Abstract
This study aims to evaluate clinical characteristics, quality of life and control of treatment and therapy satisfaction of patients with asthma in Bulgaria. A pilot study of Bulgarian patients with asthma selected by allergologists was performed. The predefined inclusion criteria were asthma diagnosis with at least 6 months of living with asthma and use of asthma medication. Patient characteristics, treatment, quality-of-life, control of asthma and therapy satisfaction were systematically assessed. A retrospective observational study was conducted among asthma patients in Sofia in 2019. A strict definition of asthma-based solely on physicians’ diagnosis was used. Allergologists from two national reference hospitals for asthma therapy selected asthma patients. Every third patient with asthma that visited the office within 5 months period, and that agreed to participate was selected for the study. Quality-of-life of patients was measured using the EQ5D Assessment Test, control of asthma was assessed using ATCQ and ATC tests. A total of 71 asthma patients were enrolled. Approximately 43.6% were male, 16.9% were smokers, occupational risk factors were low (4.22%), 25% had moderate and 38% had severe asthma. The mean scores of asthma control treatment were 16.92 ± 5.68. The group has relatively high percentages of severe asthma patients. The asthma was not well controlled. National asthma strategies should focus on prevention and early detection of the disease.
Introduction
With the worldwide progression of the severity and prevalence of asthma, there is increasing need for assessment of patients’ quality of life and satisfaction of treatment. According to the published results, asthma is a common chronic disease that affects around 300 million people worldwide, and the patients suffering from allergic rhinitis are about 400 million [Citation1].
Estimates of the global prevalence of diagnosed asthma in adults suggest 4.3% (95% CI: 4.2; 4.4) according to the results from 70 participating countries from all over the world. The questions related to asthma diagnosis and respiratory symptoms received a total of 178,215 responses from adults and the results ranged from 0.2% in China to 21.0% in Australia [Citation2]. The mean prevalence of doctor diagnosed asthma for Europe is 5.1%, the prevalence of clinical asthma (doctor diagnosed asthma and/or a treatment for asthma) 5.28% and wheezing symptoms, 10.71% [Citation2].
The prevalence of asthma in Europe in young adults (18–45 years) also showed substantial geographical variation in the 1990s, from the European Community Respiratory Health Survey (ECRHS). The prevalence of asthma varied between 5.2% in Katowice, Poland to 16.8% in Coimbra, Portugal with the median prevalence of asthma in the 19 centers − 8.6% [Citation3].
The available information for Eastern Europe shows the prevalence of asthma in the range of 1.3–2.77%, mean value 2.5 [Citation2]. According to the same study, the prevalence rate of asthma in our neighboring countries was 6.6% for Greece, 2.06% for Turkey and 5.4% for North Macedonia [Citation2,Citation4].
There is no register for asthma patients in Bulgaria but according to expert’s opinion from Bulgarian Society of Lung Diseases, these patients are about 400,000 with only 50% of them being diagnosed [Citation5]. The only nationally representative investigation was published in 2000 with a sample size of 10,000 patients. The results showed that the prevalence of asthma was 4.7% for 20- to 44-year-old patients and 9.1% for patients under 18 years. The prevalence of allergic rhinitis was 15.8% [Citation6].
A prospective pre-/post-intervention study of a single cohort of 77 adult out-patients visiting specialist asthma clinics in Ghana was conducted in 2016 [Citation7]. The aim of the study was assessment of HRQoL and peak expiratory flow rates (PEFR) one month after pharmaceutical care intervention. The results showed that delivery of a structured pharmaceutical care led to a significant improvement in asthma specific quality of life and PEFR. The mean paired difference of the HRQoL for a cohort of patients with asthma post-pharmaceutical care intervention was 0.697(95% CI: 0.490–0.900) at t = 6.85 (p < .05). The mean paired difference for PEFR post intervention was 17.533 (95% CI: 2.876–32.190) at t = 2.384 (p = .02) [Citation7].
