Abstract
Eyelids are a small anatomical structure, yet they contain several histological layers from which benign and malignant tumours can originate. Compared to other parts of the face, the eyelids are often the first place where neoplasms or disease changes are noticed. The aim of this study was to analyze eyelid tumours over a 10-year period. A retrospective study of 436 patients (450 eyes) who underwent oculoplastic surgery in an ophthalmology department over a 10-year period was performed. Descriptive, dispersion and correlation analyses were performed. The demographic analysis provided a clear assessment of the distribution and incidence of eyelid tumours according to age, size, histology and place of residence. Age and malignancy were in a positively significant relationship and increased together. The cases of benign eyelid tumours began to increase in terms of number out of the total cases observed after the age of 40, and malignant tumours after the age of 60. The trend in benign tumours continued until the age of 70, when the increase became four-fold, after which they decreased again at the expense of malignant tumours, which were already increased six-fold by the age of 70. Eighty percent of all malignant tumours of the eyelids were diagnosed after 60 years of age. A patient with an eyelid tumour is to be referred for treatment to an ophthalmologist by medical specialists of all specialties. Early patient referral is directly related to treatment success.
Introduction
Eyelids are a small anatomical structure, yet they contain several histological layers from which both benign and malignant tumours can originate. Their skin is the thinnest and most sensitive part of the skin on the human body. Compared to other parts of the face, the eyelids are often the first place where neoplasms or disease changes are noticed.
Eyelid tumours account for about 5–10% of all skin tumours. The majority of them are benign and account for about 80% of all eyelid tumours. These lesions are one of the frequent reasons for visiting an ophthalmologist. The treatment is mainly surgical and aims to preserve the anatomical structure of the eyelid, its function and, last but not least, its aesthetic appearance.
A basal classification of tumours based on their histomorphology has been proposed by the International Histological Classification of Tumours and published by the World Health Organization (WHO) [Citation1–3]. This classification distinguishes the following main histological groups: 1. Epidermal tumours, 2. Glandular tumours, 3. Stromal tumours, 4. Inflammatory lesions, resembling neoplasms.
The most common eyelid tumours are those of the first group – epidermal. Of them, 85% are in one of three groups – benign proliferations, basal cell carcinoma and melanotic lesions. In the remaining 10–15%, other tumours of the eyelids are present [Citation1,Citation4,Citation5]. Basal cell carcinoma (BCC) is one of the most common, and its incidence increases by 10% annually worldwide [Citation4,Citation6]. Of all BCC cases, 80% are in the head and neck area, 20% of which are in the eyelid area [Citation7–9].
We organized this study to analyze the tumours of the eyelids for a 10-year period, in patients operated on in the Eye Clinic – Pleven, and to compare the obtained results with similar results of other clinics. Hence, we aimed to contribute to the global statistics of eyelid tumours.
Subjects and methods
Study design
A retrospective study of 436 (450 eyes) patients operated on in the Eye Clinic Pleven (Pleven, Bulgaria) for the period from 2010 to 2019 was performed. Of all tumours of the eye and adnexa, only tumours of the eyelids were considered. All tumours were histopathologically examined after their surgical removal.
Data analysis
Kolmogorov-Smirnov and Shapiro-Wilk tests showed a normal data distribution. Analysis of variance (ANOVA/ANCOVA) was used to determine whether certain factor variables of categorical type cause systematic variation in a given variable of quantitative type. A multivariate analysis was performed for two or more independent variables of categorical type.
Correlation analysis was used to show the degree of relationship between the studied indicators. The age and size of the tumour were not categorical types, so ANOVA/ANCOVA analysis was not applicable. Bivariate correlation analysis was performed, and Pearson’s coefficient (r) was calculated. All the statistical analyses were performed with SPSS, version 26 (IBM Corp.).
Results
Descriptive analysis
Of the 436 (450 eyes) patients with eyelid tumours examined, 95 (21%) were malignant, and 355 (79%) were benign. The gender distribution was 57% (255) female and 43% (195) male. In the two large groups of benign and malignant tumours, we observed the following gender distribution: of the benign tumours 57% (201) were in women and 43% (154) in men, and of the malignant tumours 57% (54) were in women vs. 43% (41) in men. No significant difference was found regarding gender and malignancy (p = 0.97). The mean age was similar between men (57.8 years) and women (57.07 years), as in other reports [Citation10–15]. Of the patients included in this study, 28% lived in villages, and 72% in cities ().
