Abstract
Objective
MR-pro ANP is a novel peptide with multiple biological functions, especially within the cardiovascular system. It plays an important role in physiological and pathological processes in the human body and its level may be clinically relevant in new onset atrial fibrillation. The aim of this study was to determine whether elevated MR-proANP level is a predictor of new-onset atrial fibrillation in patients with acute myocardial infarction.
Methods and results
The study included 96 patients with their first diagnosis of acute myocardial infarction hospitalized in the Department of Interventional Cardiology within one year. The plasma levels of MR-proANP were determined on admission, and on the first and fifth day of hospitalisation by BRAHMS MRproANP KRYPTOR. New onset AF was diagnosed in 9.4% of patients during hospitalisation; the level of MR proANP was also found to be significantly higher in this group of patients compared to those without arrhythmia (p = 0.017). ROC curve analysis indicates that the concentration of MR-proANP is a good predictor of AF diagnosed during the hospitalisation in patients with acute myocardial infarction (AUC = 0.738, p = 0.0011).
Conclusions
MR-proANP might be a good predictor of new-onset atrial fibrillation in patients with acute myocardial infarction.
Introduction
MR-pro ANP is a novel peptide with multiple biological functions, especially in the cardiovascular system. Interest has grown in its role as biomarker over the last few years.
Atrial natriuretic peptide (ANP) plays an important role in the regulation of many physiological and pathophysiological pathways.
ANP is synthesized and secreted by cardiac muscle cells in the walls of the atria in the heart. These cells contain volume receptors which respond to the stretching of the atrial wall due to increased atrial blood volume.
MR – pro ANP concentration in the human body can be analysed by a new sandwich immunoassay that recognizes a midregional sequence of pro – ANP. It has been hypothesized that MR – pro ANP may be a more valuable marker than ANP or its precursor fragments due to its greater analytical stability, longer half-life and lack of receptor binding and protein interactions (Morgenthaler et al. Citation2004, Idzikowska and Zielińska Citation2018).
MR-proANP level is believed to play a significant role in atrial fibrillation (AF). It is the most common form of arrhythmia, affecting up to 2–3% of the population. Its prevalence increases with age, affecting 0.12%–0.16% of the population under 50 years old, 3.7%–4.2% aged 60–70 years and 10%–17% aged over 80 years; it is also more common in men than women (Zoni-Berisso et al. Citation2014). The most common risk factors for AF are cardiovascular diseases such as arterial hypertension, valvular heart disease, heart failure and coronary artery disease (Anumonwo and Kalifa Citation2014).
Although new onset of AF is known to increase morbidity and mortality in patients with acute coronary syndrome – ST segment elevation myocardial infarction (STEMI) (Lehto et al. Citation2005), no large studies have assessed the significance of MR-proANP levels in these patients.
The aim of this study was to determine whether elevated MR-proANP level is a predictor of new-onset atrial fibrillation in patients with myocardial infarction.
Clinical significance
MR-proANP level may be used as:
A good predicting factor of new-onset atrial fibrillation.
A prognostic biomarker for impaired LV systolic function.
A prognostic biomarker for left atrium enlargement.
Methods
Study population
The study included 96 patients who were admitted to our clinic with the first diagnosis of AMI (STEMI/NSTEMI) within one year. Exclusion criteria were age below 18 years old and over 80 years old, a diagnosis of chronic kidney disease (eGFR < 30), any history of cancer in the previous five years, any history of atrial fibrillation, and conservative treatment of myocardial infarction (patients who did not undergo percutaneous coronary intervention – PCI).
The study was approved by the local bioethical committee and all patients gave their informed consent to take part.
Study protocol
All patients qualified for the study were admitted to the clinic and coronary angiography with subsequent PCI was performed. Standard pharmacological therapy was administered in all eligible patients.
A series of clinical and demographic data was collected, including sex and age as well as various histories: hypertension, coronary artery disease, heart failure, hypercholesterolaemia, diabetes mellitus, chronic kidney disease and cigarette smoking. Heart rate, blood pressure and haemodynamic state were also assessed in all cases. Echocardiography was performed in all patients during the hospitalisation: ejection fraction was assessed using Simpson’s method and left atrial volume index was calculated from apical four and two chamber views. Standard laboratory tests were also performed for myocardial infarction.
The diagnosis of atrial fibrillation (defined as irregular ventricular rate and absence of P-waves) was based on continuous ECG monitoring performed during the entire hospitalisation. All qualified patients reported being free of any clinical signs of arrhythmia in the past.