Another study conducted among 196 patients (mean age − 48 years) in Germany investigate factors associated with generic HRQOL in asthma patients [Citation8]. HRQOL was assessed by the Short Form 12 Health Survey Questionnaire (SF-12), which comprises a physical (PCS-12) and a mental component (MCS-12). In multivariable analysis, PCS-12 was negatively associated with older age, being female, insufficient disease control, higher number of medications in tablet form and reporting symptoms of depression. MCS-12 was negatively associated with being female, living alone, insufficient disease control and reporting symptoms of anxiety or depression. The authors suggest that focusing on disease control and screening for depression and anxiety may be promising approaches to improve HRQOL in adult asthma patients [Citation8].
A study reported implementation of an educational program for patients with asthma in Bulgaria [Citation9]. Patient’s health-related QOL and satisfaction with pharmacy services were assessed in the beginning and at the end of the survey. It was proved that the educational approach has a potential to decrease asthma disease complications [Citation9].
A recent survey in Spain among 600 asthma patients (200 with severe asthma and 400 with non-severe asthma) shows that despite the effective therapies currently available, a significant emotional burden and QoL impairment in patients with severe asthma are observed. Although both groups had a positive attitude to and extensive knowledge of asthma, significantly more patients with severe asthma were concerned about their disease and recognized that asthma has a detrimental effect on their daily life, social integration and overall QoL. Severe asthma patients have received complaints from employers due to workdays lost attributable to asthma, which suggests that a great effort is still needed to improve the levels of social awareness about chronic respiratory conditions such as asthma [Citation10].
Clark et al. [Citation11] performed a cross-sectional survey among patients with severe asthma in Australia. The survey had two components – the first one assessed the ‘outcome of importance’ using 17 statements related to outcomes that people with severe asthma would like treated as part of their severe asthma management. The second component was based on ‘treatment aspect preferences’, which included the presentation of hypothetical scenarios in which the participant was asked to consider multiple attributes within the scenario, and decide which medication best met their needs. The results show that the highest ranked treatment priorities were improvement in quality-of-life, reducing the number and severity of asthma attacks, increasing physically activity, OCS reduction and being less breathless. Quality-of-life was considered the most important outcome that people wanted to improve [Citation11].
Those studies show that asthma is a serious health problem which influenced both the patients and the community. This fact predisposed our interest toward evaluation of clinical characteristics and satisfaction of patients with asthma in Bulgaria because such studies are not available at a national level.
The study’s main goal was to analyze the impact of asthma treatment on the QoL and therapy satisfaction of patients with asthma in Bulgaria
Subjects and methods
Ethics statement
Every patient was acquainted with the study design, its purposes and their informed consent was obtained. Approval was obtained from Ethical Committee of the Medical University of Sofia.
Study design and patient recruitment
A retrospective observational study was conducted among asthma patients in Sofia in 2019. A strict definition of asthma-based solely on physicians’ diagnosis was used.
Asthma patients in Bulgaria are registered by allergologists and are followed-up at least twice per year, in case of emergencies the patients visit the physician’s office more frequently. Only allergologists are licensed to perform spirometry and change therapy. The patients’ general practitioners (GPs) follow allergologists treatment instructions without changing the therapy. We asked allergologists from two national reference hospitals for asthma therapy to select asthma patients. Every third patient with asthma that visited the office within 5 months period, and that agreed to participate was selected for the study. A sample size of 71 patients was chosen for this study.
Inclusion and exclusion criteria
Eligibility criteria were age over 18 years, a physician and spirometry-confirmed diagnosis according to FEV1, FVC and Tiffeneau–Pinelli index (FEV1/FVC ratio) dated six months ago and asthma pharmacotherapy prescriptions in the last six months. The main exclusion criteria were presence of other respiratory diseases, such as lung carcinoma, sarcoidosis, bronchiectasis, pulmonary fibrosis, pulmonary tuberculosis or chronic obstructive pulmonary disease.
