ABSTRACT
Safe medication use necessitates interprofessional working, with calls to enhance interprofessional education (IPE) focusing on medication safety (MS) in healthcare professional (HCP) curricula. Little is known about the design, delivery or evaluation of such activities. This systematic literature review describes MS-focused IPE activities in pre-qualification HCP programmes. MedLine, EMBASE, CINAHL and ERIC were searched, relevant studies identified and data extracted. The McGill Mixed Methods Appraisal Tool was employed. The 3P (presage-process-product) theory structured deductive analysis. Thirty-one studies were included, reporting on 30 activities, mostly undertaken in North America or United Kingdom. Presage/Design: Most reported activities involved pharmacy, nursing, medical or physician assistant students learning with one or more other HCP group. Few studies matched student groups’ skills or experiences. Few studies reported theoretical underpinnings. Process/Delivery: Multiple pedagogical approaches were employed, mostly social construction, and low- and high-fidelity simulation-based learning. Few studies reported learning outcomes or summative assessment, more reported formative assessment. Product/evaluation: Outcomes measured were learners’ opinions, satisfaction or attitudes toward interprofessional working and findings were generally positive. Few studies reported on student development or outcomes specific to medication safety. Lack of integration of qualitative/quantitative components of mixed methods studies and limited outcome measurements' validity or reliability weakened study quality. MS-focused IPE for pre-qualification HCPs is well received by students. Design of future activities could be enhanced by employing theory and ensuring matching of students’ and groups’ skills, professional identity and learner attributes to enhance learning in an interprofessional setting. Future delivery should embed MS-focused IPE into the standard curricula to optimize constructive alignment, learner engagement, quality and drive development. The required skillset in pre-qualification HCP programmes to facilitate future safe medication practice, together with the associated learning outcomes and assessment approaches, should be defined. The quality of scholarly studies examining these activities needs improvement.
Introduction
Internationally, evidence identifies that medication errors are highly prevalent, often preventable and can result in significant healthcare expenditure, morbidity and mortality (Avery et al., Citation2013; Dornan et al., Citation2009; E. E. Roughead et al., Citation2016; Elliott et al., Citation2021; L. Roughead et al., Citation2013; Ryan et al., Citation2014). In 2017, the World Health Organization (WHO) launched the Third Global Patient Safety Challenge: Medication Without Harm which aims to reduce severe avoidable medication harm by 50% by 2022 (Donaldson et al., Citation2017). The associated technical reports, focusing on polypharmacy and transitions of care, identify the importance of collaborative working to achieve this goal (WHO, Citation2019a, Citation2019b). Challenges to medication safety (MS) can occur at any stage of the medication use process. Optimal medication use requires interprofessional collaborative working between many professionals, patients and carers (Bardet et al., Citation2015; Rixon et al., Citation2015; Ross et al., Citation2013; Wilson et al., Citation2016). Safe medication use typically involves a process of parallel or sequential actions, performed by a variety of healthcare professionals (HCPs) and patients or carers, with dependence on each individual stage and/or the cascade between stages (Bardet et al., Citation2015; Dornan et al., Citation2009; Franklin, Citation2014; Rosenfeld et al., Citation2018; Wilson et al., Citation2016).
Safe medication use also requires the parallel application of technical and non-technical skills (Gordon et al., Citation2015; Wilson et al., Citation2016). Medication errors have been partly attributed to a lack of knowledge and skills, both technical and non-technical (Dornan et al., Citation2009; Keers et al., Citation2013; Ross et al., Citation2013; Slight et al., Citation2013), often associated with inadequate education and training (Dornan et al., Citation2009; S. R. Maxwell et al., Citation2015). Non-technical skills are a collection of social, cognitive and personal resource skills which draw upon higher cognitive processing, such as analyzing, relating, synthesizing or evaluating (Dearden et al., Citation2015; Gordon et al., Citation2015; Krathwohl, Citation2002). Examples of non-technical skills include situational awareness or monitoring (analytical), task management (analytical), communication and teamwork (relational). The relational non-technical skills concern interpersonal skills and therefore an individual’s performance is to some extent dependent on a collective context. Relational non-technical skills overlap somewhat with interprofessional collaborative skills as both center on communication and teamwork (Barr et al., Citation2016; Gordon et al., Citation2015).
Background
Interprofessional education (IPE) relates to the practice of HCPs or students learning with, from or about each other to improve collaboration and quality of care (Keers et al., Citation2013). This “learning with, from or about” provides for interaction between two or more health/social care professional groups, thereby dissolving professional silos and promoting collaborative relationships. IPE is a relatively new notion, developed around the turn of the century with successive Cochrane systematic reviews published in 2000, 2008 and 2013 demonstrating an increasing volume of studies exploring the benefit of IPE on patient outcomes or healthcare processes (Reeves et al., Citation2013, Citation2008; Zwarenstein et al., Citation1999). The most recent of these reviews identifies a heterogeneous body of studies which report positively on a range of outcomes, for example, professional practice or patient care, but with recognized deficits in the rigor and certainty of evidence (Reeves et al., Citation2013). In 2010, the WHO endorsed the merit of IPE in supporting healthcare providers’ professional development of the knowledge and skills required to collaborate effectively in the workplace (WHO, Citation2010). Since then, the implementation of IPE has increased globally, competency frameworks for interprofessional collaborative practice have been developed and IPE has become a requirement of regulatory bodies accrediting healthcare professional training programmes (Barr et al., Citation2016; Interprofessional Education Collaborative, Citation2016).
Deficits have been identified in uni-professional pre-registration education of HCPs regarding prescribing, medication management and MS (Brady et al., Citation2009; Heaton et al., Citation2008; Kostas et al., Citation2018; Luetsch & Rowett, Citation2016; Rickles et al., Citation2010; Schmitz et al., Citation2015). HCPs have been reported to work alongside, rather than with, one another, thereby limiting communication about medications (Rixon et al., Citation2015). Calls have been made to enhance IPE supporting MS (Cordina, Citation2019; Noble et al., Citation2017), introduced early in HCP training, to maximally influence the interprofessional culture, behavior and performance in future professional practice (Dornan et al., Citation2009; Löffler et al., Citation2017). The use of theoretically guided IPE has been advocated as a way to support staff to articulate and develop their teaching practice and to enable facilitators to communicate the rationale and features of interprofessional practice (Hean et al., Citation2012).
The World Health Professions Alliance (Citation2019) identify that the best ways to deliver IPE needs to be researched. Despite this, little is known about the IPE activities focused around MS in healthcare courses and although individual studies have reported on the development, delivery and evaluation of MS-focused IPE activities, we are not aware of any previous evidence synthesis on this topic (Cordina, Citation2019). A synthesis would add value by producing an overall understanding and appraisal of the MS-focused IPE activities undertaken to date and identifying opportunities to enhance future efforts. This might help educators, regulators and policymakers in their efforts to prepare students for future safer medication practices and support researchers undertaking scholarly work on this topic. Therefore this review sought to characterize the design, delivery and evaluation of IPE activities focusing on MS, during health professional education.
Methods
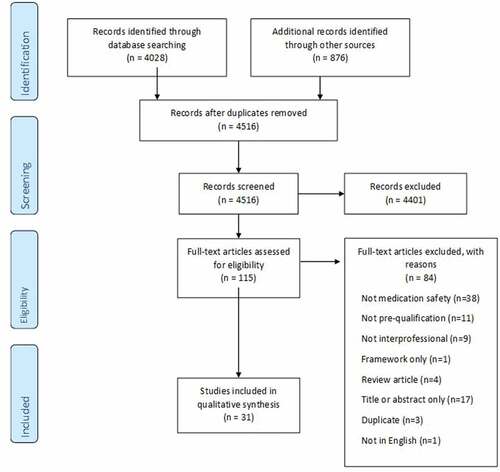
Guidance for reporting evidence synthesis in health education, the STORIES (STructured apprOach to the Reporting In healthcare education of Evidence Synthesis) statement (Gordon & Gibbs, Citation2014), and the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) (Moher et al., Citation2009), were observed.
Data sources and search strategies
Four electronic databases relating to healthcare and education were searched: MedLine, Embase, CINAHL and ERIC, applied to October 2020. Search terms addressed the following concepts and related terms: Interprofessional education (or learning or collaborative approach or multidisciplinary approach); medicine (or medication or drug) safety or error or potentially inappropriate prescribing or medication; undergraduate or bachelor student (Supplementary Material 1). Search terms and Boolean operators were adapted to each database. Forward and backward citation chasing were performed, and journal hand searches were undertaken for 2000 to 2020.
Study eligibility
Published studies reporting on IPE activities that were focused on MS among pre-qualification HCP students were included. MS was regarded as one or more of the key steps in the medication use process (prescribing, dispensing, administering, monitoring) or the topic of MS management itself (Pearson et al., Citation2015). IPE was defined as occasions where two or more professions learned with, from and about each other to improve collaborative practice and quality of care (Barr et al., Citation2016). Studies were excluded if they reported exclusively on learning in a postgraduate, post-registration or practice context. Published abstracts were excluded.
Study selection and data extraction
All identified articles were independently screened by title and abstract by both authors. Following this, the sub-set proceeded to full text review, completed independently by both authors. Differences were discussed and consensus reached regarding inclusion or exclusion.