Table 1. Distribution of cases.
The distribution of tumours according to their histology was as follows: the most cases were benign (71.8%), followed by malignant (21.3%), inflammation (6.5%), and the fewest precancerous (0.4%). Among the malignant tumours, basal cell carcinoma (BCC) ranked first at 71.9%, followed by squamous cell carcinoma (SCC) at 16.7%. Sebaceous carcinoma (SGC) ranked 3rd among malignant tumours (4.2%). In benign tumours, the distribution was as follows: cysts (38.8%) and papillomas (27.4%) are among the first representatives, followed by nevi (10.2%), keratoses (7.4%), hemangiomas (4.3%) and others.
Age and malignancy were in a positively significant relationship (p > 0.001), i.e. both indicators increased together. Over 60 years of age, a three-fold increase in malignant tumours was seen, and over 70 years, six-fold.
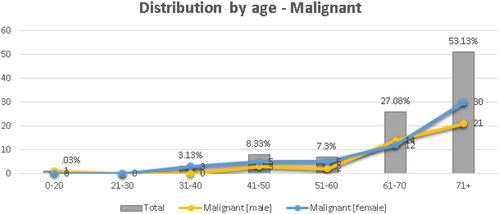
The distribution by age concerning malignancy showed a positive dependence starting from the group of 31–40 years, with about 3%. The highest percentage of malignant correlation was in the group 71+, with an expected statistical value twice as small according to the reports. There was a positively significant relationship starting from the age of 61–70 years with a percentage of 27%, reaching over 53% for the over 71 years group. An increase in malignant tumours was observed in women over 71 years of age, but the difference between the two sexes was non-significant ().
A similar proportional dependence was observed in benign tumours. The cases peaked in the first group 0–20 years, but there was a slight decrease in the last group (71+ years).
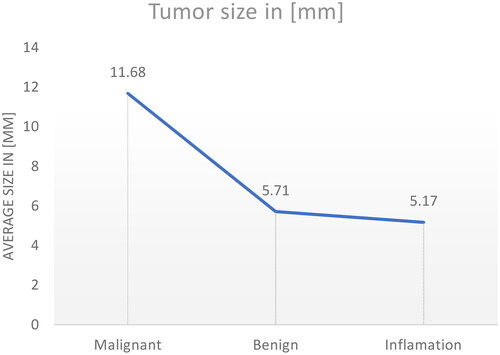
A marked trend of malignant tumours by size was observed (). Small sizes were predictably characteristic of benign tumours and inflammations, while large sizes were characteristic of malignant tumours. This dependence was statistically significant (p < 0.001).
Figure 2. Distribution by size and type of malignant, benignant eyelid tumours and inflammations (N = 450).
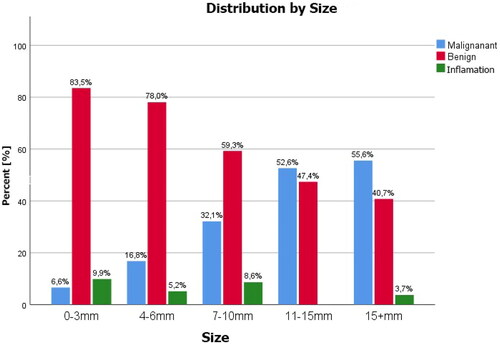
At sizes of 7 mm and above, the statistical distribution was in favour of malignant tumours. In the groups above 11 mm, malignant tumours prevailed.
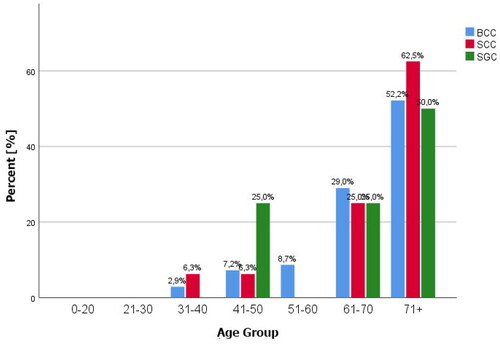
Up to 40 years of age, the frequency of malignant tumours was relatively small (4.2%), from 40 to 60 years it was 15.6%, after 60 years it was 27.1%, and after 71 years 53 .1%. The percentage ratio between tumours was as follows: BCC 71.9%, SCC 16.7%, SGC 4.2%, and others 7.2%. There was an increasing trend after 70 years for BCC, SCC and SGC, although it was less common. In the group of analysed cases, 50% of SGC cases occurred over 71 years of age. The distribution of malignant tumours was left-skewed, which is an expected result based on the literature review [Citation7,Citation10–17]. shows the age distribution of the three most common eyelid malignancies.
