ABSTRACT
Introduction: Condylar hyperplasia (CH) is one of the causes of asymmetric facial growth resulting from overgrowth or hyperactivity in the mandibular condyles. The present review article describes the clinical and histopathological features of condylar hyperplasia and condylectomy with and without orthognathic surgery as a treatment approach to address this condition.
Objectives and Conclusions: This article highlights the different classification systems to characterize CH. Clinical examination and radiographic examinations (including bone scintigraphy and single-photon emission computed tomography) over a period of time appear to be the gold standard in the diagnosis. Condylectomies, which removes a small portion of the mandibular condylar head, have been reported to produce adequate outcomes with minimal side effects on the temporomandibular joint. Timing of this surgical procedure and differences in indications and outcomes between high and low condylectomies are presented. A case report illustrating a low proportional condylectomy is reported.
Background
Condylar Hyperplasia (CH) is a term given to a growth abnormality associated with the temporomandibular joint (TMJ) caused by hyperactivity of mandibular condyle cells or a tumour [Citation1–3]. It is considered relatively uncommon, with the exact prevalence of this condition not having been reported. This condition appears to be more predominant in females with a 2:1 female-to-male ratio [Citation4]. The reported higher predominance in females is possibly correlated to a higher degree of oestrogen receptor accumulation in the TMJ region [Citation2,Citation5,Citation6]. Some studies have indicated similar incidences in both sexes and all ethnic groups [Citation7,Citation8]; while others reported a variation in the ratios between males and females [Citation9–11]. It can be described as a self-limiting abnormal condylar growth resulting overtime in intense forms of skeletal asymmetries and jaw deformities [Citation12]. Most often its onset is before puberty and the majority of patients present clinical manifestations in adolescence and young adulthood [Citation7,Citation13]. The peak occurrence of the deformity is estimated to be between 14 and 30 years of age [Citation5].
CH is characterized by continued and prolonged mandibular growth that usually proceeds until the mid-twenties [Citation14]. The aetiology remains uncertain; although vascular anomalies, Meckel’s cartridge remnants, trauma, mechanical, endocrine and genetic factors have been proposed [Citation4,Citation15]. It has been further hypothesized that two different growth regulators, one responsible for the growth in length (factor L) and one responsible for the growth in mass (factor M) might be possibly responsible for the pathogenesis in its different forms [Citation16]. On the other hand, Insulin-like growth factor 1 (IGF-1) has been implicated to play a role in the development of CH. The proliferating zone of hyperplastic condyles seems to contain high concentration of IGF-1, which increases the number of chondrocytes [Citation17,Citation18].
Histologically, the bony trabeculae on the affected side are often irregular and thick resulting in higher than normal percentages of surfaces covered with osteoid [Citation7]. Moreover, the affected condyle is characterized by the presence of an undifferentiated mesenchymal layer, with a hyperplastic and pathognomonic cartilage ‘islands’ in the proximal trabeculae [Citation19]. In a case series of 22 patients suffering from unilateral CH (UCH) with an emphasis on the histopathological aspect, it was concluded that there are 2 types of CH. The first type is generally observed in early adolescence, where the hyperplasia is represented by an exaggerated, normally proceeding growth. The histology of the condyle in these individuals is age-dependent and consists of conversion of the hyaline cartilage into fibro-cartilage. The second type is usually seen in older individuals and represents a reactive growth as a response to an eliciting agent in which the histological features of the condyle is distorted by a large mass of hyaline cartilage accompanied by degenerative changes in the form of arthrosis which causes joint pain [Citation13].
Classification
The first case report of CH was outlined in the literature in 1836 [Citation20]. Afterwards, different terminologies and classifications have been proposed to describe this clinical joint condition. The terms, hemimandibular hyperplasia (HH) and hemimandibular elongation (HE) were initially proposed by Obwegeser and Makek [Citation10] who discussed the common causes of mandibular asymmetry with emphasis on the hyperactivity of the condylar growth regulation centres. In their classification, CH was classified into three main categories: Type 1 (HE), normal condylar head with an elongated neck, prominent horizontal growth, and displaced chin and midline to the opposite side. Type 2 (HH) excessive growth of the condylar neck, head and ascending ramus with more pronounced asymmetry combined with a vertical growth vector. Type 3 (hybrid: combinations of Type 1 and 2). More recently, Wolford et al. [Citation21] proposed a classification based on clinical features and considered CH a pathological condition that affects the growth of the condylar head, neck and mandible in general. The classification included: condylar hyperplasia Type 1 (CH1), which refers to condylar and horizontal mandibular growth. This form corresponds to Obwegeser’s HE and may present clinically as bilateral symmetrical (CH1A) or unilateral asymmetrical (CH1B). As for condylar hyperplasia type 2 (CH2), a unilateral enlargement of the condylar head, neck, ramus, and body of the mandible caused either by osteochondroma of the condyle (CH2A) or an exophytic osteochondroma (CH2B) is observed. This type correspond to Obwegeser’s HH classification [Citation10]. CH3 relates to hyperplasia associated with rare benign tumours originating from the mandibular condyle and CH4 relates to hyperplasia associated with malignant tumours of condylar origin [Citation21–23].
