ABSTRACT
Increasing chronic disease rates in regional Australian communities necessitates innovative models of healthcare. We evaluated the efficacy of an interprofessional chronic disease program, delivered within a regional student-led nursing and allied health clinic in Southern Queensland, Australia. Changes to anthropometric, aerobic fitness and strength, and quality of life outcomes were examined at four time points spanning 16 months: intake, program transition (4 months), 6 and 12 months (post-transition). Our primary aim was to investigate whether the health improvements achieved during the program were sustained at 12 months in a subset of participants who provided complete data. Significant improvements were found in 6 of 11 measures, including the 6-minute walk test, grip strength, and self-reported quality of life across physical and psychosocial dimensions, with these improvements maintained to final review. No significant changes were found in body mass index (BMI), waist circumference, fat mass, or muscle mass. This is the first health clinic in regional Australia to deliver a student-led model of interprofessional and collaborative service to tackle the increasing burden of chronic disease in the community. The cost-effectiveness of this service and other potential clinical and social benefits remain to be investigated.
Introduction
Chronic diseases are persistent conditions that affect individual health and quality of life. According to the World Health Organization (World Health Organization, Citation2023), chronic diseases kill 41 million people each year, which is equivalent to 74% of all deaths worldwide. Chronic disease burden remains a global public health challenge (Murray, Citation2022); its prevalence in Australia is equally pronounced (Australian Institute of Health and Welfare, Citation2023b). The AIHW commonly reports on a group of chronic diseases, including asthma, cancer(s), cardiovascular and respiratory diseases, kidney disease, mental disorders, and osteoporosis (AIHW, Citation2023b). These conditions have been linked to lifestyle rather than hereditary factors alone (Lavie et al., Citation2019). By 2030, the economic loss due to lost productive life years from chronic diseases in Australians aged 45–64 years is projected at $20.5 billion in missing income, $7.3 billion in increased welfare payments, and $4.7 billion in lost taxes (Schofield et al., Citation2016). Prevention strategies targeting modifiable risk factors for chronic disease can therefore be more cost-effective compared to treatments administered following disease onset.
As in other parts of the globe, the effects of chronic diseases are heightened in regional, rural, and remote Australian communities (Australian Institute of Health and Welfare, Citation2022), hereafter referred to as ‘regional’. These regions are characterized by vast geographical distances, socioeconomic inequalities, limited infrastructure, and workforce shortages, which together restrict access to healthcare services (Australian Institute of Health and Welfare, Citation2022; Colman, Citation2022). The seven million Australians in regional areas, or 28% of the total population, are also more likely to engage in unhealthy behaviors such as tobacco smoking, alcohol consumption, drug use, poor dietary habits, and physical inactivity compared to their metropolitan counterparts (Australian Institute of Health and Welfare, Citation2023a). Such behaviors contribute to poorer health outcomes and a shorter life expectancy. Indeed, major cities experience 174.8 disability adjusted life years (DALY) per 1000 population, whereas remote areas have 248.6 DALY (National Rural Health Alliance, Citation2021). Compared to major cities, potentially preventable hospitalizations rise by 11% in inner, 22% in outer regional, 70% in remote, and 154% in very remote areas (National Rural Health Alliance, Citation2021). The limited access to healthcare services in regional areas calls for innovative person-centered models of care. These models should, alongside therapeutic intervention, emphasize chronic disease prevention and education, enabling individuals to proactively manage their health and disease states (Smith et al., Citation2022).
As a key component of healthcare reform, interprofessional collaborative practice (IPCP) is a potentially effective model of practice that improves staff, individual, and organizational outcomes across various settings (Körner et al., Citation2016; Wei et al., Citation2022). Recognition of the significance of IPCP has grown since the publication of the World Health Organization (Citation2010) landmark framework for action. Operationally, IPCP occurs when multiple healthcare workers from different professional backgrounds work together with end-users, families, caregivers, and communities to deliver high-quality healthcare to those in need (Lutfiyya et al., Citation2019). This approach includes support for individuals managing a chronic disease or comorbidity (Körner et al., Citation2016; Pascucci et al., Citation2021).