Figure 3. Percentage distribution of the most common eyelid malignant tumours by age – BCC-Basal cell carcinoma, SCC – squamous cell carcinoma, SGC – sebaceous gland carcionoma, (N = 450).
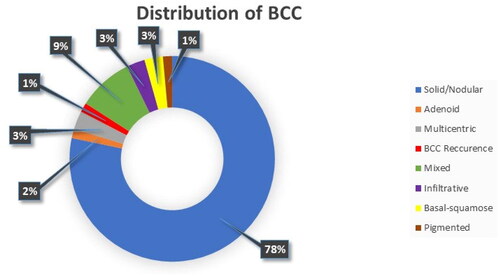
The most common malignant tumour of the eyelids was Basal cell carcinoma (BCC) − 71.9%. The histological variants shown in were most frequently observed.
The solid (nodular) variant of BCC was most common (78%), followed by the mixed variant. The rest were in smaller percentages of less than 3%.
The analysis based on incidence according to place of residence showed a highly significant dependence of malignant cases, in favour of the group living in villages, in contrast to the group living in cities, where benign cases prevailed (p < 0.001). Malignant cases in villages accounted for 31.5%, and in cities for 17.2%. Benign ones showed the opposite ratio: 68.5% in villages and 82.8% in cities.
Analysis of dispersion
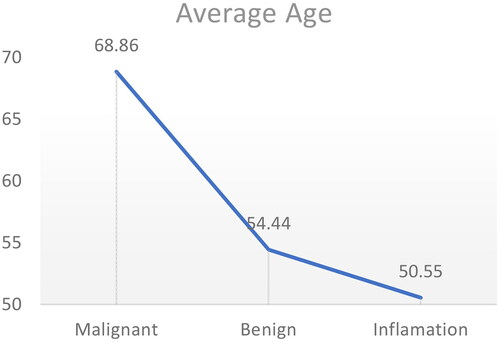
The statistical analysis revealed a significant intergroup correlation between the indicators of age, malignant and benign tumours (p < 0.001), and a non-significant correlation with inflammation (p > 0.273). The mean age for malignant tumours was 68.86 years, for benign tumours 54.44 years, and for inflammations, it was 50.55 years ().
Figure 5. Distribution of mean age (57.4 years) in the three eyelid tumour categories – Malingnant, benignant and inflammation (N = 450).
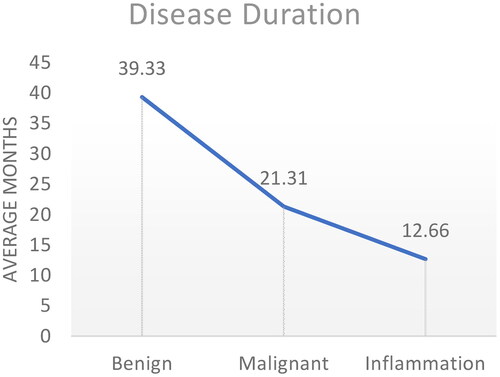
There was a positive correlation between disease duration and malignancy (p < 0.009) (). Benign tumours had the longest history (39.3 months), followed by malignant ones (21.3 months) and the earliest to have medical help sought were inflammations – at an average of 12.6 months.
Tumour size showed within-group significance for the malignant and benign groups but no significance for inflammation. The detailed distribution is given in the correlation analysis, but it can be seen from that the mean size for malignant tumours was 11.68 mm and for benign tumours 5.71 mm, and the difference between these two groups was significant (p < 0.0001).