MR-proANP assay
Venous blood samples were drawn three times during hospitalisation: on admission to hospital, on the first day of hospitalisation and on the fifth day. Blood samples were centrifuged and then all tubes with plasma were frozen and then stored below −20 C until assay.
The MR-proANP assay was performed using BRAHMS MR-proANP KRYPTOR.
Statistical analysis
Categorical variables were summarized as frequencies with percentage values. Continuous variables were expressed as medians with interquartile range. The Shapiro-Wilk test was used to confirm whether the variables were normally distributed: those without a normal distribution were analysed using non-parametric statistics. Correlations were assessed using Spearman’s rank correlation coefficient. Continuous variables were compared using the Mann-Whitney U-test, and categorical variables using chi-squared tests with Yates’s correction for continuity. ROC curves were used to assess the suitability of MR-proANP levels in predicting new onset AF.
All statistical analyses were performed using STATISTICA 13.3 (StatSoft Inc, USA). A p-value <0.05 was considered statistically significant.
Results
Our cohort consisted of 96 patients, aged 65 (58; 71) years, 33% of whom were women. Of this group, 53% of patients were admitted with a diagnosis of STEMI of the inferior wall. A diagnosis of NSTEMI was noted among 23% of all patients. Eighty six percent of patients were in Killip class I. The majority of patients were diagnosed with two-vessel disease by coronary angiography. In total, 9.4% (9/96) of the patients were diagnosed with the new onset atrial fibrillation. Other clinical features of the group, and concomitant therapy, are presented in .
Table 1. Patients characteristics, coronary angiography findings and concomitant treatment in whole study group on admission to hospital.
Mean MR-proANP levels were significantly higher on admission than on the first and fifth day of hospitalisation. The mean MR-proANP plasma concentration was 151.2 pmol/L (range 99.9–282.7) on admission, 99.03 pmol/L (81.6–174.7) on the first day of hospitalisation, and 104.6 pmol/L (78.6–164.8) on the fifth day.
At all three time points, moderate correlations were observed between the MR-proANP concentration vs age (p = <0.001; R = 0.44, p = <0.001; R = 0.52, p = <0.001; R = 0.54) and weaker correlations were found between MR-proANP vs systolic blood pressure (p = 0.005; R= −0.27, p = 0.007; R= −0.26, p = 0.035; R= −0.21) .
At all three time points, no relationship was observed between MR-proANP levels and sex, heart rate, history of hypertension, hyperlipidaemia, heart failure, prior myocardial infarction, diabetes, obesity or smoking. However, Killip class > I on admission was associated with higher values of MR-proANP (p = 0.105 on admission, p = 0.0134 on day 1, p = 0.0330 on day 5) as was renal failure.
Patients with normal systolic LV function had lower values of MR-proANP than those with impaired systolic LV function (p = 0.005 on admission, p = <0.001 on day 1, p = <0.001 on day 5). A moderate relationship was also observed between MR-proANP and left atrial volume index (LAVI): the patients with an enlarged left atrium demonstrating a higher level of MR – proANP. This relationship was observed for all three measurements (p = <0.001; R > 0.4).
Four deaths occurred during hospitalisation. Those who died did not differ significantly from the survivors in terms of MR-proANP concentration at any of the three time points.
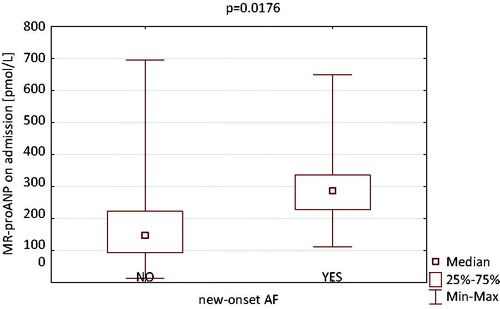
The most interesting discovery was that patients with significantly higher levels of MR-proANP assessed on admission were significantly more likely to be diagnosed with new onset atrial fibrillation during hospitalisation, compared to those with lower levels (p = 0.017; ).
Figure 1. The comparison of MR-proANP concentration between patients with new onset-atrial fibrillation and without one.