The full potential of IPCP is only realized when it is underpinned by robust interprofessional education (IPE), where two or more professions learn from, with and about each other to improve collaboration and quality of care (World Health Organization, Citation2010). This type of education is designed to prepare current and future healthcare workers for IPCP (Martin et al., Citation2021). Healthcare teams that embrace IPE principles are well-equipped to maximize collaborative skills, share information, identify client needs, resolve conflict, and ultimately deliver care tailored to the preferences of each individual (Sangaleti et al., Citation2017). Activities to deliver IPE include clinical simulation, in-person and online problem-based learning, and work-integrated learning experiences (Jones et al., Citation2015; Olson & Bialocerkowski, Citation2014). The delivery of IPE to health students on university clinical placement via service-learning models has the potential to contribute to the enhancement of knowledge, skills, and competencies (Pullon et al., Citation2016), while providing solutions to real community health needs (Forbes et al., Citation2021; Hopkins et al., Citation2022). Student-focussed IPE placement opportunities also open pathways to workforce recruitment, which remains a problem in regional Australia (Martin et al., Citation2023).
Student-led interprofessional clinics, where students work with preceptors, clients, and students from other health professions, are an effective service-learning model to deliver IPE (Hopkins et al., Citation2022). These clinics extend education beyond a single-discipline placement (Lai et al., Citation2015) and prepare (typically final year) students for IPCP. A number of reviews (Hopkins et al., Citation2022; Kent & Keating, Citation2015) and studies (Farlow et al., Citation2015; Haggarty & Dalcin, Citation2014; Lawrence et al., Citation2015) have reported on the experiential nature of clinics operating under this service model, referred to as interprofessional education and collaborative practice (IPECP; Martin et al., Citation2021), including in an Australian context (Forbes et al., Citation2021; Gustafsson et al., Citation2016; Kent et al., Citation2016; Lai et al., Citation2015). The extent to which IPECP is integrated in student-led clinics varies across studies and settings in terms of team structure, clinical involvement, and length of exposure (Hopkins et al., Citation2022).
Given the unique challenges faced by regional communities in Australia, including an elevated burden of chronic disease and workforce shortages, adopting models of IPCP is considered priority. The efficacy of this healthcare service model is, however, predicated on the delivery and uptake of comprehensive IPE. Student-led clinics represent prime settings to blend IPCP and IPE to form an effective model of IPECP. The purpose of this study, therefore, is to evaluate the efficacy of an interprofessional chronic disease program delivered within a regional student-led nursing and allied health clinic in Southern Queensland, Australia. The primary aim is to investigate whether improvements to participant health outcomes are maintained following program transition at the 6- and 12-month review points.
Background
The Health and Wellness Clinic
The Health and Wellness clinic (hereby referred to as “HaWC”) is located in Toowoomba and serves the Darling Downs Region (Southern Queensland, Australia). This region, covering a geographical area of 95,500 km2 (5.5% of the state), ranks first in Australia for the highest rate of physical inactivity; 70% of adults are overweight or obese (Darling Downs and West Moreton Primary Health Network [PHN], Citation2018). Given this, HaWC targets community-dwelling individuals at low-to-rising risk of chronic disease, as well as those diagnosed with a chronic condition. The establishment and operational costs of the clinic are funded through the Rural Health Multidisciplinary Training (RHMT) program, an initiative of the Australian Government Department of Health and Aged Care (Citation2023).
Clinic purpose
HaWC focusses on preventing chronic disease to alleviate pressure on local health services. Services are co-delivered by dieticians, exercise physiologists, physiotherapists, psychologists, registered nurses, and social workers. Given the focus on IPECP, the clinic provides nursing and allied health students with a unique placement experience in a regional setting. University students are exposed to various interprofessional opportunities, including observing other professions, participating in case conferences, and delivering services in collaboration with others from different professions. The six competency domains from the Canadian Interprofessional Health Collaborative (Canadian Interprofessional Competency Framework, Citation2010) framework are core to program delivery.
