ABSTRACT
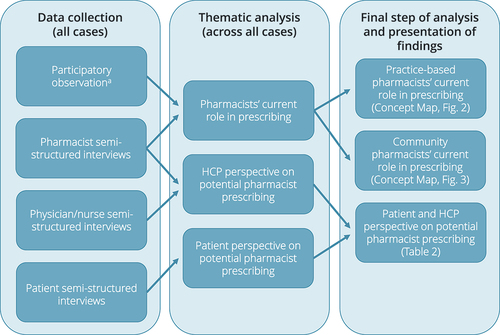
In some countries, pharmacists have obtained prescribing rights to improve quality and accessibility of care and reduce physician workload. This case study explored pharmacists’ current roles in and potential for prescribing in primary care in the Netherlands, where prescribing rights for pharmacists do not exist. Participatory observations of pharmacists working in either general practice or community pharmacy were conducted, as were semi-structured interviews about current and potential practice. The latter were extended to patients and other healthcare professionals, mainly general practitioners, resulting in 34 interviews in total. Thematic analyses revealed that pharmacists, in all cases, wrote prescriptions that were then authorized by a physician before dispensing. General practice-based pharmacists often prescribed medications during patient consultations. Community pharmacists mainly influenced prescribing through (a) medication reviews where the physician and/or practice nurse often were consulted to make treatment decisions, and (b) collaborative agreements with physicians to start or substitute medications in specific situations. These findings imply that the pharmacists’ current roles in prescribing in the Netherlands resemble collaborative prescribing practices in other countries. We also identified several issues that should be addressed before formally introducing pharmacist prescribing, such as definitions of tasks and responsibilities and prescribing-specific training for pharmacists.
Introduction
The global population is aging, and healthcare needs are increasing (United Nations, Citation2022). Older individuals are prone to multimorbidity and complex pharmacotherapy, which puts pressure on prescribers (Wastesson et al., Citation2018). At the same time, healthcare professional shortages are rising (World Health Organization, Citation2016). Ensuring patient safety related to medication and accessibility to appropriate pharmacotherapy are major challenges to national health systems (Donaldson et al., Citation2017; World Health Organization, Citation2016). To address these challenges, prescribing rights have been provided to healthcare professionals other than physicians (Department of Health, Citation2006; Stewart et al., Citation2017). Prescribing by nurses and pharmacists seems at least as effective as prescribing by physicians (Weeks et al., Citation2016), and patient and healthcare professional experiences with prescribing by pharmacists are positive (Jebara et al., Citation2018).
For countries and regions that currently do not have formal roles for pharmacist prescribing, it is important to understand if – and to what extent – pharmacists are already involved in prescribing practice. Previous researchers have identified multiple factors that influence the implementation of pharmacist prescribing (Edwards et al., Citation2022; Jebara et al., Citation2018). Examples of facilitators are an established need for pharmacist prescribing, postgraduate training, and interprofessional collaboration. Barriers often relate to liability, limited pharmacist diagnostic skills, and a lack of infrastructural, organizational, and financial support. These studies were mainly conducted in the United Kingdom (UK), and most of the studies were conducted post-implementation, which limits the transferability of the research findings. It is therefore reasonable to conduct such investigations in any country or setting planning to establish pharmacist prescribing.
Background
Different models and policies of pharmacist prescribing exist across countries (Adams et al., Citation2023; Canadian Pharmacists Association, Citation2023; Jebara et al., Citation2018). One example is independent prescribing, defined as prescribing by a pharmacist responsible and accountable for the assessment of patients with undiagnosed or diagnosed conditions and for decisions about the clinical management required, including prescribing (Department of Health, Citation2006). In the UK, independent pharmacist prescribers can manage any clinical condition and prescribe any medication within their clinical competence. These pharmacists work mainly in interprofessional care settings, such as hospital wards and general practices (General Pharmaceutical Council, Citation2019). In other countries, independent pharmacist prescribing may be restricted by a specific formulary – a list of medications or health conditions (Adams et al., Citation2023; Canadian Pharmacists Association, Citation2023). Another example of a pharmacist prescribing model is collaborative or dependent prescribing, where prescribing is done in the context of a collaborative agreement with a single or group of physicians or by a multidisciplinary team, such as in New Zealand (Pharmacy Council, Citation2021). In Canada and the United States of America (USA), pharmacist prescribing differs between provinces and states, ranging from no prescribing authority at all to independent prescribing authority (Adams et al., Citation2023; Canadian Pharmacists Association, Citation2023).
In most European countries, pharmacist prescribing does not exist. In the Netherlands, nurse practitioners can prescribe medications within their area of expertise and only for less complex and routine care (Bruijn-Geraets et al., Citation2018). In addition, some specialized nurses are authorized to prescribe a limited number of medications within their specialization, following a diagnosis by a physician, and within the context of a local collaborative agreement. Pharmacists cannot obtain prescribing rights. They have however become more actively involved in pharmacotherapy through collaboration with physicians and nurses, and some pharmacists have also started working within general practices with a focus on optimizing individuals patients’ pharmacotherapy (Hazen et al., Citation2021; Verdoorn et al., Citation2019). This is not unique for the Netherlands, as other countries have introduced pharmacists into general practice (Kempen et al., Citation2023). These developments have been supported by an understanding that interprofessional collaboration – in this case among pharmacists, physicians, and nurses – leads to more effective health care and improved patient outcomes (Angibaud et al., Citation2024; Hazen et al., Citation2018; Kwint et al., Citation2013; Wei et al., Citation2022). Advanced pharmacy practices, defined as practices of pharmacists with a relatively high degree of interprofessional collaboration with general practitioners (GPs), probably most closely resemble pharmacist prescribing in primary care. Whether and what model of pharmacist prescribing should be introduced in countries without prescribing rights for pharmacists, and what measures should be taken for its implementation, are key questions to address. It was therefore interesting to investigate what prescribing model would fit current advanced pharmacy practices in the Netherlands. Hence, the aim of this study was to explore the pharmacists’ current roles in prescribing and potential for prescribing in advanced pharmacy practice in primary care in the Netherlands.