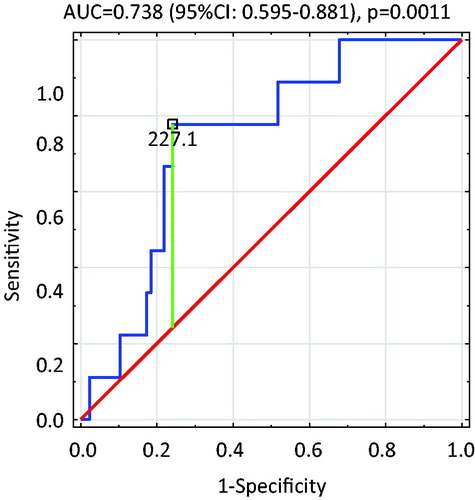
The ROC curve analysis indicated that MR-proANP concentration was a strong predictor of AF diagnosed during the hospitalisation in patients with acute coronary syndrome (AUC = 0.738, 95%CI; 0.595–0.881; p = 0.0011; ). The cut-off value for MR-proANP was calculated as 227.1 pmol/L, with the OR of the new-onset AF being 11.0 (95%CI; 2.12–57.07).
Figure 2. ROC curve-variable tested: the concentration of MR-proANP on admission in identifying patients at risk of AF during hospitalisation in patients with ACS.
Univariate logistic regression analysis of the range of data collected on admission found only MR-proANP level assessed on admission and age to be significant factors predicting AF (p = 0.0351, p = 0.0300 respectively). ROC curve analysis found MR-proANP concentration to be a stronger predictor of new-onset AF than NT-proBNP concentration (AUC = 0.74 vs AUC= 0.521; p = 0.0142).
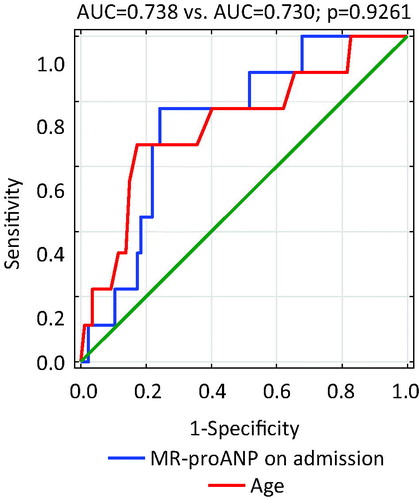
A comparison of the ROC curves of MR-proANP and age found no significant differences in AUC (0.738; 95%CI; 0.595–0.881 vs 0.73 95%CI 0.546–0.913; p = 0.9261; ), suggesting that age is also a good predictor of new-onset AF. The cut-off value for age was 72 years old.
Stepwise forward logistic regression analysis found only MR-proANP assessed on admission to be a significant factor predicting new-onset AF (p = 0.0351).
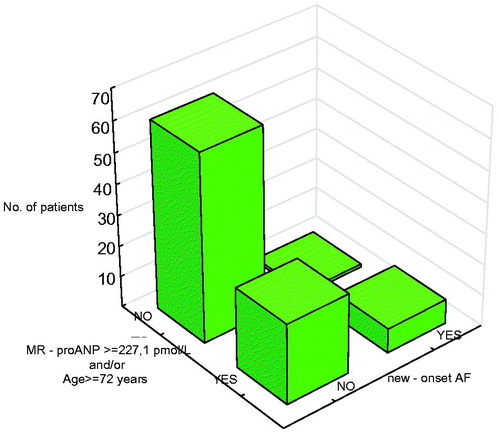
A simple algorithm for assessing the risk of AF in patients with acute coronary syndrome was prepared based on cut-off levels from ROC curves. The patients were divided into two groups: younger patients (<72 years old) with a low level of MR-proANP (<227.1 pmol/L) (group 1) and others (group 2). It was found that the older patients and those with a higher concentration of MR-proANP demonstrated a significantly higher chance of atrial fibrillation during hospitalisation: more than 18-fold higher (). This observation could be important when choosing suitable antiplatelet treatment (clopidogrel/ticagrelor/prasugrel) for use with anticoagulant therapy.
Discussion
No large studies assessing the significance of MR-proANP levels have so far been performed in patients with new- onset AF and acute coronary syndrome. However, elevated plasma NT-proBNP level has been found to be a strong predictor of new-onset AF in patients with acute myocardial infarction (p = 0.004) (Dorje et al. Citation2013), and NT-proBNP has demonstrated significant prognostic value in patients with myocardial infarction, with high concentrations being associated with a greater risk of developing new-onset atrial fibrillation (Parashar et al. Citation2010). In the present study, ROC curve analysis of MR-proANP and NT-proBNP concentrations on admission found MR-proANP concentration to be a stronger predictor of new-onset AF than NT-proBNP (AUC = 0.74 vs AUC = 0.521; p = 0.0142).
A meta-analysis of the prognostic role of left ventricular ejection fraction (LVEF) and left atrial diameter in the occurrence of AF after acute myocardial infarction (AMI) found lower LVEF levels to be associated with new-onset AF occurrence after myocardial infarction and increased left atrium diameter levels to be related to greater risk of new-onset AF following AMI. The analysis included 10 studies including a total of 7493 patients. Patients were divided into two groups: AF group and non – AF group (Zeng et al. Citation2017).