Data were either independently extracted by both authors or led by one author and cross-referenced by the other. Data extractions were reviewed, differences were discussed, and consensus was reached. This was guided by a data extraction template, based on the 3P theory, which captured detail regarding the design (presage), delivery (process) and evaluation (product) of learning activities and study characteristics.
Quality assessment
A quality assessment of reviewed studies was completed by both authors using the standardized McGill Mixed-Methods Appraisal Tool (MMAT) (Hong et al., Citation2018). The MMAT enables evaluation of the methodological rigor of qualitative, quantitative and mixed-methods studies. Disagreements were resolved through discussion.
Data analyses and syntheses
Data extracted were described, tabulated and synthesized. Reported learning outcomes were categorized as addressing either interprofessional (IP) competencies, MS competencies or both. Learning outcomes relating to IPE were mapped by one author, with expertise in IPE, against the Interprofessional Education Collaborative’s (Interprofessional Education Collaborative, Citation2016) Core Competencies for Interprofessional Collaborative Practice, and the Canadian Interprofessional Health Collaborative (Citation2010). Learning outcomes relating to MS were mapped by one author, with expertise in medication safety, against the WHO’s suggested knowledge and performance learning outcomes in the MS chapter of the Patient Safety Curriculum Guide (World Health Organization, Citation2009). The focus of the learning activity was categorized against the key steps in the medication use process (prescribe, dispense, administer, monitor) and/or as MS management. Any theoretical model or framework or theoretical underpinnings that were used to plan the activities were identified.
The 3P theory provided the framework for deductive analysis (Biggs, Citation1993). The 3P model considers planning (presage), conducting (process) and evaluating (product) learning activities and therefore provides a useful framework for synthesizing review results with the aim to generating recommendations for the future design, delivery and evaluation of IPE about MS among pre-qualification HCP students.
Results
Study characteristics
Of the 4156 studies identified in the literature search, 31 studies, all published since 2010, were included, describing 30 MS-focused IPE activities (). Two studies reported on the same activity (studies 10, 11). Most studies were undertaken in north America (n = 16) or the United Kingdom (n = 10) (). Study designs were largely descriptive, restricted to posttest evaluation (n = 12) (1, 2, 7, 8, 10, 11, 12, 14, 18, 20, 24; 25; 28) or pre-post- test design (n = 13) (3; 4; 5; 6; 9; 13; 15; 16; 17; 19; 21; 22; 26; 27; 29; 31) with only two studies utilizing either a historic (23) or non-interprofessional comparator group (30). A variety of mixed methods (n = 18) (1; 2; 4; 8; 9; 11; 12; 13; 14; 16; 17; 18; 21; 24; 26; 29; 30; 31), quantitative (n = 9) (3; 5; 6; 15; 19; 20; 22; 23; 27) and qualitative (n = 4) (7; 10; 25; 28) approaches were used to evaluate the learning activities.
Table 1. Overview of study design.
Study quality was mediocre (Supplementary material 2). Qualitative data were poorly presented, particularly in mixed-methods studies which primarily focused on quantitative data. Challenges were identified with the integration of qualitative/quantitative components of mixed methods studies, representativeness of study samples in quantitative studies and validity or reliability of the outcome measurements employed.
Presage – planning learning activities
The primary drivers for MS-focused IPE were accreditation or health organization standards (n = 15) (1, 3, 4, 5, 7, 8, 9, 10, 11, 14, 15, 20, 22, 25, 31), improving education in medication safety (n = 15) (2, 6, 12, 13, 17, 18, 19, 21, 23, 24, 27, 28, 29, 30) or improving interprofessional collaboration in practice (26) (Supplementary material 3). Twenty studies focused on multiple steps in the medication use process (2, 3, 4, 7, 10, 11, 12, 13, 14, 15, 16, 19, 21, 23, 24, 26, 27, 29, 30, 31). The most common focus was prescribing or medication review (n = 24), (1, 2, 3, 4, 6, 7, 10, 11, 12, 13, 14, 15, 16, 19, 20, 21, 22, 24, 26, 27, 28, 29, 30, 31) and monitoring (n = 12) (2, 4, 8, 10, 11, 14, 15, 19, 21, 23, 26, 27).
For most studies (n = 19), faculty professional background matched those of the students involved in the activity (1, 3, 5, 6, 8, 10, 11, 13, 14, 15, 19, 20, 21, 22, 24, 28, 29, 30, 31). Faculty expertise was rarely described as specialist clinical expertise relevant to the activity (16, 24, 30), IPE and/or medication safety expertise (18, 26) and simulation-based learning specialization (31). Three studies provided facilitators with training (5, 8) or resources (29). Activity content was reportedly developed collaboratively between participating programmes (3, 13, 16, 19, 20, 21, 26, 29, 30, 31), primarily pharmacy-led (4, 5, 14, 22, 25) or involved clinical staff (10, 11, 26).
Activities typically involved a combination of pharmacy (n = 27) (2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 21, 22, 23, 24, 25, 26, 27, 28, 30), medicine (n = 24) (1, 2, 5, 6, 7, 8, 9, 10, 11, 13, 15, 16, 17, 18, 19, 20, 21, 23, 24, 26, 27, 28, 29, 30), nursing (n = 19) (1, 3, 8, 9, 13, 14, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 29, 31) or physician assistant students (n = 6) (4, 5, 17, 18, 23, 24) (Supplementary material 3). Discrete studies also included other HCP students (12, 31). Seventeen studies included a combination of two professions (1, 2, 3, 4, 7, 10, 11, 12, 14, 15, 20, 22, 25, 27, 28, 29, 30), eight studies included three professions (5, 6, 8, 9, 13, 19, 21, 31), four involved four professions (17, 23, 24, 26) and two involved up to seven professions (16, 18). Most activities exclusively involved pre-qualification students from a mixture of program years (n = 27), while the remaining three activities involved pre-registration students learning with post-registration clinicians (18, 21, 24). Assuming that HCP courses are typically 4–5 years’ duration, most studies involved students in the senior stage of their HCP course (5, 6, 7, 8, 9, 12, 13, 14, 15, 26, 27, 28, 29, 30), some reported a mixture (1, 4, 17, 19, 21, 23, 24, 31), a minority reported junior level (3, 11, 20, 25) and three did not report this (16, 18, 22). One study enrolled pre-qualification students and post-qualification students into separate learning activities (27). Few studies explicitly reported that students had prior IPE experience (3, 7, 12, 25), or prior medication-related skills or knowledge, (1, 2, 3, 11, 24, 27, 29, 30, 31). Some studies reported the basic knowledge between professional groups varied (1, 3, 11, 21, 26, 30). Fifteen activities assigned pre-activity preparation which was typically completed as self-directed learning (1, 3, 4, 8, 10, 14, 17, 18, 21, 23, 25, 29, 30, 31) while in one study, nursing students were pre-assigned experiential learning at a hospital (22).
Nine studies reported a theoretical or conceptual framework to support planning the learning activity, including theories of IPE (2, 30), simulation training (4, 7, 11, 14, 19, 21, 31), contact theory (11, 26) and the Jigsaw learning technique (6).
Process – conducting learning activities
Activities were mostly classroom- or lecture theater-based (1, 5, 6, 9, 11, 12, 13, 16, 21, 22, 27, 28, 29, 30), used simulated learning involving simulated patients, high fidelity mannequins or simulated practice environments (7, 8, 14, 17, 18, 19, 23, 31), a practice-based setting (2, 24, 25, 26), a virtual learning environment (3, 4), a conference style (10, 11) or a non-patient-facing hospital space (15). Eleven studies (ten activities) reported a mandatory participation embedded within the curriculum (2, 3, 8, 10, 11, 14, 18, 20, 28, 29, 30), eleven reported voluntary or extra-curricular participation (1, 4, 7, 9, 15, 16, 17, 21, 22, 26, 27) and seven reported a mixed approach, with the activity being mandatory for some learner groups and voluntary for others (5, 12, 13, 19, 23, 24, 25). In two reports it was unclear whether participation was mandatory or voluntary (6, 31). Contact time for most activities was reported as hours (1, 4, 5, 6, 12, 13, 14, 15, 16, 18, 19, 20, 21, 23, 24, 25, 27, 28, 29, 30), or day(s) (2, 8, 9, 10, 11, 22, 26) and four studies did not report this detail (3, 7, 17, 31).
Several pedagogical methods were employed: social construction of learning (1, 2, 4, 5, 6, 7, 8, 10, 12, 13, 14, 15, 17, 18, 19, 20, 21, 23, 24, 27, 28, 29, 30, 31); simulation-based learning, including case-based learning (4, 5, 6, 7, 9, 10, 11, 12, 13, 14, 15, 16, 18, 20, 21, 27, 28, 30), role playing (3, 8, 10, 14, 17, 18, 19, 20, 23, 26, 28, 31), high-fidelity virtual patient simulation (10, 11), and high-fidelity mannequins and suites (19, 23); experiential learning in a clinical environment (2, 24, 25, 28) or a medication therapy management call center (26). A minority of studies reported a didactic element (1, 5, 6, 9, 10, 15), typically complementing a simulation. Several studies employed group analysis and reflection (2, 7, 18). Most activities assigned a group collective task, most commonly case management (4, 6, 8, 10, 11, 12, 13, 19, 21, 24, 26, 27, 29, 31), group presentation (1, 2, 5, 15, 30), error disclosure (17, 18, 23) or significant event analysis (10, 11). Seven studies reported no group collective task (3, 9, 14, 16, 20, 22, 25), while one study did not report this detail (28).
