ABSTRACT
Clinical reasoning is a core ability in the health professions, but the term is conceptualised in multiple ways within and across professions. For interprofessional teamwork it is indispensable to recognise the differences in understanding between professions. Therefore, our aim was to investigate how nurses, physicians, and medical and nursing students define clinical reasoning. We conducted 43 semi-structured interviews with an interprofessional group from six countries and qualitatively analysed their definitions of clinical reasoning based on a coding guide. Our results showed similarities across professions, such as the emphasis on clinical skills as part of clinical reasoning. But we also revealed differences, such as a more patient-centered view and a broader understanding of the clinical reasoning concept in nurses and nursing students. The explicit sharing and discussion of differences in the understanding of clinical reasoning across health professions can provide valuable insights into the perspectives of different team members on clinical practice and education. This understanding may lead to improved interprofessional collaboration, and our study's categories and themes can serve as a basis for such discussions.
Introduction
Clinical reasoning (CR) can play a critical role in the health professions and is essential for clinical practice and patient safety. It is a core ability that students have to acquire during their education (Higgs et al., Citation2019), and health profession educators largely agree on a need to teach CR explicitly and longitudinally in health profession education (Kononowicz et al., Citation2020). Despite the importance of clinical reasoning for the education and practice in healthcare, it is a term that has been defined and conceptualised in multiple ways.
A variety of terms are used in CR research, such as clinical decision-making, clinical judgment, or medical problem solving (Holder, Citation2018; Koufidis et al., Citation2021), which are similarly not well defined. For example, Kahlke and Eva (Citation2018) conducted an interview study with professionals from the fields of medicine, nursing, pharmacy, and social work to define the term “critical thinking.” They discovered that biomedical critical thinking was dominant. In nursing, the concepts of critical thinking, clinical reasoning, and clinical judgment are typically interrelated sets of processes that are important for the nursing process (Victor-Chmil, Citation2013). Young et al. (Citation2020) conducted a qualitative analysis of the literature to identify terms describing clinical reasoning. They encountered 110 different terms, which they clustered into six categories intending to support using a precise terminology across healthcare professions. In another study they asked a team of researchers from various backgrounds (e.g., medicine, rehabilitation, or cognitive psychology), for their personal definitions and conceptualisations of clinical reasoning and based on these developed boundary conditions of what is and is not clinical reasoning (Young et al., Citation2018). For example, communication skills were identified as not part of the clinical reasoning process. Such a heterogeneous understanding of clinical reasoning is a challenge for interprofessional collaboration and teaching clinical reasoning (Young et al., Citation2020).
In our EU-funded project we aimed to develop an interprofessional curriculum for health professions students and educators (DID-ACT, https://www.did-act.eu). During the first phase of our collaboration, we realised that within our multi-professional consortium we had different conceptualisations of clinical reasoning, similar to the experiences of Young et al. (Citation2018). Therefore, we needed to develop a common understanding prior to starting curriculum development. We also wanted to better understand our main target groups for our curriculum—nurses, physicians, medical and nursing students to be able to better meet their needs and consider their level of understanding. These target groups typically do not have much expertise in the theoretical foundations of CR in contrast to the researcher study population of Young et al. (Citation2018, Citation2020), and to our knowledge such a study looking into CR conceptualisations of health professionals/health professional educators and students without specific experience in CR research has not yet been conducted.
Therefore, our aim was to explore how nurses, physicians, nursing, and medical students (who are neither experienced in CR research nor experts in CR teaching) define clinical reasoning. We also wanted to explore differences and similarities between the definitions and compare them to the definitions from the literature and CR researchers analysed by Young et al. (Citation2018, Citation2019, Citation2020). The results of this study can facilitate interprofessional collaboration and education on this topic.
Methods
To answer these questions, we implemented a qualitative content analysis. We based our study on interviews conducted with healthcare professionals and students without a background in CR research or teaching. We asked the interviewees how they define CR.
Reflexivity
We selected our study team to enable us to have a broad perspective on the topic. The team includes members who represent a junior perspective (LH as a final year medical student, MS as a PhD candidate, and CG as a recent PhD graduate). But we also had more experienced researchers (SD, SH, AK, IH, CS), who had experience in qualitative research and a background in clinical reasoning-related research. The nursing profession was represented by CG and CS and the medical profession by MS and SD; all medical and nursing representatives were experienced practicing healthcare professionals. We discussed our understanding of relevant concepts and all steps of the study implementation within our team and made joint decisions. For our study, we agreed on a definition of interprofessional collaboration provided by Higgs et al. (Citation2019): “Clinicians work ‘deliberately,’ together with the patient and family to provide optimal health care” that acknowledges “many differences [between health professions], including their professinal cultures” but has in common “their caring for the patient and family” (p. 185).