Obwegeser’s classification system has been the most often used in the description of CH with its distinct types. However, recently a retrospective study using cluster analysis to determine direction of overgrowth in UCH patients, called into question the concept of two distinct vectors of condylar growth (vertical or horizontal). The authors found instead a diagonal growth vector in the majority of patients [Citation24].
Clinical features
The clinical facial and occlusal features vary according to the abnormal growth vector being vertical or horizontal in nature. The abnormal vertical growth (HH) is characterized by three-dimensional enlargements of the affected side of the mandible. An ipsilateral downgrowth of the condyle with minimal midline or chin deviation but significant sloping of the ipsilateral mandibular occlusal plane [Citation5,Citation25,Citation26]. An ipsilateral open bite is usually seen in the initial stages, but the compensatory downward maxillary growth especially in the prepubertal stages on the affected side to maintain occlusion usually results in a substantial occlusal cant. Because of the overgrowth of the dentoalveolar segment, the inferior alveolar bundle remains in its position close to the lower border of the mandible [Citation25]. The whole face appears rotated. The rapid rate of mandibular growth with the maxilla not being able to catch up might also result in a lateral open bite. Dentally, the lower anterior teeth tip towards the affected side. Posterior teeth on the affected side roll in lingually to compensate and maintain the occlusion [Citation5].
On the other hand, the abnormal horizontal growth (HE) is characterized by a deviated chin and mandibular midline to the unaffected side [Citation25]. The lower border of the mandible on both sides lies in the same level, with an absence of open bite and maxillary cant. Dentally, the ipsilateral mandibular molars tend to tip labially to maintain occlusion. Clinically, this clinical presentation resembles functional mandibular lateral deviation [Citation12]. The excessive growth of both the vertical and horizontal planes characterizes the combined form [Citation27]. A hypothesis suggested by Obwegeser to explain the difference with respect to HH, posits that the hyperactivity generating the HE form does not create a ‘real’ CH but rather an elongation of the entire hemimandible terminating at the symphysis, with normal histological traits. He hypothesized that various growth regulators are responsible for the different types of condylar hyperactivity between the two forms [Citation10].
Comprehensive medical history and clinical evaluation are key elements in diagnosis and treatment planning of CH. The progressive asymmetrical growth that presents at puberty aids in the initial diagnosis and should be differentiated from the asymmetrical growth that has been present since birth that suggests another possible aetiology [Citation27]. Moreover, consensus is still lacking in the literature concerning a gold standard for its diagnosis and the histopathological features associated with its development [Citation28,Citation29]; therefore, one cannot rely solely on the histopathological findings for diagnosis [Citation26].
Plain imaging can only be used for initial inspection and screening for CH but cannot be relied upon for definitive diagnosis [Citation30]. Habets et al. [Citation31,Citation32] concluded that 6% vertical height difference between the two sides of the panoramic radiographs resulted in 3% asymmetry. Those images with 3% asymmetry or less were not indicative of true asymmetry but rather the result of technical irregularities [Citation31,Citation32]. Moreover, the use of two consecutive lateral cephalograms (6- to 12-month intervals) has been suggested as a method to assess condylar hyperactivity [Citation23]. Computed tomography (Ct) is of benefit in surgical planning and plays a role in differentiating between the smooth condylar growth in condylar hyperactivity and the bony growth arising from a osteochondroma [Citation33]. Cone-beam CT (CBCT) with the advantage of lower doses than conventional CT is currently used for the virtual three-dimensional (3D) surgical treatment planning [Citation34]. But the most important determinant in the diagnosis of facial asymmetry with CH remains the assessment of condylar activity [Citation35]. The introduction of scintigraphy with the usage of Technetium 99 m-methyl diphosphonate (99mTc-MDP) made it possible to determine the activity or inactivity of the condylar growth centres [Citation36]. Because of the inconsistency and lack of specificity for this technique to distinguish between true condylar growth activity and active hyperplasia, single-photon emission computed tomography (SPECT) has taken an important role in the diagnosis of condylar hyperactivity provided that it has greater ability to show more specifically the condylar hyperactivity; therefore considered more reliable than (99mTc-MDP) [Citation37]. It has been reported that a 10% difference or more between the 2 condyles in SPECT analysis is associated with the active form of CH [Citation38],[Citation26]. However, SPECT cannot differentiate between condylar hyperactivity and infective, inflammatory, or healing conditions [Citation34] and its findings sometimes might be inconclusive in younger patients or slowly progressive hyperplasia [Citation38]. Furthermore, scintigraphy does not clearly discriminate between genuine CH and reactive processes due to arthrosis which may have clinical implications [Citation13]. The latest, positron emission tomography (PET) techniques might be a promising diagnostic tool for CH [Citation39]. Additionally, differential diagnosis must be excluded with other common causes of facial asymmetry including syndromes like hemifacial microsomia, trauma to jaws, and benign or malignant condylar cartilage tumours. Hence, the importance of relating the clinical picture to the radiological and histological findings.
