Abstract
Purpose
Studies revealed that silencing of low-density lipoprotein receptor-related protein-1 (LRP1) expression can cause inhibition of adipogenesis in animal model and contribute to reduced body size. But there is no study that has explored the association of LRP1 with body mass index (BMI) of human adults. Therefore, the aim of this study was to investigate the relationship of LRP1 with undernutrition.
Methods
A total of 270 Bangladeshi slum-dwelling adults were enrolled as case control design. Their socio-economic, demographic, anthropometric and biomedical data were collected. Plasma LRP1, C-reactive protein (CRP), alpha-1 acid glycoprotein (AGP) and ferritin levels were measured by ELISA, haemoglobin by HemoCue and zinc by atomic absorption spectrometry.
Results
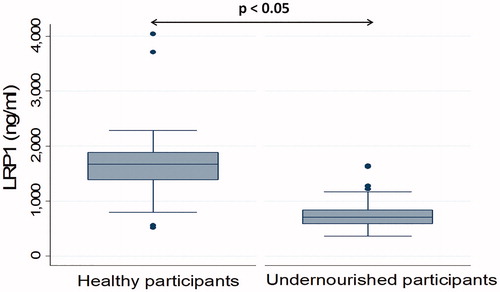
The median (IQR) values of plasma LRP1 were 1673.1 (1382.5–1886.2) ng/mL in healthy participants and 707.7 (588.6–839.9) ng/mL in undernourished participants, respectively. A strong positive correlation (r = 0.70, p < 0.05) between LRP1 and BMI was found. Multivariable logistic regression analysis revealed a positive association between low plasma LRP1 (Adj. OR = 0.98, CI = 0.98, 0.99 and p < 0.05) and undernutrition.
Conclusions
The study found that increased level of LRP1 is associated with increased BMI, whereas lower level is associated with low BMI.
Introduction
Malnutrition is a public health concern all over the world, particularly in developing countries (Müller et al. Citation2005). It is an imbalanced nutritional condition that includes both under- and over-nutrition. The adults having body mass index (BMI) <18.5 kg/m2 are referred to be undernourished, while over-nutrition includes overweight and obesity (Bharati et al. Citation2019, WHO Citation2021). It has been estimated that undernutrition is on the rise and reached 821 million people in 2017 around the world, whereas in Southern Asia the prevalence of undernutrition is 14.8% (Organization Citation2018). In Bangladesh, the scenario is even worse; nearly 30% of the adult population including both female and male were undernourished in 2011 (Biswas et al. Citation2017). This figure got reduced to 16% for adult women in 2015 (Organization Citation2016). Undernutrition affects adulthood by reducing performance capacity and low productivity of work as well as leading to complicated pregnancy outcome and poor health conditions (Nube et al. Citation2003, Benson et al. Citation2006, Biswas et al. Citation2017). Several factors such as inadequate dietary intake, swallowing issues, eating/chewing problem, dysphagia, depressive symptoms and older age are associated with weight loss and low BMI and can cause undernutrition among adults (Tamura et al. Citation2013). Overall, environmental, genetic and epigenetic changes may cause undernutrition in children (Ahmed et al. Citation2009, Schmidt Citation2014, Uchiyama et al. Citation2018), but there is a paucity of evidence to support a causal relation of these factors with undernutrition in adults.