Data collection
As part of the DID-ACT project we conducted semi-structured interviews with practicing physicians and nurses from our partner countries in Europe (Germany, Poland, Slovenia, Sweden, and Switzerland) to identify barriers and challenges in implementing a clinical reasoning curriculum (Sudacka et al., Citation2021). The first question in these interviews was “How would you define clinical reasoning (in your profession)?” Participants for the interviews were recruited by project partners following a purposive sampling approach (Creswell, Citation2012) inviting physicians, nurses, medical and nursing students to participate. We purposefully sampled a variety of clinically active healthcare professionals with some or no research experience in clinical reasoning and a work experience of at least 3 years. Additionally, we selected students from different years in their study program ranging from years 2–4 for nursing and 3–6 for medical students. The interviews were held and recorded via telephone or video conferencing in the native language of the participants or in English when the interviewer and participant did not have a common native language. After having conducted the 29 interviews we scanned the responses and decided that saturation had not yet been reached, especially as we did not have sufficient responses from nurses. Therefore, we continued the purposeful sampling by approaching nursing professionals and students. Two of our authors (LH, CG) then conducted 14 additional interviews that covered just this one question. We selected seven interviews to be coded in the end to check for saturation. The responses of the interviewees were transcribed, if necessary translated into English by the interviewer, and collected in a spreadsheet in anonymised form. All interviewers were fluent in English and experienced in teaching about clinical reasoning in English. Additionally, they could consult a native speaker in case of questions.
Data analysis
summarises the steps involved in data collection and analysis. We developed a coding guide for the interviews based on the eight categories of terminology developed in previous studies: players (i.e., stakeholders or actors in a clinical encounter in which CR takes place), purpose/goal of reasoning, outcome of reasoning, reasoning performance, reasoning processes, reasoning skills, context of reasoning, and focus (Young et al., Citation2018, Citation2020). In addition, we developed new categories inductively based on the analysed data. When we came across themes that did not fit into one of the existing categories, we defined and agreed upon additional categories. We formulated two or three guiding questions for each category, which helped us to develop a common understanding and discriminate between the categories (see online supplement 1 for more information).
We developed a coding guide (see online supplement 1) based on the description of these categories and tested and refined it by coding five randomly selected definitions. After that, IH (associate professor of medical education), MS (pediatric resident, medical educator), and LH (medical student) coded all interviews independently and divergent codings were resolved by discussion. Additionally, the final codings were reviewed and discussed with CS and CG (nurses) and finally discussed and agreed upon by the remaining authors.
We analysed the categories by assigning the different terms or text passages of the definitions to one of these categories, and then we grouped the codes in each category into themes. For the category “focus of clinical reasoning” we coded each definition based on the four subcategories suggested by Young et al. (Citation2018):
the individual cognitive processes of the healthcare provider
the interaction between patient and healthcare provider
the interaction between patient and healthcare provider, with allowance for other data sources
very few limits, with anything that “contributed to the final outcome of reasoning”
Ethical approval
This study was conducted as part of a larger study within the Erasmus+ funded knowledge alliance DID-ACT (612454-EPP-1- 2019-1-DE-EPPKA2-KA) and confirmed to be exempted from a detailed ethical review by the Institutional Review Board of the University of Bern, Switzerland (decision: Req-2020–00074). All methods were performed in accordance with the relevant guidelines and regulations of participating institutions. All participants voluntarily participated in this study and provided informed consent.
Results
Overall, we conducted 43 interviews with medical students (n = 9), physicians (n = 13), nursing students (n = 9), and nurses (n = 12) from different countries (). The categories and their themes are described here, in , and illustrated in .
Figure 2. Overview of identified categories with a description and the identified themes as bullet points (if applicable) or a short summary.
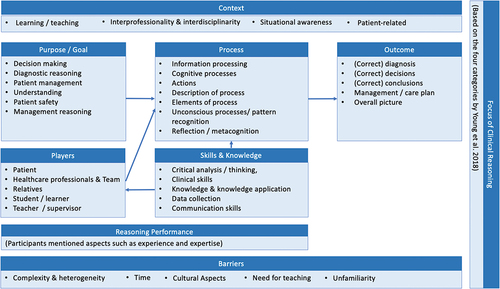
Table 1. Overview of participants.
Table 2. Categories addressed by the different professions.
Categories and themes
In addition to the eight predefined categories, we developed an additional category of “Challenges of clinical reasoning.” provides the frequencies with which participants covered aspects of the categories. Most often participants included an outcome and purpose/goal of clinical reasoning, whereas reasoning performance and challenges were less often covered.