Management
Treatment goals for CH relies in improving both aesthetic and functional outcomes, with limiting further future facial malformation and recurrence. A comprehensive surgical-orthodontic assessment is a must with clear emphasis on the choice of early surgical intervention to lessen the amount of condylar activity, or later intervention after the facial growth has ceased and the condylar activity is burned out [Citation40]. Treatment outcomes rely mainly on patients’ concerns and expectations, condylar growth activity, treatment timing, type of the condylar surgery and the future need for orthognathic surgery [Citation41]. Decision for the appropriate treatment is determined mainly by the pattern of growth activity and the progression of the asymmetry [Citation11,Citation42]. Due to the lack of consensus in classification, different treatment protocols have been published and suggested for the management of unilateral CH [Citation2]. Treatment procedures and clinical management of CH have not been yet standardized, and many surgical protocols have been proposed for its management [Citation2,Citation26,Citation43]. The most common reported treatment options for CH are: orthognathic surgery as a sole treatment, surgical treatment consisting of resection of the temporomandibular joint [(high or low (proportional) condylectomies] or a combination between both, performed in either one or two surgical sessions. The choice of treatment essentially depends on the activity of the condyle and the age of the patient [Citation44]. Majority of the studies recommended early intervention due to the hyperactivity of the condyle which can be addressed at an earlier age ensuring minimum intervention and excellent aesthetic and functional results [Citation26]. Overall, it can be observed that most common treatment options performed in the literature for patients with CH has been high condylectomy with orthognathic surgery carried out at same or later times with articular disc replacement as a variable in case by case option [Citation23,Citation44,Citation45]. Chin asymmetry with a deviation greater than 10 mm from midline are associated with higher demands to correct surgically, taking into consideration that observers can perceive facial asymmetry within 5 mm chin deviation from the midline [Citation46]. Below is a summary of the treatment options for CH, their protocols, efficacy, and reported outcomes.
Orthognathic surgery for CH
Usually considered an option once the disease is inactive due to self-limiting course of the disease or previous condylar surgery. Mainly aims to restore facial and jaws balance, aesthetics, and function. Bilateral ramus osteotomy has been reported in the literature since the early 50’s as a treatment option for non-growing patients with facial deformities because of CH [Citation47–49]. Motamedi [Citation50] evaluated 13 cases (12 men and 1 woman, mean age 25.8 years) of CH treated with mandibular ramus osteotomy (7 had bilateral osteotomies, 6 had unilateral, 2 were combined with maxillary LeForte osteotomy) throughout the 10 year period. His study showed favourable outcomes with unilateral ramus osteotomy of the affected side, bilateral osteotomies had no extra advantage, and combination with LeForte 1 osteotomy was effective in restoring occlusal canting in dentally compensated cases. He further stated that the procedure is not universally applicable in all cases and precise preclinical assessment is usually needed. In borderline cases, the operation should be performed on the affected side first, if things go as planned, surgery must be avoided on the opposite side [Citation50]. Choung & Nam [Citation51] presented a case series of 4 patients with CH surgically treated with vertical and sagittal intraoral ramus osteotomies with complete extraction of the condylar segment and remodelling the condyle with drills. After 3 years follow-up, condyles showed no signs of resorption or necrosis and had normal functionality. Posnick et al. [Citation3] in a retrospective cohort aimed to assess the occlusal stability and mandibular growth, 2 years after surgery, in 76 subjects younger than 26 years old, (age range: 14–25) whom underwent bimaxillary orthognathic surgery to treat HE. The authors found that favourable occlusion can be achieved and maintained long term. There was no need for an ablative open joint procedure to arrest condylar growth in any of their included subjects. Vernucci et al. [Citation52] in a population of 128 subjects with unilateral hemimandibular hyperactivity reported that canting of the maxillary occlusal plane measured on an articulator or CBCT is an important parameter to determine the proper orthodontic surgical approach. If the canting is over 5 mm, the complete correction of the maxillary occlusal plane needs a surgical upward rotation of the over-erupted maxillary side (‘V shape’ LeFort I osteotomy) followed by orthodontic therapy; intrusion of the posterior teeth on the affected side can be also dealt with using miniplates. They further illustrated that in cases where the condyle is not active, orthodontic surgical combined treatment with the classic three phases of pre-surgical preparation, orthognathic surgery, and post-surgical orthodontics, remains the best option.
TMJ surgery (high or low condylectomies) with or without orthognathic surgery
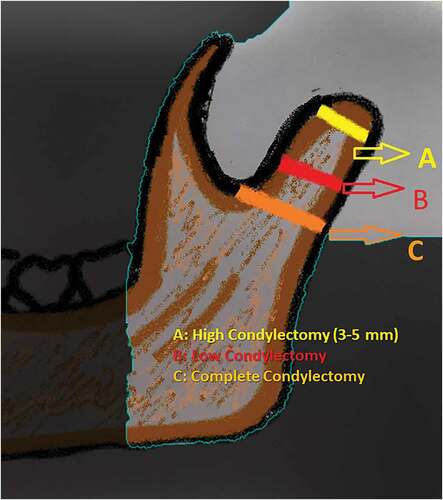
This is the most common treatment option in cases of active condylar growth based on the fact that resection of growth centre is essential to prevent relapse [Citation10]. It can be carried alone or with orthognathic surgery. The term condylectomy refers to several procedures: low (proportional), high condylectomy, and complete condylectomy (). In the classic definition condylectomy refers to complete removal of the condyle and the subsequent joint reconstruction.