Students were typically organized into small IP groups of 2–4 members (2, 4, 14, 18, 19, 21, 23, 24, 28, 29, 30, 31) or larger IP groups of 5–22 members (1, 5, 6, 8, 10, 11, 12, 13, 16, 17, 20, 22, 26). In one study students worked within their own professions and shared information asynchronously with another profession but did not work together in interprofessional groups (3). Some studies did not describe student groupings (7, 9, 15, 25, 27). Faculty and/or clinical staff facilitated most (n = 26) activities (1, 2, 3, 4, 5, 6, 7, 8, 10, 11, 12, 13, 14, 16, 18, 19, 20, 21, 23, 24, 26, 28, 29, 30, 31). One activity tasked pharmacy students to teach nursing students (70). Nineteen activities were delivered to more than 100 students (1, 2, 3, 5, 6, 8, 10, 11, 13, 14, 16, 17, 18, 20, 23, 28, 29, 30, 31), eight activities to between 22 and 80 students (4, 9, 12, 15, 22, 24, 26, 27), one pilot activity to eight students (21) and two studies did not report this (7, 19).
Reported learning outcomes were exclusively IPE-related (n = 8) (8, 16, 17, 18, 19, 20, 25, 26), a mixture of IPE- and MS-related (n = 6) (1, 2, 3, 11, 29, 31), exclusively MS-related (n = 3) (13, 28, 30), while 14 studies did not report any learning outcomes (4, 5, 6, 7, 8, 9, 10, 12, 14, 15, 21, 22, 23, 24, 27). One study reported separate learning outcomes for the medical (MS- and IPE-related) and pharmacy students (MS-related) (11). The IPE-related learning outcomes included: experiencing an interprofessional interaction (1), understanding of other professions’ roles and responsibilities (2, 3, 11, 16, 17, 18, 20, 25, 26, 29, 31), teams and teamwork (2, 3, 11, 16, 17, 20, 25, 26, 31), appraising, reflecting on and evaluating practice (13, 19), values and ethics, (3, 17, 25) and interprofessional communication (3, 11, 16, 17, 18, 19, 20, 25, 26, 29). The WHO Knowledge and Performance Learning Outcomes that mapped to the reported MS-related outcomes were: know that use of medicines is associated with risks (1), know common sources of error (29), know the responsibilities associated with prescribing and administering medication (3, 29), know the benefits of a multidisciplinary approach to medication safety (2, 3, 11, 29, 31), know how to make medication use safer (11), do tailor prescribing for each patient (1, 11, 13, 28), do practice taking thorough medication histories (13, 29), do know which medications are high risk (31), do be very familiar with the medications he/she prescribes or dispenses (2), do develop checking habits (2, 13), do report and learn from errors (11, 28) and do understand and practice drug calculations (13). The remaining learning outcomes listed by the WHO in their curriculum (Know: scale of medication error, how to recognize common hazardous situations; Do: use memory aids) were not evident in the activities described (WHO, Citation2009). The MS learning outcomes addressed technical skills for three studies (1, 11, 31) and a mixture of technical and non-technical skills for six studies (2, 3, 13, 28, 29, 30).
One study reported formal summative assessment of learning the MS component (prescribing) and of medical students and not pharmacy students (30). Most studies reported some kind of formative assessment for learning, most commonly using debriefing or other group feedback, model answers or rubrics for faculty-, self- or peer-assessment, or performance scores from faculty observation of team IP interactions (1, 2, 3, 4, 6, 7, 8, 10, 11, 12, 13, 14, 15, 17, 18, 20, 21, 23, 24, 25, 26, 29, 30, 31). Three studies reported formative assessment and self-evaluation of IPE-related learning outcomes (2, 16, 19), and one assessed interprofessional performance during a team activity using the Creighton Interprofessional Collaborative Evaluation (C-ICE ©) instrument, however the mark did not contribute to graded assessment (4). One study formatively assessed students’ pharmacotherapy knowledge scores (22). The subject of these assessments was generic interprofessional skills (4, 5, 16), technical medication safety skills (1, 10, 13, 22, 24, 25, 30), non-technical medication safety skills (18, 31) or some mixture of these (2, 3, 14, 17, 21, 23, 26).
Product – evaluating learning activities
Almost all studies variably used a combination of quantitative and/or qualitative methods to investigate student opinions of and satisfaction with the learning activity (n = 24) and attitudes toward IPE (n = 20) ().
Opinions and satisfaction were captured quantitatively using self-devised surveys (1, 2, 3, 4, 5, 6, 8, 12, 15, 17, 18, 23), and qualitatively using open-ended questions (2, 8, 10, 11, 16, 21, 26, 29, 30, 31), student reflections (4), focus groups (7, 13, 17), or semi-structured interviews (13, 14, 28). Quantitatively, students were generally satisfied, with all post-activity quantitative scores being high for student perception of the activity (1, 5, 17), likelihood to recommend the activity (2), mode of delivery (3, 4, 12, 18), increased practice confidence (3, 12) and usefulness for learning (6, 14, 15, 23, 24, 31). Two studies reported that medical (5) and pharmacy (8) students were less satisfied with the activity than their peers. Qualitatively, students reported improved knowledge and awareness of professional skills (2, 7, 14, 17, 21, 24) and increased practice confidence (4, 8, 17, 30). Students were complimentary about the learning experience (12, 13, 17, 21, 28, 31), the learning approaches (4, 8, 31), and the organizational and logistical oversight (10, 31). Single studies reported: frustration amongst pharmacy students’ understanding of what their roles were in the team environment (8), the problematic absence of some professions (13), and dominance in simulations by one professional group (17).
Attitudes toward IP collaboration were gathered quantitatively using self-devised (2, 8, 14, 26), and validated questionnaires (4, 5, 9, 11, 15, 16, 19, 21, 22, 27, 29, 30) and qualitatively, post-activity either through open-ended questions (1, 9, 10, 14, 30), student reflections (4), focus groups (7, 17) or semi-structured interviews (14, 28). One study developed and validated the Student Acceptance of Interprofessional Learning (SAIL-10) questionnaire (6). All but three activities (8, 11, 14), gathered quantitative data before and after the learning activity and with the exception of one (26), all of these reported improved attitudinal scores (4, 5, 6, 8, 9, 14, 15, 16, 19, 21, 22, 27, 29, 30). Hardisty et al., (13) collected a modified Readiness for Interprofessional Learning Scale (RIPLS) but did not report findings. One study administered a patient satisfaction survey and reported a positive patient experience (26). Qualitative data demonstrated that students valued learning collaboratively (2, 4, 10, 11, 16, 17, 28), improving understanding of professional roles and dispelling stereotypes (7, 14, 26, 28, 30), and realizing the importance of teamwork using realistic examples (9, 14). Students highlighted the issue of timing close to that of other assignments or tasks as a negative aspect of IPE (1, 10, 14) and sought earlier IPE introduction within the curriculum (30). There was significant variability in the between-profession differences reported amongst some studies, with no clear patterns or trends observed (5, 9, 16, 17, 19, 21, 29).
Few studies reported, qualitatively (1, 2, 7, 8, 11, 21, 28) or quantitatively (2, 8, 11, 15, 23, 29, 30), on outcomes specific to medication safety. Both qualitatively (1, 2, 7, 8, 11, 21) and quantitatively (8, 15, 29, 30) there were reports of student participants’ sense of value of the learning activity on perceived awareness, understanding, confidence and competence in MS tasks. Individual studies reported on: student perceived learning gains across a range of technical and non-technical skills (11), medical student participants’ application of learning gained into practice (28), a significant pre-post activity increase in participant self-rated ability to achieve the MS learning outcomes (2), improvement in proficiency scores describing a team’s medication error communication and disclosure performance (23), and improved pharmacotherapy knowledge-based scores (22, 31). Non-technical skills outcomes that were evident in the review were: feeling more competent to collaboratively manage polypharmacy (2), shared mental modeling (8), group error disclosure (17, 23), situation monitoring (19) and collaborative case management (31). Patients in receipt of an IP student delivered service agreed that it helped them with their medication knowledge and self-management (26). One study summatively assessed end of year medical student prescribing knowledge and reported no significant difference between students who received uni- or IP education (30). Two studies performed in the patient-facing clinical setting reported positively on student medication review performance (2, 24).
Discussion
This review provides evidence that MS-focused IPE among pre-qualification HCP students is feasible and can be delivered virtually or in patient-facing, simulated or classroom-based settings. Most activities involved medical, pharmacy and nursing students and a minority involved other HCP students. Few activities were integrated into the overall curriculum or formed part of a wider IPE programme strategy. Most activities were discrete events of hours’ duration and reported assessment as/for learning, while one study described formative assessment of learning for one of the two professional groups involved. Student satisfaction with the activities and their enhanced attitudes toward IP working were commonly reported. The review provided limited, low certainty evidence that MS-focused IPE may improve students’ confidence and perception of competence for performing technical medication tasks and that it may improve medication knowledge scores and team performance. There is an absence of evidence about whether the gains seen with IPE were superior to uniprofessional education, largely due to the descriptive, non-comparative study designs employed.