Players
In over 65% of the definitions a patient was mentioned, often in a passive role, such as “the whole process of how to treat a patient” (1, nursing student). In nurses’ definitions, patients were described in a more active role (e.g., “they [nursing students], together with a patient, plan the execution of the best possible nursing intervention.” [28, nurse]). For example, “clinical reasoning is when I am confronted with clinical symptoms” (15, physician). An overview about the players is shown in .
Table 3. Players addressed by the different participant groups.
Purpose/Goal of clinical reasoning
Within this category we identified seven main themes: (a) decision-making, (b) diagnostic reasoning, (c) patient management, (d) understanding, (e) ensuring patient safety, and (f) management reasoning. Physicians, nurses, and students of both professions covered in their definitions the themes of decision making, and diagnostic reasoning, (e.g., “It is the clinical decision making of the physician” [13, physician], “the aim of being able to formulate a nursing diagnosis” [27, nurse]). All groups covered various aspects of patient management, (e.g., “the individual patient you manage” [4, medical student]). Nursing students also highlighted the need for “being there for the patient” (39) and nurses pointed out the need for balancing patient needs and treatments (12), the need to “motivate the patient” (12), and “the setting of objectives, as well as the definition of measures that can serve to accomplish these objectives” (30). Nurses and nursing students emphasised the purpose of clinical reasoning as understanding a situation and a patient’s needs and developing an overall picture, for example “It [clinical reasoning] is about how I think or reason to understand a situation” (34, nursing student) and about making the next person understand (18, nurse). Physicians emphasised the goal of “understanding if our approach is working” (5). Nurses also included the importance of patient safety and survival, (e.g., ”[…] to have the ability for clinical reasoning or not can be directly decisive for whether the patient I care for survives or not” [31] and “It [clinical reasoning] has a certain purpose that you should minimize as many errors as you can” [37]). In addition, physicians and medical students covered aspects of management reasoning, (e.g. “How I come […] to a therapy” [2, medical student] or “finding […] a suitable therapy” [13, physician]).
Outcomes
This category covers the following main themes: (a) (correct) diagnosis, (b) (correct) decisions, (c) (correct) conclusions, (d) management/care plan, and (e) overall picture. As an overarching theme we identified aspects of quality. All four groups covered the outcome of the correct diagnosis, including differential or working diagnoses, in their definitions. For example, medical students said: “It [clinical reasoning] is the kind of thinking that brings you to the right diagnosis” (4) and nurses concluded “Clinical reasoning describes […] the determination of a nursing diagnosis” (29). Also, all groups covered correct decisions as outcome of clinical reasoning in their definitions. Physicians phrased it as “This [clinical reasoning] includes […] decisions about communication, settings, ambulatory treatment or admission to hospital” (7) and nurses mentioned the “decisions made with the patient” (12). Nursing students not only included the decision itself, but also the “rationale behind the clinical decisions I make” (41). The outcome of the management/care plan is addressed by all groups, but in different ways. Although medical students and physicians focused on “the suitable therapy” (13, physician) and “diagnostics” (23, medical student), nurses and nursing students covered aspects such as “nursing plan, (i.e., define goals and measures)” (12, nurse) and nurses mentioned the “joint responsibility to implement interventions/interventions” (36). Similar to the purpose category, nurses and nursing students mentioned the overall picture as an outcome. They said, for example: “the composite picture of the patient’s situation” (35, nurse) or “quick overall picture over the patient and situation” (42, nursing student). The overarching theme of quality was predominantly present in definitions of nurses with phrases such as “best suited evidence-based support” (27), but also “being aware that misdiagnoses are possible” (29). Aspects of quality also emerged in medical students’ definition as “this should be a validated way” (3). All professions covered quality aspects in combination with the other themes, such as “best possible care for the patient” (39, nursing student) or “the correct diagnosis” (21, medical student).