Methods
Study design
This study had a multiple case study approach including participatory observation and semi-structured interviews with thematic data analyses across all cases. A case study is an in-depth study of a phenomenon within a specific social system (a case) in its real-life context (Jónasdóttir et al., Citation2018). In a multiple case study, multiple cases are simultaneously or sequentially involved to generate a broader understanding of the particular phenomenon (Crowe et al., Citation2011). In this study, the phenomenon was the pharmacists’ current and potential roles in prescribing in the Netherlands.
Setting and case sampling
The study included six advanced pharmacy practices in primary care in the Netherlands, each practice acting as one case: three general practices with a practice-based pharmacist and three community pharmacies with close collaboration with general practice. Close collaboration was defined as performing clinical medication reviews with shared patient information (e.g., diagnoses and laboratory test results) and having regular pharmacotherapy audit meetings where community pharmacists and GPs structurally discussed pharmacotherapy and made agreements on local prescribing policy (van Mil, Citation2005). The cases were identified through the authors’ professional networks and using a purposive sampling approach to ensure variety in terms of urban environment (Centraal Bureau voor de Statistiek [Statistics Netherlands], Citation2023) and geographic location in the Netherlands. All three community pharmacies were part of a healthcare center that included a general practice. Co-location of community pharmacies and general practices has become more common in the Netherlands in recent decades. The selected community pharmacies previously had participated in a pilot interview study about the pharmacists’ roles in prescribing (Kohli, Citationn.d.). In multiple case studies, two to three cases are suggested when the theory is straightforward and similar results are expected, and five or more if the theory is more subtle (Crowe et al., Citation2011). We expected that six cases would be sufficient for this study.
Population and recruitment
Per case, we aimed to include 1–2 pharmacists, 2–4 patients, and 1–3 physicians or nurses, hence approximately 30–40 participants in total. For each case, one lead pharmacist was approached by telephone and after expressing their initial interest, the pharmacist received the study information by e-mail. The lead pharmacist then coordinated access to the case and recruitment of potential participants in consultation with the researchers. The researchers arranged written informed consent from each person before participation.
Pharmacists were subjected to participatory observation, followed by a semi-structured interview. Semi-structured interviews were also conducted with adult patients who recently had been in contact with one of the pharmacists, and with physicians or nurses who collaborated with these pharmacists. Preferably, these patients, physicians, and nurses had been in contact with the pharmacists during the observations. Patients were excluded if they were not able to provide informed consent (e.g., due to cognitive impairment).
Data collection
A case study manual was used to promote coherence of participant recruitment and data collection across all sites. The manual consisted of detailed instructions related to recruitment, participatory observation, and semi-structured interviewing, including observation forms and interview guides (Online supplement 1). The guidance and its contents were based on the literature (Crowe et al., Citation2011; Jónasdóttir et al., Citation2018), preliminary findings from pilot interviews (Kohli, Citationn.d.), and the research team’s practice experience. Data collection was performed between October and December 2022 by three research assistants (YB, HM, and LV). Each research assistant was responsible for data collection in two cases, supervised by one senior researcher (either TK or AH).
Participatory observations
Participatory observation of pharmacists occurred for at least two observation days per case. The observation days were chosen based on the pharmacists’ availability and an expected high degree of activities related to the pharmacists’ roles in prescribing during these days (e.g., planned patient consultations and/or GP discussions as part of medication reviews). During these days, the researcher observed and made field notes about the pharmacist’s actions and activities related to influencing prescribing in individual patients, using an observation form (Online supplement 1). Informal interviews with the pharmacist and data collection of relevant documents (primarily pharmacotherapy audit meeting agreements and work descriptions) were conducted as part of the participatory observation ().
Semi-structured interviews
Semi-structured interviews were held with patients and healthcare professionals, as soon as possible after the observations (). The interview guide consisted of fixed topics related to current practice and pharmacist-physician/nurse collaboration, future pharmacist prescribing, and conditions to consider for the formal introduction of pharmacist prescribing (Online supplement 1). Patient interviews preferably were held at the patient’s home, although patients were free to choose the interview location. Healthcare professional interviews were held at the practice or pharmacy. All interviews were audio-recorded. For each of the three community pharmacy cases, the pharmacist interview from the previously mentioned pilot study was included. We received the audio recordings after approval by the participant (Kohli, Citationn.d.). These interviews had been conducted April to June 2022 by AK (see Acknowledgements). The interview guide was different, but the topics were similar to those in this study: the pharmacist’s tasks related to prescribing, collaboration with GPs, barriers to this collaboration, and future plans related to prescribing. All audio recordings were transcribed by one of the research assistants using an intelligent verbatim transcription approach (Bucholtz, Citation2000). A second researcher checked the transcription for accuracy. One additional interview with a nurse practitioner was performed and transcribed by TK in May 2023, to complement one of the cases where a physician/nurse interview was lacking.