The term low (proportional) condylectomy refers to the removal of the active portion of the condyle in cases of TMJ tumours and additionally resecting some of the bone on the affected side to match the unaffected side, thus correcting the mandibular height. When low condylectomy is used for the removal of osteochondroma, the healthy side is used as a reference to level the occlusal plane [Citation53–55]. On the other hand, the term high condylectomy refers to the removal of the most superior aspect of the mandibular condyle (5 mm), which is considered the most active growth region of the condylar head [Citation45]. The presence of condylar activity is a very important parameter for this therapeutic approach. It has been suggested that condylectomy stops the condylar overgrowth and eliminates the future asymmetry [Citation10]. Contouring, osteotomies, grafts and genioplasty might be done if needed to improve facial symmetry [Citation56,Citation57].
The timing of these surgeries is a subject of debate [Citation21,Citation25,Citation58]. There is no agreement on when to perform condylectomy; those who advice against it are cautious about functional alterations of the TMJ [Citation59,Citation60]. Brusati et al. [Citation56] evaluated articular function in 15 patients (mean age 22) whom underwent high condylectomy and found that postoperative articular function was satisfactory but not excellent. In fact, function was only good if the patient followed the postoperative physiotherapy schedule. Therefore, condylectomy can be considered for the elective treatment of active CH in adults and is more advisable for treatment of younger patients. However, An age over 18 years old has been reported as a gold standard for condylectomy [Citation12]. Some studies reported lower risk of relapse and more stable outcomes when condylectomy is performed for adults compared to adolescents [Citation5,Citation21–23,Citation55]. Two standard scintigraphic measurements of bone activity within 6 months are usually required to indicate the presence of active growth in which condylectomy should be performed [Citation45,Citation58]. On the other hand, some authors suggested a routine yearly scintigraphic measurements in growing patients when visible signs of mandibular asymmetry and deformity are present, which might help determine the best time for surgical intervention [Citation5,Citation36,Citation58]. Early intervention ensures excellent aesthetic and facial outcomes and minimize future intervention when combined with orthodontics. Wolford et al. suggested early intervention for females on average at 14 years old and 16 years old for males. The authors further state the need for a second surgical intervention in the group of patients that underwent only orthognathic surgery to correct their asymmetry, while those who underwent orthognathic surgery and high condylectomy relapse was not seen [Citation22,Citation23]. Moreover, Abotaleb et al. stated that it may be necessary to do early high condylectomy once the diagnosis is confirmed [Citation40].
Small asymmetries with relatively stable occlusion and less dentoalveolar discrepancies might possibly be treated with condylectomy and osteomodelling or/and orthognathic surgery. Larger discrepancies due to increased growth in all three dimensions should be addressed with surgery in sequential treatment staging [Citation45]. Progressive jaw asymmetry that develops within a short-time frame is an indication for condylectomy to prevent the accentuation of the asymmetry [Citation10,Citation23]. It should be kept in mind that amount of excised condyle might also be responsible for autorotation of the unaffected condyle to the affected side (excised side) which could influence the later mandibular position that will affect future surgeries and orthodontic treatment [Citation12].
Indications and effectiveness prognosis of high and low condylectomies
High condylectomy
High condylectomy has been a common technique for treating active UCH. There is an increased number of chondrocytes with an increased production of connective tissue associated with CH [Citation53]. Thus, when the upper layers of the condyle are compromised, a high condylectomy could contribute to restricting aberrant growth of the condylar head [Citation14].
The literature offers different perspectives and treatment modalities for high condylectomy. It is yet not clear whether high condylectomy as a solo surgical procedure is sufficient to correct asymmetry [Citation26]. The efficacy of high condylectomy on its own has been investigated in a group of 36 adult subjects (mean age = 22.7 years), in which this surgical procedure was performed (4 mm to 5 mm from the upper pole of the condyle). In this study, only six subjects required a secondary orthognathic surgery [Citation44]. The use of CBCT radiographs in another study of 25 subjects (mean age 23) with UCH showed that orthodontic treatment with high condylectomy is effective in correcting facial asymmetry [Citation61]. Jones and Tire [Citation45] treated a group of 17 subjects in a case series with high condylectomy and simultaneous orthognathic surgery and found relatively satisfactory outcomes in all cases. Moreover, in a retrospective study of 27 patients with CH [mean age of 22.8 years for the HE and HH group and 47 years for the osteochondroma group (OC)] who underwent high condylectomy, secondary jaw surgery was less required in patients with HE (26.7%) than patients with HH (100%). Compensatory growth in the OC was the mildest, therefore orthodontic treatment was minor and asymmetry was resolved by removing the hyperplastic tissues. Asymmetry may persist in HH due to the hyperplasia in the mandible and body region that necessitates an additional surgery [Citation62]. In an updated CH classification, Wolford et al. [Citation23] placed high condylectomy with disc repositioning and orthognathic surgery as the preferred treatment for unilateral and bilateral CH. More recently, Abotaleb et al. [Citation40] indicated the efficacy of a single-stage high condylectomy and orthognathic surgery in adults, and stated that despite the termination of the disease and aesthetic improvement associated with high condylectomy in early adolescence, constant orthodontist-surgeon follow-up is required.