The 3P theory has been widely used in IPE previously to highlight information gaps and connections between phases and provided a useful model to distinguish between different factors that influence the planning, delivery and outcome of the educational activities in this review (Freeth & Reeves, Citation2004; O’Leary et al., Citation2019; Reeves et al., Citation2016; Reeves & Freeth, Citation2006). Profession-specific considerations in relation to knowledge, skills, capabilities, experience, dominance and power observed within the 3P framework may inform future MS-focused IPE initiatives. Institutional and authority support (Carpenter & Dickinson, Citation2016; Hean & Dickinson, Citation2005) at presage (Reeves & Freeth, Citation2006) is important to foster positive intergroup attitudes in IPE. Consistent with the wider IPE literature, and without adding anything new specific to medication safety, logistics, timetable alignment, timing of IPE relative to assessment periods, cross-institutional working and staff commitment were all highlighted in this review (Achike et al., Citation2014; Bridgeman et al., Citation2018; Ernawati et al., Citation2015; Guilding et al., Citation2018; Guirguis et al., Citation2020; Kayyali et al., Citation2019; Nagge et al., Citation2017; Shelvey et al., Citation2016). Faculty relationships and context priorities for delivering IPE may positively (Achike et al., Citation2014; Chua et al., Citation2019; Hardisty et al., Citation2014; Nagge et al., Citation2017) or negatively (Begley et al., Citation2019; Ragucci et al., Citation2016; Rotz & O’Neill, Citation2020) influence student engagement and learning. Choices around teaching space (Guilding et al., Citation2018) and mode of delivery (Bartlett & Kinsey, Citation2020; Begley et al., Citation2019) were dependent on learner numbers and geographical issues, often blurring the lines between presage and process. In terms of information gaps, faculty characteristics involved in activity development and facilitation were frequently poorly reported (Anderson & Lakhani, Citation2016; Bartlett & Kinsey, Citation2020; Chua et al., Citation2019; Cooke et al., Citation2017; Guirguis et al., Citation2020; Kostas et al., Citation2018; Marshall et al., Citation2020; Ragucci et al., Citation2016; Rotz & O’Neill, Citation2020; Seselja Perisin et al., Citation2019; Shelvey et al., Citation2016) and there was limited emphasis on facilitator preparation and training: a planning oversight which will compromise the sustainability of MS-focused IPE within these institutions.
IPE is ideally planned in a collaborative manner, involving all relevant professions and stakeholders, with an agreed IPE strategy that meets different programmes’ expectations (Barr et al., Citation2016). Collaboration was evident in this review through IP activity planning working groups (Achike et al., Citation2014; Bartlett & Kinsey, Citation2020; Guilding et al., Citation2018, Citation2020; Langford et al., Citation2020; Motycka et al., Citation2018; Nagge et al., Citation2017; Paterson et al., Citation2015; Schussel et al., Citation2019; Stewart et al., Citation2010; VandeWaa et al., Citation2019), embedding the activity as core curriculum in all participating programmes (Anderson & Lakhani, Citation2016; Bartlett & Kinsey, Citation2020; Cooke et al., Citation2017; Guilding et al., Citation2020; McDonough et al., Citation2017; Nagge et al., Citation2017) and IP faculty facilitation (Achike et al., Citation2014; Bartlett & Kinsey, Citation2020; Bridgeman et al., Citation2018; Chua et al., Citation2019; Hardisty et al., Citation2014; Kayyali et al., Citation2019; McDonough et al., Citation2017, p. 24; Stewart et al., Citation2010; VandeWaa et al., Citation2019). Issues occurred where planning was driven-by or prioritized for one profession: MS-focused IPE which pertained to pharmacy curricula (Begley et al., Citation2019; Ragucci et al., Citation2016), was developed and facilitated primarily by pharmacy faculty (Begley et al., Citation2019; Bridgeman et al., Citation2018) or was voluntary for non-pharmacy students (Begley et al., Citation2019; Bridgeman et al., Citation2018; Ragucci et al., Citation2016), experienced scheduling (Bridgeman et al., Citation2018) and engagement issues (Begley et al., Citation2019; Ragucci et al., Citation2016) from non-pharmacy professions, who also reported less satisfaction (Bridgeman et al., Citation2018; Ragucci et al., Citation2016), poorer attitudes (Bridgeman et al., Citation2018) and inferior learning (Begley et al., Citation2019). In contrast, MS-focused IPE which were part of a medicine-focused strategy (Achike et al., Citation2014; Anderson & Lakhani, Citation2016), actively involved medical faculty during planning (Achike et al., Citation2014; Chua et al., Citation2019; Hardisty et al., Citation2014; Nagge et al., Citation2017) or were timed to align with experiential learning within the medical curriculum (Anderson & Lakhani, Citation2016; Kostas et al., Citation2018; Reumerman et al., Citation2021; Stewart et al., Citation2010) seemed to elicit comparable reactions and attitudes from both medical students and other professions, however often failed to consider the prior experience and curricula of other professions (Achike et al., Citation2014; Chua et al., Citation2019; Stewart et al., Citation2010). Medicine faculty involvement in IPE can be limited in comparison to other professions, particularly if there is a perceived threat to power balance or traditional medical hierarchy (Baker et al., Citation2011). Pharmacy leadership may be perceived as this threat to hierarchy, leading to poorer faculty collaboration, which further manifests in medical student engagement and outcomes (Begley et al., Citation2019; Bridgeman et al., Citation2018; Ragucci et al., Citation2016). Nursing participation and evaluation was sometimes undervalued due to absence of nursing faculty involvement at presage (Hardisty et al., Citation2014; Kayyali et al., Citation2019; Rotz & O’Neill, Citation2020), voluntary student participation and underrepresentation (Achike et al., Citation2014; Hardisty et al., Citation2014; Rotz & O’Neill, Citation2020; Stewart et al., Citation2010), under-preparation (Achike et al., Citation2014) and compromised data collection (Kayyali et al., Citation2019; Marshall et al., Citation2020; Ragucci et al., Citation2016; Stewart et al., Citation2010). Therefore, meaningful engagement of medicine faculty, without compromise to the collective leadership of other professions at presage, may support the acquisition of outcomes which are consistent across professions and approaches which are sustainable in the longer term (Guilding et al., Citation2018, Citation2020; Paterson et al., Citation2015; Taylor et al., Citation2012). The challenges of achieving a common IPE strategy across several professions are manifold as evidenced through the implementation of several extra-curricular activities, where all or some students volunteered to participate (Achike et al., Citation2014; Begley et al., Citation2019; Bridgeman et al., Citation2018; Cooke et al., Citation2017; Ernawati et al., Citation2015; Hardisty et al., Citation2014; Langford et al., Citation2020; Marshall et al., Citation2020; Paterson et al., Citation2015; Powell et al., Citation2020; Ragucci et al., Citation2016; Reumerman et al., Citation2021; Rotz & O’Neill, Citation2020; Schussel et al., Citation2019; Seselja Perisin et al., Citation2019). Student feedback called for more IPE experiences within their curricula (Langford et al., Citation2020; Motycka et al., Citation2018) and clear vertical and horizontal approaches to IPE within their own programmes (Taylor et al., Citation2012). These shortcomings may impact engagement and sustainability, particularly if a strategy is focused exclusively on the curricular needs of just one programme. Future work should explore ways to embed MS-focused IPE within a programmatic IPE strategy and how to foster equitable institutional support across participating faculty.
IPE is grounded in contact theory, the notion that bringing individuals of diverse backgrounds together can modify (positively or negatively) stereotypes and attitudes toward ingroups and outgroups (Carpenter & Dickinson, Citation2016; Hean & Dickinson, Citation2005). Intergroup contact anxiety should be considered both as a result of and a determinant of communication and teamwork in the context of non-technical skills learning in health safety (Gordon et al., Citation2017). The principle of least interest suggests that those who have the greatest power are the least likely to collaborate with one they view as inferior (Seselja Perisin et al., Citation2019). The findings in this review add to the evidence that the assurance of equal status, and the avoidance of competition between groups is necessary to nurture positive intragroup relations and facilitate learning. A mismatch in professional groups’ prior learning related to technical medication skills (Schussel et al., Citation2019), IPE experience (Ragucci et al., Citation2016), non-technical skills (Curley et al., Citation2018), or exposure to clinical practice settings (Anderson & Lakhani, Citation2016) was associated with negative findings such as limited change in IP attitudes (Schussel et al., Citation2019), compromised self-reported learning scores (Ragucci et al., Citation2016), lower satisfaction with the learning activity (Curley et al., Citation2018), and student perceived mismatch in capabilities (Anderson & Lakhani, Citation2016). Unbalanced alignment of participant professional roles with activity focus or tasks was associated with compromised IPE acceptance scores (Chua et al., Citation2019), self-confidence (Bartlett & Kinsey, Citation2020) and frustration with the lack of role clarity in the team environment (Curley et al., Citation2018). The provision of pre-activity preparation material supports each student group to bring what they have learnt in their uni-professional curriculum to and share it with other groups so that they learn with, from and about each other interprofessionally (Bartlett & Kinsey, Citation2020; Guilding et al., Citation2018; Marshall et al., Citation2020; McDonough et al., Citation2017; Paterson et al., Citation2015; Schussel et al., Citation2019; Stewart et al., Citation2010; Taylor et al., Citation2012; VandeWaa et al., Citation2019). Failure to provide preparation material to nursing students hindered their involvement in a workshop activity with medicine (Achike et al., Citation2014). Although Guilding et al, considered contact theory during presage, they reported that lack of engagement by some students compromised the experience and perceptions of IP attributes for others (Guilding et al., Citation2018, Citation2020). They propose explicit uniprofessional education on professional identity formation before IPE as a method to influence students’ expectations and experiences when they do come together in IPE. The findings in this review therefore endorse the contact theory that bringing diverse groups together can either positively or negatively affect attitudes and stereotypes and demonstrate that planning and pre-activity preparation should assure that the activity facilitates equal status by matching each professional group’s capacity, by the content being understandable and interesting to all, and the tasks being within their capability. Further, specific to MS-focused IPE, it suggests that matching may need to consider the groups’ prior learning across multiple variables: professional identity formation; technical, non-technical and IP skills and prior exposure to clinical practice settings, so as to support positive contact.