Low-density lipoprotein receptor-related protein-1 (LRP1) is an endocytic receptor that plays important role in binding and internalization of a wide range of biological ligands (Lillis et al. Citation2008). It functions in various cellular activities including proliferation, migration and differentiation of cell as well as activation of lysosomal enzymes (Lillis et al. Citation2008, Safina et al. Citation2016). It has a potential role in phagocytosis, which is necessary for removal of infectious agents (Lillis et al. Citation2008), thus improves health condition through elimination of infection. Moreover, it also plays a pivotal role in adipogenesis and lipid metabolism in mature adipocytes. A previous study indicates that expression of LRP1 is upregulated in adipose tissue of obese human and mouse (Masson et al. Citation2009). The study also showed that silencing of LRP1 expression in mouse inhibits adipogenesis through inhibition of nuclear peroxisome proliferator-activated receptor γ, which is vital for the initiation of adipogenesis (Masson et al. Citation2009). Another study also demonstrated that reduced expression of LRP1 could contribute to stunted phenotype in children (Uchiyama et al. Citation2018). The study also reported that reduced body size, loss of intestinal barrier function as well as gut inflammation have been observed in LRP1 knockout mice (Uchiyama et al. Citation2018). In addition, it has been elicited that LRP1 (in adipocyte) knockout mice have small amount of fat and lipid depleted adipocytes which caused reduced body weight (Chappell et al. Citation1993, Citation1994, Nykjaer et al. Citation1993). Therefore, a reduction in the level of adipocytic LRP1 might have an effect on body weight and BMI. Genetic analysis revealed contradictory results about the relationship between BMI and LRP1 gene. LRP1 genotype has a strong influence on BMI and waist circumference (Vučinić et al. Citation2017), while another study found no association between certain single nucleotide polymorphism (SNP) of LRP1 gene and BMI (Frazier-Wood et al. Citation2012). But there is no study that has explored the association of LRP1 with BMI of human adults. However, it is not feasible to examine the association of adipocytic LRP1 with BMI due to invasive collection procedure (abdominal lipectomy) of adipose tissue. But plasma LRP1 can fill that void as it is a biomarker of adipocytic LRP1 and plasma LRP1 also represents the volume of adipose tissue (de Gonzalo-Calvo et al. Citation2016, Citation2018). In this study, we aimed to investigate the relationship of plasma LRP1 with undernutrition in Bangladeshi adults who lives in slums.
Clinical significance
Undernutrition is an alarming issue all over the world and affects adulthood by reducing performance capacity and low productivity of work.
There is a paucity of biological causes for undernutrition. Adipocytic LRP1 is one of the causal biological molecules for undernutrition and can be a biomarker to indicate this phenomenon.
Due to invasive collection procedure (abdominal lipectomy) of adipose tissue, it is ethically not feasible to investigate the level of adipocytic LRP1 in case of undernourished individual. But plasma LRP1 can fill that void as it is a biomarker of adipocytic LRP1 and also represent the volume of adipose tissue.
Plasma LRP1 can measure the level of adipocytic LRP1 which can be a therapeutic target to treat the undernutrition.
Materials and methods
Study design, participants and study site
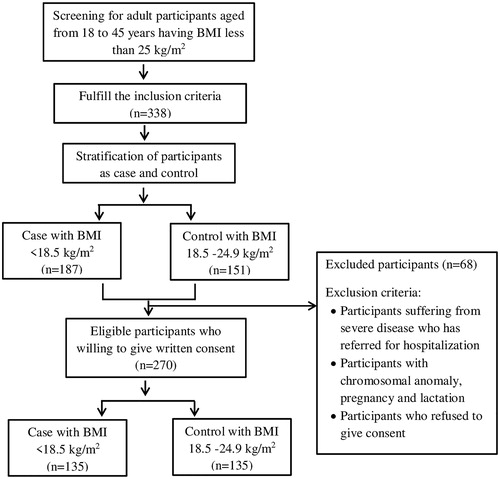
A group of 270 Bangladeshi adults were recruited in a case-control manner from our ongoing ‘Bangladesh Environmental Enteric Dysfunction (BEED)’ study. The detailed study protocol has been published elsewhere (Mahfuz et al. Citation2017). The case group was comprised of 135 undernourished participants (BMI <18.5 kg/m2). A total of 135 healthy participants (BMI from 18.5 kg/m2 to 24.9 kg/m2) without any history of chronic diseases were enrolled as controls. shows the criteria for screening, exclusion and enrolment of the study participants. Study participants were recruited from Bauniabadh area of Mirpur, Dhaka, Bangladesh.
Ethical consideration
The study protocol was approved by the institutional review board of the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b). All participants were informed about the study and written consents were obtained from them.
Data collection, sample collection and laboratory analyses
Anthropometric, socio-economic and demographic data were collected from each of the study participants by trained field staff. Two millilitres of venous blood was collected in a blood collection tube (S-Monovette 7.5 mL, Sarstedt, Numbrecht, Germany) by phlebotomist after maintaining all the aseptic conditions and transported to laboratory under cold-chain maintenance. Plasma was collected by centrifugation at 4000 rpm for 10 minutes and preserved at −80 °C prior to biomarker analysis. Plasma biomarkers including LRP1, C-reactive protein (CRP), alpha-1 acid glycoprotein (AGP) and ferritin were measured using commercially available ELISA kits. Zinc was measured in plasma by atomic absorption spectrometry technique and HemoCue Hb 201 System was used to measure haemoglobin. All the laboratory work were done at the parasitology laboratory of icddr,b.