Data analysis
Qualitative data analyses were performed across all cases using NVivo software (Lumivero, Denver, USA). The pharmacists’ current tasks, processes, and contacts related to prescribing were analyzed, based on participatory observation data and pharmacist interview data (). First, two team members (HM and TK) familiarized themselves with the data and performed initial coding independently, by coding the raw text data from one case in NVivo. Then, an iterative approach of consensus discussions, independent coding of data from all cases, and data interpretation was used to develop the coding framework and themes. Due to differences in the findings between general practice-based pharmacists and community pharmacists, as perceived by the researchers (see Findings, subheading “The pharmacists’ current roles in prescribing”), two separate analyses were conducted. For each analysis, a Concept Map was made in NVivo to visualize the pharmacists’ current tasks, processes, and contacts (categories) in relation to the different stakeholders and systems the pharmacist interacted with (themes). Finally, the Concept Map was translated to English by one of the researchers (TK) and scrutinized by the other researchers.
Patient and healthcare professional perspectives were analyzed based on all interview data (). First, two separate analyses were performed across all six cases: one for patient interviews, and one for pharmacist, physician, and nurse interviews. Two researchers (LV and YB) performed initial coding of interviews from one case independently, to get familiar with the data. No clear differences in these findings between practice-based and community pharmacists were perceived by the researcher, hence the data of all six cases were collectively analyzed. An iterative approach of consensus discussions and data interpretation was also used for these analyses (supervised by TK and AH) to develop the coding framework, categories, and themes. This approach included translating the final themes into English. In addition, for this article, the two analyses (patient and healthcare professional perspectives) were combined in one framework (i.e., sub-themes that emerged from the data were similar for both analyses, although the content of these themes could differ; see Findings, subheading “The patient and healthcare professional perspectives on pharmacist prescribing”).
Researcher characteristics
Data collection and analysis were primarily performed by research assistants: two Master of Pharmacy students (YB and HM) and one Master of Medicine student (LV). Before the study, the students took an online qualitative research course (18 hours in total). The students were supervised by TK and AH, both pharmacists, and LvD, a social scientist. Other senior researchers were MH and HFK, both pharmacists, and DZ, a GP. HFK also acted as the lead pharmacist for one community pharmacy case. Peer scrutiny of the study plan and methodology was undertaken by SKS, a social scientist from Sweden, and DS, a pharmacist from the UK. All supervisors, senior researchers and peer scrutineers were trained and experienced in qualitative research, and they were familiar with the study topic.
Ethical considerations
Ethical approval waiver was provided by the medical research ethics committee of the VU University Medical Center Amsterdam (METc VUmc; reference number 2022.0646). No ethical approval was needed for this study according to the Dutch Medical Research Involving Human Subjects Act (WMO), because neither were the participants being subjected to actions nor were rules of behavior imposed on the participants. Informed consent was obtained from all participants before participation.
Findings
Across all cases, 8 pharmacists were observed during 15 total days (). Semi-structured interviews were held with 34 participants: 14 patients, 10 pharmacists, 8 GPs, 1 geriatrician, and 1 nurse practitioner. The interviews lasted 22 to n60 minutes (mean: 39 minutes). The patients’ ages ranged from 62 to 91 years old, half (n = 7) were female, and 4 had a higher education or university degree (Online supplement 2). The majority of the healthcare professionals had 10 or more years of work experience (n = 15) and were female (n = 13).
Table 1. Case and participant characteristics.
The pharmacists’ current roles in prescribing
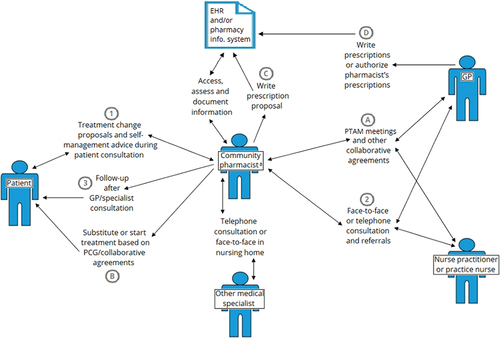
The pharmacists’ current roles in prescribing, based on the observations and pharmacist interviews, appeared through interaction with patients, electronic health information systems, GPs, nurse practitioners or practice nurses, other medical specialists, and (other staff in) community pharmacies (). The pharmacists’ tasks, processes, and contacts in relation to these interacting stakeholders (e.g., patients) and systems differed between practice-based and community pharmacists. Therefore, these findings are depicted and described separately below.
Figure 2. Concept map of the practice-based pharmacists’ current roles in prescribing, with the tasks, processes, and contacts in relation to the different interacting stakeholders and systems. The pharmacists’ most prominent role in prescribing was (1) making treatment changes during patient consultation, and then (2) writing prescriptions in the EHR system (3) for the GP to authorize. EHR, electronic health record; GP, general practitioner; PTAM, pharmacotherapy audit meeting.
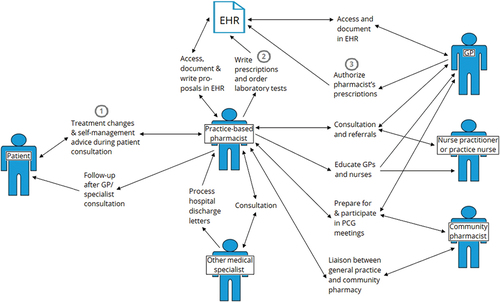
Figure 3. Concept map of the community pharmacists’ current roles in prescribing, with the tasks, processes, and contacts in relation to the different interacting stakeholders and systems. The pharmacists’ main roles in prescribing seemed (1) making treatment change proposals during patient consultation (2) for which the GP often was consulted to make treatment decisions that were then (3) reported back to the patient, and (A) collaborative agreements with GPs that allow (B) pharmacists and patients to decide on starting or substituting medications in specific situations. In those situations, (C) the pharmacist writes a prescription (D) for the GP to authorize. aDelegated to pharmacy assistant in case of less complex or routine situations. EHR, electronic health record; GP, general practitioner; PTAM, pharmacotherapy audit meeting.