In the ideal, assessment should drive learning and align with learning outcomes (Scott, Citation2020) to enable meaningful learner engagement. One study in this review presented formal (summative) assessment of individual student learning of prescribing knowledge (matching questions) and performance (objective structured clinical exam), with the potential to appraise both technical and non-technical skills, and aligned with the reported learning outcome (Taylor et al., Citation2012). However, although most studies reported on some degree of formative individual or collective assessment as/for learning (Achike et al., Citation2014; Anderson & Lakhani, Citation2016; Bartlett & Kinsey, Citation2020; Begley et al., Citation2019; Bridgeman et al., Citation2018; Cooke et al., Citation2017; Curley et al., Citation2018; Marshall et al., Citation2020; McDonough et al., Citation2017; Motycka et al., Citation2018; Nagge et al., Citation2017; Paterson et al., Citation2015; Reumerman et al., Citation2021; Rotz & O’Neill, Citation2020; Seselja Perisin et al., Citation2019; Taylor et al., Citation2012; VandeWaa et al., Citation2019), only some of them described learning outcomes (Achike et al., Citation2014; Anderson & Lakhani, Citation2016; Bartlett & Kinsey, Citation2020; Curley et al., Citation2018; Hardisty et al., Citation2014; Marshall et al., Citation2020; McDonough et al., Citation2017; Nagge et al., Citation2017; Rotz & O’Neill, Citation2020; Taylor et al., Citation2012; VandeWaa et al., Citation2019). Some studies reported assessment as/for learning, in the absence of reported learning outcomes (Begley et al., Citation2019; Bridgeman et al., Citation2018; Cooke et al., Citation2017; Guilding et al., Citation2018; Guirguis et al., Citation2020; Kayyali et al., Citation2019; Paterson et al., Citation2015; Powell et al., Citation2020; Ragucci et al., Citation2016; Seselja Perisin et al., Citation2019) and a minority reported neither learning outcomes nor any assessment as/for learning (Ernawati et al., Citation2015; Kostas et al., Citation2018). For some studies, the focus of the assessment differed from the reported learning outcomes, for example, defining IP learning outcomes and providing feedback on individual technical medication skills (Bartlett & Kinsey, Citation2020; Curley et al., Citation2018; Rotz & O’Neill, Citation2020). These mismatches between learning outcomes and assessment approaches potentially disable student engagement and development because it is unclear what knowledge, skills or behavior the learning activity seeks to develop. The absence of formal, summative assessment is not surprising and is indeed potentially appropriate given the duration of the reported activities, typically described as hours, with a small minority running over 1–3 days. Most studies reported the session contact hours, as distinct from the learning hours inclusive of (self)-directed learning. Assessment of IPE at undergraduate level is challenging, and the formative assessment methods described in this review appeared on the whole to align with current guidance (Rogers et al., Citation2017). Future activities should define learning outcomes and associated assessment approaches, and signpost how and if engagement in a discrete MS-focused IPE activity contributes to the learner’s overall programme development.
Seminal investigations into the causes of medication errors identify inadequate intra- or interprofessional communication and teamworking as frequent contributory factors (Dornan et al., Citation2009; Ryan et al., Citation2014). Therefore, the nature of how groups of students interact and co-operate, and how this is assessed, may be important to drive the development of non-technical skills and collective performance required to develop future safe medication practices and medication safety (Dearden et al., Citation2015; Gordon et al., Citation2015). This also aligns with two conditions of the contact hypothesis, as applied to IPE, necessary to reduce negative intergroup attitudes and stereotypes: (1) groups should have common goals and (2) should co-operate, not compete. Most activities (n = 21) in this review reported assigning a collective task to the IP group (Achike et al., Citation2014; Anderson & Lakhani, Citation2016; Begley et al., Citation2019; Bridgeman et al., Citation2018; Curley et al., Citation2018; Guilding et al., Citation2018, Citation2020; Guirguis et al., Citation2020; Hardisty et al., Citation2014; Kostas et al., Citation2018; Marshall et al., Citation2020; McDonough et al., Citation2017; Motycka et al., Citation2018; Paterson et al., Citation2015; Ragucci et al., Citation2016; Reumerman et al., Citation2021; Schussel et al., Citation2019; Seselja Perisin et al., Citation2019; Stewart et al., Citation2010; Taylor et al., Citation2012; VandeWaa et al., Citation2019), including group case management, group presentation, group error disclosure or significant event analysis. Most (n = 14) of these formatively assessed group efforts, typically using discussion, feedback and debriefing (Anderson & Lakhani, Citation2016; Begley et al., Citation2019; Chua et al., Citation2019; Curley et al., Citation2018; Marshall et al., Citation2020; McDonough et al., Citation2017; Motycka et al., Citation2018; Paterson et al., Citation2015; Ragucci et al., Citation2016; Reumerman et al., Citation2021; Schussel et al., Citation2019; VandeWaa et al., Citation2019), in one case by application of the group’s treatment plan to a SimMan (Guilding et al., Citation2020) and in another using a validated tool to assess and provide feedback on team performance (Begley et al., Citation2019). Some of these studies also evaluated the group effort and reported this as a study outcome measure: assessing team proficiency (Ragucci et al., Citation2016), administering tools to assess perceptions of interprofessionalism, collaboration or teamwork before and after the intervention (Begley et al., Citation2019; Curley et al., Citation2018; Kostas et al., Citation2018; Motycka et al., Citation2018; Reumerman et al., Citation2021; Schussel et al., Citation2019). In several evaluations, the baseline scores were so high as to limit the potential to observe any intervention-related improvement (Kostas et al., Citation2018; Motycka et al., Citation2018; Schussel et al., Citation2019). Assessment of IPE in pre-qualification courses should preferably consider both individual and collective performance (Rogers et al., Citation2017). Little is known about how best to assess medication safety at pre-qualification stage. The WHO patient safety curriculum for improving medication safety describes individual, not collective, knowledge- and performance-related learning outcomes (WHO, Citation2009). The UK pre-qualification national prescribing safety assessment focuses on individual, technical prescribing performance (Maxwell et al., Citation2017). Published consensus on learning outcomes to enhance non-technical skills in the context of medication safety largely relates to individual performance in a collective setting (Gordon et al., Citation2015), although there is a lack of consensus on how to assess non-technical skills in undergraduate medical education (Gordon et al., Citation2019). Research should focus on defining the skillset (individual and collective skills, technical and non-technical), the associated learning outcomes and assessment approaches necessary in pre-qualification HCP courses to support future IP practice and medication safety post-qualification.
There is limited evidence within this review that learning which was designed at presage or process with a theoretical basis was more likely to advance learning: two studies designed the activity on an IPE theoretical framework, constructed the activity around sound pedagogical approaches, building on prior knowledge, scaffolding the learning. These studies demonstrated positive alignment between learning outcomes, assessment approaches and provided evidence of actual or perceived learning development (Anderson & Lakhani, Citation2016; Taylor et al., Citation2012); six studies designed the activity around simulation-based learning theoretical frameworks and showed evidence of congruence between learning outcomes, nature of student engagement and interaction with and during the activity, assessment approaches and learning evaluation (Begley et al., Citation2019; Cooke et al., Citation2017; Kayyali et al., Citation2019; Motycka et al., Citation2018; Paterson et al., Citation2015; VandeWaa et al., Citation2019). These six studies all presented evidence of perceived or actual learning development. A greater proportion of the theory-based activities, compared to those without, presented a patient-centered focus (). The evidence in this review supports the assertion that theory-based IPE design and delivery, within presage and process, enables more effective product: the development and evaluation of learning, albeit that such planning is intellectually rigorous and time consuming (Hean et al., Citation2012). It follows, therefore, that for higher education institutions to deliver effective MS-focused IPE, they should invest in and resource faculty’s time and efforts to do so.