Process
The main themes in this category are the following: (a) information processing, (b) cognitive processes, (c) actions, (d) general description of process, (e) elements of process, (f) unconscious processes/pattern recognition, and (g) reflection/metacognition. Overall, nurses, physicians, and nursing students covered all these themes with their definitions, whereas medical students did not touch upon elements of the process, unconscious processes/pattern recognition, and reflection/metacognition. Concerning information processing, all participants included symptom-related aspects like being “confronted with clinical symptoms” (15, physician) or “look at symptoms and signs” (33, nursing student), but also more generally information use, development, and interpretation (21, medical student). However, nursing students tended toward a more subjective perspective like “subjective observations and values are very important [and is] based on what you experience in the meeting with the person instead of looking at the […] parameters” (32). Cognitive processes include the “opportunity to make cognition visible” (24) mentioned by medical students and that clinical reasoning “is about the mental process” (23). Physicians explained that part of clinical reasoning is “drawing conclusions from the next steps” (26). For nurses and nursing students “to connect the dots” (18, nurse), “how to think in a clinical situation” (38, nurse), “how I think as a nurse or how you think in your profession” (34, nursing student), and perspectives and views were important. Thus, a nursing student mentioned that you have to “see people from a philosophical perspective [… whereas] doctors start from the disease perspective […] and we [nurses] try to see the whole person in a different way” (33, nursing student). Some of the definitions included actions, for instance, physicians explained that “Clinical reasoning is what I do every day” (16) and similarly nursing students commented “it [clinical reasoning] […] describes our daily work with patients” (40). Many definitions contained a general elaboration on the process of clinical reasoning. Medical students considered it a “pathway to get there [to a diagnosis and a therapy]” (2), physicians described it as ‘“ kind of algorithm” (25), and nursing students thought it was important to have a “systematic approach” (41), to “proceed methodically”’ (34), and to “work after the care process” (33). Nurses” definitions showed the broadest variety with a “holistic, individual, and problem-based way” (29), an “unbiased approach” (29), a “problem solving approach” (38) or that the process “runs in loops” (27). Related to the description of the process, we also found specific elements or as a nurse put it “just like baking a cake, you need all of the elements” (18). Such elements from nurses were for example “decision models, among others ethical ones” (30) and “new technologies can be integrated into the process” (30). Nursing students brought up “Checklists for focusing on the gist can be helpful” (41) and physicians emphasised in addition, that “purposefulness is here perhaps crucial” (10). Related to the unconscious nature of the process and pattern recognition physicians covered that “This process [clinical reasoning] is implicit, the association just happens, on the other hand it is explicit, like, I know I have this idea […]” (15). Similarly, nursing students included that “Over time, such processes become more and more unconscious and automated” (41) and nurses emphasised to “trust your own gut feeling” (37). The last theme we identified within this category was reflection and metacognition, which was richly covered by nurses and nursing students saying that “it is important that you discuss why you think the way you do, how you come to the conclusions you make” (36, nurse), “the principle of ‘think aloud’ can help” (41, nursing student), or “by asking the ‘why,’ the process can be actively called into consciousness and thus reviewed by the person thinking” (41, nursing student).
Skills and knowledge
The main themes included in this category are as follows: (a) critical analysis/thinking, (b) clinical skills, (c) knowledge and knowledge application, (d) data collection, and (e) communication skills. Nurses and nursing students covered all these themes, whereas medical students did not cover aspects of data/information collection and communication skills and physicians did not include aspects related to communication and knowledge and knowledge application.
Critical analysis/thinking was covered by nurses for example as “the ability to think or reason” (35) and by medical students and physicians as “analyze the patient’s case” (3, medical student) and “analyzing data” (8, physician). Nursing students and nurses also highlighted the ability of prioritisation (e.g., that it is “important to be able to prioritize and link the different aspects of the case” [41, nursing student]).
In the clinical skills theme history taking plays an important role in both professions, but also the obtaining of “examination results” (13, physician), the performing of “additional examinations” (15, physician), and “markers, such as lab results and ECG” (32, nursing student) were mentioned across professions.
The importance of knowledge and knowledge application was emphasised in various ways mostly by nursing and nursing students. They mentioned that it is important to have “different types of knowledge, partly nursing and medical knowledge” (33, nursing student) and that CR is about “integration of theoretical and practical knowledge” (43, nursing student). They also provided different types of knowledge such as “research knowledge” (40, nursing student), “empirical knowledge” (30, nurse), “scientific knowledge” (31, nurse) and that “the professional needs to be […] able to use this theoretical knowledge in the practical situation” (35, nurse).
General terms, such as collecting (patient-related) data (8, physician; 27, nurse) were covered by physicians and nurses. However, nurses also elaborated that clinical reasoning is “based on a structured information gathering about the patient” (12) and a nursing student explained that ”[experienced nurses] see a patient and they immediately know what to ask and examine” (34).
Finally, we identified the theme of communication skills in this category with slightly different focuses among professions. Nursing students emphasised that interprofessional “communication, especially with physicians and physiotherapists, plays an important role” (39) as well as using “a specific terminology when documenting” (42). Nurses emphasised the ability to communicate with colleagues across professions (e.g., “the ability to clearly state in a short summary, what is happening with [the] patient [and] using professional language that is well understood within clinicians” [18]). Nursing students and nurses focused on the communication with patients saying, for example, that “the personal talk, as well as sensitivity for what the illness means for the particular person, are essential” (41, nursing student) or “using the appropriate means of therapeutic communication […] together with a patient” (28, nurse). Additionally, the aspect of communication with students was brought up by nurses by saying that “especially with students, I think that communication about how to think is extremely important” (36).