Therefore, it seems like high condylectomy is commonly performed in adults. Despite the fact that high condylectomy alone with postoperative orthodontic treatment has achieved relatively satisfactory outcomes [Citation22], it yielded more predictable and stable outcomes when performed with simultaneous orthognathic surgery in the same surgical session. In studies in which high condylectomies were reported as the sole treatment for CH, there was a high chance that these cases could have possibly better managed with proportional condylectomy instead [Citation63].
As for the effects of high condylectomy on jaw function, it has been indicated that high condylectomy plays a role in the improvement of functional occlusion besides facial aesthetics [Citation64]. In six adult patients’ (mean age 27 years) whomwho underwent Le Fort I osteotomy and high condylectomy [Citation14], jaw function was not impaired, maximum interincisal opening was not affected and patients were pain free.
Low (proportional) condylectomy
The proportional condylectomy protocol was initially proposed by Delaire to solve the aetiology of CH by resecting the condylar growth centre and correcting the mandibular malformation [Citation65]. Preoperative cephalometric analysis was used to determine the resection size needed. This approach relied on estimating the vertical distance between the mandibular angles [Citation65] and included a full removal of the cartilaginous cap. The articular disk was preserved, and additional surgical procedures were needed (maxillary osteotomy, contralateral sagittal split ramus osteotomy, inferior border ostectomy, and genioplasty). Early active functional rehabilitation, consisting of lateral deduction and centred propulsion, was repeated several times a day. In addition, intermaxillary elastics were used postoperatively to aid the condylar stump reach the glenoid fossa. The clinical efficacy of this protocol was evaluated retrospectively in 73 patients with UCH whom had proportional condylectomy at the age of 24 years [Citation2]. It was concluded that proportional condylectomy was an effective method to solve both CH and the adaptive deformation.
The advantage of proportional condylectomy lies primarily in reducing the need for a secondary orthognathic surgery. The average reported age to perform proportional condylectomy was 19 years old in majority of the studies [Citation2,Citation63,Citation66,Citation67], which indicates a potentially greater capacity at an earlier age for condylar remodelling and adaptation of hard and soft tissues, providing some evidence that proportional condylectomy might help avoid secondary orthognathic surgery (). Farina et al. [Citation53] in a retrospective descriptive observational study of 16 patients with active CH (age ranged between 14 and 33 years old) whom were treated with low condylectomy recommended this procedure due to its ability to resolve the aetiology of hyperplasia and allow occlusal, facial and skeletal alterations produced by pathology to be alleviated; thus, reducing the chances of performing orthognathic surgery at a later stage. They also stressed on the importance of the postoperative functional therapy phase with elastic bands which play an integral role in regaining mandibular function [Citation56,Citation68]. Recently, an updated protocol based on computer-guided surgical technique was proposed in which the position of the resection plane relies on 3D virtual mirroring, the definition of the vertical discrepancies, and a custom designed surgical cutting guide used to transfer the virtual plan to the surgical field. This method allowed more predictability and precision in the technique [Citation67]. Moreover, proportional condylectomy is usually performed at a level lower than what is considered high condylectomy allowing the attainment of equal posterior facial heights between the hyperplastic and the healthy sides, preserving functionality and stability of the articulation without complications [Citation55].
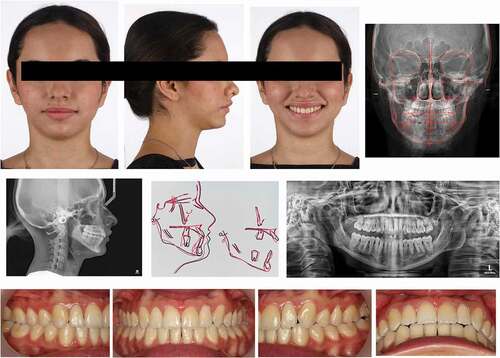
Figure 2. Pretreatment records of a 21 year-old female patient with UCH diagnosed through clinical examination with periodic follow ups and bone scintigraphy. Clinical presentation was consistent with HE (Obwegeser classification) or CH type 1 (Wolford classification)
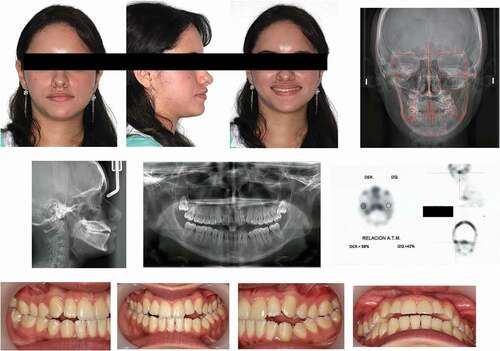
Figure 3. Low (proportional) condylectomy of the right condyle with removal of approximately 9 mm of the condylar head. Dental midlines matched in the operating table

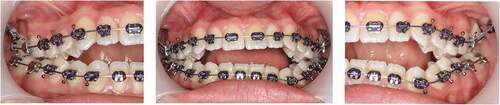
Figure 4. Resulting anterior openbite after the proportional condylectomy. Temporary Anchorage devices (mini-implants) placed in the malar bone emerging through the buccal aspect of the maxillary first molars to intrude the maxillary posterior segment and correct the overbite
In a current systematic review that has evaluated the efficacy for both proportional and high condylectomy, it was shown that proportional condylectomy was considered superior to high condylectomy and was recommended as the treatment option in cases of osteochondroma due to the active and constant growth associated with this benign neoplasm. Furthermore, proportional condylectomy can be used as an initial treatment replacing high condylectomy for clinical cases with increased growth activity and prominent asymmetry and can be considered as a sole treatment in cases with mild or even moderate midline deviation and mandibular occlusal canting [Citation66].