Target population
The HaWC program targets adults (≥16 years of age) at risk of chronic disease or those with acquired disease. However, priority is given to individuals who are yet to be diagnosed. A typical participant in the program would be inactive, overweight, and have poor eating habits. Comorbidities are common, including mild, longer-term physical, psychological, or biopsychosocial conditions that contribute to an unhealthy lifestyle. Prospective participants are referred by a General Practitioner (GP) and triaged for eligibility and their capacity to engage in all program components.
Methods
Design and ethical approval
This was a cohort study with repeated measures. Ethical approval was granted by the University of Queensland covering prospective (exemption: 2022/HE000076) and retrospective (waiver 2022/HE000928) data usage.
Study scope
The HaWC program monitors changes in physiological, psychological, and behavioral factors at four time points comprising intake, program transition (4 months), 6 and 12 months (post-transition). An initial study introduced the clinic described service components and student placement outcomes, as well as lessons learned from the first 3 years of operation to inform quality improvement (Walker et al., Citation2024). The same study also found significant improvements across various health measures. However, the scope of the analysis was limited to changes between intake and transition without extended follow-up, which would be necessary for a comprehensive understanding of longer-term program effects (Walker et al., Citation2024). This study builds on those initial findings and focusses on anthropometric, aerobic fitness, strength, and quality of life outcomes in a subset of participants who provided complete data up to 12 months after program transition.
Eligibility
An initial triage interview session was conducted by a clinical educator and health student to assess participant eligibility for the program. The collected information included demographics, anthropometrics, chronic disease history and risk, health behaviors (e.g., physical activity, diet, drinking, and smoking habits), blood pressure, medication information, and individual availability to attend HaWC services.
To be included in the HaWC program, participants were required to have two or more of the following modifiable risk factors: (a) hypertension ≥140/90 mmHg; (b) Body Mass Index (BMI) ≥25 kg/m2; (c) high cholesterol (GP referral and/or positive for currently medicated); (d) high blood glucose levels (GP referred); (e) physical activity less than the Physical Activity Guidelines set out by the Australian Department of Health (i.e., being active on most days [mild activities], or ≥2.5 to 5 hours of moderate physical activity per week, or 1.25 to 2.5 hours of vigorous physical exercise, and muscle strengthening sessions for 2 days per week); and (f) eating less than two servings of fruit and five servings of vegetables per day.
Triage priority assessment
Eligible participants were categorized into one of the three triage priority groups at an initial IPECP case conference. Triage group one, the priority group, included participants who had not been diagnosed with a chronic disease and were yet to take prescribed medication. Triage group two comprised participants who met two inclusion criteria and had been using medication(s) for less than 2 years to manage a diagnosed chronic condition. Participants in triage group three presented with two or more inclusion criteria; however, they had been diagnosed with more than one chronic disease and have been taking medication(s) for 2 or more years.
The Health and Wellness Clinic program structure
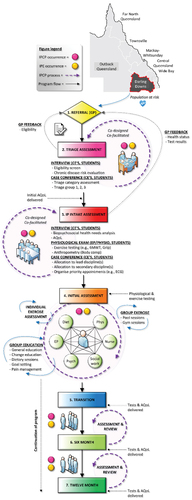
The IPECP program is visualized in . Key phases include referral and triage, intake assessment, transition, and the 6- and 12-month review points. Student placement length varied according to discipline requirements during the 16-week structured component of the program (i.e., intake to transition). The average placement duration was 7.2 weeks. Placement frequency, cumulative weeks, and average duration per discipline are outlined elsewhere (Walker et al., Citation2024).
Figure 1. The HaWC IPECP program. Positions in the program are offered to a total of 25 people per block (50 per year) who progress as a group from intake through to 12-month post-transition follow-up. Participant groups are aligned with academic semesters and therefore student availability to lead the program content.
Intake assessment
Participants who completed the triage and eligibility checks, and who were offered a place on the HaWC program, attended an interprofessional intake assessment session. The assessment involved a biopsychosocial health needs analysis, physiological exams, and a case conference. The case conferences served as an opportunity for students to develop their IPCP capabilities through discussion of a given participant’s presenting issues and concerns with clinical educators. These meetings were used to identify initial actions for each professional discipline and priority appointments (e.g., electrocardiogram).