Statistical analyses
Exploratory data analyses were performed to describe the characteristics of the enrolled participants using Mann–Whitney’s U test and Chi-square test. The variables following skewed distributions were presented as median with inter-quartile ranges, whereas categorical variables were presented as frequencies with percentages. Mann–Whitney’s U test was used to detect the differences in the age, BMI as well as plasma biomarker including LRP1, CRP, AGP, haemoglobin, zinc and ferritin, while Chi-square test were used for comparing categorical variables (sex, smoking status and substance abuse) of the undernourished and healthy participants. Spearman's correlation coefficients (r) were calculated to assess the correlation of the level of plasma LRP1 with BMI, levels of haemoglobin, zinc, ferritin and inflammatory markers (CRP and AGP). A multivariable logistic regression analysis was performed to measure the association between plasma LRP1 level and undernutrition, where presence (BMI <18.5 kg/m2) or absence (BMI from 18.5 kg/m2 to 24.9 kg/m2) of undernutrition was the outcome variable and level of plasma LRP1 was the explanatory variable. In this study age, sex, smoking status and haemoglobin were considered as cofounding variables on the basis of literature review (Frazier-Wood et al. Citation2012) and variables including CRP, AGP, zinc, ferritin with p value <0.05 in bivariate analysis were also included as confounding variables. In all the analyses, p value less than <0.05 was considered statistically significant. All the analyses were done using STATA version 13 (StataCorp, College Station, TX).
Results
Descriptive information of the study participants
presents the descriptive statistics of the participants. Among the participants nearly one-third was male. The median (IQR) ages of the healthy and undernourished participants were 24 (19–30) years and 21 (19–26) years, respectively. The median (IQR) BMI of the healthy and undernourished participants was 21.8 (20.2–23.5) kg/m2 and 17.4 (16.8–18) kg/m2, respectively. Approximately, 14% healthy and 5% undernourished participants were smokers and all smokers were male. Moreover, smoking status significantly (p < 0.05) differs between these two study groups. Almost similar numbers of healthy and undernourished participants were addicted with different types of substances such as betel leaf, areca nut, slaked lime.
Table 1. Descriptive characteristics of the study participants.
Plasma biomarker levels in the study participants
The levels of CRP, AGP, haemoglobin, zinc and ferritin were significantly (p < 0.05) higher in healthy participants compared to undernourished participants (). The median (IQR) value of CRP, AGP, haemoglobin, zinc and ferritin was 2.1 (0.9–4.4) mg/L, 75.8 (62.9–95.9) mg/dL, 13.2 (12–14.3) g/dL, 0.74 (0.7–0.8) mg/L, 59.9 (26.4–123.2) ng/mL in healthy participants and 0.8 (0.2–1.7) mg/L, 64.7 (52.9–86.9) mg/dL, 12.4 (11.4–13.4) g/dL, 0.71 (0.6–0.8) mg/mL, 43.7 (19.9–80.2) ng/mL in undernourished participants, respectively.
Correlation among biochemical parameters and anthropometric measurements
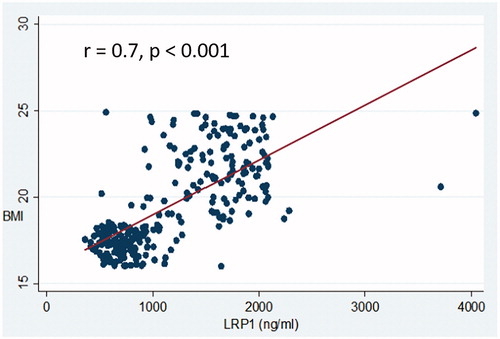
There was a strong positive (r = 0.7) correlation between LRP1 and BMI and this finding was statistically significant (p < 0.05) (). Similarly, positive correlation was found for CRP, AGP, Hb, ferritin and zinc with LRP1 and BMI. Correlations among different variables are presented in .
Table 2. Spearman’s correlation of LRP1 with BMI and different biomarkers both in healthy and undernourished participants.
The association between plasma LRP1 and undernutrition
Comparison of plasma LRP1 level between undernourished and healthy participants revealed that plasma LRP1 level was significantly (p < 0.05) lower in undernourished participants compare to healthy participants (). The median (IQR) values of plasma LRP1 in undernourished and healthy participants were 707.7 (588.6–839.9) ng/mL and 1673.1 (1382.5–1886.2) ng/mL, respectively ().
