ABSTRACT
Improving patient safety and the culture of care are health service priorities that coexist with financial pressures on organisations. Research suggests team training and better team processes can improve team culture, safety, performance, and clinical outcomes, yet opportunities for interprofessional learning remain scarce. Perioperative practitioners work in a high pressure, high-risk environment without the benefits of stable team membership: this limits opportunities and momentum for team-initiated collaborative improvements. This article describes an interprofessional course focused on crises and human factors which comprised a 1-day event and a multifaceted sustainment programme for perioperative practitioners, grouped by surgical specialty. Participants reported increased understanding and confidence to enact processes and behaviours that support patient safety, including: team behaviours (communication, coordination, cooperation and back-up, leadership, situational awareness); recognising different perspectives and expectations within the team; briefing and debriefing; after action review; and using specialty-specific incident reports to generate specialty-specific interprofessional improvement plans. Participants valued working with specialty colleagues away from normal work pressures. In the high-pressure arena of front-line healthcare delivery, improving patient safety and theatre efficiency can often be erroneously considered conflicting agendas. Interprofessional collaboration amongst staff participating in this initiative enabled general and specialty-specific interprofessional learning that transcended this conflict.
Introduction
Health system improvement increasingly focuses on improving patient safety and the culture of care. Within the United Kingdom such improvements are National Health Service (NHS) priorities. Poor teamwork is considered a major factor in adverse events and patient safety failures (e.g. Manser, Citation2009). Research suggests team training and better team processes can improve team culture, safety, and clinical outcomes (e.g. Haynes et al., Citation2009; Neily et al., Citation2010; Schmutz & Manser, Citation2013), yet opportunities for team learning activities remain scarce.
Responding to the growing evidence-base and local contextual factors, doctors and nurses at Barts Health NHS Trust in London, UK, created an interprofessional training course in crises and human factors for perioperative teams. The course aims to improve perioperative teamwork and engender a safety culture through interprofessional learning (IPL) and interprofessional problem-solving. This report outlines the course and presents some early participant feedback. A follow-up study will be reported subsequently.
Background
This initiative comprises IPL and interprofessional practice development planning during a core training day (CTD), plus multiple sustainment activities within the workplace.
Perioperative staff do not work with the same colleagues every shift. Nevertheless, nursing, anaesthetic, and support staff tend to work within surgical specialties, alongside specialist surgeons. Therefore, surgical specialties were targeted one-by-one to quickly build a “critical mass” of participants within each specialty. This approach has the potential to build shared understanding (inter-subjectivity) among co-workers (Billett, Citation2014) more quickly than theatre department mixed specialty training. Perioperative staff (surgeons, anaesthetists, theatre and recovery nurses, radiographers, healthcare support workers, porters, and schedulers) working in the targeted specialty were asked to participate in the CTD, in groups of 10–15 participants, during a four-week period.
The CTD was led by two to three experienced human factors and team training facilitators, who ensured collaboration and open discussion. Five key learning objectives (LOs) were made explicit, to:
Appreciate the elements of effective teamwork.
Explore and share perceptions of exemplary team member behaviour.
Co-create strategies to ensure effective team briefings and debriefings occur.
Understand the after action review (AAR) process (Walker, Andrews, Grewcock, & Halligan, Citation2012).
Understand how incident reporting can be used to generate team learning and effect change.
A recently refined framework that identifies five elements for teamwork (communication, coordination, cooperation & back-up behaviour, leadership, and situational awareness; Hull, Arora, Kassab, Kneebone & Sevdalis, Citation2011) was used to develop the learning activities. This framework was presented, then experienced through practical team exercises that required the five elements for successful completion (LO1). Workshops addressing LOs 2, 3, and 5 used small group work and facilitated whole group discussion. In one workshop, for example, participants reviewed recent incident reports from their own surgical specialty. Interprofessional discussion generated new ideas and improvement plans (LO5).
AAR is a structured debrief technique used to generate team learning after a safety incident (Walker et al., Citation2012). The CTD included a simulated AAR and facilitated discussion of potential applications for the team (LO4).
The sustainment strategy included a monthly theatres newsletter, a display of safety data in theatres, support to facilitate the delivery of AARs after incidents and patient safety failures, a weekly governance meeting, and seminars delivered by leading safety culture experts.
Methods
The study adopted a quasi-experimental post intervention (with follow-up) design and aimed to identify if the IPL and problem-solving initiated by this interprofessional training course is followed by improved team behaviours and theatre efficiency.
Data collection
Participant feedback and self-assessed learning from the CTD (questionnaire completed at the end of the day; reported in this article) plus a follow-up study (routinely collected theatre management and safety data) were triangulated with questionnaires completed by perioperative staff (to be reported in a subsequent article). Likert scales gauged agreement with six statements (see below) and satisfaction with 15 facets of the CTD (1 very poor; 5 very good). Four text boxes were provided for responses to open questions.