Reasoning performance
Only a few definitions included expressions of reasoning performance, such as expertise, experience, and competence, thus we were not able to develop themes in this category. For example, physicians explained that “clinical reasoning […] is a modern term for clinical […] expertise” (9), whereas nursing students thought that clinical reasoning is “largely about experience” (34) and nurses elaborated that “based on their […] competences they […] develop critical thinking” (28).
Context of clinical reasoning
In this category we identified contextual aspects relevant for clinical reasoning in the following themes: (a) learning/teaching clinical reasoning, (b) patient-related, (c) interprofessionality, and interdisciplinarity (i.e., collaboration between different disciplines in medicine such as internal medicine and surgery), and (d) situational awareness. All groups, but especially students included some aspects of clinical reasoning in an educational setting. For example, nursing students explained in his/her definition that “during the training we have mostly practiced our clinical reasoning when we have been out on internships” (33) and medical students explained “this [clinical reasoning] should be a validated way that could be taught to other doctors” (3).
Mainly nurses and nursing students considered patient-related aspects, which include a patient’s situation and needs, but also aspects of shared decision-making and person-centered care. Only one physician considered the “involvement of […] relatives in communication‘ (13) as a contextual factor. However, nurses and nursing students provided a great variety of how and why patients need to be considered. Such as ’[clinical reasoning] should always be adapted to individual patient preferences” (40, nursing student), or “It is important that the patient is informed and understands what will be done and agrees, only then there is a compliance” (12, nurse) or “a special focus should be put on the particular characteristics of each patient” (41, nursing student).
Nurses, nursing students, and physicians elaborated on the theme of interprofessional and interdisciplinary collaboration. Physicians included the “involvement of other professions” (13), nursing students also mentioned that “this [clinical reasoning] is done intra- and interdisciplinary” (40) and by “different health professions” (42). Nurses varied most in their descriptions of this theme, providing phrases such as “as a team, on eye-level” (29) or “an interprofessional approach is desirable” (30). All four groups provided some elaboration of the situation or setting in which clinical reasoning takes place. Apart from general terms like “clinical situation” (e.g., [36, nurse]) some participants provided more specific examples: Physicians mentioned “any setting (e.g., hand-off, ward round, case discussion)” (17), nursing students an “emergency situation” (43), and nurses “prehospital care” (37) or “intensive care units” (36).
Challenges of clinical reasoning
Nurses, nursing students, and physicians covered the topic of challenges of clinical reasoning in their definitions. Thus, we identified five different themes within this category: (a) complexity and heterogeneity of the concept, (b) time, (c) need for teaching, (d) cultural aspects, and (e) unfamiliarity with clinical reasoning.
Nurses and physicians described clinical reasoning as a “very complex [emphasis added]” (7, physician) and “difficult concept to explain” (35, nurse). Nurses added a heterogeneous understanding: “The perspective of nurses on the patient is to a certain extent different from the physicians” (12). Nursing students focused on difficulties for novicesfor example, a student elaborated: “Especially at the beginning of one’s professional career, clinical reasoning is a difficult task because there is only very limited access to experiential knowledge” (40). Another theme covered by nurses was the need for time expressed as “time is needed” (31) or “reasoning may not take up so much space” (37).
A third theme that emerged from the definitions was the need for teaching or education about clinical reasoning. This was especially mentioned by nursing students, for example students wished that “we had practiced clinical reasoning more even during theory sections” (33) and mentioned that clinical reasoning was “not explicitly discussed during my studies” (40). Cultural aspects were mentionedfor example, related to collaboration, nurses stated: “In some wards you do not work in interprofessional teams, and how should you then create a common picture of the situation if you do not reason together […] When something has gone wrong, […] we are talking about the event, but we are not talking about that it may be due to errors in our clinical reasoning.” (36) Finally, participants expressed some degree of unfamiliarity with the concept of clinical reasoning, such as “I cannot think of any definitions of written” (18, nurse) or “I think we do not have much clinical reasoning” (37, nurse).
Focus of clinical reasoning
shows an overview about the focus assigned to the definitions. In most cases the focus is on the interaction between a patient and a health professional with allowance for other data sources (e.g., definition 31 in online supplement 2). However, in some (n = 7, 43.8%) of these definitions (mainly from physicians) the interaction with the patient was only implicit and the focus on “other data sources” like medical literature (e.g., definition 27 in online supplement 2).
Table 4. Focus of clinical reasoning (Young et al., Citation2018) according to the different participant groups.