Characteristics, risk factors and clinical outcomes
Collected data included demographic characteristics (age, gender); smoking status (non, former or current smoker); occupational status; clinical data (duration, spirometry (FEV1, FVC and Tiffeneau–Pinelli index)) asthma status based on airflow limitation and a retrospective assessment of the level of treatment required to control symptoms and exacerbations (moderate, severe, very severe asthma); pharmacotherapy (for 2018 and 2019); comorbidity and co-medication; healthcare resource utilization (GP visits, specialists’ visits, hospitalizations); disability; days off work due to asthma).
Quality-of-life of patients was measured using the EQ5D Assessment Test where a best health state is described whit score 1 in EQ5D test. The patients were asked to answer to the questions of Asthma treatment quality control (ATCQ test) and asthma control test (ACT test). Both value sets produced indices ranging from 0 to 4 for ATCQ results and up to 25 points for ACT results. If the obtained ATCQ results are under 1 this means well controlled asthma; between 2 and 3, not well controlled asthma and results over 3 are related to very poorly controlled asthma. ACT results between 5 and 19 indicate not well controlled asthma, while 20-25 points showed well controlled asthma. When asthma is well-controlled, patients have no night and day symptoms, lead active life, have little or no need for reliever medication, have normal or near-normal lung function, and no exacerbations [Citation12, Citation13]. To evaluate the level of uncontrolled asthma, the following complex criteria were applied as recommended by ERS/ATS2014: ACT score less than 20, ACQ greater than 1.5 and FEV1 < 80% [Citation13].
Clinical data were provided by the allergologists. The patient data were collected through an interview performed by the physician.
In this work, we present the results for the quality of life, control of asthma and satisfaction with asthma therapy and their probable relations.
Statistics
Descriptive statistics, t-test and parametric analyses ANOVA (analysis of variance) were applied to assess correlations among data of interest. MedCalc ver.20.009 Software was used.
Results
Demographics
In total, 71 asthma patients were enrolled. The majority were 31–50 years (32.4%) and 61–80 years (26.8%), over half were male, 11.3% reported allergic rhinitis. About 65% of the patients worked and only a small part (4.22%) reported occupational risk factors; and 82% were non-smokers ().
Table 1. Demographics and clinical characteristics of patients.
Clinical characteristics
About 29% were diagnosed less than 5 years ago and 67% between 6 and 40 years ago. The mean durability of asthma for the cohort was 14.95 ± 10.69 years. The result for FEV1 for 63.37% was under 80%. The clinical data about duration of asthma, FEV1, FVC, Tiffeneau–Pinelli index and reported patients’ outcomes are presented in .
Patient reported outcomes
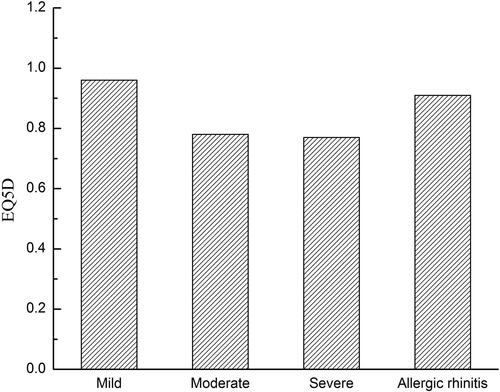
Asthma is a long-term inflammatory disease which influences the quality of patients’ life. Mean EQ5D scores for patients were 0.814 ± 0.22, while 39% (28 patients) declared perfect health. The quality of life according to severity of illness is presented in . Mean EQ5D score for males (n = 31) was 0.903 ± 0.15 (58% declared status 1) and for females (n = 34) 0.728 ± 0. 26 (24% declared perfect health status).
