molecular Response), and a reduction of 0.1% [BCR-ABL1 on the international scale (IS) <0.1%], for a MMR (Major Molecular Response) [Citation18]. MR 4.0-log reduction from a standardized baseline (MR4.0; BCR-ABL1 <0.01% IS) and MR 4.5-log reduction from a standardized baseline (MR4.5; BCR-ABL1 <0.0032% IS) were also assessed [Citation20]. The early trend in the BCR-ABL/ABL ratio may be clinically useful for the early identification of patients who respond poorly to imatinib treatment [Citation21]. Patients with an EMR (Early Molecular Response) are supposed to have a superior outcome and may continue on therapy, with regular monitoring by real-time PCR. They usually present with a much lower disease burden which makes them more suitable for conventional non-transplant therapy [Citation21]. In the NOVEL study, at 3 months, 20 out of 27 patients achieved EMR (BCR-ABL1<10% IS) [Citation10]. In a study from 2016 Nilotinib resulted in higher rates of early molecular response [Citation22]. In accordance with those results we achieved even higher rates of EMR. In our cohort, 25 out of our 27 patients (93%) presented with BCR-ABL1<10% IS ().
In the same study [Citation22] at 3 months’ time more than half of all patients on Nilotinib achieved a molecular response 4.5. According to Kuo et al. [Citation10], 36.5% of the patients discontinued Nilotinib treatment due to an unsatisfactory therapeutic effect. The cumulative MMR rate by 3 months was estimated to 11.9%, and none of the patients achieved MR4.0 or MR4.5. By 24 months, 56.8% achieved MMR, 16.2% MR4.0 and 7.4% MR4.5 [Citation10]. In our study, 15 of our patients (55.6%) with CML reached MMR (BCR-ABL<0.1%) upon their second molecular test. MR4.0 (<0.01%) was achieved in 16 patients (59.3%) at the average time of nine months following treatment. MR4.5 (<0.0032%) was estimated only in patients who had had the test done at least three times following initial diagnosis (22 patients). Therefore, in our study, MR4.0 and MR4.5 was detected at higher levels compared to the NOVEL study. Similarly to earlier studies [Citation22], 55.6% of our patients (out of 27) with CML reached MMR (BCR-ABL<0.1%) upon their second molecular test. Altogether MR4.5 was achieved at approximately 9.5 months after initiation of Nilotinib treatment in 63.6% of patients.
Although the Cepheid System is very sensitive in estimating the expression level of the fusion gene, the negative result could indicate a very low number of the gene transcripts rather than a complete absence of such (). That is why some laboratories consider an increase of 0.5 log to be insignificant [Citation18]. Nevertheless, the system demonstrates low inter-laboratory variation and clinically demonstrated limit of detection of <4.5-log reduction (0.0032%) [Citation23] and proves adequate for the identification of leukemia cells harboring the BCR-ABL gene fusion from blood samples. In our study, 13 individuals reached a negative value of the fusion gene expression (). That should be interpreted as a very low amount of the Ph(+) cells below the detection limit of the machine and not complete eradication of the mutational transcripts. This can be confirmed by the subsequent results in those patients as the values return to the detection range of the device. As a whole, in all 27 patients there was a stable decrease in the amount of the expressed transcript, which was maintained from the third month’s measurement on.
Conclusions
In this study the treatment with Nilotinib was well-tolerated and proved effective in achieving molecular response in patients with chronic phase of CML monitored at the Clinic of Hematology at “St.Ivan Rilski” Hospital, Sofia, Bulgaria.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability
All data (anonymized) that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Branford S, Hughes T. Detection of BCR-ABL mutations and resistance to imatinib mesylate. Methods Mol Med. 2006;125:93–106.
- Assouline S, Lipton JH. Monitoring response and resistance to treatment in chronic myeloid leukemia. Curr Oncol. 2011;18(2):e71–e83.
- Hochhaus A, Krei S, Corbin AS, et al. Molecular and chromosomal mechanisms of resistance to imatinib (STI571) therapy. Leukemia. 2002;16(11):2190–2196.
- Druker BJ, Guilhot F, O’Brien SG, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355(23):2408–2417.