Multivariable logistic regression analysis showed that lower level of plasma LRP1 (Adj.OR = 0.98, CI = 0.98, 0.99 and p value <0.05) was positively associated with undernutrition. In bivariate analysis, age, sex, LRP1, CRP, AGP, haemoglobin, zinc, ferritin and smoking status were found to be associated with adult undernutrition. But, only LRP1, CRP and smoking status were found to be associated with undernutrition upon adjustment for age, sex, substance abuse, AGP, haemoglobin, ferritin and zinc in multivariable analysis, where, lower level of LRP1 and CRP was positively associated with undernutrition. The findings were significant in case of both bivariate and multivariate analyses. The results of logistic regression analysis are presented in .
Table 3. Multivariable logistic regression analysis to explore the association between plasma LRP1 and undernutrition.
Discussion
In the present study, significant positive association was found between lower level of plasma LRP1 and undernutrition in Bangladeshi adults. Overall, our study results revealed that plasma LRP1 level was significantly lower in undernourished participants compared to their corresponding healthy controls. Such lower level of plasma LRP1 might be a consequence of reduced expression of LRP1 in adipocytes (de Gonzalo-Calvo et al. Citation2018). This finding is supported by the study conducted by Uchiyama et al. (Citation2018), where they reported that reduced expression of LRP1 can contribute to stunted phenotype in children. In addition, this reduced expression of LRP1 may also reflect that there are fewer adipocytes in undernourished individuals because study (Masson et al. Citation2009) indicates that LRP1 is crucial for differentiation of adipocytes. Both the stunted children and undernourished adults are alluded to suffer from undernutrition. From the nutritional point of view, it can be inferred that reduced expression of LRP1 may be associated with both stunted and undernourished condition. In addition, Spearman’s correlation between plasma LRP1 and BMI also demonstrated a strong positive correlation between these two variables. This finding suggests that increased level of LRP1 is associated with increased BMI while a decreased level is associated with low BMI. On the other hand, genetic analysis published conflicting findings such as BMI and waist circumference were strongly influenced by LRP1 genotype, while another study found no association between BMI and some SNP of LRP1 gene in human (Frazier-Wood et al. Citation2012, Vučinić et al. Citation2017). Moreover, multivariable logistic regression analysis suggests that lower level of LRP1 is associated with undernutrition in Bangladeshi adults. A study conducted in undernourished participants found an association between CRP and undernutrition (Coutinho et al. Citation2006), which is also in accordance with our finding. Another study found that plasma CRP level was lower in undernourished participants (Loprinzi et al. Citation2015), which is consistent with our finding. The lower level of CRP might be due to limited synthetic capacity of liver in undernourished adult. Moreover, CRP level was positively correlated with BMI in our analysis which is also supported by another study (Kao et al. Citation2009). Our study results also showed that smoking status is higher in healthy participants compared to undernourished participants as well as effect size of the association between smoking and undernutrition is very large. This may be due to more expendable capacity of healthy participants for smoking than undernourished participants because of higher family income of healthy participants compared to undernourished participants.
Various aspects such as environmental and genetic factors as well as epigenetic changes may cause undernutrition in adults and children (Benson et al. Citation2006, Ahmed et al. Citation2009, Tamura et al. Citation2013, Uchiyama et al. Citation2018). LRP1 is an endocytic receptor, crucial for the initiation of adipogenesis through activation of nuclear peroxisome proliferator-activated receptor γ, responsible for weight gain. On the other hand, silencing of LRP1 expression can cause inhibition of adipogenesis in mouse model, causing reduced body weight (Masson et al. Citation2009). Studies showed that, dietary lipids in chylomicron remnants enter into hepatocytes by the action of LRP1 through binding to Apolipoprotein E (ApoE), lipoprotein lipase (LpL) and hepatic lipase (Beisiegel et al. Citation1989, Citation1991, Kowal et al. Citation1989, Kounnas et al. Citation1995). It has been reported that ApoE is crucial for triglycerides accumulation in adipocytes and found to have a pivotal role in adipocytes differentiation and obesity (Yue et al. Citation2004, Huang et al. Citation2006, Gao et al. Citation2007). There is strong evidence that LRP1 plays important role in some signal transduction pathways that are crucial for cell proliferation and cell migration. In addition, LRP1 also mediates trafficking and storage of lipid in adipocytes (Terrand et al. Citation2009). Another study also revealed that impairment of triglyceride rich lipoprotein (TGRL) assimilation in adipose tissue is accompanied by the absence of LRP1, resulting in reduced fat mass (Hofmann et al. Citation2007). Hence, there might have little lipid/TG available to store in adipocytes in case of undernutrition due to lower LRP1. Altogether, these findings strongly suggest that lower level of LRP1 may have an effect on adipocytes differentiation and also associated with undernutrition.