Patients
The practice-based pharmacists’ most prominent task and role in prescribing was during patient consultations (). Patients either had a care need, often a drug-related problem, for which they had an appointment with the pharmacist, or the contact was initiated by the GP. The pharmacists were also involved in patient follow-up and monitoring of treatment effects. All three practice-based pharmacists performed less complex clinical examinations (e.g., measuring blood pressure). The pharmacists had a high degree of autonomy, making treatment changes (i.e., drug start, stop, substitution, dosage change or repeat) during patient consultation. The pharmacists treated any health condition in primary care if it was within their area of competence. If the pharmacists were uncertain, they followed up with the patient after consulting the GP or a specialist. All practice-based pharmacists also seemed to develop areas of competence and expertise over time, some for which they had dedicated consultation hours:
My focus used to be on polypharmacy in frail elderly. […] But then it developed … ADHD, hormone replacement therapy, hay fever, starting and stopping antidepressants. So basically, everything that is related to medication is now being referred to me as much as possible.
Community pharmacists also consulted with patients, mainly to solve specific drug-related problems or to conduct medication reviews in older patients (). In these situations, their role in prescribing seemed less direct and autonomous compared to the practice-based pharmacists. Sometimes, the community pharmacist made treatment changes during patient consultations, especially when no prescription was needed (e.g., stopping or tapering treatment). More often, they first contacted the GP or nurse practitioner to make treatment decisions. Thereafter, the GP, nurse or pharmacist followed up with the patient. All community pharmacists provided repeat prescription services. Pharmacists in one case processed daily requests for prescription renewals by patients over telephone. They assessed whether appropriate monitoring had taken place, wrote repeat prescriptions for the GP to authorize and had a fixed moment with one of the GPs each day to discuss cases, if needed: “We then have a conversation [with the patient] and, actually, what we propose to the GP [to re-prescribe], they just trust us on that” (Case 6, pharmacist 2).
In contrast to practice-based pharmacists, community pharmacists had a direct role in prescribing in the context of local agreements with GPs to change dosage, add, or substitute medications (). These agreements were usually made during pharmacotherapy audit meetings and often concerned specific situations, patient groups, or clinical decision rules. Examples were correcting the dosage of a child’s antibiotic prescription, changing to an appropriate inhaler, and substituting an equivalent treatment in case of drug shortages. Less complex or routine prescribing tasks (e.g., adding a laxative to opioid treatment) were often delegated to pharmacy technicians within the community pharmacy. Sometimes, the medication was dispensed to the patient without (waiting for) formal authorization by the GP: “We have working agreements regarding clinical decision rules. Add a proton pump inhibitor, add macrogol, etcetera. We adjust prescriptions and it’s the pharmacist’s judgment whether or not authorization by the doctor is necessary” (Case 4 pharmacist 3).
Electronic health information systems
Each practice-based pharmacist directly worked and wrote prescriptions in the practice’s electronic health record (EHR) system (). Those prescriptions then had to be authorized by the GP before the prescription could be filled in a pharmacy. The pharmacists explicitly wrote notifications if they wanted the GP to look at a prescription before authorization. They also ordered and interpreted laboratory tests in relation to disease management. One participant stated that “What often happens is that the doctor quickly examines the type of medication and then assesses whether this is risk medication. […] If it’s not high-risk medication, the doctor will probably approve it without actually having seen the prescription” (Case 3, pharmacist).
All three community pharmacies had their own pharmacy information system, which they used to process prescriptions, manage clinical decision rules, and write prescriptions (). There was some degree of interoperability between the pharmacy’s and general practice’s systems (e.g., sharing certain laboratory test results and the possibility for GPs to authorize pharmacists’ prescriptions). In one case, pharmacists could access the general practice’s EHR system, if needed.
GPs and other primary care professionals
In all cases, pharmacists and GPs/nurses referred patients to each other, and – in addition to electronic communication – they had face-to-face discussions about patients in the context of medication reviews or in case of specific questions (): “I explicitly consult the GP in situations in which I have doubts myself or if I notice that the patient has doubts, because that trust in the GP is more established and my role in this is still new” (Case 1, pharmacist).
Most pharmacists had weekly or (bi-)monthly scheduled meetings with GPs. In two cases, the practice-based pharmacist mentioned providing pharmacotherapy education to GPs and other practice staff (). The practice-based pharmacists functioned as a liaison between their general practice and the community pharmacy. All pharmacists prepared for and participated in pharmacotherapy audit meetings, which were important for community pharmacists to make prescribing agreements ().
Other medical specialists
Sometimes, the pharmacists consulted other medical specialists to get advice or clarification about a patient’s treatment or to propose specific treatment changes for the specialist to decide upon ():
It happens often that I send a teleconsultation to a specialist: “I have this and this in mind.” Then it is nice that they say: “I would do the same.” That you get that confirmation. […] And the next time, you’ll do it yourself.
One community pharmacist collaborated on a regular basis with a geriatrician to conduct medication reviews in nursing home patients (). They had face-to-face discussions about potential changes to the patients’ pharmacotherapy. We observed that the specialist was in charge of making the final decision about what to change. On the other hand, this pharmacist worked more independently in case of drug shortages: “I always text message the otorhinolaryngologists: ‘Hi, I changed it [the prescription] to [a brand name],’ ‘Oh, fine,’ they answer. Or we report it systematically, which is often done by e-mail throughout the region and then it’s all right” (Case 5, pharmacist).
The patient and healthcare professional perspectives on pharmacist prescribing
Two main themes were identified during the analyses of the patient and healthcare professional perspectives: (a) perspectives on potential pharmacist prescribing, and 2) conditions for its introduction in future practice ().
Table 2. Themes, sub-themes, and categories related to the patient and healthcare professional perspectives on pharmacist prescribing.
Theme 1: Perspectives on potential pharmacist prescribing.