The 3P product findings reported within this review identify that there is limited, low certainty evidence that MS-focused IPE was no less effective (non-inferior) to uniprofessional education regarding individual technical medication safety performance (Taylor et al., Citation2012) and group performance (Ragucci et al., Citation2016) and that MS-IPE carries the potential to influence IP competence, MS-related technical or non-technical skills. It has been recommended that systematic reviews of learning should elucidate how, why, when and for whom educational interventions work (Gordon et al., Citation2017; Wong et al., Citation2012). The evidence presented here is limited in this regard. Additionally, quality assessment highlighted an absence of rigor, particularly to qualitative data collected (Begley et al., Citation2019; Hardisty et al., Citation2014; Reumerman et al., Citation2021; Taylor et al., Citation2012; VandeWaa et al., Citation2019), and a lack of triangulation between qualitative and quantitative data sources in mixed-methods designs (Begley et al., Citation2019; Ernawati et al., Citation2015; Guirguis et al., Citation2020; Hardisty et al., Citation2014; Reumerman et al., Citation2021; Taylor et al., Citation2012; VandeWaa et al., Citation2019). Although it is beyond the scope of this review to appraise the choice of instrument to measure perceptions of teamwork, collaboration and interprofessionalism, it is worth noting that several of the applied tools identified baseline scores at the upper end of the range. It is unclear whether this reflects on the validity of the tool or the students’ baseline development. This review reports on literature published before October 2020 and it is possible that material that emerged in the year following has been omitted. Future scholarly research on MS-focused IPE should address these gaps at study design, to reduce planning oversights and improve the validity of learning and evaluation outcomes. The protocol for this systematic review was not pre-registered and although available from the authors, the absence of pre-publication potentially lessens the credibility of the reported methods and findings.
Conclusion
The evidence presented in this systematic review shows that MS-focused IPE for pre-qualification HCPs may support the acquisition of technical and non-technical skills aligned with medication safety. Careful planning is required to ensure matching of students’ and groups’ technical and non-technical skills, professional identity and learner attributes to enhance learning in an interprofessional setting. Overcoming challenges to embedding MS-focused IPE into the standard curricula is necessary to optimize constructive alignment, learner engagement, quality and drive development. Future work should define the required skillset in pre-qualification HCP programmes to facilitate future safe medication practice, together with the associated learning outcomes and assessment approaches. Higher education institutions should consider the support available to faculty and clinical staff to plan, deliver and evaluate MS-focused IPE and optimize the visibility of and access to this support to students and faculty alike. There is room to improve the quality of scholarly studies examining these MS-focused IPE by employing comparative study design, selecting valid and reliable outcome measures and evaluating learning and development outcomes.
Supplemental Material
Download MS Word (81.1 KB)Supplemental Material
Download MS Word (12.9 KB)Supplemental Material
Download MS Word (21.6 KB)Acknowledgments
None.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
Notes on contributors
TC Grimes
Tamasine Grimes, B.Sc.(Pharm), M.Sc., PhD, MPSI is Associate Professor in the Practice of Pharmacy at the School of Pharmacy and Pharmaceutical Sciences, Trinity College Dublin. Dr Grimes has a special interest in interprofessional education, medication safety and clinical pharmacy.
EM Guinan
Emer Guinan is an Assistant Professor in Interprofessional Learning at the School of Medicine, Trinity College Dublin. Dr Guinan has a special interest in exercise oncology and interprofessional education.
References
- Achike, F. I., Smith, J., Leonard, S., Williams, J., Browning, F., & Glisson, J. (2014). Advancing safe drug use through interprofessional learning (IPL): A pilot study. The Journal of Clinical Pharmacology, 54(7), 832–839. https://doi.org/10.1002/jcph.289
- Anderson, E., & Lakhani, N. (2016). Interprofessional learning on polypharmacy. The Clinical Teacher, 13(4), 291–297. https://doi.org/10.1111/tct.12485
- Avery, A. J., Ghaleb, M., Barber, N., Franklin, B. D., Armstrong, S. J., Serumaga, B., Dhillon, S., Freyer, A., Howard, R., Talabi, O., & Mehta, R. L. (2013). The prevalence and nature of prescribing and monitoring errors in English general practice: A retrospective case note review. British Journal of General Practice, 63(613), e543–e553. https://doi.org/10.3399/bjgp13X670679
- Baker, L., Egan-Lee, E., Martimianakis, M. A., & Reeves, S. (2011). Relationships of power: Implications for interprofessional education. Journal of Interprofessional Care, 25(2), 98–104. https://doi.org/10.3109/13561820.2010.505350
- Bardet, J.-D., Vo, T.-H., Bedouch, P., & Allenet, B. (2015). Physicians and community pharmacists collaboration in primary care: A review of specific models. Research in Social and Administrative Pharmacy, 11(5), 602–622. https://doi.org/10.1016/j.sapharm.2014.12.003
- Barr, H., Gray, R., Helme, M., Low, H., & Reeves, S. (2016). CAIPE: Interprofessional Education Guidelines 2016. Fareham (UK): CAIPE (Centre for Advancement of Interprofessional Education). ISBN: 978-0-9571382-3-0. https://www.caipe.org/download/caipe-interprofessional-education-guidelines-2016-1-pdf/
- Bartlett, J. L., & Kinsey, J. D. (2020). Large-group, asynchronous, interprofessional simulation: Identifying roles and improving communication with student pharmacists and student nurses. Currents in Pharmacy Teaching and Learning, 12(6), 763–770. https://doi.org/10.1016/j.cptl.2020.01.023
- Begley, K., O’Brien, K., Packard, K., Castillo, S., Haddad, A. R., Johnson, K., … Pick, A. (2019). Interprofessional telehealth case activities improve students’ perceptions of their ability to provide collaborative care. American Journal of Pharmaceutical Education, 8383(4), 474–481. doi:10.5688/ajpe6880.
- Biggs, J. B. (1993). From theory to practice: A cognitive systems approach. Higher Education Research & Development, 12(1), 73–85. https://doi.org/10.1080/0729436930120107
- Brady, A., Malone, A., & Fleming, S. (2009). A literature review of the individual and systems factors that contribute to medication errors in nursing practice. Journal of Nursing Management, 17(6), 679–697. https://doi.org/10.1111/j.1365-2834.2009.00995.x
- Bridgeman, M. B., Rusay, M., Afran, J., Yeh, D. S., & Sturgill, M. G. (2018). Impact of an interprofessional medication error workshop on healthcare student perception. Currents in Pharmacy Teaching and Learning, 10(7), 975–981. https://doi.org/10.1016/j.cptl.2018.04.013
- Canadian Interprofessional Health Collaborative (2010). A national interprofessional competency framework. ISbN 9781. ISbN 9781926819075 926819075 https://www.mcgill.ca/ipeoffice/ipe-curriculum/cihc-framework
- Carpenter, J., & Dickinson, C. (2016). Understanding interprofessional education as an intergroup encounter: The use of contact theory in programme planning. Journal of Interprofessional Care, 30(1), 103–108. https://doi.org/10.3109/13561820.2015.1070134
- Chua, S. S., Lai, P. S. M., Sim, S. M., Tan, C. H., & Foong, C. C. (2019). Acceptance of interprofessional learning between medical and pharmacy students in a prescribing skills training workshop: Pre-post intervention study. BMC Medical Education, 19(1), 101. https://doi.org/10.1186/s12909-019-1525-y
- Cooke, C., Gormley, G. J., Haughey, S., & Barry, J. (2017). Tracing the prescription journey: A qualitative evaluation of an interprofessional simulation-based learning activity. Advances in Simulation, 2(1), 14. https://doi.org/10.1186/s41077-017-0047-0
- Cordina, M. (2019). Preparing the health workforce to enhance medication safety. Research in Social and Administrative Pharmacy, 15(7), 813–814. https://doi.org/10.1016/j.sapharm.2019.03.002
- Curley, L. E., Jensen, M., McNabb, C., Ram, S., Torrie, J., Jowsey, T., & McDonald, M. (2018). Pharmacy student perspective of interprofessional learning in a simulated ward environment course. American Journal of Pharmaceutical Education August 2019, 83(6), 6848. https://doi.org/10.5688/ajpe6848
- Dearden, E., Mellanby, E., Cameron, H., & Harden, J. (2015). Which non‐technical skills do junior doctors require to prescribe safely? A systematic review. British Journal of Clinical Pharmacology, 80(6), 1303–1314. https://doi.org/10.1111/bcp.12735
- Donaldson, L. J., Kelley, E. T., Dhingra-Kumar, N., Kieny, M.-P., & Sheikh, A. (2017). Medication without harm: WHO’s third global patient safety challenge. The Lancet, 389(10080), 1680–1681. https://doi.org/10.1016/S0140-6736(17)31047-4
- Dornan, T., Ashcroft, D., Heathfield, H., Lewis, P., Miles, J., Taylor, D., … Wass, V. (2009). An in-depth investigation into causes of prescribing errors by foundation trainees in relation to their medical education: EQUIP study (pp. 1–215).London, United Kingdom: General Medical Council.