The current literature indicates a wide scope of proposed aetiology, diagnostic tools, preferred time of intervention and treatment option for CH. Therefore, further well-constructed comparative studies are necessary to determine the right procedure for best aesthetic and functional outcomes [Citation26].
Conclusions
CH involves the increased growth of the mandibular condyles and occurs in adolescents and adults. Different classification systems have been proposed that are based on the growth vectors involved and the unilateral or bilateral involvement of the mandibular condyles. The diagnosis relies primarily on clinical evaluation and radiographic imaging. Condylectomies with and without orthognathic surgery appear as a treatment approach that is able to arrest the asymmetric clinical manifestations and may reduce the extent of a developing asymmetry with growth.
Ethics approval
This review article does not require an approval by an ethics committee.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Karssemakers L, Nolte J, Tuinzing D, et al. Microcomputed tomographic analysis of human condyles in unilateral condylar hyperplasia: increased cortical porosity and trabecular bone volume fraction with reduced mineralisation. Br J Oral Maxillofacial Surg. 2014;52(10):940–944.
- Mouallem G, Vernex-Boukerma Z, Longis J, et al. Efficacy of proportional condylectomy in a treatment protocol for unilateral condylar hyperplasia: a review of 73 cases. J Craniomaxillofac Surg. 2017;45(7):1083–1093.
- Posnick JC, Perez J, Chavda A. Hemimandibular elongation: is the corrected occlusion maintained long-term? Does the mandible continue to grow? J Oral Maxillofacial Surg. 2017;75(2):371–398.
- Raijmakers PG, Karssemakers LH, Tuinzing DB. Female predominance and effect of gender on unilateral condylar hyperplasia: a review and meta-analysis. J Oral Maxillofacial Surg. 2012;70(1):e72–e76.
- Nitzan DW, Katsnelson A, Bermanis I, et al. The clinical characteristics of condylar hyperplasia: experience with 61 patients. J Oral Maxillofacial Surg. 2008;66(2):312–318.
- Alyamani A, Abuzinada S. Management of patients with condylar hyperplasia: a diverse experience with 18 patients. Ann Maxillofac Surg. 2012;2(1):17.
- Gray R, Sloan P, Quayle A, et al. Histopathological and scintigraphic features of condylar hyperplasia. Int J Oral Maxillofac Surg. 1990;19(2):65–71.
- Matteson SR, Proffit WR, Terry BC, et al. Bone scanning with 99m technetium phosphate to assess condylar hyperplasia: report of two cases. Oral Surg Oral Med Oral Pathol. 1985;60(4):356–367.
- Angiero F, Farronato G, Benedicenti S, et al. Mandibular condylar hyperplasia: clinical, histopathological, and treatment considerations. CRANIO®. 2009;27(1):24–32.
- Obwegeser HL, Makek MS, 1986, Hemimandibular hyperplasia—hemimandibular elongation. J maxillofacial surg. 14:183–208.
- Rodrigues DB, Castro V. Condylar hyperplasia of the temporomandibular joint: types, treatment, and surgical implications. Oral Maxillofacial Surg Clin. 2015;27(1):155–167
- Nelke KH, Pawlak W, Morawska-Kochman M, et al. Ten years of observations and demographics of hemimandibular hyperplasia and elongation. J Craniomaxillofac Surg. 2018;46(6):979–986.
- Slootweg PJ, Müller H, 1986, Condylar hyperplasia. A clinico-pathological analysis of 22 cases. J Maxillofac surg. 14:209–214.
- Lippold C, Kruse-Losler B, Danesh G, et al. Treatment of hemimandibular hyperplasia: the biological basis of condylectomy. Br J Oral Maxillofacial Surg. 2007;45(5):353–360.
- Chia MS, Naini FB, Gill DS. The aetiology, diagnosis and management of mandibular asymmetry. Orthodontic Update. 2008;1(2):44–52
- Obwegeser HL, Obwegeser JA. New clinical-based evidence for the existence of 2 growth regulators in mandibular condyles: hemimandibular elongation in hemifacial microsomia mandible. J Craniofacial Surgery. 2010;21(5):1595–1600.
- Götz W, Lehmann TS, Appel TR, et al. Distribution of insulin-like growth factors in condylar hyperplasia. Ann Anat. 2007;189(4):347–349.