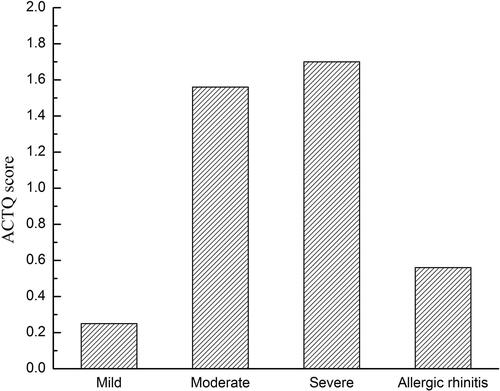
Asthma control is considered to reflect disease activity - fluctuations in symptoms, limitation of everyday activities or use of a rescue inhaler [Citation14]. Asthma control was measured by using ATCQ and ACT test – self reported measure of asthma control. Тhe results showed that 27 patients had well controlled asthma because their ACTQ scores were less than 1 (38%) at the time of the study visit and 28 patients (39%) had not well controlled asthma. There was very poorly controlled asthma in 21% of the group. We obtained that, for the whole group, asthma is not well controlled: the mean ACTQ score is 1.29 ± 1.21. presents the relationships between ACTQ scores and severity of asthma. Moderate and severe asthma are not well treated, while mild asthma and allergic rhinitis are well treated.
Gender connected treatment results were confirmed. ACTQ score for females was about two times higher than those for men. The mean ACTQ score for males was 0.81 ± 1.11, indicating that asthma was well controlled; and for females the ACTQ score was 1.73 ± 1.16 indicating not well controlled asthma. There was very poorly controlled asthma in 4 men (13%) and 9 women (26%).
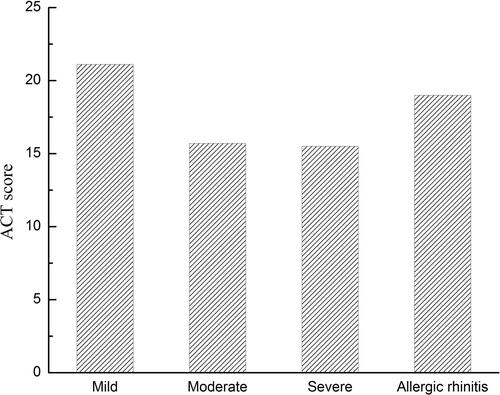
The results from the asthma control test showed that the asthma of the group was not well controlled (mean value of ACT score was 16. 92 ± 5.68) but over 41% of the patients had controlled asthma with an ACT scores greater than 20. Only 5.6% of the patients had well controlled asthma (score = 25). From the results of the interview, we obtained that 32% of the males and 76% of women had not well controlled asthma with ACT scores under 20 points (mean value 19.83 ± 4.81for men and 14.08 ± 5.29 for women), with the t-test indicating statistically significant differences (p < .0001). presents that moderate asthma is well controlled in contrast with severe and very severe asthma.
Co-morbidity and severity of asthma
The majority of patients had concomitant diseases − 80.29%. The percent of patients without concomitant diseases was 19.7%; 26% of them had at least one concomitant disease and 54% had two or more comorbidities (). The severity of the illness was assessed − 11.2% had mild asthma, 28% moderate and 38% a severe form of asthma (). Based on the combined assessment, over 80% of patients with severe and very severe asthma had concomitant diseases and 55% of them suffered from more than two diseases (). The percent of patients without concomitant diseases was between 15% in the case of severe asthma and 33% in case of rhinitis.
Table 2. Concomitant diseases in patients with asthma (no data for seven patients).
Within the asthma patients most common disease were cardiovascular problems (39.44%), followed by respiratory (33.81%) and musculoskeletal diseases (19.72%). The percent of allergenic rhinitis is 24%.