However, our present findings indicate a relationship between the levels of MR-proANP and left ventricular ejection fraction; however, univariate analysis found that LVEF was not a significant factor predicting AF. This supports previous observations (Parashar et al. Citation2013). Similarly, left atrium volume index was not found to be a predictor.
CRP level has been found to be an independent predictor of new onset AF in patients with AMI (p = 0.039) (Sanchez et al. Citation2003, Gedikli et al. Citation2008). Similarly, patients who developed AF during hospitalisation have also been found to have higher CRP levels than those without AF, with stepwise multivariable logistic regression analysis identifying CRP as a predictor of AF. A previous study found CRP levels on day 2–4 to be independently higher in patients with AF (OR 1.15, 95% CI 1.04–1.27) (Yoshizaki et al. Citation2012). Our findings do not indicate any significant correlation between CRP concentration and the occurrence of AF.
In addition, our findings do not suggest any relationship between new-onset AF in AMI patients and hypertension, diabetes and obesity, as also noted previously by Vukmirovic et al. (Citation2017) and Rhyou et al. (Citation2018). However a study of 216 patients with myocardial infarction found hypertension to be a predicting factor of AF (p = 0.002) (Iqbal et al. Citation2019), while another found AMI patients who developed AF to be more likely to demonstrate hypertension (p = 0.033) (Parashar et al. Citation2013). In addition, the development of new-onset AF was found to be predicted by hypertension in a GRACE registry of ACS (Mehta et al. Citation2003) and PURSUIT trial (Al-Khatib et al. Citation2001).
The GISSI-3 study (Pizetti et al. Citation2001) found both diabetes and hypertension to be predictors of new onset AF after acute MI. However, opinions regarding the predictive value of diabetes for new onset AF are divided, with some previous studies supporting these findings (Lehto et al. Citation2005, Vukmirovic et al. Citation2017) and others not (Parashar et al. Citation2013).
Although obesity has been found to be associated with the occurrence of new-onset AF in patients with myocardial infarction (OR 2.28) (Guenancia Ch et al. Citation2014) this has yet to be confirmed in large studies.
In our group of patients, age appeared to be a significant factor predicting AF (p = 0.0300). The cut-off value for age was 72 years. A meta-analysis of 11 studies including 9570 patients summarising the clinical risk factors for new onset AF in acute myocardial infarction indicated that age was associated with new-onset atrial fibrillation occurrence after AMI. The patients were divided into groups according to the occurrence of AF during hospitalisation (He et al. Citation2019). This finding confirmed a number of others where age was a predictor of AF: the GUSTO I trial (Crenshaw et al. Citation1997), the OPTIMAAL trial including patients with AMI and signs of left ventricular dysfunction (Lehto et al. Citation2005) and the GISSI − 3 trial (Pizetti et al. Citation2001), as well as the HORIZONS-AMI trial (Rene et al. Citation2014), which compared different antithrombotic regimens and stents during primary PCI in patients with STEMI. Age has also been found to be a strong predictor of AF in AMI patients (Vukmirovic et al. Citation2017, Rhyou et al. Citation2018) (p = <0.001 in both studies).
In the present study, no significant correlation was found between AF and higher Killip class, with univariate analysis indicating that Killip class > 1 was not a significant predictor of AF. Similar observations were made in the TRIUMPH study (Parashar et al. Citation2010). In addition, a study of 600 patients with STEMI and NSTEMI found no difference in Killip class between patients diagnosed with AF during hospitalisation and those with sinus rhythm (Vukmirovic et al. Citation2017). In contrast, the OPTIMAAL trial (Lehto et al. Citation2005) and GISSI-3 study (Pizetti et al. Citation2001) found higher Killip class to be significantly associated with the development of AF. In addition, new-onset AF has been associated with a greater chance of cardiogenic shock (16.0% vs 8.3%; p = 0.038) (Rhyou et al. Citation2018), and Killip class IV was found to be the most significant predictor of the development of AF (OR 1.58 95% CI 1.45–1.73) (Rathore et al. Citation2000).
Limitations of the study
The study uses a relatively small group of patients, and this should be taken into consideration when interpreting the results.
Conclusion
New onset atrial fibrillation was diagnosed in 9.4% of the patients presenting with acute myocardial infarction. Patients with new-onset AF demonstrated higher MR-proANP concentrations than those without. Our findings indicate that MR-proANP level might be a good predictor of AF. MR-proANP measurements should be included in the standard panel of laboratory tests for patients with AMI.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Al-Khatib, S.M., et al., 2001. Atrial fibrillation and mortality among patients with acute coronary syndromes without ST-segment elevation: results from the PURSUIT trial. The american journal of cardiology, 88 (1), 76–79.