Discussion
In our study we investigated how practicing physicians, nurses, medical- and nursing students define clinical reasoning. We believe that this adds a valuable perspective to the previous work that focused on how clinical reasoning is defined by experts in clinical reasoning research and in the health professions and health profession education literature (Holder, Citation2018; Young et al., Citation2018, Citation2019, Citation2020).
For the DID-ACT project the discussion of the study results facilitated the development of our own definition of CR, which served as the basis for our curriculum development process. We agreed on defining CR as “Clinical Reasoning encompasses health professionals thinking and acting in assessment, diagnostic, and management processes in clinical situations taking into account the patient‘s specific circumstances and preferences.” During the development of the CR curriculum and the train-the-trainer course in this project, we also incorporated the results of this study into the design of several interprofessional learning units, for example, about the basic principles of CR and the roles of the healthcare professionals in this process. In general, we believe that such differences and similarities of CR conceptualisations should inform curriculum development of CR, and the results also show a clear need for teaching CR in an interprofessional setting.
Overall, the categories we used from the studies of Young et al. (Citation2018, Citation2019, Citation2020) to analyse the definitions worked very well, and we found that the emerging themes from the definitions aligned nicely with these categories. However, we discovered one additional category—barriers for clinical reasoning which includes the complexity of the concept, need for time, aspects of teaching, and cultural aspects. Moreover, we identified additional themes within categories, such as the purpose of understanding or knowledge and knowledge application as a theme related to the skills category. We believe that these additions confirm that clinical reasoning is a multifaceted construct, with different understandings (Young et al., Citation2018), with an even broader understanding among practitioners in our study compared to experts in the field.
Similarities in defining clinical reasoning
Despite the great variety, we discovered some similarities in the definitions of our participants, this includes aspects that have been rarely included by all participants or aspects that have been widely covered. Some aspects of clinical reasoning have hardly been covered across professions. This includes cognitive errors and biases, which was only indirectly covered by patient safety and the lack of communication about errors in clinical reasoning. Consistent with previous work by Chew et al. (Citation2017), this may suggest that there is a lack of awareness concerning such aspects, which should be addressed more explicitly in the healthcare professions and education to reduce errors and ensure equal treatment for all patients. Also, participants rarely mentioned aspects related to performance of clinical reasoning. Young et al. (Citation2020) pointed out that performance aspects are mainly included as part of clinical reasoning assessment. Interestingly, our participants mentioned teaching and learning of clinical reasoning, but not assessment, which might explain the infrequent mentioning of performance aspects.
On the other hand, participants across professions emphasised that clinical skills, such as history taking/asking questions, are part of clinical reasoning. In contrast to that, some experts explicitly regarded clinical skills as not part of clinical reasoning (Young et al., Citation2018).
Differences in defining clinical reasoning
Similar to previous studies (Young et al., Citation2018, Citation2019, Citation2020), we discovered a great variety and differences in the definitions of clinical reasoning. For example, nurses and nursing students provided a more patient-centered view of clinical reasoning in which the patient has a more active role and aspects such as understanding the patient and his/her needs were essential parts of clinical reasoning. Interestingly, clinical reasoning experts in the study by Young et al. (Citation2018) also saw patients in a more passive role as “the source of history, physical examination findings, lab results, and diagnostic cues.”
Definitions by nurses and nursing students tended to be broader with different perspectives, involving different health professionals and emphasising the importance of interprofessional teamwork. This was visible in the Player category, but they also emphasised the importance of interprofessional collaboration as part of clinical reasoning context and the holistic nature of the clinical reasoning process. Similarly, Mohammadi-Shahboulaghi et al. (Citation2021) identified a “holistic cognitive process” when analysing literature from the field of nursing education. In our study, awareness of the heterogeneous conceptualisation of clinical reasoning was present among professionals (nurses and physicians) but not among students. This lack of awareness could have important implications for the teaching and assessment of clinical reasoning, as it emphasises the importance of clearly defining the terminology of clinical reasoning when teaching it to students, so that learners can have a precise idea of the subject matter, and teaching is not overcomplicated by being based on a “terminological Rorschach test” (Young et al., Citation2019).
The process of analysing concepts based on stakeholder viewpoints from different professions has been applied in other fields. A good example is the discussion about the definition of health (Huber et al., Citation2011). We can draw a parallel between the process described by Huber et al. and what we experienced in our study. The involvement of non-expert stakeholders reflects the culture of healthcare practice in the description of the concept. We share Huber et al.’s view that a conceptual framework with several dimensions, like the one we have proposed based on our research, is an important tool to help formulate operational definitions depending on the needs of a particular situation. Such definitions could inform measurement, research, and evaluation in the field (Huber et al., Citation2011). In our case the analysis of the concept helped us to reach a generally agreed direction in which to look and based on that to develop an interprofessional clinical reasoning curriculum.