- Chen Y, Ke J, Long X, et al. Insulin-like growth factor-1 boosts the developing process of condylar hyperplasia by stimulating chondrocytes proliferation. Osteoarthritis Cartilage. 2012;20(4):279–287.
- Eslami B, Behnia H, Javadi H, et al. Histopathologic comparison of normal and hyperplastic condyles. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2003;96(6):711–717.
- Adams R, editor. Case history of Mary Keefe. Medical Section of the British Association, Bristol Meeting; 1836.
- Wolford LM, Movahed R, Perez DE. A classification system for conditions causing condylar hyperplasia. J Oral Maxillofacial Surg. 2014;72(3):567–595.
- Wolford LM, Mehra P, Reiche-Fischel O, et al. Efficacy of high condylectomy for management of condylar hyperplasia. Am J Orthod Dentofacial Orthop. 2002;121(2):136–151.
- Wolford LM, Morales-Ryan CA, García-Morales P, et al., editors. Surgical management of mandibular condylar hyperplasia type 1. Baylor University Medical Center Proceedings. Taylor & Francis; 2009.
- Gateno J, Coppelson KB, Kuang T, et al. A Better Understanding of Unilateral Condylar Hyperplasia of the Mandible. J Oral Maxillofac Surg. 2021 May;79(5):1122–1132.
- Obwegeser H, Makek M. Hemimandibular hyperplasia—Hemimandibular elongation. Plast Reconstr Surg. 1987;80(2):327.
- Ghawsi S, Aagaard E, Thygesen TH. High condylectomy for the treatment of mandibular condylar hyperplasia: a systematic review of the literature. Int J Oral Maxillofac Surg. 2016;45(1):60–71.
- Higginson J, Bartram A, Banks R, et al. Condylar hyperplasia: current thinking. Br J Oral Maxillofacial Surg. 2018;56(8):655–662.
- Hansson T, Öberg T, Carlsson GE, et al. Thickness of the soft tissue layers and the articular disk in the temporomandibular joint. Acta Odontol Scand. 1977;35(1–3):77–83.
- Richards L, Lau E, Wilson D. Histopathology of the mandibular condyle. J Oral Pathol Med. 1985;14(8):624–630.
- Nolte J, Karssemakers L, Grootendorst D, et al. Panoramic imaging is not suitable for quantitative evaluation, classification, and follow up in unilateral condylar hyperplasia. Br J Oral Maxillofacial Surg. 2015;53(5):446–450.
- Habets L, Bezuur J, Naeiji M, et al. The Orthopantomogram®, an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J Oral Rehabil. 1988;15(5):465–471.
- Habets L, Bezuur J, Van Ooij C, et al. The orthopantomogram, an aid in diagnosis of temporomandibular joint problems. I. The factor of vertical magnification. J Oral Rehabil. 1987;14(5):475–480.
- Andrade NN, Gandhewar TM, Kapoor P, et al. Osteochondroma of the mandibular condyle–Report of an atypical case and the importance of computed tomography. J Oral Biol Craniofac Res. 2014;4(3):208–213.
- Shintaku WH, Venturin JS, Langlais RP, et al. Imaging modalities to access bony tumors and hyperplasic reactions of the temporomandibular joint. J Oral Maxillofacial Surg. 2010;68(8):1911–1921.
- Bohuslavizki K, Brenner W, Kerscher A, et al. The value of bone scanning in pre-operative decision-making in patients with progressive facial asymmetry. Nucl Med Commun. 1996;17(7):562–567.
- Wen B, Shen Y, Wang C-Y. Clinical value of 99Tcm-MDP SPECT bone scintigraphy in the diagnosis of unilateral condylar hyperplasia. Sci World J. 2014;2014.
- Hodder S, Rees J, Oliver T, et al. SPECT bone scintigraphy in the diagnosis and management of mandibular condylar hyperplasia. Br J Oral Maxillofacial Surg. 2000;38(2):87–93.
- Saridin C, Raijmakers P, Al Shamma S, et al. Comparison of different analytical methods used for analyzing SPECT scans of patients with unilateral condylar hyperactivity. Int J Oral Maxillofac Surg. 2009;38(9):942–946.
- Laverick S, Bounds G, Wong WL. [18F]-fluoride positron emission tomography for imaging condylar hyperplasia. Br J Oral Maxillofacial Surg. 2009;47(3):196–199.
- Abotaleb B, Bi R, Telha W, et al. Treatment measures of hemimandibular hyperplasia and associated facial deformities. J Craniomaxillofac Surg. 2021;49(2):126–134.
- Almeida LE, Zacharias J, Pierce S. Condylar hyperplasia: an updated review of the literature. Korean J Orthod. 2015;45(6):333.
- Di Blasio C, Di Blasio A, Pedrazzi G, et al. How does the mandible grow after early high condylectomy? J Craniofacial Surgery. 2015;26(3):764–771.
- Chiarini L, Albanese M, Anesi A, et al. Surgical treatment of unilateral condylar hyperplasia with piezosurgery. J Craniofacial Surgery. 2014;25(3):808–810.
- Villanueva-Alcojol L, Monje F, González-García R. Hyperplasia of the mandibular condyle: clinical, histopathologic, and treatment considerations in a series of 36 patients. J Oral Maxillofacial Surg. 2011;69(2):447–455.