Scope of practice
Different views existed among participants regarding the extent of autonomy that pharmacists should have when obtaining prescribing rights, ranging from “only in consultation with the GP” (Case 3, patient 1) to pharmacists “having all rights to change medication or to prescribe” (Case 5, patient 2). However, there seemed to be a collective understanding among participants that it is the physician’s job to diagnose. Many participants suggested that pharmacists could have a prescribing role in patients with chronic conditions, after the diagnosis was made by the physician, and make changes to already prescribed treatments. Many participants also thought that, in view of current practice, pharmacists should be able to prescribe within the limits of protocol-based care or based on local agreements with GPs. In one case, the GPs had recently agreed that, if there are any drug shortages, “the pharmacists can make a decision themselves” (Case 4, nurse) about what to substitute and that it is up to the pharmacists to judge when they need to consult the GP: “Anything that is via a protocol, you [as a pharmacist] can just do that. Then you know how it works. If it falls outside of that, it’s good to discuss it” (Case 3, GP 1).
A more limited or restricted form of prescribing could also mean having the right to prescribe medication for minor ailments or uncomplicated health conditions, as mentioned by several participants. It was unclear what these conditions exactly were, but headaches, hay fever, and high blood pressure were mentioned by some patients. Some pharmacists felt they would be able to prescribe antibiotics for uncomplicated urinary tract infections, whereas one GP mentioned this as an example “that’s really not going to happen” (Case 1, GP 1). Other possible forms of prescribing would be the right to repeat chronic prescriptions “which they actually already do right now” (Case 4, patient 1), or to deprescribe medications that are no longer of benefit.
Possible settings and level of organisation
For most patients, it did not really seem to matter where the pharmacist was located, as long as they worked “in collaboration with a physician” (Case 6, patient 2). GPs who spoke about possible settings seemed more hesitant about community pharmacy than general practice. Most of the participants seemed to believe that the scope of practice and/or division of tasks should be organized locally: “I think it becomes complicated if you want to organize it at national level. So, my idea is that if it happens locally as much as possible, then it will spread at some point” (Case 2, pharmacist).
Potential benefits
Reduction in physician workload was often mentioned as potential benefit of pharmacist prescribing. GPs who had been working closely with a practice-based pharmacist noted that they were already noticing this benefit. Other potential benefits that were mentioned by several participants, were improvements in accessibility, efficiency, and pharmacists’ job satisfaction: “And it’s also frustrating when the deadline has passed and you come back for more meds, and they tell you ‘Nope, you got to go see the GP first.’ Such a waste of time” (Case 5, patient 2).
Potential risks
One potential risk, often expressed by patients and GPs, was fragmentation of health care or loss of control by the GP. Patients emphasized the importance of having a designated point of contact in primary care, and were concerned that adding a pharmacist with prescribing rights might result in confusion regarding liability: “But who is then responsible for the bigger picture?” (Case 5, GP).
According to both patients and healthcare professionals, another possible risk is medication errors, which may impact the quality of care. This risk may be related to the fragmentation of health care or the pharmacists’ lack of clinical competence, as pharmacists might misdiagnose or fail to act upon potential red flags. A third concern was the potential conflict of interest that arises when pharmacists have financial benefit of prescribing and retailing medications.
Theme 2: Conditions for the introduction of pharmacist prescribing in future practice.
Defining tasks and responsibilities, and support for and knowledge of (new) pharmacist role
Participants believed that clear tasks and responsibilities were important to avoid confusion and get support for pharmacist prescribing. Pharmacists indicated a need to create awareness about their role in patient care and clearly explain how and why they should have a prescribing role so that patients, GPs, and other stakeholders can support it. This support would be needed at local and national level: “I can imagine the national general practitioners’ association or the pharmacists’ association […] A lobby should be started for that. With health insurers as well.“(Case 2, GP 2).
Collaboration and trust
Collaboration between pharmacists and physicians and trust by physicians and patients in pharmacists were deemed essential to support pharmacist prescribing. The general view of participants was that trust is built over time by working together: “GPs and pharmacists need to know each other, work together and trust each other.” (Case 1, pharmacist).
Pharmacist workforce capacity and workload
Another important practical prerequisite raised was that pharmacists need to have enough capacity to increase their role in prescribing. There might not be enough pharmacists or enough time for pharmacists to take on a prescribing role: “It’s just like an air mattress: if the pressure drops at the GP, it goes up at the pharmacy. And can they handle it?” (Case 2, patient 1).
Pharmacists’ competencies
Pharmacists indicated a need to be competent to prescribe. Skills related to diagnosing, consulting, and clinical reasoning and decision-making were often explicitly mentioned. Some participants also mentioned that a certain professional attitude was important (i.e., dare to deal with uncertainties, know your limitations, and take responsibility):
What happened the other day, that I was trying to taper medication with a patient and if it goes wrong, you don’t think: “GP, now this patient is yours again.” […] That is also exciting and scary at times, but you have to learn that.
Patients and other healthcare professionals generally believed that they knew little about the pharmacists’ current education, but that it was important to know about the pharmacists’ capabilities. All pharmacists mentioned that some kind of post-graduate training was needed to become competent to prescribe, with some participants stressing the importance of practice-based learning.
Interoperability of systems and shared patient information
Working in the same system or having a high degree of interoperability between the health information systems was another important prerequisite discussed. Patients and GPs stressed the importance of informing the GP if a pharmacist would prescribe medication. Diagnoses, health measurements, and laboratory results were often mentioned by pharmacists as essential information to have: “Why should I go to the pharmacist, if I know that he/she does not have the relevant information?” (Case 5, patient 2).