Satisfaction of treatment
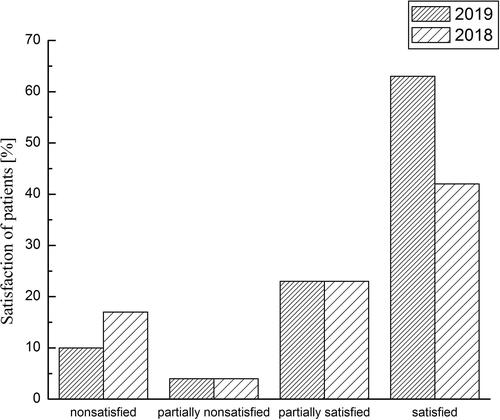
The satisfaction of treatment was investigated and the results of the interview showed that 63% of the patients were satisfied with the treatment, 23% partially satisfied, 4% partially unsatisfied and 10% unsatisfied. The results in 2019 are better than those from the previous year (). Men were more satisfied than women (84% vs. 41%).
The satisfaction of treatment and QoL of patients were investigated according to co-morbidity and severity of asthma. QoL and satisfaction of treatment of the patients with moderate and severe asthma who have two or more concomitant diseases (N = 25) were compared with QoL and the satisfaction of treatment of the patients from the same severity of asthma with up to one concomitant disease (N = 19). The obtained results for QoL showed that it decreases with the increase of concomitant disease (0.71 ± 0.26 vs. 0.86 ± 0.16). The difference is statistically significant (p = .03). The satisfaction of treatment of the patients is higher in the subgroup with less co-morbidities (2.47 ± 0.96 vs. 2.33 ± 0.81) but the difference is not statistically significant (p = .17).
We also compared the subgroup of patients with mild asthma and allergic rhinitis who reported no more than one concomitant diseases (N = 12) with subgroup of patients with moderate and severe asthma who have no more than one concomitant diseases (N = 19). In this case, the values of QoL indexes and satisfaction of treatment scores are higher in the group with mild asthma (0.97 ± 0.07 vs. 0.86 ± 0.16 for QoL and 2.75 ± 0.97 vs. 2.47 ± 0.96 for satisfaction scores). (The results for QoL are statistically significant (p = 0.03) while the difference in satisfaction scores is not statistically significant.). Thus, the results highlights that the increase of the number of concomitant diseases and severity of asthma decreased the QoL of patients and their satisfaction of treatment.
Discussion
Asthma has significant impact on lost productivity and reduced ability to work because of its long-lasting durability. We obtained that asthma is a lifelong condition for 67.71% of patients (the durability 6–40 year, the mean durability for this subgroup is 19.44 ± 8.71 years.). Asthma progressed with time as its mean durability for the cohort was 14.95 ± 10.69 years and the patients could learn to manage the illness. In case of such long durability the question for the effectiveness of treatment and the control of asthma is important, which explain the focus of our study.
One of the main factors which is known to influence the QoL of asthma patients is asthma control. According to Global Initiative for Asthma (GINA), 45.1% of patients have uncontrolled asthma while the results of ACTQ showed 21% of patients who have uncontrolled asthma. Our results of ACT score showed that 59% of the patients have less than 20 points which indicates that the most of the patients are with uncontrolled asthma [Citation14]. Mean scores of asthma control treatment were 16.92 ± 5.68. According to Ilmarinen et al. [Citation13], the mean score of uncontrolled asthma is 18 [Citation13–20], while we obtained a score of 15.5. The ACT and ACTQ scores present that mild asthma is well controlled in contrast with moderate and severe asthma. The ATCQ has been demonstrated to correlate with QoL [Citation21]. When assessing the effect of asthma control on the QoL of our patients, we observed for not very well controlled moderate and severe asthma: the scores are associated with lower indexes for QoL − 0.78 and 0.77, respectively.
The report of Jarvis et al. [Citation3] showed that asthma was associated with allergic rhinitis. A study on the incidence of asthma and rhinitis in North Macedonia done by the Institute of Occupational Medicine in Skopje reported that the prevalence of chronic rhinitis (the origin is not defined) is 30.2% [Citation4]. In our study, eight patients were included with diagnosis of allergic rhinitis and another nine patients had rhinitis as a concomitant disease; in total, 24% of asthma patients had rhinitis. The results are 8.2% higher than those published 30 years ago [Citation6]. This fact is probably related with increase of air pollution. In the EU, the prevalence of allergic rhinitis is on average 23% (between 17% in Italy and 29% in Belgium) according to [Citation16].