In our study, we only measured the plasma LRP1 level but we did not measure the expression level of adipocytic LRP1 in undernourished participants due to invasive collection procedure of adipose tissue. In addition, we did not investigate the effect of inhibition of LRP1 expression in case of human to explore whether reduced expression may or may not contribute to undernutrition due to ethical consideration. Moreover, this study has been conducted as a cross-sectional nature that’s why ‘cause and effect’ cannot be drawn from this study. In addition, there is a lack of balanced case and control group regarding age and sex. These are the limitations of this study. However, this was the first study that explored the relationship between plasma LRP1 level and undernutrition in human adults, which is the strength of this study. This study also reported about the correlation between plasma LRP1 and BMI of adults at the first time.
Conclusions
Our results suggest that increased level of LRP1 is associated with increased BMI, whereas lower level is associated with low BMI in adults. This result suggests the importance of investigating the association between plasma LRP1 and undernutrition in children.
Author contributions
TA conceptualized the study. MMH and SMF wrote the manuscript and analysed the data. SMF also designed the study and supervised the data collection. MMH and MAG did the laboratory analysis. SD critically reviewed the manuscript and developed the final version. MM, SMF involved in the development of study protocol. All authors commented on manuscript and approved the final version.
Acknowledgements
The authors would like to thank all the participants and their parents for sharing their time and providing consent and information necessary for the successful completion of the study. The authors also acknowledge the contribution of icddr,b's core donors including Governments of the People’s Republic of Bangladesh, Canada, Sweden and UK for their continuous support and commitment to the icddr,b's research efforts.
Disclosure statement
The authors declared no conflict of interests.
Data availability statement
The data set that was created during the study is not publicly available due to the restriction of funder. However, suggestion for data analysis can be made to corresponding author.
Additional information
Funding
References
- Ahmed, T., et al., 2009. Use of metagenomics to understand the genetic basis of malnutrition. Nutrition reviews, 67 (Suppl. 2), S201–S206.
- Benson, T., et al., 2006. Trends and issues in child undernutrition. Disease and mortality in Sub Saharan Africa. 2nd edition. Washington (DC): The International Bank for Reconstruction and Development/The World Bank.
- Beisiegel, U., et al., 1989. The LDL-receptor-related protein, LRP, is an apolipoprotein E-binding protein. Nature, 341 (6238), 162–164.
- Beisiegel, U., et al., 1991. Lipoprotein lipase enhances the binding of chylomicrons to low density lipoprotein receptor-related protein. Proceedings of the national academy of sciences of the United States of America, 88 (19), 8342–8346.
- Bharati, S., et al., 2019. Malnutrition and anaemia among adult women in India. Journal of biosocial science, 51 (5), 658–668.
- Biswas, T., et al., 2017. The prevalence of underweight, overweight and obesity in Bangladeshi adults: data from a national survey. PLoS One, 12 (5), e0177395.
- Chappell, D.A., et al., 1993. Lipoprotein lipase induces catabolism of normal triglyceride-rich lipoproteins via the low density lipoprotein receptor-related protein/alpha 2-macroglobulin receptor in vitro. A process facilitated by cell-surface proteoglycans. Journal of biological chemistry, 268 (19), 14168–14175.
- Chappell, D.A., et al., 1994. Cellular catabolism of normal very low density lipoproteins via the low density lipoprotein receptor-related protein/alpha 2-macroglobulin receptor is induced by the C-terminal domain of lipoprotein lipase. Journal of biological chemistry, 269 (27), 18001–18006.
- Coutinho, H.M., et al., 2006. Pro-inflammatory cytokines and C-reactive protein are associated with undernutrition in the context of Schistosoma japonicum infection. The American journal of tropical medicine and hygiene, 75 (4), 720–726.
- de Gonzalo-Calvo, D., et al., 2016. Circulating levels of soluble low-density lipoprotein receptor-related protein 1 (sLRP1) as novel biomarker of epicardial adipose tissue. International journal of cardiology, 223, 371–373.
- de Gonzalo-Calvo, D., et al., 2018. Soluble LRP1 is an independent biomarker of epicardial fat volume in patients with type 1 diabetes mellitus. Scientific reports, 8 (1), 1054.