Intake to program transition
During the 16-week period between intake and transition, participants attended a combination of individual and group-based exercise and education sessions, as well as individual consultations according to their health priorities. Participants were expected to attend the clinic three times per week to fully engage with all components of the program. Education content, led by students with support from clinical educators, included topics on behavior change (i.e., preparing for change, goal setting, dealing with setbacks, maintaining a healthy mind), health management (i.e., movement, nutrition, pain management, improved sleep), and cooking demonstrations.
As participants neared program transition, they were enrolled into a “Moving Forward” session to identify the methods by which they would maintain health behaviors in a community setting. Each participant received a pre-exercise assessment by the exercise physiology and physiotherapy teams and an individualized exercise plan was formulated. This included individual and group-based gymnasium, pool, and outdoor exercise sessions across the duration of the program. Exercise programs were tailored to individual needs based on pathophysiology, goals, exercise history, physical limitations, capabilities, and exercise preferences.
Individual consultation type and frequency was determined collaboratively with the participant throughout the program and was recorded in a personal “Wellness Plan” developed at intake. The wellness plan and physiological assessment documents served as records of participants’ progress, documenting changes in health behaviors and outcomes. At 5 weeks into the program, initial interprofessional goals were determined and strategies discussed. These goals were adjusted based on participant feedback received during a progress review around 4 weeks later, after which the program continued for another 5 weeks. Students contributed to the wellness plan and had access to a data progress measures document to better understand the progress made by each participant.
Transition to 12-month follow-up
A “Transition Summary” was sent to the referring GP outlining individual achievements throughout the program. During the periods between transition and 6 months, and 6 and 12 months post-transition, participants were encouraged to independently implement the newly acquired knowledge and skills within a community setting. At 6- and 12-month follow-up, participants were invited to return to HaWC for follow-up assessments. Assessment of Quality of Life (AQoL) was reassessed and goals from their previous assessment were reviewed, adjusted or maintained, and ongoing strategies discussed. A final assessment was completed including review of all aspects of the program and a “Program Summary” report sent to the referring GP. The IPECP program therefore spanned 16 months total.
Outcome measures and procedures
Anthropometrics
The TANITA Body Composition Analyzer DC-430 MA calculated BMI using bodyweight and height data. Bioelectrical impedance analyzed body composition, including percent body fat, fat mass, and muscle mass. The TANITA scales were connected to a laptop running GMON – Health Monitor software. Waist circumference, a key anthropometric measure in chronic disease risk (Australian Institute of Health and Welfare, Citation2023c), was measured according to the World Health Organization (Citation2008) protocol for waist measurement.
Aerobic fitness and strength
The 6-minute walk test (6MWT) and grip strength test measured exercise performance and strength, respectively. As a measure of functional exercise capacity, the 6MWT (Enright, Citation2003) has demonstrated excellent test–retest reliability (intra-class correlation coefficient = 0.96; 95% CI: 0.91 to 0.98; p < .001; Eden et al., Citation2018). In this context, continuous pulse oximetry (heart rate and blood oxygen saturation), pre/post-blood pressure, and rating of perceived exertion were recorded during the 6MWT. Each test was completed on a flat 15-m-long section of track within an air-conditioned gymnasium.
Hand grip strength has been shown to correlate with lower extremity muscular strength, including quadriceps strength and other biomarkers for health (Bohannon et al., Citation2012). Grip strength was measured using the Jamar Plus Digital Hand Dynamometer, which supports a maximum grip force of 90 kg (200 lb). Participants used the dynamometer while seated upright, with arms by their sides and elbows flexed at 90 degrees. Both right and left hands were assessed, and results recorded. The reported result is the average of three attempts per hand.
Assessment of quality of life (AQoL)
Quality of life was measured using the AQoL-8D instrument, a reliable and valid multi-attribute utility tool (Richardson, Iezzi, et al., Citation2014; Richardson, Sinha, et al., Citation2014). The AQoL-8D includes 35 items that form eight dimensions: (a) Independent Living; (b) Happiness; (c) Mental Health; (d) Coping; (e) Relationships; (f) Self-Worth; (g) Pain; and (h) Senses. Responses to each item range from a 4-point to a 6-point scale. Collectively, the eight dimensions are further combined to form two “super-dimensions,” AQoL physical and AQoL psychosocial, measured using standardized scores between 0 and 100 with a lower score indicating inferior health states.