According to the literature, the prevalence of asthma is consistently higher in females than males [Citation3]. Vianello et al. [Citation17] also reported that females were predominant (59%) among asthma patients in the Italian population. Our study confirmed such gender differences. These differences are not possible to be explained with smoking or occupational risk factors because it is known that there is significantly higher smoking prevalence and occupational risk factors in Bulgarian men. In our cohort also the percentage of never-smoker men (74%) is higher than the percentages of never-smoker women (68%). The results are possibly related to risk factors other than cigarette smoking and occupational risk factors like air pollution which is too high. It is known that Bulgaria has the highest mortality in Europe because of air pollution [Citation18].
The main clinical characteristic of asthma patients is the severity of the illness. It was found that 38% of patients with asthma from the cohort had severe asthma. Our findings about the severity of asthma are different from the results reported for Western Europe and the EU. The reports about the severity of asthma are contradictory. Patients with severe asthma are estimated to comprise 5–10% in Western Europe [Citation13]. In Italy, according to data based on prescribed and dispensed asthma medications, the prevalence of severe asthma is 0.07% in the general population and 3.2% among asthmatic patients when only adherent patients were considered. Patients with uncontrolled asthma despite a treatment were 1.2% of asthmatics [Citation17]. The asthma prevalence in Germany is 7.3%, of which 8.7% (0.6% absolute) were treated with corticosteriods [Citation20].
We supposed that the situation in our neighbor countries like Serbia would more closely resemble Bulgaria, with a high level of severe asthma, but the prevalence of asthma in Belgrade, Serbia is 6.8% in adults and only (3.2%) have severe persistent asthma [Citation21].
The situation in our country is unknown, so a larger cohort of patients is needed to obtain a more accurate estimate. The other possible explanation is the fact that the patients who visit the leading clinical asthma center in the country usually are those who have serious problems.
Bulgarian patients’ satisfaction with prescribed therapy is high, as more than 60% were satisfied (). The study was not focused on finding correlation between the type of therapy or inhaler devices, adherence, asthma control, quality of life and satisfaction, which will be subject to further representative studies in the Bulgarian asthma population. We expect, as it has been demonstrated in other systematic reviews, that Bulgarian patients’ satisfaction is likely to be associated with higher adherence and asthma control [Citation20]. A Spanish cross-sectional, observational Asthma Satisfaction, Control and Adherence (ASCONA) study among 778 patients with moderate or severe asthma revealed that high patient satisfaction with an inhaler is related to high adherence, asthma control, non-severe asthma and no trouble with an inhaler, male gender and younger age. Moreover, those who have been diagnosed earlier experienced higher therapy satisfaction [Citation20].
Our study has several limitations. The collection of data was standardized, based on physician diagnosis and registers but some data like number of visits of GP, specialist, days in hospital) was based on self-reporting, which are the potential source of bias. Long-term analysis of data is needed to predict how control of asthma can be linked to patients’ quality of life. This was a single center experience, and the sample size is not representative, so the results cannot be generalized to the whole population.
Conclusions
To our knowledge, this is the first study conducted in Bulgaria focusing on the impact of asthma treatment on patients’ QoL and satisfaction with therapy. Evaluation of asthma control as a predictor of QoL could help to better understand the real effect on patients’ lives. It will serve as a basis for further studies on the prevalence and asthma control in the general population.
The results present high percentages of severe asthma patients. Air pollution and/or the chosen clinical center might be related to this finding. National asthma strategies should focus on prevention and early detection of the disease. Regarding clinical practice, the results of this study highlight the importance of improvement in diagnostic methods.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, [PM]. The data are not publicly available due to [restrictions, e.g. their containing information that could compromise the privacy of research participants].