- de Lavallade H, Apperley JF, Khorashad JS, et al. Imatinib for newly diagnosed patients with chronic myeloid leukemia: incidence of sustained responses in an intention-to-treat analysis. J Clin Oncol. 2008;26(20):3358–3363.
- Blay JY, von Mehren M. Nilotinib: a novel, selective tyrosine kinase inhibitor. Semin Oncol. 2011;38 Suppl 1(Suppl 1(0 1):S3–S9.
- Kantarjian H, Talpaz M, O’Brien S, et al. Survival benefit with imatinib mesylate therapy in patients with accelerated-phase chronic myelogenous leukemia–comparison with historic experience. Cancer. 2005;103(10):2099–2108.
- Weisberg E, Manley P, Mestan J, et al. AMN107 (nilotinib): a novel and selective inhibitor of BCR-ABL. Br J Cancer. 2006;94(12):1765–1769.
- O’Hare T, Walters DK, Stoffregen EP, et al. In vitro activity of Bcr-Abl inhibitors AMN107 and BMS-354825 against clinically relevant imatinib-resistant Abl kinase domain mutants. Cancer Res. 2005;65(11):4500–4505.
- Kuo CY, Wang PN, Hwang WL, et al. Safety and efficacy of nilotinib in routine clinical practice in patients with chronic myeloid leukemia in chronic or accelerated phase with resistance or intolerance to imatinib: results from the NOVEL study. Ther Adv Hematol. 2018;9(3):65–78.
- Kantarjian HM, Giles F, Gattermann N, et al. Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood. 2007;110(10):3540–3546.
- Eghtedar A, Kantarjian HJ, O’Brien E, et al. Outcome after failure of second generation tyrosine kinase inhibitors treatment as first-line therapy for patients with chronic myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2013;13(4):477–484.
- Hochhaus A, Saglio M, García-Gutiérrez G, et al. Expert opinion-management of chronic myeloid leukemia after resistance to second-generation tyrosine kinase inhibitors . Leukemia. 2020;34(6):1495–1502.
- Beillard E, Pallisgaard N, van der Velden VH, et al. Evaluation of candidate control genes for diagnosis and residual disease detection in leukemic patients using ‘real-time’ quantitative reverse-transcriptase polymerase chain reaction (RQ-PCR) - a Europe against cancer program. Leukemia. 2003;17(12):2474–2486.
- Nikolova D, Damyanova V, Hrischev V, et al. Philadelphia-positive case negative for JAK2 V617F mutation with hyperdiploidic karyotype: a case report. Mol Clin Oncol. 2019;11(6):607–611.
- Branford S, Cross NC, Hochhaus A, et al. Rationale for the recommendations for harmonizing current methodology for detecting BCR-ABL transcripts in patients with chronic myeloid leukaemia. Leukemia. 2006; 20(11):1925–1930.
- Jobbagy Z, van Atta R, Murphy KM, et al. Evaluation of the Cepheid GeneXpert BCR-ABL assay. J Mol Diagn. 2007;9(2):220–227.
- Hughes T, Deininger M, Hochhaus A, et al. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors: review and recommendations for harmonizing current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108(1):28–37.
- Hughes T. ABL kinase inhibitor therapy for CML: baseline assessments and response monitoring. Hematology Am Soc Hematol Educ Program. 2006;2006(1):211–218.
- Larson RA, Hochhaus A, Hughes TP, et al. Nilotinib vs imatinib in patients with newly diagnosed Philadelphia chromosome-positive chronic myeloid leukemia in chronic phase: ENESTnd 3-year follow-up. Leukemia. 2012;26(10):2197–2203.
- Wang L, Pearson K, Ferguson JE, et al. The early molecular response to imatinib predicts cytogenetic and clinical outcome in chronic myeloid leukaemia. Br J Haematol. 2003;120(6):990–999.
- Hochhaus A, Saglio G, Hughes TP, et al. Long-term benefits and risks of frontline nilotinib vs imatinib for chronic myeloid leukemia in chronic phase: 5-year update of the randomized ENESTnd trial. Leukemia. 2016;30(5):1044–1054.
- Cepheid Xpert BCR-ABL Ultra Package Insert 301-2194. 2021.