In this study, a weighted utility score was computed by combining information from both super-dimensions to provide an overall preference-adjusted index of health status, measured using the scale 0.00 (worst-death) to 1.00 (best-health). The Qualtrics platform was used to gather AQoL data and utility calculations followed that prescribed (Centre for Health Economics, Citation2023).
Data extraction
Participant data were collected using clinic management software (Practice Master Professional) and extracted for July 2019 to December 2022, inclusive. In the second half of 2019, participant enrollment into the program occurred continuously. From mid-2020 onwards, potentially eligible participants were invited to HaWC in block entry format. Anthropometric, aerobic fitness and strength, and quality of life data were manually extracted from clinical records and stored in CSV format to allow for statistical processing.
Data analysis
Demographics and descriptive statistics were tabulated. Independent samples t tests were used to examine potential baseline differences between completers and non-completers. Completers were defined as those participants who returned to the clinic for review at all four time points and provided complete data versus those that either started and did not reach transition or reached transition but did not return for the required follow-up reviews.
Group mean differences were analyzed using one-way repeated measures analysis of variance (ANOVA) tests, with the outcome measure as the continuous dependent variable and time as the categorical independent variable. Sphericity was not assumed, and so the Greenhouse–Geisser test was selected to correct for unequal variances of the differences in scores. Effect size estimates (partial eta squared; ηp2), included in omnibus tests, were defined as small (.01), medium (.06) and large (.14; Cohen, Citation1988). The Shapiro–Wilk test and histograms were evaluated to confirm that data were approximately normally distributed. An alpha value of p < .05 two-tailed was considered significant for analyses. The probability of making a type I error in post-hoc comparisons of group mean differences (95% CI) was adjusted using Bonferroni-corrections. Statistical analyses and graph creation were undertaken using IBM SPSS Statistics (v. 28.0) and GraphPad Prism (v. 9.5.1).
Results
Baseline differences
Demographic data are presented in , including a comparison between completers and non-completers at program intake. Participants who returned at 6 and 12 months were, on average, significantly older than non-completers. Notably, all participants in the ≤40-year age group did not complete, and only two participants from the 40- to 49-year age group went through to completion. AQoL-adjusted utility scores were significantly higher at baseline for completers compared to non-completers, as were psychosocial scores.
Table 1. Participants demographics and comparison of variables between completers and non-completers at baseline/intake (N = 135).
Triage categorisation
As shown in , a majority of participants were assigned to the second triage group, fulfilling two of the inclusion criteria. These participants had been on medication for less than 2 years and had a diagnosed chronic condition. Approximately one-third of participants had comorbidities and were categorized in triage group three. Fewer participants fell into the priority population group.
Table 2. Frequency and proportion of completers within each triage category.
Changes to outcome measures
As summarized in , results revealed statistically significant improvements in 6 out of the 11 variables assessed, including 6MWT, grip strength in both the dominant and non-dominant hands, AQoL adjusted utility, AQoL physical, and AQoL psychosocial.
Table 3. Results of the repeated measures analysis of variance (ANOVA) tests for each dependent variable.
Anthropometrics
Weight, BMI, waist circumference, fat mass, and muscle mass did not change significantly (p > .05) from intake to 12-month follow-up (, Panel a-e).
Aerobic fitness and strength
As shown in , the results of the 6MWT significantly improved over time. Multiple comparisons showed improvements in distance walked from intake to transition (MD = −63.8 m, 95% CI: −102.9 to −24.7, p < .001), intake to 6 months (MD = −65.2 m, 95% CI: −111.1 to −19.4, p < .01), and intake to 12 months (MD = −56.8 m, 95% CI: −100.9 to −12.6, p < .01; , Panel a). No statistically significant differences were found between transition, 6 and 12 months (p > .05).