- Elliott, R. A., Camacho, E., Jankovic, D., Sculpher, M. J., & Faria, R. (2021). Economic analysis of the prevalence and clinical and economic burden of medication error in England. BMJ Quality & Safety, 30(2), 96–105. https://doi.org/10.1136/bmjqs-2019-010206
- Ernawati, D. K., Lee, Y. P., & Hughes, J. (2015). Indonesian students’ participation in an interprofessional learning workshop. Journal of Interprofessional Care, 29(4), 398–400. https://doi.org/10.3109/13561820.2014.991911
- Franklin, B. (2014). Medication errors: Do they occur in isolation? BMJ Quality & Safety, 23(5), e1. https://doi.org/10.1136/bmjqs-2014-002924
- Freeth, D., & Reeves, S. (2004). Learning to work together: Using the presage, process, product (3P) model to highlight decisions and possibilities. Journal of Interprofessional Care, 18(1), 43–56. https://doi.org/10.1080/13561820310001608221
- Gordon, M., Box, H., Halliwell, J.-A., Farrell, M., Parker, L., & Stewart, A. (2015). Enhancing health care non-technical skills: The TINSELS programme. The Clinical Teacher, 12(6), 413–417. https://doi.org/10.1111/tct.12433
- Gordon, M., Farnan, J., Grafton-Clarke, C., Ahmed, R., Gurbutt, D., McLachlan, J., & Daniel, M. (2019). Non-technical skills assessments in undergraduate medical education: A focused BEME systematic review: BEME Guide No. 54. Medical Teacher, 41(7), 732–745. https://doi.org/10.1080/0142159X.2018.1562166
- Gordon, M., Fell, C. W. R., Box, H., Farrell, M., & Stewart, A. (2017). Learning health ‘safety’ within non-technical skills interprofessional simulation education: A qualitative study. Medical Education Online, 22(1), 1272838. https://doi.org/10.1080/10872981.2017.1272838
- Gordon, M., & Gibbs, T. (2014). STORIES statement: Publication standards for healthcare education evidence synthesis. BMC Medicine, 12(1), 143. https://doi.org/10.1186/s12916-014-0143-0
- Guilding, C., Hardisty, J., Randles, E., Statham, L., Green, A., Bhudia, R., Thandi, C. S., & Matthan, J. (2018). Making it work: The feasibility and logistics of delivering large-scale interprofessional education to undergraduate healthcare students in a conference format. Journal of Interprofessional Care, 32(5), 653–655. https://doi.org/10.1080/13561820.2018.1496074
- Guilding, C., Hardisty, J., Randles, E., Statham, L., Green, A., Bhudia, R., Thandi, C. S., Teodorczuk, A., Scott, L., & Matthan, J. (2020). Designing and evaluating an interprofessional education conference approach to antimicrobial education. BMC Medical Education, 20(1), 360. https://doi.org/10.1186/s12909-020-02252-9
- Guirguis, F., Andrade, R., Beck, C., Ellen, D., Slivecka, J., & Richard, C. L. (2020). Partners in pharmacy: An intraprofessional educational event with pharmacy and pharmacy technician students. Currents in Pharmacy Teaching and Learning, 12(3), 302–306. https://doi.org/10.1016/j.cptl.2019.12.010
- Hardisty, J., Scott, L., Chandler, S., Pearson, P., & Powell, S. (2014). Interprofessional learning for medication safety. The Clinical Teacher, 11(4), 290–296. https://doi.org/10.1111/tct.12148
- Hean, S., Craddock, D., Hammick, M., & Hammick, M. (2012). Theoretical insights into interprofessional education: AMEE Guide No. 62. Medical Teacher, 34(2), e78–101. https://doi.org/10.3109/0142159x.2012.650740
- Hean, S., & Dickinson, C. (2005). The contact hypothesis: An exploration of its further potential in interprofessional education. Journal of Interprofessional Care, 19(5), 480–491. https://doi.org/10.1080/13561820500215202
- Heaton, A., Webb, D. J., & Maxwell, S. R. (2008). Undergraduate preparation for prescribing: The views of 2413 UK medical students and recent graduates. British Journal of Clinical Pharmacology, 66(1), 128–134. https://doi.org/10.1111/j.1365-2125.2008.03197.x
- Hong, Q. N., Pluye, P., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., … O’Cathain, A. (2018). Mixed methods appraisal tool (MMAT), version 2018. IC Canadian Intellectual Property Office, Industry Canada. IOS Press. https://content.iospress.com/articles/education-for-information/efi180221
- Interprofessional Education Collaborative (2016). Core competencies for interprofessional collaborative practice: 2016 update. https://aamc-meded.global.ssl.fastly.net/production/media/filer_public/70/9f/709fedd7-3c53-492c-b9f0-b13715d11cb6/core_competencies_for_collaborative_practice.pdf
- Kayyali, R., Harrap, N., Albayaty, A., Savickas, V., Hammell, J., Hyatt, F., Elliott, K., & Richardson, S. (2019). Simulation in pharmacy education to enhance interprofessional education. International Journal of Pharmacy Practice, 27(3), 295–302. https://doi.org/10.1111/ijpp.12499
- Keers, R. N., Williams, S. D., Cooke, J., & Ashcroft, D. M. (2013). Causes of medication administration errors in hospitals: A systematic review of quantitative and qualitative evidence. Drug Safety, 36(11), 1045–1067. https://doi.org/10.1007/s40264-013-0090-2
- Kostas, T., Thomas, J., Thompson, K., Poston, J., & Levine, S. (2018). Improving medical and pharmacy student confidence in medication management and attitudes about interprofessional collaboration by utilizing an interprofessional module. Journal of Interprofessional Care, 32(6), 790–793. https://doi.org/10.1080/13561820.2018.1512957
- Krathwohl, D. (2002). A revision of bloom’s taxonomy: An overview. Theory into Practice, 41(4), 212–218. https://doi.org/10.1207/s15430421tip4104_2
- Langford, D. J., Gordon, D. B., Loeseer, J. D., Tauben, D. J., & Doorenbos, A. Z. (2020). Evaluation of an interprofessional active learning session on acute pain and opioid use disorder using the interprofessional collaborative competency attainment scale. Journal of Interprofessional Care, 34(2), 193–201. https://doi.org/10.1080/13561820.2019.1629398
- Löffler, C., Koudmani, C., Böhmer, F., Paschka, S. D., Höck, J., Drewelow, E., Stremme, M., Stahlhacke, B., & Altiner, A. (2017). Perceptions of interprofessional collaboration of general practitioners and community pharmacists - a qualitative study. BMC Health Services Research, 17(1), 224. https://doi.org/10.1186/s12913-017-2157-8
- Luetsch, K., & Rowett, D. (2016). Developing interprofessional communication skills for pharmacists to improve their ability to collaborate with other professions. Journal of Interprofessional Care, 30(4), 458–465. https://doi.org/10.3109/13561820.2016.1154021
- Marshall, C., Van Der Volgen, J., Lombardo, N., Hamasu, C., Cardell, E., & Blumenthal, D. K. (2020). A mixed methods approach to assess the impact of an interprofessional education medical error simulation. American Journal of Pharmaceutical Education, 84(2), 7133. https://doi.org/10.5688/ajpe7133
- Maxwell, S. R. J., Coleman, J. J., Bollington, L., Taylor, C., & Webb, D. J. (2017). Prescribing safety assessment 2016: Delivery of a national prescribing assessment to 7343 UK final-year medical students. British Journal of Clinical Pharmacology, 83(10), 2249–2258. https://doi.org/10.1111/bcp.13319
- Maxwell, S. R., Cameron, I. T., & Webb, D. J. (2015). Prescribing safety: Ensuring that new graduates are prepared. The Lancet, 385(9968), 579–581. https://doi.org/10.1016/S0140-6736(14)62339-4
- McDonough, K. A., White, A. A., Odegard, P. S., & Shannon, S. E. (2017). Interprofessional error disclosure training for medical, nursing, pharmacy, dental, and physician assistant students. MedEdPORTAL, 13, 10606. https://doi.org/10.15766/mep_2374-8265.10606
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
- Motycka, C., Egelund, E. F., Gannon, J., Genuardi, F., Sautam, S., Stittsworth, S., Young, A., & Simon, L. (2018). Using interprofessional medication management simulations. Currents in Pharmacy Teaching and Learning, 10(7), 982–989. https://doi.org/10.1016/j.cptl.2018.04.010
- Nagge, J. J., Lee-Poy, M. F., & Richard, C. L. (2017). Evaluation of a unique interprofessional education program involving medical and pharmacy students. American Journal of Pharmaceutical Education, 81(10), 6140. https://doi.org/10.5688/ajpe6140
- Noble, C., Brazil, V., Teasdale, T., Forbes, M., & Billett, S. (2017). Developing junior doctors’ prescribing practices through collaborative practice: Sustaining and transforming the practice of communities. Journal of Interprofessional Care, 31(2), 263–272. doi:10.1080/13561820.2016.1254164.
- O’Leary, N., Salmon, N., Clifford, A., O’Donoghue, M., & Reeves, S. (2019). ‘Bumping along’: A qualitative metasynthesis of challenges to interprofessional placements. Medical Education, 53(9), 903–915. https://doi.org/10.1111/medu.13891
- Paterson, R., Rolfe, A., Coll, A., & Kinnear, M. (2015). Interprofessional prescribing masterclass for medical students and non-medical prescribing students (nurses and pharmacists) a pilot study. Scottish Medical Journal, 60(4), 202–207. https://doi.org/10.1177/0036933015606583
- Pearson, P., Scott, L., Hardisty, J., & Green, A. (2015). Educational Interventions. In Tully M.P. and Franklin B.D. (Eds.), Safety in medication use (pp. 171–186). CRC Press.