Correlation analysis
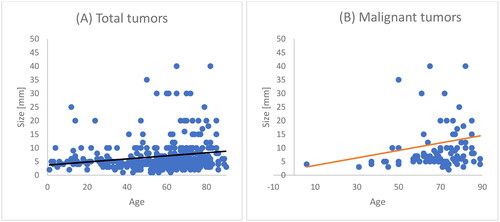
It can be seen from that there was a positive significant correlation of age to tumour size (p < 0.01), with older age being associated with a larger tumour size. This trend was even more pronounced in malignant tumours as a separate sample.
Discussion
Characteristics by sex
The gender distribution in all age subgroups was even, except for the over 70 years group, where there were almost twice as many women as men. This distribution correlates with the National Statistical Institute (NSI) data for 2021 [Citation18]. In the NSI sample, it is clear that for the general population over 70 years, there are twice as many women as men. The presence of more women in this age group corresponds to most tumours occurring in women in the same group, and hence, for all tumour groups (malignant, benign and inflammatory) women were twice as many as men in the age subgroup over 70 years.
Characteristics by age
Our analysis showed that most tumours were represented in the group over 60 years of age. In the 0–20 year group there was a distinct peak due to inflammatory tumours (excluding chalazion). An increase in the total number of tumours was seen after 40 years of age. By the age of 40, all eyelid tumours were 17% of the total cases observed, by the age of 60 they increased to 47%. Tumours after 60 years of age accounted for 53% of all eyelid tumours analyzed in this study, with the greater percentage being over 71 years of age. Similar data are also reported by other authors [Citation11–13].
In the group analysis by age, we found large differences in the distribution by histology. Benign tumours began to increase in number after 40 years of age, and malignant tumours after 60 years. In benign cases, this trend continued until the age of 70, when the increase became four-fold, after which they decreased again at the expense of malignant cases, which by the age of 70 already showed a six-fold increase. Our calculations showed that 80% of malignant tumours were distributed after 60 years of age, which is similar to larger cohorts analyzed by other authors [Citation11]. The greater percentage of benign tumours was characteristic of a younger age in contrast to malignant tumours, and the separation period between the two groups was 20 years on the abscissa of the age distribution. Inflammations showed an equal distribution in all age groups.
In confirmation of the age descriptive analysis, correlation and variance analyzes were performed to test for within-group significance. We found that the average age for the appearance of malignant tumours was 68.8 years, and for benign tumours 54.4 years (p < 0.001). In the case of inflammation, this relationship was not significant (p > 0.273). The results are in agreement with other authors [Citation11].
We observed a positive correlation of age to tumour size (p < 0.01), with older age being associated with larger tumour size. The same trend was even more pronounced for malignant tumours as a separate sample.
Benign tumours are seen at a younger age, when patients are more active and seek medical attention more often. Conversely, malignant tumours occur in older patients who often postpone seeking medical attention until a point when the tumour grows and becomes difficult to treat.
Characteristics by residence and occupation
The statistics provided by NSI at the beginning of 2021, according to which 72.9% of the population lives in cities and 27.1% in villages, correspond to our results [Citation19]. Although the sample is asymmetric and those living in the city represent the larger percentage, after the cross-sectional analysis, it can be concluded that the older population (60+ years) with eyelid tumours mainly lived in the villages (p < 0.002) . On the other hand, we found a highly significant dependence (p < 0.001) of malignant cases in the group living in villages, in contrast to the group living in cities, where benign cases prevailed. Malignant cases in villages accounted for 31.5% compared to those in cities (17.2%), whereas benign cases showed the opposite ratio: 68.5% in villages and 82.8% in cities. This result could be explained by the easier access to – and consequently – early seeking of qualified medical care by the population living in cities or an unproven harmful factor leading to malignancy, which is not the subject of this analysis.
Conclusions
Eyelid tumours are one of the frequent reasons for visiting an ophthalmologist. In the local population analyzed here, benign tumours began to increase in number after the age of 40, and malignant tumours after the age of 60. In the case of benign tumours, this trend continued until the age of 70, when the increase became four-fold, after which they decreased again at the expense of malignant tumours, which increased six-fold up to the age of 70. Age and malignancy were positively significantly correlated and increased together. Of all malignant tumours of the eyelids, 80% were diagnosed after 60 years of age.
A patient with an eyelid tumour is to be referred for treatment to an ophthalmologist by medical specialists of all specialties. Early patient referral is directly related to treatment success.