Data analysis
Likert-scale responses were summarised with descriptive statistics and graphs. Free-text responses were examined through inductive content analysis (Elo & Kyngäs, Citation2008). Two authors (TS & HM) independently reviewed the data, generated and refined themes; then they compared and discussed the independent theme lists. After several rounds of coding and discussion, the authors agreed upon a single set of themes.
Ethical considerations
The study design was reviewed under the Queen Mary University London “fast-track” research ethics process for very low-risk research and also discussed with the Barts Health NHS Trust Research Governance Team.
Results
Between January and November 2014, 130 staff working across six surgical specialties (orthopaedics, maxilla-facial, renal, vascular, trauma, and neurosurgery) were offered CTD places; 122 (94%) attended: 46 surgeons, 30 anaesthetists, 46 nurses and other health professionals (theatre and recovery nurses, radiographers, operating department practitioners, and porters); 102 (84% of attendees) provided feedback. Within each group, participants spanned very junior to the most senior practitioners.
Feedback was very positive: mean scores ranged from 4.5 to 5.0.
Over 85% of participants agreed or strongly agreed with the following statements: “I would like our team to review our theatre incidents regularly” (100%); “I better understand what my team members would consider exemplary behaviour” (99%); “I feel better prepared to participate in team debriefs using the AAR tool” (95%); “I feel better prepared to participate in, or run, team briefing or debriefing” (93%); and “I feel better prepared to use the WHO surgical checklist” (87%).
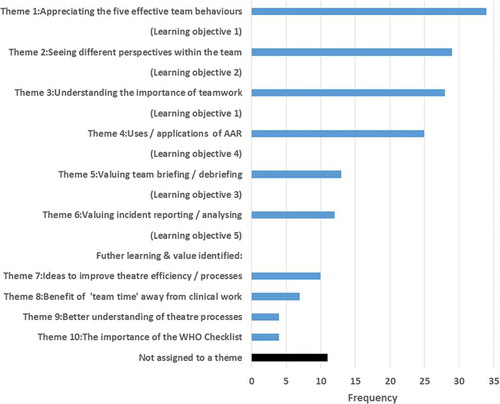
illustrates frequencies for themes emerging from 177 free-text statements responding to the request “Please describe two things you have learnt or found interesting today”. Themes T1–T6 relate to the content and LOs of the CTD. T1 included comments that referred to an element of the effective teamwork framework (Hull et al., Citation2011), while T3 contained comments about the importance of teamwork. T2 grouped comments recognising different perspectives within the team, e.g. “realise needs and problems of other groups” and “learning what the other sub-teams see as exemplary behaviour”. Comments relating to AAR formed T4, e.g. “how AAR can make people feel supported and may encourage more to raise issues”. T5 included comments that valued briefing/debriefing and T6 related to making or analysing incident reports.
Themes T7–T10 represented learning outcomes beyond the five explicit LOs: theatre process and efficiency-focused (T7); ideas for improvements and increased understanding (T9); appreciation of team time away from daily pressures (T8); and recognising the importance of the WHO Safer Surgery Checklist (T10).
Discussion
Post-CTD feedback from participants was very positive: each component was valued, agreement with the provided statements was high, and the analysis found that participants’ perceived learning from the training linked to each explicit LO and the wider objectives. Some areas for improvement were identified through the evaluation, and addressed. Reactions to the CTD also helped focus the ongoing sustainment programme.
Collegiate sharing of perceptions and improvement ideas and the development of tools to support daily work became possible when the participants were engaged in interprofessional discussion and problem-solving, away from the time pressures and professional hierarchies of daily work. The tools included specialty-specific briefing cards encompassing the safety-related information needs of the nursing, anaesthetic, and surgical teams, to help realise effective team briefings (LO3).
Ethnography focused on safety cultures in operating theatres (Gillespie, Gwinner, Chaboyer, & Fairweather, Citation2013) has emphasised the importance of building shared understandings through open communication, managing contextual stressors, speaking up in a strongly hierarchical culture, and the strains of fluid team membership. In response, the CTD setting allowed different professional discourses (Rowland & Kitto, Citation2014) about safety and efficiency to be heard and incorporated into a co-constructed interprofessional multi-vocal narrative (Clark, Citation2014). This is important because nurses and doctors experience interprofessional collaboration differently (Sollami, Caricati, & Sarli, Citation2015).
The CTDs generated planned improvements to interprofessional perioperative practices, which aimed to improve both safety and efficiency: several hinged on improved co-ordination of contributions to perioperative work, a challenge that has also been explored by Lillebo and Faxvaag (Citation2015). Deeper understanding of different perspectives within the team may lead to more effective team behaviours (Hull et al., Citation2011) and thus better, safer teamwork (Manser, Citation2009).