- Frazier-Wood, A.C., et al., 2012. Preliminary evidence for an association between LRP-1 genotype and body mass index in humans. PLOS One, 7 (2), e30732.
- Gao, J., et al., 2007. Involvement of apolipoprotein E in excess fat accumulation and insulin resistance. Diabetes, 56 (1), 24–33.
- Huang, Z.H., et al., 2006. Endogenous ApoE expression modulates adipocyte triglyceride content and turnover. Diabetes, 55 (12), 3394–3402.
- Hofmann, S.M., et al., 2007. Adipocyte LDL receptor-related protein-1 expression modulates postprandial lipid transport and glucose homeostasis in mice. The journal of clinical investigation, 117 (11), 3271–3282.
- Kao, T.-W., et al., 2009. Associations between body mass index and serum levels of C-reactive protein. South African medical journal, 99 (5), 326–330.
- Kounnas, M.Z., et al., 1995. The cellular internalization and degradation of hepatic lipase is mediated by low density lipoprotein receptor-related protein and requires cell surface proteoglycans. The journal of biological chemistry, 270 (16), 9307–9312.
- Kowal, R.C., et al., 1989. Low density lipoprotein receptor-related protein mediates uptake of cholesteryl esters derived from apoprotein E-enriched lipoproteins. Proceedings of the national academy of sciences of the United States of America, 86 (15), 5810–5814.
- Lillis, A.P., et al., 2008. LDL receptor-related protein 1: unique tissue-specific functions revealed by selective gene knockout studies. Physiological reviews, 88 (3), 887–918.
- Loprinzi, P.D., et al., 2015. Association of body mass index with cardiovascular disease biomarkers. American journal of preventive medicine, 48 (3), 338–344.
- Mahfuz, M., et al., 2017. Bangladesh Environmental Enteric Dysfunction (BEED) study: protocol for a community-based intervention study to validate non-invasive biomarkers of environmental enteric dysfunction. BMJ open, 7 (8), e017768.
- Masson, O., et al., 2009. LRP1 receptor controls adipogenesis and is up-regulated in human and mouse obese adipose tissue. PLoS One, 4 (10), e7422.
- Müller, O., et al., 2005. Malnutrition and health in developing countries. Canadian medical association journal = journal de l'Association medicale canadienne, 173 (3), 279–286.
- Nube, M., et al., 2003. Gender and adult undernutrition in developing countries. Annals of human biology, 30 (5), 520–537.
- Nykjaer, A., et al., 1993. The alpha 2-macroglobulin receptor/low density lipoprotein receptor-related protein binds lipoprotein lipase and beta-migrating very low density lipoprotein associated with the lipase. The journal of biological chemistry, 268 (20), 15048–15055.
- Organization, 2018. Food and agriculture organization of the United Nations. Food security and nutrition around the world. Rome: The Organization.
- Organization, 2016. State of food security and nutrition in Bangladesh 2015. James P. Grant School of Public Health (JPGSPH), BRAC University, Helen Keller International, and the Bangladesh Bureau of Statistics. Dhaka [Accessed 29 August 2016].
- Safina, D., et al., 2016. Low-density lipoprotein receptor-related protein 1 is a novel modulator of radial glia stem cell proliferation, survival, and differentiation. Glia, 64 (8), 1363–1380.
- Schmidt, C.W., 2014. Beyond malnutrition: the role of sanitation in stunted growth. Environmental health perspectives, 122 (11), A298–A303.
- Tamura, B.K., et al., 2013. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: a systematic review of the literature. Journal of the American medical directors association, 14 (9), 649–655.
- Terrand, J., et al., 2009. LRP1 controls intracellular cholesterol storage and fatty acid synthesis through modulation of Wnt signaling. The journal of biological chemistry, 284 (1), 381–388.
- Uchiyama, R., et al., 2018. Histone H3 lysine 4 methylation signature associated with human undernutrition. Proceedings of the national academy of sciences of the United States of America, 115 (48), E11264–E11273.
- Vučinić, N., et al., 2017. The LRP1 gene polymorphism is associated with increased risk of metabolic syndrome prevalence in the Serbian population. Balkan journal of medical genetics, 20 (1), 51–58.
- WHO, 2021. Available from: www.who.int/features/qa/malnutrition/en/.
- Yue, L., et al., 2004. Divergent effects of peroxisome proliferator-activated receptor gamma agonists and tumor necrosis factor alpha on adipocyte ApoE expression. The journal of biological chemistry, 279 (46), 47626–47632.