We believe that our study and especially the adapted coding guide could be used in a study in a larger setting, similarly to how we used and expanded the categories developed by Young et al. Such a study could address the limitations of our study and include a greater variety of health professions, countries, and regions. The study could focus not only on the content of the definitions but also the way how CR is defined by different professions and influenced by the level of experience. It could also ask for definitions of related terms, such as critical thinking, decision-making, or clinical judgment, to identify similarities and differences when using these terms in the literature and by the health professionals. The terms used in CR research in addition to clinical reasoning, such as critical thinking or clinical judgment, could be mapped and differences and similarities visualised when comparing frameworks for these terms and conducting interviews with different stakeholders on how they define these terms.
Limitations
Despite the strengths of our study, which are the international sample of practicing physicians, nurses, and students of both professions and the interprofessional and international team of researchers, we are aware that our study has some limitations. First, we conducted the interviews in the native language of the participants whenever possible, to make sure that participants were not limited by any language barriers. However, despite very careful translations of the definitions into English some misinterpretations or misunderstandings might have happened.
Second, we focused our interviews only on physicians and nurses and students of these professions, not covering other health professions, such as physiotherapists or occupational therapists. Adding interviews with these professions might further broaden the conceptualisation and should be considered in a future study.
Third, although we included healthcare professionals from different countries, they all represent global Northern countries, and we acknowledge that we cannot exclude having divergent findings with healthcare professionals from global Southern countries. We also followed a broad sampling approach in selecting our study participants based on clinical experience/years of study and therefore did not ask any detailed personal question about the participants’ background.
Conclusion
The sharing of different understanding of clinical reasoning across health professions can improve collaboration by giving valuable insights into the understandings of the team members (Young et al., Citation2018). However, for interprofessional collaboration it is also indispensable that each profession retains its own identity or perspective and merging all the different conceptualisations into one concept threatens the ”true power of interprofessional practice” (Loftus, Citation2012). Thus, we see the results of our study as a basis for communication among the different practicing health professions to better understand each other and recognise differences and similarities and based on this improve collaboration and education in clinical reasoning. We encourage all health professionals to start this discussion in their clinical and educational environments.
Supplemental Material
Download Zip (159.2 KB)Acknowledgments
We thank all our study participants for consenting and sharing their perspectives with us. We also owe a big thank you to the whole DID-ACT consortium, who supported this study by preparing and conducting the interviews.
Disclosure statement
The study described in this manuscript is part of the doctoral thesis of LH. No other potential conflict of interest was reported by the authors.
Data availability statement
The definitions and the coding guide are available as online supplements.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/13561820.2023.2208605.
Additional information
Funding
Notes on contributors
Lukas Huesmann
Lukas Huesmann is a doctoral candidate at the Chair of Medical Education Sciences at the University of Augsburg, Germany. Having received his medical degree from Ludwig-Maximilians-University in Munich, his research focuses on clinical reasoning and interprofessional learning.
Małgorzata Sudacka
Małgorzata Sudacka, PhD candidate, MD, during pediatric specialization, is an assistant in Department of Medical Education at Jagiellonian University Medical College in Kraków, Poland. Her main interest is enhancing and rising awareness of clinical reasoning teaching methods.
Steven J. Durning
Steven J Durning, MD, PhD, MACP is professor and vice chair, Department of Medicine and Director Center for Health Professions Education.
Carina Georg
Carina Georg, RN, CCRN, PhD, is a lecturer and researcher at the department of Nursing, Karolinska Institutet , Sweden. Her research interest include medical education, clinical reasoning, technology- enhanced learning, and assessment.
Sören Huwendiek
Sören Huwendiek, MD, PhD, MME, FAMEE, is a pediatrician, pediatric rheumatologist, medical educator and medical education researcher with a great interest in improving healthcare education for the sake of patients. He is associate Professor for Medical Education in Bern and since 2012, he has been the head of the Department for Assessment and Evaluation of the Institute for Medical Education in Switzerland.
Andrzej A. Kononowicz
Andrzej A. Kononowicz, MSc, PhD, is an associate professor at Jagiellonian University Medical College in Kraków, Poland. He graduated in computer science, received a PhD in biomedical engineering and a habilitation degree in health sciences. His research focuses on technology-enhanced learning and clinical reasoning.
Claudia Schlegel
Claudia Schlegel, RN, PhD, is a lecturer and researcher at the Bern College of Higher Education of Nursing, Bern, Switzerland, and The Federal Institute of Technology Zurich (ETH Zurich), Switzerland. Her research interest includes medical education, interprofessional education, and technology- enhanced learning.
