Abstract
Adherence is the degree to which the patient’s behaviour and actions correspond to the physician’s established treatment regimen regarding timing, dose and frequency. Patient counselling by both oncologists and pharmacists and optimization of the therapeutic regimen can critically impact decision-making and adherence to therapy. We performed a two-step study to identify factors influencing adherence to therapy from the perspective of oncology hospital pharmacists in Bulgaria. The results show that the major factors affecting anticancer therapy adherence are the manifestation of adverse drug reactions and distrust in therapy. These could be overcome with improved communication between patients, oncologists and pharmacists on therapy aspects and more active involvement of the hospital pharmacists in therapy monitoring with a main focus on identifying possible drug-related problems based on safety profile, drug-drug interactions and non-adherence.
Keywords:
Introduction
Adherence is the degree to which a patient’s behaviour and actions correspond to the physician’s established treatment regimen regarding timing, dose and frequency [Citation1].
Patient adherence is important to achieve therapeutic goals and reduction in hospitalization and complications-related costs. The adherence rate is a frequently used indicator for patients’ therapeutic response in oncology [Citation2]. A higher rate of adherence is associated with an increased likelihood of six-year 3-log disease reduction [Citation3]. The estimated level of adherence to therapy in patients receiving oral anticancer medicines ranges between 50% and 90% [Citation4, Citation5]. The reported average adherence rate to prescribed oral chemotherapy over 12 weeks is 89.3%. Women were more adherent than men. The overall rate of improvements in patient symptoms as depressive symptoms, quality of life and satisfaction with clinician communication and treatment are associated with better adherence [Citation6].
The limited pharmacist’s education in haematology and oncology in universities could hinder their participation in disease management. US pharmacy students, for example, have lectures on oncology therapy in the main course, but only 30% of them go to oncology practice for 4–6 weeks [Citation7, Citation8]. Adherence courses are also rarely included and not very successfully developed in university and postgraduate curricula among European medical universities [Citation9, Citation10].
A lot of studies have analysed the potential role of the pharmacist in medication adherence in oncology patients. A recently published meta-analysis summarizes the results and conclusions from 20 randomized-control trials and 15 meta-analyses [Citation11]. Meta-analysis focuses on the different aspects of pharmacists’ expertise as trustful partners in the monitoring process of oncology patients. It concluded that the pharmacist’s role is mainly aimed at providing rational medicine utilization, focusing on drug interactions and safety profiles.
The main goal of our study is to analyse the attitude and readiness of oncology hospital pharmacists in terms of activities described in the literature aiming at oncology treatment and adherence from the perspective of the Bulgarian healthcare setting.
Methods and materials
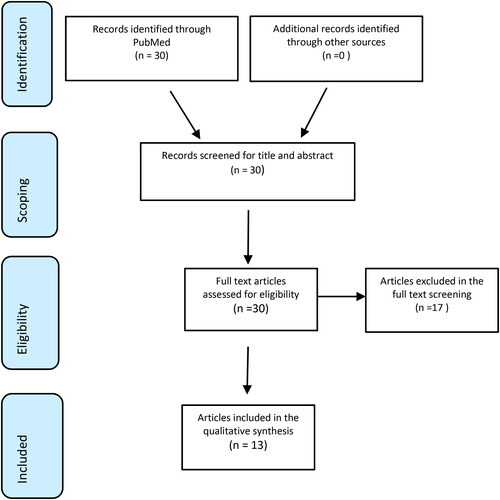
We conducted the study in two phases: (1) a scoping literature review to identify the potential role of pharmacists in improving adherence to therapy in oncology patients, and (2) an online anonymous survey among oncology hospital pharmacists in Bulgaria based on a direct questionnaire assessing their attitude to impact and improve adherence to oncology therapy. A scoping review was used as a basis for the online survey.
Scoping review
With the scoping review, we aimed to identify and analyse published articles with a focus on the potential role of pharmacists in adherence to therapy in oncology patients. We chose the scoping review methodology as it proved to be a useful tool in previous studies in which we aimed to collect published data for a specific topic and to use the results as a basis for subsequent surveys among specific focus groups [Citation12]. To conduct the literature review we used the methodology of scoping review based on the framework provided by Arskey and ÒMalley [Citation13] and further clarified by Levac, Colquhoum and ÒBrien [Citation14]. We opted for the methodology of scoping reviews because it saves time and is designed to identify evidence, key characteristics and factors related to a specific concept. It is also very useful for identifying knowledge gaps in a given field. The literature search was conducted through the PubMed database, using predefined keywords: patients; oncology; adherence and pharmacists. The search was limited to English-language articles published in the past 10 years with abstracts and full texts. Identified articles were screened first in the title and abstract screening phase, and then those included were reviewed in full text. The following exclusion criteria were used: (1) No abstract; (2) Not English language, (3) Not published in the past 10 years; (4) Not discussing pharmacists’ role in adherence to oncology treatment. We do not further systematize the publications because we use them only as a step to create the online survey.