- Jones RHB, Tier GA. Correction of facial asymmetry as a result of unilateral condylar hyperplasia. J Oral Maxillofacial Surg. 2012;70:1413–1425.
- Naini FB, Donaldson ANA, McDonald F, et al. Assessing the influence of asymmetry affecting the mandible and chin point on perceived attractiveness in the orthognathic patient, clinician, and layperson. J Oral Maxillofacial Surg. 2012;70(1):192–206.
- Gottlieb O. Hyperplasia of the mandibular condyle. J oral surg. 1951;9(2):118–135.
- Rowe N. Aetiology, clinical features, and treatment of mandibular deformity. Br Dent J. 1960;108:45–64.
- Hinds EC, Reid LC, Burch RJ. Classification and management of mandibular asymmetry. Am J Surg. 1960;100(6):825–834.
- Motamedi MHK. Treatment of condylar hyperplasia of the mandible using unilateral ramus osteotomies. J Oral Maxillofacial Surg. 1996;54(10):1161–1169.
- Choung P-H, Nam I-W. An intraoral approach to treatment of condylar hyperplasia or high condylar process fractures using the intraoral vertico-sagittal ramus osteotomy. J Oral Maxillofacial Surg. 1998;56(5):563–570.
- Vernucci RA, Mazzoli V, Galluccio G, et al. Unilateral hemimandibular hyperactivity: clinical features of a population of 128 patients. J Craniomaxillofac Surg. 2018;46(7):1105–1110.
- Fariña R, Pintor F, Pérez J, et al. Low condylectomy as the sole treatment for active condylar hyperplasia: facial, occlusal and skeletal changes. An observational study. Int J Oral Maxillofac Surg. 2015;44(2):217–225.
- Mehra P, Arya V, Henry C. Temporomandibular joint condylar osteochondroma: complete condylectomy and joint replacement versus low condylectomy and joint preservation. J Oral Maxillofacial Surg. 2016;74(5):911–925.
- Wolford LM, Movahed R, Dhameja A, et al. Low condylectomy and orthognathic surgery to treat mandibular condylar osteochondroma: a retrospective review of 37 cases. J Oral Maxillofacial Surg. 2014;72(9):1704–1728.
- Brusati R, Pedrazzoli M, Colletti G. Functional results after condylectomy in active laterognathia. J Craniomaxillofac Surg. 2010;38(3):179–184.
- Deleurant Y, Zimmermann A, Peltomäki T. Hemimandibular elongation: treatment and long‐term follow‐up. Orthod Craniofac Res. 2008;11(3):172–179.
- Vásquez B, Olate S, Cantín M, et al. Histomorphometric analysis of unilateral condylar hyperplasia in the temporomandibular joint: the value of the condylar layer and cartilage island. Int J Oral Maxillofac Surg. 2017;46(7):861–866.
- Bertolini F, Bianchi B, De Riu G, et al. Hemimandibular hyperplasia treated by early high condylectomy: a case report. Int j adult orthodontics orthognathic surg. 2001;16(3): 227–234
- Marchetti C, Cocchi R, Gentile L, et al. Hemimandibular hyperplasia: treatment strategies. J Craniofac Surg. 2000;11(1):46–53.
- Wu C, Meng Q, Deng M, et al. Cone–beam computed tomographic analysis of maxillary and mandibular changes after high condylectomy combined with orthodontic treatment for active unilateral condylar hyperplasia. Br J Oral Maxillofacial Surg. 2018;56(8):692–697.
- Kim J-Y, Ha T-W, Park J, et al. Condylectomy as the treatment for active unilateral condylar hyperplasia of the mandible and severe facial asymmetry: retrospective review over 18 years. Int J Oral Maxillofac Surg. 2019;48(12):1542–1551.
- Fariña R, Olate S, Raposo A, et al. High condylectomy versus proportional condylectomy: is secondary orthognathic surgery necessary? Int J Oral Maxillofac Surg. 2016;45(1):72–77.
- Meng Q-G, Li Y-J, Long X, et al. Condylar and occlusal changes after high condylectomy and orthodontic treatment for condylar hyperplasia. J Huazhong Univ Sci Technol Med Sci. 2015;35(2):265–270.
- Delaire J, Gaillard A, Tulasne J. The place of condylectomy in the treatment of hypercondylosis. Revue de Stomatologie et de Chirurgie Maxillo-faciale. 1983;84(1):11–18.
- Nino-Sandoval TC, Maia FPA, Vasconcelos BC. Efficacy of proportional versus high condylectomy in active condylar hyperplasia—a systematic review. J Craniomaxillofac Surg. 2019;47(8):1222–1232.
- Sembronio S, Tel A, Costa F, et al. An updated protocol for the treatment of condylar hyperplasia: computer-guided proportional condylectomy. J Oral Maxillofacial Surg. 2019;77(7):1457–1465.
- Pantoja R, Martinez B, Encina S, et al. Vertical condylar hyperplasia, clinical and histologic aspects. Apropos of 2 cases. Revue de Stomatologie et de Chirurgie Maxillo-faciale. 1994;95(4): 285–291