Part of the CTD focused on the surgical specialty’s last 50 incident reports. This generated high levels of engagement and positive feedback, which may subsequently support higher levels of incident reporting and safety improvements, as has been noted elsewhere following a brief training intervention focused on patient safety (Nagelkerk et al., Citation2014).
In relation to study limitations, inevitably for a post-intervention evaluation, the outcomes reported by participants are mainly knowledge gain, insights, and planned actions: we know that participants like the CTD but we do not yet know if it improves patient safety and perioperative team performance. Our ongoing follow-up study aims to detect longer-term changes in perceptions, behaviour, and theatre efficiency. These will not necessarily be easy to discern or isolate from other factors. The effects may be small due to the challenges of following through on planned changes upon return to busy, resource-constrained working environments (Christofilos, DeMatteo, & Penciner, Citation2015). The work of operating theatres is closely coupled with the work of other hospital departments which also contribute to patient safety and operating theatres’ efficiency. This will limit the discernible impact of IPL and practice development among perioperative practitioners. Furthermore, patient safety and service efficiency are such strong local and national agendas that multiple improvement initiatives coexist, making it difficult to isolate the impact of any one: that is simply the reality of research in modern healthcare environments.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Funding
Training delivery within this project was funded in part by the Herbert Frederick Day Award, a locally administered fund to improve perioperative care at the Royal London Hospital. No salaries were funded or payments made to the authors from this award.
Additional information
Funding
References
- Billett, S. R. (2014). Securing intersubjectivity through interprofessional workplace learning experiences. Journal of Interprofessional Care, 28, 206–211. doi:10.3109/13561820.2014.890580
- Christofilos, V., DeMatteo, D., & Penciner, R. (2015). Outcomes of commitment to change statements after an interprofessional faculty development program. Journal of Interprofessional Care, 29, 273–275. doi:10.3109/13561820.2014.950725
- Clark, P. G. (2014). Narrative in interprofessional education and practice: Implications for professional identity, provider–patient communication and teamwork. Journal of Interprofessional Care, 28, 34–39.
- Elo, S., & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. doi:10.1111/j.1365-2648.2007.04569.x
- Gillespie, B. M., Gwinner, K., Chaboyer, W., & Fairweather, N. (2013). Team communications in surgery: Creating a culture of safety. Journal of Interprofessional Care, 27(5), 387–393. doi:10.3109/13561820.2013.784243
- Haynes, A., Weiser, T., Berry, W., Lipsitz, S., Breizat, A., Dellinger, P., & Gawande, A., for the Safe Surgery Saves Lives Study Group. (2009). A surgical safety checklist to reduce morbidity and mortality in a global population. New England Journal of Medicine, 360, 491–499. doi:10.1056/NEJMsa0810119
- Hull, L., Arora, S., Kassab, E., Kneebone, R., & Sevdalis, N. (2011). Observational Teamwork Assessment for Surgery: Content validation and tool refinement. Journal of the American College of Surgeons, 212(2), 234–243. doi:10.1016/j.jamcollsurg.2010.11.001
- Lillebo, B., & Faxvaag, A. (2015). Continuous interprofessional coordination in perioperative work: An exploratory study. Journal of Interprofessional Care, 29, 125–130. doi:10.3109/13561820.2014.950724
- Manser, T. (2009). Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica, 53(2), 143–151. doi:10.1111/j.1399-6576.2008.01717.x
- Nagelkerk, J., Perterson, T., Pawl, B. L., Teman, S., Anyngu, A. C., Mlynarczyk, S., & Baer, L. J. (2014). Patient safety culture transformation in a children’s hospital: An interprofessional approach. Journal of Interprofessional Care, 28, 358–364. doi:10.3109/13561820.2014.885935
- Neily, J., Mills, P., Young-Xu, Y., Carney, B., West, P., Berger, D.,… Bagian, J. (2010). Association between implementation of a medical team training program and surgical mortality. Journal of the American Medical Association, 304(15), 1693–1700. doi:10.1001/jama.2010.1506
- Rowland, P., & Kitto, S. (2014). Patient safety and professional discourses: Implications for interprofessionalism. Journal of Interprofessional Care, 28, 331–338. doi:10.3109/13561820.2014.891574
- Schmutz, J., & Manser, T. (2013). Do team processes really have an effect on clinical performance? A systematic literature review. British Journal of Anaesthesia, 110(4), 529–544. doi:10.1093/bja/aes513
- Sollami, A., Caricati, L., & Sarli, L. (2015). Nurse-physician collaboration: A meta-analytical investigation of survey scores. Journal of Interprofessional Care, 29, 223–229. doi:10.3109/13561820.2014.955912
- Walker, J., Andrews, S., Grewcock, D., & Halligan, A. (2012). Life in the slow lane: Making hospitals safer, slowly but surely. Journal of the Royal Society of Medicine, 105(7), 283–287. doi:10.1258/jrsm.2012.120093