Online survey
The national study was carried out from December 2023 to January 2024, targeting oncology hospital pharmacists. Data were collected anonymously via an online survey created using the Google® Forms platform. The applied method was a direct questionnaire consisting of 12 closed questions distributed among domains assessing (1) demographic characteristics of oncology patients, (2) awareness of patients about drug-related problems (DRPs) and pharmacist-patient communication and (3) patients’ awareness about adherence to therapy and tools and approaches for adherence and communication improvement. The response rate was 100% as all pharmacists who started the online study completed the questionnaire.
All the extracted data were validated, systemized, compared and analysed through descriptive statistics in Excel v. 2016.
No ethical approval was needed for the conduction of the survey as it does not include any patient information and sensitivity data but collects data based on pharmacists’ opinions and experience.
Results
Scoping review
The scoping review identified 13 articles meeting the predefined criteria.
The list of the included articles (n = 13) with basic objectives is summarized in .
Table 1. List of articles included in the scoping literature review.
The results from the scoping review show that clinical and hospital pharmacists’ involvement in adherence is aimed at dose adjustment, patient awareness about the disease and therapy and impact medication-taking behaviour.
Оnline survey
The response rate of the online survey for the pilot phase was that 26 hospital pharmacists filled in the questionnaire. Of them 75% (n = 18), stated to dispense medicines for oncology patients from different parts of the country irrespective of the regional city, and the gender of the patients. The majority of the patients are in the age group of 40–65 years. The results from the demographic domain are summarized in .
Table 2. Results from demographic characteristics of patients from a pharmacist’ perspective.
The next part of the questionnaire aimed to explore the factors influencing adherence to therapy and the role of the hospital pharmacist. The results are summarized in .
Table 3. Results from the questionnaire regarding the factors and opportunities to influence adherence according to hospital pharmacists.
The results from the survey show that the most frequently reported factors from patients’ side affecting adherence to therapy are the manifestation of adverse drug reactions − 75% of the respondents and distrust in the prescribed therapy (18% of the respondents). The majority of the pharmacists (79%) responded that they consult their patients when dispensing their medication and also discuss the importance of regular intake of medication and the need for adherence to therapy
The risk of lower adherence, however, could be avoided with improved discussion with oncologists and pharmacists and achievement of therapeutic response. The latter depends mostly on timely diagnosis and access to the most appropriate therapy based on diagnostic categorization.
The results from the pilot study also show that hospital pharmacists and oncologists have the opportunity to communicate prescribed therapy in terms of adherence but still improvement in this area could be considered.
Discussion
To the best of our knowledge, this is the first study in Bulgaria to analyse adherence to treatment among oncology patients from the perspective of hospital pharmacists. Our results confirm already published ones focusing on the role of pharmacists in consultation on anticancer medication. According to the pharmacists who took part in the survey, some of the main reasons for lower adherence to therapy are the manifestation of adverse events and the distrust in the ongoing therapy. They also consider that what might encourage patients to take medicines as prescribed is the presence of a response to therapy and discussion with a doctor or pharmacist.
The impact of oncology pharmacists on patients’ beliefs and attitudes about therapy is very important and can be a major driver of clinical outcomes. Al-Taie et al. showed that patients with diabetes and cancer who were assigned to both usual and clinical pharmacy care, pharmacotherapy optimization and regular recommendations experienced a significant increase in medication adherence (p = .0049), a significant increase in diabetes self-care activities and also reported less deterioration in quality of life [Citation28].
Oncology pharmacists have specialized knowledge of anticancer medicines and their specific role in the treatment. The pharmacists are also experts in seven major aspects including selection, supply, storage, dispensing, prescribing, administration and education. Their role as an assistant during the recovery phase and adherence to chemotherapy regimens is essential for optimal treatment and outcome [Citation29]. The main role in improving patient adherence is to overcome some barriers such as forgetfulness, side effects of anticancer drugs, drug-related toxicity, depression and falling asleep in time before taking drugs [Citation30].