Legislation, regulations and reimbursement, and solution for potential conflict of interest
Change in law, working agreements, and financial compensation were other conditions noted for the implementation of prescribing rights for pharmacists. Finally, pharmacists and physicians mentioned that the potential conflict of interest (prescribing and retailing medication) should be addressed, although several participants thought that it might not be such a significant problem: “Every barrel has a rotten apple. […] There are also GPs who commit fraud. […] So, I don’t think that in itself is such a big problem. You simply assume that everyone has their professional ethics in place” (Case 5, GP).
Discussion
This study was the first to employ a case study approach to explore pharmacists’ current roles in and potential for prescribing in advanced pharmacy practice in a country without formal prescribing rights for pharmacists. We observed that general practice-based pharmacists in the Netherlands often prescribed medication during patient consultations with a high degree of autonomy. Community pharmacists with close collaboration with GPs mainly influenced prescribing through medication reviews where the physician or nurse practitioner often was consulted to make treatment decisions. These pharmacists had a more direct role in prescribing through collaborative agreements with physicians to start or substitute medications or to repeat prescriptions for chronic use in certain patients. Based on patient and healthcare professional interviews, there seems potential for pharmacist prescribing in some restricted or collaborative form and several conditions for its formal introduction were mentioned.
The pharmacists’ current roles in prescribing in this study seem to resemble collaborative prescribing practices in other countries (Adams et al., Citation2023; Pharmacy Council, Citation2021). In New Zealand, pharmacists who are part of a multidisciplinary healthcare team can initiate or modify pharmacotherapy and may order and interpret laboratory tests after the diagnosis has been made by the GP, similar to the activities by general practice-based pharmacists in this study. Local pharmacotherapy audit meeting agreements currently made between Dutch community pharmacists and GPs seem similar to population-based collaborative practice agreements that are common in the USA. Patients and other participants also mentioned potential prescribing roles for pharmacists related to minor ailments or uncomplicated health conditions, repeat prescriptions, and deprescribing medications. In a recently published qualitative study from the Netherlands, citizens who were informed about opportunities for pharmacy prescribing sketched an ideal future scenario involving a multi-professional primary care center where pharmacists could prescribe medication for minor ailments and for certain chronic diseases after diagnosis by a GP (Kempen et al., Citation2024). Several examples of these roles also exist in countries with pharmacist prescribing (Canadian Pharmacists Association, Citation2023; Jebara et al., Citation2018).
Potential benefits and risks identified in this study (e.g., decreased physician workload but increased medication errors) have been mentioned before as well (Edwards et al., Citation2022; Jebara et al., Citation2018), although one of the main concerns regarding fragmentation of health care or loss of control by the GP seems more apparent in our study. Perhaps, this concern is more legitimate in the Netherlands, where the GP plays a relatively strong role in ensuring continuity of care and as gatekeeper for specialist and hospital care compared to other countries (Faber et al., Citation2012). Interoperability of health information systems may be important to address this concern.
Several concerns, such as those related to liability and pharmacists’ diagnostic skills, are often voiced pre-implementation, but seem less common in post-implementation studies (Jebara et al., Citation2018). Perhaps this is due to the collaboration with physicians that often exists when pharmacists prescribe. Trust and understanding builds through interprofessional collaboration and may alleviate preexisting concerns in local practice. Pharmacist prescribing may also strengthen this collaboration as it may create more interdependence between GPs and pharmacists and increases the need to clarify goals, tasks, and responsibilities at local level (Reeves et al., Citation2010). Many patients in this study, as well as in the citizen perspective study (Kempen et al., Citation2024), explicitly stated that they would trust pharmacists in a prescribing role as long they collaborated with physicians. Most participants in this study also believed that the implementation of pharmacist prescribing should be organized locally, which supports the idea of a collaborative or dependent prescribing model. The consequence of such a model is that pharmacists are dependent on physicians to collaborate and negotiate about tasks and responsibilities, which may be time-intense and arbitrary (Adams et al., Citation2023). In the UK, independent prescribers tend to work in interprofessional collaborative care settings where their scope of practice seems agreed upon at local hospital or general practice level as well (General Pharmaceutical Council, Citation2019; Petty, Citation2019). According to the sociologist Abbott (Citation1988), jurisdictional claims by professions about their scope of practice are often first made and settled in the local workplace domain, followed by the public and legal domains. Getting formal prescribing rights would however require a change in national law. In the case of nurse practitioners in the Netherlands, legalizing informal local prescribing practice by a national law amendment resulted in more efficient care processes and encouraged other nurse practitioners to develop their role (Bruijn-Geraets et al., Citation2018).
Other important prerequisites that were identified in this study (e.g., the presence of post-graduate training for pharmacists) have frequently been mentioned in studies on both pharmacist and nurse prescribing (Edwards et al., Citation2022; Jebara et al., Citation2018). What this post-graduate training would need to consist of what we mean by diagnostic or clinical skills and to what extent pharmacists should acquire these, requires more exploration.
If the introduction of pharmacist prescribing is considered, policymakers could use the pharmacists’ current roles in prescribing, identified in this study, as a basis for legislation. These findings may also be applicable to other countries where pharmacists have started working in close collaboration with or within general practices (Kempen et al., Citation2023). The support for pharmacist prescribing among larger stakeholder groups and the exact model of prescribing need further investigation, but an interprofessional collaborative context seems warranted. Our findings also imply that a structured and targeted approach addressing the conditions identified in this study may facilitate its implementation.