- Powell, B., Jardine, K. D., Steed, M., Adams, J., & Mason, B. (2020). Enhanced nursing self-awareness and pharmacotherapy knowledge-base: Peer-teaching and nursing/pharmacy interprofessional education. Medical Education Online, 25(1), 1814551. https://doi.org/10.1080/10872981.2020.1814551
- Ragucci, K. R., Kerri, D. H., & Shrader, S. P. (2016). Evaluation of interprofessional team disclosure of a medical error to a simulated patient. American Journal of Pharmaceutical Education, 80(8), 138. https://doi.org/10.5688/ajpe808138
- Reeves, S., Fletcher, S., Barr, H., Birch, I., Boet, S., Davies, N., McFadyen, A., Rivera, J., & Kitto, S. (2016). A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Medical Teacher, 38(7), 656–668. https://doi.org/10.3109/0142159x.2016.1173663
- Reeves, S., & Freeth, D. (2006). Re-examining the evaluation of interprofessional education for community mental health teams with a different lens: Understanding presage, process and product factors. Journal of Psychiatric and Mental Health Nursing, 13(6), 765–770. https://doi.org/10.1111/j.1365-2850.2006.01032.x
- Reeves, S., Perrier, L., Goldman, J., Freeth, D., & Zwarenstein, M. (2013). Interprofessional education: Effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, (3), 1465–1858. John Wiley & Sons, Ltd. https://doi.org/10.1002/14651858.CD002213.pub3
- Reeves, S., Zwarenstein, M., Goldman, J., Barr, H., Freeth, D., Hammick, M., & Koppel, I. (2008). Interprofessional education: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews, (1). https://doi.org/10.1002/14651858.CD002213.pub2
- Reumerman, M. O., Richir, M. C., Domela Nieuwenhuis, P. M., Sultan, R., Daelmans, H. E. M., Springer, H., Muller, M., van Agtmael, M. A., & Tichelaar, J. (2021). The clinical and educational outcomes of an inter-professional student-led medication review team, a pilot study. European Journal of Clinical Pharmacology, 77(1), 117–123. https://doi.org/10.1007/s00228-020-02972-3
- Rickles, N. M., Noland, C. M., Tramontozzi, A., & Vinci, M. A. (2010). Pharmacy student knowledge and communication of medication errors. American Journal of Pharmaceutical Education, 74(4), 60. https://doi.org/10.5688/aj740460
- Rixon, S., Braaf, S., Williams, A., Liew, D., & Manias, E. (2015). Pharmacists’ interprofessional communication about medications in specialty hospital settings. Health Communication, 30(11), 1065–1075. https://doi.org/10.1080/10410236.2014.919697
- Rogers, G. D., Thistlethwaite, J. E., Anderson, E. S., Abrandt Dahlgren, M., Grymonpre, R. E., Moran, M., & Samarasekera, D. D. (2017). International consensus statement on the assessment of interprofessional learning outcomes. Medical Teacher, 39(4), 347–359. https://doi.org/10.1080/0142159x.2017.1270441
- Rosenfeld, E., Kinney, S., Weiner, C., Newall, F., Williams, A., Cranswick, N., Wong, I., Borrott, N., & Manias, E. (2018). Interdisciplinary medication decision making by pharmacists in pediatric hospital settings: An ethnographic study. Research in Social and Administrative Pharmacy, 14(3), 269–278. https://doi.org/10.1016/j.sapharm.2017.03.051
- Ross, S., Ryan, C., Duncan, E. M., Francis, J. J., Johnston, M., Ker, J. S., McKay, G., Maxwell, S., McKay, G., McLay, J., Webb, D. J., Bond, C., & Lee, A. J. (2013). Perceived causes of prescribing errors by junior doctors in hospital inpatients: A study from the PROTECT programme. BMJ Quality & Safety, 22(2), 97–102. https://doi.org/10.1136/bmjqs-2012-001175
- Rotz, M. E., & O’Neill, D. D. (2020). Exploring second professional year pharmacy student reflections after an interprofessional shadowing experience with nursing students in critical care units: A qualitative study. Journal of Interprofessional Care, 2021 May 4; 35(3), 383–90. https://doi.org/10.1080/13561820.2020.1769579
- Roughead, E. E., Semple, S. J., & Rosenfeld, E. (2016). The extent of medication errors and adverse drug reactions throughout the patient journey in acute care in Australia. International Journal of Evidence-Based Healthcare, 14 (3), 113–122. (Issue 3: Medication Safety Issue). https://doi.org/10.1097/xeb.0000000000000075
- Roughead, L., Semple, S., & Rosenfeld, E. (2013). Literature review: Medication safety in Australia. Australian Commission on Safety and Quality in Health Care, Sydney. https://www.safetyandquality.gov.au/sites/default/files/migrated/Literature-Review-Medication-Safety-in-Australia-2013.pdf
- Ryan, C., Ross, S., Davey, P., Duncan, E. M., Francis, J. J., Fielding, S., MacLeod, J., Lee, A. J., MacLeod, M. J., Maxwell, S., McKay, G. A., McLay, J. S., Webb, D. J., Bond, C., & Johnston, M. J. (2014). Prevalence and causes of prescribing errors: The prescribing outcomes for trainee doctors engaged in clinical training (PROTECT) study. PloS One, 9(1), e79802. https://doi.org/10.1371/journal.pone.0079802
- Schmitz, K., Lenssen, R., Rosentreter, M., Groß, A., & Eisert, A. (2015). Wide cleft between theory and practice: Medical students’ perception of their education in patient and medication safety. Die Pharmazie-An International Journal of Pharmaceutical Sciences, 70(5), 351–354. https://doi.org/10.1691/ph.2015.4836
- Schussel, K. E., Forbes, S., Taylor, A. M., & Cooley, J. H. (2019). Implementation of an interprofessional medication therapy management experience. American Journal of Pharmaceutical Education, 83(3), 6584. https://doi.org/10.5688/ajpe6584
- Scott, I. M. (2020). Beyond ‘driving’: The relationship between assessment, performance and learning. Medical Education, 54(1), 54–59. https://doi.org/10.1111/medu.13935
- Seselja Perisin, A., Mestrovic, A., Bozic, J., Kacic, J., Bukic, J., Leskur, D., … Modun, D. (2019). Interprofessional pharmacotherapy workshop: Intervention to improve health professionals’ and students’ attitudes towards collaboration between physicians and pharmacists. Journal of Interprofessional Care, 33(5), 456–463. https://doi.org/10.1080/13561820.2018.1541875
- Shelvey, B. M., Coulman, S. A., & John, D. N. (2016). Evaluating an undergraduate interprofessional education session for medical and pharmacy undergraduates on therapeutics and prescribing: The medical student perspective. Adv Med Educ Pract, 7, 661–670. https://doi.org/10.2147/amep.S116618
- Slight, S. P., Howard, R., Ghaleb, M., Barber, N., Franklin, B. D., & Avery, A. J. (2013). The causes of prescribing errors in English general practices: A qualitative study. British Journal of General Practice, 63(615), e713–e720. https://doi.org/10.3399/bjgp13X673739
- Stewart, M., Purdy, J., Kennedy, N., & Burns, A. (2010). An interprofessional approach to improving paediatric medication safety. BMC Medical Education, 10(1), 19. https://doi.org/10.1186/1472-6920-10-19
- Taylor, D., Yuen, S., Hunt, L., & Emond, A. (2012). An interprofessional pediatric prescribing workshop. American Journal of Pharmaceutical Education, 76(6), 111. https://doi.org/10.5688/ajpe766111
- The World Health Professions Alliance. (2019). WHPA statement on interprofessional collaborative practice. https://www.whpa.org/node/30
- VandeWaa, E., Bealle Rudd, A., Estis, J. M., & Gordon-Hickey, S. (2019). Safe medication administration in patients with communication disorders: A simulation-enhanced interprofessional education approach. Journal of Allied Health, 48(4), 257–262. https://www.ingentaconnect.com/content/asahp/jah/2019/00000048/00000004/art00004
- Wilson, A. J., Palmer, L., Levett-Jones, T., Gilligan, C., & Outram, S. (2016). Interprofessional collaborative practice for medication safety: Nursing, pharmacy, and medical graduates’ experiences and perspectives. Journal of Interprofessional Care, 30(5), 649–654. https://doi.org/10.1080/13561820.2016.1191450
- Wong, G., Greenhalgh, T., Westhorp, G., & Pawson, R. (2012). Realist methods in medical education research: What are they and what can they contribute? Medical Education, 46(1), 89–96. https://doi.org/10.1111/j.1365-2923.2011.04045.x
- World Health Organization. (2009). WHO patient safety curriculum guide for medical schools. (2009). https://www.who.int/patientsafety/education/curriculum_guide_medical_schools/en/
- World Health Organization. (2010). Framework of action on interprofessional education and collaborative practice. http://whqlibdoc.who.int/hq/2010/WHO_HRH_HPN_10.3_eng.pdf
- World Health Organization. (2019a). Medication safety in polypharmacy: Technical report. ( 2019). https://apps.who.int/iris/bitstream/handle/10665/325454/WHO-UHC-SDS-2019.11-eng.pdf
- World Health Organization. (2019b). Medication safety in transitions of care: Technical report. ( 2019). https://apps.who.int/iris/bitstream/handle/10665/325453/WHO-UHC-SDS-2019.9-eng.pdf?ua=1
- Zwarenstein, M., Atkins, J., Barr, H., Hammick, M., Koppel, I., & Reeves, S. (1999). A systematic review of interprofessional education. Journal of Interprofessional Care, 13(4), 417–424. https://doi.org/10.3109/13561829909010386