Umar et al. focused on the potential role of clinical pharmacists in predicting possible DRPs with prescribed anticancer therapy in oncology patients. The results of their study among 137 patients showed that 73.2% of the total DRPs were due to inappropriate combinations of medicines. The inclusion of clinical pharmacists led to 90.9% resolved DRPs [Citation31].
In China, a new model was developed for an integrated program to improve communication and collaboration providing continuous monitoring of cancer patients. There was a significant difference in patient satisfaction in the two groups (p < .05). Fewer patients in the integrated pharmacy services group had clinic and emergency visits compared with the routine care group (33.1% vs. 59.2%; p < .05) [Citation32].
Digital applications improving adherence could be also implemented in the everyday practice and could be a possible way to improve adherence among oncology patients. They are still rarely used among hospital pharmacists in Bulgaria.
Our study has a few limitations mainly related to the absence of prior validation of the questionnaire and the small number of respondents. The latter limitation is considered to be improved with further dissemination of the survey.
Conclusions
The major factors affecting adherence to anticancer therapy are a manifestation of adverse drug reactions and distrust in medicines. These could be overcome with improved communication between patients, oncologists and pharmacists on therapy aspects and more active involvement of the hospital pharmacists in therapy monitoring.
Acknowledgements
SK and GP developed the questionnaire and conducted the online survey. NR performed the literature review. MD and ZM wrote the methodology and contributed to analysing and writing. JA contributed to writing and validating the data results. All authors contributed to the article and approved the submitted version.
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The authors declare no conflict of interest.
Data availability statement
The data that support the findings reported in this study are available from the corresponding author [MD] upon reasonable request.
Additional information
Funding
References
- Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–47. doi: 10.1111/j.1524-4733.2007.00213.x.
- Ruddy K, Mayer E, Partridge A. Patient adherence and persistence with oral anticancer treatment. CA Cancer J Clin. 2009;59(1):56–66. doi: 10.3322/caac.20004.
- Marin D, Bazeos A, Mahon F-X, et al. Adherence is the critical factor for achieving molecular responses in patients with chronic myeloid leukemia who achieve complete cytogenetic responses on imatinib. J Clin Oncol. 2010;28(14):2381–2388. doi: 10.1200/JCO.2009.26.3087.
- Verbrugghe M, Verhaeghe S, Lauwaert K, et al. Determinants and associated factors influencing medication adherence and persistence to oral anticancer drugs: a systematic review. Cancer Treat Rev. 2013;39(6):610–621. doi: 10.1016/j.ctrv.2012.12.014.
- Bassan F, Peter F, Houbre B, et al. Adherence to oral antineoplastic agents by cancer patients: definition and literature review. Eur J Cancer Care (Engl). 2014;23(1):22–35. doi: 10.1111/ecc.12124.
- Jacobs JM, Pensak NA, Sporn NJ, et al. Treatment satisfaction and adherence to oral chemotherapy in patients with cancer. J Oncol Pract. 2017;13(5):e474–e485. doi: 10.1200/JOP.2016.019729.
- Kwon J, Ledvina D, Newton M, et al. Oncology pharmacy education and training in the United States schools of pharmacy. Curr Pharm Teach Learn. 2015;7(4):451–457. doi: 10.1016/j.cptl.2015.04.005.
- Paolella GA, Boyd AD, Wirth SM, et al. Adherence to oral anticancer medications: evolving interprofessional roles and pharmacist workforce considerations. Pharmacy (Basel). 2018;6(1):23. doi: 10.3390/pharmacy6010023.
- Benbrahim N, Garcia-Cardenas V, Saez-Benito L, et al. Adherence: a review of education, research, practice and policy in Spain. Pharm Pract. 2009;7(3):125–138.
- Dircks M, Mayr A, Freidank A, et al. Advances in clinical pharmacy education in Germany: a quasi-experimental single-blinded study to evaluate a patient-centred clinical pharmacy course in psychiatry. BMC Med Educ. 2017;17(1):251. doi: 10.1186/s12909-017-1092-z.
- Fentie A, Huluka S, Gebremariam G, et al. Impact of pharmacist-led interventions on medication-related problems among patients treated for cancer: a systematic review and meta-analysis of randomized control trials. Res Social Adm Pharm. 2024;20(5):487–497. doi: 10.1016/j.sapharm.2024.02.006.
- Dimitrova M, Jakab I, Mitkova Z, et al. Potential barriers of patient involvement in health technology assessment in Central and Eastern european countries. Front Public Health. 2022;10:922708. doi: 10.3389/fpubh.2022.922708.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. (doi: 10.1186/1748-5908-5-69.