Limitations
Although research trustworthiness was addressed in diverse ways throughout the study, some limitations need to be considered. First, study cases were identified through the researchers’ professional networks, and participants within each case were recruited by one lead pharmacist. This may have led to bias in the selection of participants, which may decrease the transferability of our research findings. However, we deliberately looked for advanced pharmacy practices as examples of the potential roles of pharmacists in primary care that do not necessarily reflect usual care in the Netherlands. To what extent these findings apply to pharmacists in primary care in the Netherlands, also in less advanced pharmacy practices, remains to be studied. Second, observations were only performed in 2–4 days per case, and notes and interview transcripts were not checked with the participants. Hence, we may have missed certain aspects related to the pharmacists’ roles in prescribing. Third, 7 out of 11 researchers had a pharmacy background, which may have colored their interpretation of the study findings. We have therefore paid close attention to the interpretation of and critical review by those with a background in medicine and social science.
Conclusion
Pharmacists in advanced pharmacy practice in Dutch primary care have multiple ways of influencing prescribing in individual patients, resembling collaborative prescribing practices that exist in other countries. The pharmacists’ current roles in prescribing could therefore provide a basis for pharmacist prescribing legislation. Several conditions should be addressed if and before such legislation is introduced, including definitions of tasks and responsibilities, prescribing-specific training for pharmacists, and shared patient information.
Online supplement 2_Participant_characteristics.docx
Download MS Word (16.1 KB)Online supplement 1_Observation_form_and_interview_guides.docx
Download MS Word (31.3 KB)Acknowledgments
The authors would like to thank all participants for their contribution to this research. We would also like to thank Hennie Boeije for her advice on case study methodology, Aradhana Kohli for sharing the pilot study interview transcripts, and Maren Schilling for the figure design support.
Disclosure statement
LvD received funding from Biogen and TEVA Pharmaceuticals for studies not related to this study. No other potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/13561820.2024.2374017
Additional information
Funding
Notes on contributors
Thomas G. H. Kempen
Thomas Kempen is assistant professor at the Utrecht Institute for Pharmaceutical Sciences, Utrecht University, the Netherlands.
Yosra Benaissa
Yosra Benaissa has obtained her MSc of Pharmacy degree at Leiden University Medical Center, the Netherlands.
Haijo Molema
Haijo Molema has obtained his MSc of Pharmacy degree at University of Groningen, the Netherlands.
Lea E. Valk
Lea Valk has obtained her Medical degree at University Medical Center Utrecht, the Netherlands.
Ankie C. M. Hazen
Ankie Hazen is assistant professor at Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, the Netherlands.
Mette Heringa
Mette Heringa is manager research at SIR Institute for Pharmacy Practice and Policy in Leiden, the Netherlands.
Henk-Frans Kwint
Henk-Frans Kwint is manager care and innovation at SIR Institute for Pharmacy Practice and Policy in Leiden, the Netherlands.
Dorien L. M. Zwart
Dorien Zwart is professor at Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, the Netherlands.
Sofia Kälvemark Sporrong
Sofia Kälvemark Sporrong is professor at the Department of Pharmacy, Uppsala University, Sweden.
Derek Stewart
Derek Stewart is professor at the College of Pharmacy, QU Health, Qatar University, Qatar.
Liset van Dijk
Liset van Dijk is programme leader at Nivel, Netherlands Institute for Health Services Research in Utrecht and professor at Groningen Research Institute of Pharmacy, University of Groningen, the Netherlands.
References
- Abbott, A. (1988). The system of professions: An essay on the division of expert labor. University of Chicago Press.
- Adams, A. J., Weaver, K. K., & Adams, J. A. (2023). Revisiting the continuum of pharmacist prescriptive authority. Journal of the American Pharmacists Association, 63(5), 1508–1514. https://doi.org/10.1016/j.japh.2023.06.025
- Angibaud, M., Jourdain, M., Girard, S., Rouxel, L., Mouhib, A., Nogueira, A., Rat, C., & Huon, J. F. (2024). Involving community pharmacists in interprofessional collaboration in primary care: A systematic review. BMC Primary Care, 25(103). https://doi.org/10.1186/s12875-024-02326-3
- Bruijn-Geraets, D. P., van Eijk-Hustings, Y. J. L., van Bessems-Beks, M. C. M., Essers, B. A. B., Dirksen, C. D., & Vrijhoef, H. J. M. (2018). National mixed methods evaluation of the effects of removing legal barriers to full practice authority of Dutch nurse practitioners and physician assistants. British Medical Journal Open, 8(6), e019962. https://doi.org/10.1136/bmjopen-2017-019962
- Bucholtz, M. (2000). The politics of transcription. Journal of Pragmatics, 32(10), 1439–1465. https://doi.org/10.1016/S0378-2166(99)00094-6
- Canadian Pharmacists Association. (2023, June 1). Scope of practice. https://www.pharmacists.ca/advocacy/scope-of-practice/
- Centraal Bureau voor de Statistiek [Statistics Netherlands]. (2023, June 30). Kerncijfers wijken en buurten 2022 [Key figus districts and neighborhoods 2022]. CBS. https://www.cbs.nl/nl-nl/maatwerk/2023/14/kerncijfers-wijken-en-buurten-2022
- Crowe, S., Cresswell, K., Robertson, A., Huby, G., Avery, A., & Sheikh, A. (2011). The case study approach. BMC Medical Research Methodology, 11(1), 100. https://doi.org/10.1186/1471-2288-11-100
- Department of Health. (2006). Improving patients’ access to medicines: A guide to implementing nurse and pharmacist independent prescribing within the NHS in England. UK Department of Health, Social Services and Public Safety.