- Anumonwo, J.M., and Kalifa, J., 2014. Risk factors and genetics of atrial fibrillation. Cardiology clinics, 32 (4), 485–494.
- Crenshaw, B.S., et al., 1997. Atrail fibrillation in the setting of acute myocardial infarction: the GUSTO – I experience. Global Utilization of Streptokinase and TPA for occluded coronary arteries. Journal of the american college of cardiology, 30 (2), 406–413.
- Dorje, T., et al., 2013. Plasma N-terminal pro-brain natriuretic peptide levels predict new-onset atrial fibrillation in patients with acute myocardial infarction. International journal of cardiology, 168 (3), 3135–3137.
- Gedikli, O., et al., 2008. Association between serum C-reactive protein elevation and atrial fibrillation after first anterior myocardial infarction. Clinical cardiology, 31 (10), 482–487.
- Guenancia CH, Stamboul, K., et al., 2014. Obesity and new-onset atrial fibrillation in acute myocardial infarction: a gender specific risk factor. International journal of cardiology, 176 (3), 1039–1041.
- He, J., et al., 2019. Clinical risk factors for new – onset atrial fibrillation in acute myocardial infarction. Medicine, 98 (26), e15960.
- Idzikowska, K., and Zielińska, M., 2018. Midregional pro-atrial natriuretic peptide, an important member of the natriuretic peptide family: potential role in diagnosis and prognosis of cardiovascular disease. The journal of international medical research, 46 (8), 3017–3029.
- Iqbal, Z., et al., 2019. New-onset atrial fibrillation in patients presenting with acute myocardial infarction. Cureus, 11 (4), e4483.
- Lehto, M., et al., 2005. Prognostic risk of atrial fibrillation in acute myocardial infarction complicated by left ventricular dysfunction: the OPTIMAL experience. European heart journal, 26 (4), 350–356.
- Mehta, R.H., et al., 2003. Comparison of outcomes of patients with acute coronary syndromes with and without atrial fibrillation. Am. J. Cardiol, 92 (9), 1031–1036.
- Morgenthaler, N.G., et al., 2004. Immunoluminometric assay for the midregion of pro-atrial natriuretic peptide in human plasma. Clinical chemistry, 50 (1), 234–236.
- Parashar, S., et al., 2013. New – onset atrial fibrillation after acute myocardial infarction and its relationship to admission biomarkers [from the TRIUMPH registry]. The American journal of cardiology, 112 (9), 1390–1395..
- Parashar, S.L.J., et al., 2010. Elevated BNP predicts new onset atrial fibrillation complicating acute myocardial infarction: analysis of the TRIUMPH registry. Journal of the American college of cardiology, 55 (10), A7.E61.
- Pizetti, F., et al., 2001. GISSI-3 Investigators. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI-3 data. Heart, 86, 527–532.
- Rathore, S.S., et al., 2000. Acute myocardial infarction complicated by atrial fibrillation in the elderly: prevalence and outcomes. Circulation, 101 (9), 969–974.
- Rene, A.G., et al., 2014. Impact of atrial fibrillation in patients with ST-elevation myocardial infarction treated with percutaneous coronary intervention (from the HORIZONS-AMI trial). The American journal of cardiology, 113 (2), 236–242.
- Rhyou, H.I., et al., 2018. Clinical factors associated with the development of atrial fibrillation in the year following STEMI treated by primary PCI. Journal of cardiology, 71 (2), 125–128.
- Sanchez, P.L., et al., 2003. Do baseline C-reactive protein levels predict the new-onset of atrial fibrillation in patients with acute coronary syndrome? European heart journal, 24 (5), 509.
- Vukmirovic, M., et al., 2017. Predictions and outcomes of atrial fibrillation in the patients with acute myocardial infarction. Open medicine, 12, 115–124.
- Yoshizaki, T., et al., 2012. Activated inflammation is related to the incidence of atrial fibrillation in patients with acute myocardial infarction. Internal medicine, 51 (12), 1467–1471.
- Zeng, R.X., et al., 2017. Left ventricular ejection fraction and left atrium diameter related to new-onset atrial fibrillation following acute myocardial infarction: systematic review and meta-analysis. Oncotarget, 8 (46), 81137–81144.
- Zoni-Berisso, M., et al., 2014. Epidemiology of atrial fibrillation: European perspective. Clinical epidemiology, 6, 213–220.