Inga Hege
Inga Hege, MD, CompSc is Associate Professor for Medical Education at the University of Augsburg and Ludwig-Maximilains-University in Munich, Germany.
References
- Chew, K. S., Kueh, Y. C., & Abdul Aziz, A. (2017). The development and validation of the clinicians’ awareness towards cognitive errors (CATChES) in clinical decision making questionnaire tool. BMC Medical Education, 17(1), 58. https://doi.org/10.1186/s12909-017-0897-0
- Creswell, J. W. (2012). Educational research: Planning, conducting, and evaluating quantitative and qualitative research (4th ed.). Pearson.
- Higgs, J., Jensen, G., Loftus, S., & Christensen, N. (2019). Clinical reasoning in the health professions (4th ed.). Elsevier.
- Holder, A. G. (2018). Clinical reasoning: A state of the science report. International Journal of Nursing Education Scholarship, 15(1), 20160024. https://doi.org/10.1515/ijnes-2016-0024
- Huber, M., Knottnerus, J. A., Green, L., van der Horst, H., Jadad, A. R., Kromhout, D., Leonard, B., Lorig, K., Loureiro, M. I., van der Meer, J. W. M., Schnabel, P., Smith, R., van Weel, C., & Smid, H. (2011). How should we define health? The BMJ, 343, d4163. https://doi.org/10.1136/bmj.d4163
- Kahlke, R., & Eva, K. (2018). Constructing critical thinking in health professional education. Perspectives on Medical Education, 7(3), 156–165. https://doi.org/10.1007/s40037-018-0415-z
- Kononowicz, A. A., Hege, I., Edelbring, S., Sobocan, M., Huwendiek, S., & Durning, S. J. (2020). The need for longitudinal clinical reasoning teaching and assessment: Results of an international survey. Medical Teacher, 42(4), 457–462. https://doi.org/10.1080/0142159X.2019.1708293
- Koufidis, C., Manninen, K., Nieminen, J., Wohlin, M., & Silén, C. (2021). Unravelling the polyphony in clinical reasoning research in medical education. Journal of Evaluation in Clinical Practice, 27(2), 438–450. https://doi.org/10.1111/jep.13432
- Loftus, S. (2012). Rethinking clinical reasoning: Time for a dialogical turn. Medical Education, 46(12), 1174–1178. https://doi.org/10.1111/j.1365-2923.2012.04353.x
- Mohammadi-Shahboulaghi, F., Khankeh, H., & HosseinZadeh, T. (2021). Clinical reasoning in nursing students: A concept analysis. Nursing Forum, 56(4), 1008–1014. https://doi.org/10.1111/nuf.12628
- Sudacka, M., Adler, M., Durning, S. J., Edelbring, S., Frankowska, A., Hartmann, D., Hege, I., Huwendiek, S., Sobocan, M., Thiessen, N., Wagner, F., & Kononowicz, A. A. (2021). Why is it so difficult to implement a longitudinal clinical reasoning curriculum? A multicenter interview study on the barriers perceived by European health professions educators. BMC Medical Education, 21(1), 575. https://doi.org/10.1186/s12909-021-02960-w
- Victor-Chmil, J. (2013). Critical thinking versus clinical reasoning versus clinical judgment: Differential diagnosis. Nurse Educator, 38(1), 34–36. https://doi.org/10.1097/NNE.0b013e318276dfbe
- Young, M., Thomas, A., Gordon, D., Gruppen, L., Lubarsky, S., Rencic, J., Ballard, T., Holmboe, E., Da Silva, A., Ratcliffe, T., Schuwirth, L., & Durning, S. J. (2019). The terminology of clinical reasoning in health professions education: Implications and considerations. Medical Teacher, 41(11), 1277–1284. https://doi.org/10.1080/0142159X.2019.1635686
- Young, M., Thomas, A., Lubarsky, S., Ballard, T., Gordon, D., Gruppen, L. D., Holmboe, E., Ratcliffe, T., Rencic, J., Schuwirth, L., & Durning, S. J. (2018). Drawing boundaries: The difficulty in defining clinical reasoning. Academic Medicine, 93(7), 990–995. https://doi.org/10.1097/ACM.0000000000002142
- Young, M., Thomas, A., Lubarsky, S., Gordon, D., Gruppen, L. D., Rencic, J., Ballard, T., Holmboe, E., Da Silva, A., Ratcliffe, T., Schuwirth, L., Dory, V., & Durning, S. J. (2020). Mapping clinical reasoning literature across the health professions: A scoping review. BMC Medical Education, 20(1), 107. https://doi.org/10.1186/s12909-020-02012-9