- Donaldson, L. J., Kelley, E. T., Dhingra-Kumar, N., Kieny, M.-P., & Sheikh, A. (2017). Medication without harm: WHO’s third global patient safety challenge. The Lancet, 389(10080), 1680–1681. https://doi.org/10.1016/S0140-6736(17)31047-4
- Edwards, J., Coward, M., & Carey, N. (2022). Barriers and facilitators to implementation of non-medical independent prescribing in primary care in the UK: A qualitative systematic review. British Medical Journal Open, 12(6), e052227. https://doi.org/10.1136/bmjopen-2021-052227
- Faber, M. J., Burgers, J. S., & Westert, G. P. (2012). A sustainable primary care system: Lessons from the Netherlands. The Journal of Ambulatory Care Management, 35(3), 174–181. https://doi.org/10.1097/JAC.0b013e31823e83a4
- General Pharmaceutical Council. (2019). GPhC survey of registered pharmacy professionals 2019. Author. https://www.pharmacyregulation.org/about-us/research/gphc-survey-registered-pharmacy-professionals-2019
- Hazen, A., de Bont, A. A., Boelman, L., Zwart, D. L. M., de Gier, J. J., de Wit, N. J., & Bouvy, M. L. (2018). The degree of integration of non-dispensing pharmacists in primary care practice and the impact on health outcomes: A systematic review. Research in Social and Administrative Pharmacy, 14(3), 228–240. https://doi.org/10.1016/j.sapharm.2017.04.014
- Hazen, A., Sloeserwij, V., Pouls, B., Leendertse, A., de Gier, H., Bouvy, M., de Wit, N., & Zwart, D. (2021). Clinical pharmacists in Dutch general practice: An integrated care model to provide optimal pharmaceutical care. International Journal of Clinical Pharmacy, 43(5), 1155–1162. https://doi.org/10.1007/s11096-021-01304-4
- Jebara, T., Cunningham, S., MacLure, K., Awaisu, A., Pallivalapila, A., & Stewart, D. (2018). Stakeholders’ views and experiences of pharmacist prescribing: A systematic review. British Journal of Clinical Pharmacology, 84(9), 1883–1905. https://doi.org/10.1111/bcp.13624
- Jónasdóttir, S. K., Hand, C., Misener, L., & Polgar, J. (2018). Applying case study methodology to occupational science research. Journal of Occupational Science, 25(3), 393–407. https://doi.org/10.1080/14427591.2018.1480409
- Kempen, T. G. H., Koumi, R., & Sporrong, S. K. (2023). Pharmacists in general practice: What do they do? A qualitative case study. International Journal of Clinical Pharmacy, 45(6), 1472–1482. https://doi.org/10.1007/s11096-023-01619-4
- Kempen, T. G. H., van Dijk, L., Floor-Schreudering, A., Kohli, A., Kwint, H.-F., Schackmann, L., van Tuyl, L. H. D., & Heringa, M. (2024). Potential for pharmacist prescribing in primary care: A Dutch citizen perspective. Exploratory Research in Clinical and Social Pharmacy, 14, 100453. https://doi.org/10.1016/j.rcsop.2024.100453
- Kohli, A. (n.d.). Rapportage huidige rol van de apotheker bij het voorschrijven [Report about the current role of the pharmacist in prescribing]. Unpublished.
- Kwint, H.-F., Bermingham, L., Faber, A., Gussekloo, J., & Bouvy, M. L. (2013). The relationship between the extent of collaboration of general practitioners and pharmacists and the implementation of recommendations arising from medication review. Drugs & Aging, 30(2), 91–102. https://doi.org/10.1007/s40266-012-0048-6
- Petty, D. (2019). Clinical pharmacist roles in primary care networks. Prescriber, 30(11), 22–26. https://doi.org/10.1002/psb.1802
- Pharmacy Council. (2021). Pharmacist Prescribers. https://pharmacycouncil.org.nz/pharmacist/pharmacist-prescribers/
- Reeves, S., Espin, S., Lewin, S., & Zwarenstein, M. (2010). Interprofessional teamwork for health and social care (1st ed.). John Wiley & Sons, Inc.
- Stewart, D., Jebara, T., Cunningham, S., Awaisu, A., Pallivalapila, A., & MacLure, K. (2017). Future perspectives on nonmedical prescribing. Therapeutic Advances in Drug Safety, 8(6), 183–197. https://doi.org/10.1177/2042098617693546
- United Nations. (2022). World population prospects 2022: Summary of results. https://population.un.org/wpp/Publications/
- van Mil, F. (2005). Pharmaceutical care in community pharmacy: Practice and research in the Netherlands. Annals of Pharmacotherapy, 39(10), 1720–1725. https://doi.org/10.1345/aph.1G141
- Verdoorn, S., Kwint, H.-F., Blom, J. W., Gussekloo, J., Bouvy, M. L., & Kesselheim, A. S. (2019). Effects of a clinical medication review focused on personal goals, quality of life, and health problems in older persons with polypharmacy: A randomised controlled trial (DREAMeR-study). PLOS Medicine, 16(5), e1002798. https://doi.org/10.1371/journal.pmed.1002798
- Wastesson, J. W., Morin, L., Tan, E. C. K., & Johnell, K. (2018). An update on the clinical consequences of polypharmacy in older adults: A narrative review. Expert Opinion on Drug Safety, 17(12), 1185–1196. https://doi.org/10.1080/14740338.2018.1546841
- Weeks, G., George, J., Maclure, K., & Stewart, D. (2016). Non‐medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database of Systematic Reviews, 2017(10), 11. https://doi.org/10.1002/14651858.CD011227.pub2
- Wei, H., Horns, P., Sears, S. F., Huang, K., Smith, C. M., & Wei, T. L. (2022). A systematic meta-review of systematic reviews about interprofessional collaboration: Facilitators, barriers, and outcomes. Journal of Interprofessional Care, 36(5), 735–749. https://doi.org/10.1080/13561820.2021.1973975
- World Health Organization. (2016). Global strategy on human resources for health: Workforce 2030. Health Workforce Team. https://www.who.int/publications/i/item/9789241511131