Author contributions
All authors (GB, ChB, SM) have equal contribution to the study including: patient follow-up, conception and study design, data analysis, writing, revision and final article preparation. There are no other parties to acknowledge.
Informed consent
Not applicable.
Statement of Ethics
The study was conducted in accordance with the principles for human experimentation as defined in the Declaration of Helsinki, local Good Clinical Practice guidelines and local Medical University of Pleven institution guidelines (Ethics Committee approval No. 716-KENID/12.1.2023).
Availability of data and materials
Data are available on request due to privacy or other restrictions.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Singh A, Damato B, Pe’er J, et al. Clinical ophthalmic oncology. Vol 1. 1st ed. 1600 John F. Kennedy Boulevard, Suite 1800, Philadelphia, PA 19103-2899, USA: Elsevier’s Health Sciences Rights Department; 2007.
- Rosai J, Sobin LH. Histological typing of tumours of the thymus. In: International histological classification of tumours. Berlin Heidelberg: Springer-Verlag; 1999. ci.nii.ac.jp. Accessed October 21, 2020. https://ci.nii.ac.jp/naid/10014676418/
- Sobin LH. The international histological classification of tumours. Bull World Health Organ. 1981;59(6):813–819.
- Cook BE, Bartley GB. Epidemiologic characteristics and clinical course of patients with malignant eyelid tumours in an incidence cohort in Olmsted County, Minnesota. Ophthalmology. 1999;106(4):746–750.
- Kersten RC, Ewing-Chow D, Kulwin DR, et al. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology. 1997;104(3):479–484.
- Wong CSM, Strange RC, Lear JT. Basal cell carcinoma. BMJ. 2003;327(7418):794–798.
- Singh U, Kolavali RR. Overview of eyelid tumours. In: Surgical ophthalmic oncology. Cham: Springer; 2019. 3–10.
- Lasudry J. Prise en charge des tumeurs palpébrales: considérations générales. J Fr Ophtalmol. 2011;34(10):741–754.
- Pe’er J. Pathology of eyelid tumours. Indian J Ophthalmol. 2016;64(3):177.
- Zlatarova ZI, Dokova KG. Incidence of non-melanoma eyelid malignancies in Bulgaria (2000-2015). Ophthalmic Epidemiol. 2021;28(3):198–204.
- Wang L, Shan Y, Dai X. Clinicopathological analysis of 5146 eyelid tumours and tumour-like lesions in an eye Centre in South China, 2000-2018: a retrospective cohort study. BMJ Open. 2021;11:41854.
- Bagheri A, Tavakoli M, Kanaani A, et al. Eyelid masses: a 10-year survey from a tertiary eye hospital in Tehran. Middle East Afr J Ophthalmol. 2013;20(3):187–192.
- Eren MA, Gündüz AK. Demographic features and histopathological diagnosis in primary eyelid tumours: results over 19 years from a tertiary center in Ankara, Turkey. Int J Ophthalmol. 2020;13(8):1287–1293.
- Yu SS, Zhao Y, Zhao H, et al. A retrospective study of 2228 cases with eyelid tumours. Int J Ophthalmol. 2018;11(11):1835–1841.
- Kaliki S, Bothra N, Bejjanki KM, et al. Malignant eyelid tumours in India: a study of 536 asian indian patients. Ocul Oncol Pathol. 2019;5(3):210–219.
- Huang YY, Liang WY, Tsai CC, et al. Comparison of the clinical characteristics and outcome of benign and malignant eyelid tumours: an analysis of 4521 eyelid tumours in a tertiary medical center. Biomed Res Int. 2015;2015
- Ul Kadir SM, Rani Mitra M, Rashid R, et al. Clinicopathological analysis and surgical outcome of eyelid malignancies: a study of 332 cases. J Skin Cancer. 2022;2022:1–9.
- Population by statistical regions, age, place of residence and sex | National Statistical Institute. [cited 2022 Dec 15]. https://www.nsi.bg/en/content/2977/population-statistical-regions-age-place-residence-and-sex.
- Population by districts, municipalities, place of residence and sex | National Statistical Institute of Bulgaria. [cited 2022 Dec 15]. https://www.nsi.bg/en/content/2975/population-districts-municipalities-place-residence-and-sex.