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- Pawankar R, Canonica GW, Holgate ST, et al., editors. World Allergy Organization (WAO) White Book on Allergy. From the Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2014. Milwaukee: WAO; 2011. p. 1–216. Available from: http://www.ginasthma.org/)
- To T, Stanojevic S, Moores G, et al. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC Public Health. 2012;12:204.
- Jarvis D, Newson R, Lotvall J, et al. Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Eur J Allergy Clin Immunol. 2012;67(1):91–98.
- Zdraveska M, Dimitrievska D, Todevski D, et al. Joint incidence of asthma and rhinitis in macedonia. Open Respir Med J. 2015;9:52–58.
- Milushewa P, Doneva M, Petrova G. Availability and reimbursement of biological products for severe asthma in Bulgaria. SAGE Open Med. 2020;8:2050312120951067–2050312120951067.
- Mileva G, Popov T, Staneva M, et al. Frequency and characteristics of allergic diseases in Bulgaria. Allergy Asthma. 2000;5:3–32.
- Anum PO, Anto BP, Forson AG. Structured pharmaceutical care improves the health-related quality of life of patients with asthma. J Pharm Policy Pract. 2017;10:8–15.
- Böhmer M, Brandl M, Brandstetter S, et al. Factors associated with generic health-related quality of life in adult asthma patients in Germany: cross-sectional study. J Asthma. 2017;54(3):325–334.
- Petkova V. Pharmaceutical care for asthma patients: a community pharmacy-based pilot project. Allergy Asthma Proc. 2008;29(1):55–61.
- Chiner E, Hernández C, Blanco-Aparicio M, et al. Patient perspectives of the influence of severe and non-severe asthma on their quality of life: a national survey of asthma patients in Spain. Clin Respir J. 2022;16(2):130–141.
- Clark VL, Gibson PG, McDonald VM. What matters to people with severe asthma? Exploring add-on asthma medication and outcomes of importance. ERJ Open Res. 2021;7(1):00497–2020.
- Milenković B, Ristić S, Mirović D, et al. Validation of the serbian version of the asthma control test. Vojnosanit Pregl. 2019;76:1029–1036.
- Ilmarinen P, Juboori H, Tuomisto LE, et al. Effect of asthma control on general health-related quality of life in patients diagnosed with adult-onset asthma. Sci Rep. 2019;9(1):16107.
- Burden A. European Respiratory Society, Global Initiative for Asthma (GINA): global strategy for asthma management and prevention. Update 2014 and Online Appendix. Available from: https://ginasthma.org/wp-content/uploads/2019/01/2014-GINA.pdf
- Chen H, Gould M, Blanc P, et al. Asthma control, severity, and quality of life: quantifying the effect of uncontrolled disease. J Allergy Clin Immunol. 2007;120(2):396–401.
- Bauchau V, Durham S. Prevalence and rate of diagnosis of allergic rhinitis in Europe. Eur Respir J. 2004;24(5):758–764.
- Vianello A, Caminat M, Andretta M, et al. L. Prevalence of severe asthma according to the drug regulatory agency perspective: an Italian experience. World Allergy Organ J. 2019;12(4):100032–100033.
- Air Pollution and Mortality in BG (http://env-health.org/IMG/pdf/heal_briefing_air_bulgaria_eng.pdf). Available from: https://www.webmd.com/asthma/asthma-risk-factors
- Taube C, Bramlage P, Hofer A, et al. Prevalence of oral corticosteroid use in the German severe asthma population. ERJ Open Res. 2019;5(4):00092–2019.
- Plaza V, Giner J, Calle M, et al. Impact of patient satisfaction with his or her inhaler on adherence and asthma control. Allergy Asthma Proc. 2018;39(6):437–444.
- Dimitrova D, Youroukova V. Severe asthma - definitions, immunological characterization and molecular- targeted therapy. Thorac Med. 2015;7:9–25.