- Hansen EA, Pietkiewicz JM, Blum BL. Evaluation of the feasibility and utility of a pharmacist-centered collaborative drug therapy management program for oncology-based symptom management. J Pharm Pract. 2016;29(3):206–211. doi: 10.1177/0897190014557626.
- Djebbari F, Stoner N, Lavender VT. A systematic review of non-standard dosing of oral anticancer therapies. BMC Cancer. 2018;18(1):1154. doi: 10.1186/s12885-018-5066-2.
- Birand N, Boşnak AS, Diker Ö, et al. The role of the pharmacist in improving medication beliefs and adherence in cancer patients. J Oncol Pharm Pract. 2019;25(8):1916–1926. doi: 10.1177/1078155219831377.
- Defoe KD, Jupp J, Leslie T. Integration of clinical pharmacists into an ambulatory, pediatric hematology/oncology/transplant clinic. J Oncol Pharm Pract. 2019;25(3):607–612. doi: 10.1177/1078155217752534.
- Mackler E, Segal EM, Muluneh B, et al. 2018 Hematology/oncology pharmacist association best practices for the management of oral oncolytic therapy: pharmacy practice standard. J Oncol Pract. 2019;15(4):e346–e355. doi: 10.1200/JOP.18.00581.
- Holle LM, Segal EM, Jeffers KD. The expanding role of the oncology pharmacist. Pharmacy (Basel). 2020;8(3):130. doi: 10.3390/pharmacy8030130.
- Crul M, Oosterhof P. The oncology pharmacist as part of the palliative treatment team. Int J Pharm Pract. 2020;28(1):92–96. doi: 10.1111/ijpp.12583.
- Joy AM, Nandakumar UP, Sharad C, et al. Role of clinical pharmacist in the medication adherence behaviour of cancer patients: an interventional study. Pharm Hosp Clin. 2021;56(3):291–297. doi: 10.1016/j.phclin.2021.05.002.
- Pirolli AV, Brusamarello T, Everton SS, et al. The role of the clinical pharmacist in guiding adjuvant hormonal therapy in patients with breast cancer. J Oncol Pharm Pract. 2022;28(6):1368–1374. doi: 10.1177/10781552211029361.
- Ghiggia A, Bianco A, Castelli L, et al. Adherence to oral chemotherapy: evidence from a randomised clinical trial. Eur J Cancer Care (Engl). 2021;30(1):e13336. doi: 10.1111/ecc.13336.
- Oliveira CS, Silva MP, Miranda Í, et al. Impact of clinical pharmacy in oncology and hematologycenters: a systematic review. J Oncol Pharm Pract. 2021;27(3):679–692. doi: 10.1177/1078155220976801.
- Neuner J, Weil E, Fergestrom N, et al. Feasibility of a pharmacist-led symptom monitoring and management intervention to improve breast cancer endocrine therapy adherence. J Am Pharm Assoc (2003). 2022;62(4):1321–1328.e3. doi: 10.1016/j.japh.2022.03.001.
- Novosadova M, Filip S, Molnarova V, et al. Clinical pharmacist in oncology palliative medicine: drug compliance and patient adherence. BMJ Support Palliat Care. 2023;13(e3):e1308–e1317. doi: 10.1136/spcare-2023-004212.
- Al-Taie A, Izzettin FV, Sancar M, et al. Impact of clinical pharmacy recommendations and patient counselling program among patients with diabetes and cancer in outpatient oncology setting. Eur J Cancer Care (Engl). 2020;29(5):e13261. doi: 10.1111/ecc.13261.
- Carolyn SJM. Role of pharmacists in optimizing the use of anticancer drugs in the clinical setting. IPRP. 2014;3:11–24. doi: 10.2147/IPRP.S40428.
- Krikorian S, Pories S, Tataronis G, et al. Adherence to oral chemotherapy: challenges and opportunities. J Oncol Pharm Pract. 2019;25(7):1590–1598. doi: 10.1177/1078155218800384.
- Umar RM, Apikoglu-Rabus S, Yumuk PF. Significance of a clinical pharmacist-led comprehensive medication management program for hospitalized oncology patients. Int J Clin Pharm. 2020;42(2):652–661. doi: 10.1007/s11096-020-00992-8.
- Qi H, Zhu L, Chen L, et al. Reduced emergency room visits and improved medication adherence of an integrated oncology pharmaceutical care practice in China. J Oncol Pharm Pract. 2021;27(6):1503–1515. doi: 10.1177/10781552211027218.