Figure 3. Changes in aerobic fitness, grip strength, and quality of life measures at intake, program transition (16 weeks), 6 and 12 months (post-transition). Panel a, six-minute walk test (6MWT) (m); panel b, grip strength dominant hand (kg); panel c, grip strength non-dominant hand (kg); panel d, preference-adjusted assessment of quality of life (AQoL); panel e, AQoL physical; panel f, AQoL psychosocial. * denotes threshold of statistical significance, * = p < .05; ** = p < .01; *** = p < .001.
Grip strength of the dominant hand significantly improved over time. Multiple comparisons revealed improvements from intake to transition (MD = −3.5 kg, 95% CI: −6.2 to −0.8, p < .01; , Panel b). Likewise, grip strength of the non-dominant hand significantly improved (F(1.49, 25.3) = 4.12, p = .039, ηp2 = 0.195), notably from intake to transition (MD = −3.4 kg, 95% CI: −5.8 to −0.9, p < .01; , Panel c). No statistically significant differences were found between the remaining time points for either dominant or non-dominant hand grip strength (p > .05).
Quality of life
Significant improvements were observed in AQoL preference-adjusted utility scores (). Multiple comparisons showed significant improvements from intake to all other time points (transition: MD = −0.12, 95% CI: −0.19 to −0.06, p < .001; 6 months: MD = −0.10, 95% CI: −0.17 to −0.03, p < .01; 12 months: MD = −0.08, 95% CI: −0.16 to −0.01; p = .021; , Panel D). No statistically significant differences were found between transition, 6 and 12 months (p > .05).
Participants’ AQoL physical scores significantly improved over time. Multiple comparisons revealed improvements from intake to all other time points (transition: MD = −8.4, 95% CI: −13.2 to −3.6, p < .001; 6 months: MD −6.7, 95% CI: −11.4 to −1.9, p < .01; 12 months: MD = −6.1, 95% CI: −11.3 to −0.9, p = .013; , Panel E). No statistically significant differences were found between transition, 6 and 12 months (p > .05).
Based on our findings, participants’ AQoL psychosocial scores also significantly improved. Comparisons revealed improvements from intake to transition (MD = −6.0, 95% CI: −10.0 to −1.9, p < .01) and intake to 6 months (MD = −4.4, 95% CI: −8.5 to −0.3, p = .029; , Panel F). No statistically significant differences were found between transition, 6 and 12 months (p > .05).
The HaWC program appeared to confer a benefit on physical performance measures and self-reported quality of life, with (a) the most significant changes consistently observed between intake and transition and (b) those improvements were maintained to final review, which occurred long after participants had transitioned out of the program and into a community setting.
Discussion
We evaluated the efficacy of an interprofessional chronic disease prevention and management program, delivered within a regional student-led nursing and allied health clinic in Southern Queensland, Australia. This study builds on initial work describing the development of the HaWC program, including evidence of positive changes in health outcomes at program transition, and several key lessons learned over the first 3 years of operation (Walker et al., Citation2024). It also adds to the growing body of literature describing student-led health clinics (Farlow et al., Citation2015; Forbes et al., Citation2021; Gustafsson et al., Citation2016; Haggarty & Dalcin, Citation2014; Hopkins et al., Citation2022; Lai et al., Citation2015; Lawrence et al., Citation2015; Martin et al., Citation2021).
Baseline characteristics and differences
Differences between participant groups were found prior to program start. First, participants who returned to the clinic at follow-up were, on average, older than non-completers. This pattern was most evident in the youngest age group (≤40 yrs), which had the highest attrition rate. Older adults may be better able to adhere to program demands due to increased leisure time and reduced work commitments or retirement. Second, the AQoL adjusted utility and AQoL psychosocial scores were significantly higher for completers at baseline. Given that higher scores on these tests are indicative of better mental health, wellbeing, and social support, it could be that individual motivation and resilience is enhanced, thus improving program adherence. These and other potential differences should be further explored to better understand program engagement, drawing attention to participants who may require further support at intake.
A key aim of this study was to investigate whether potential changes to health outcomes were sustained at the 6- and 12-month review points. Indeed, the overarching purpose of HaWC is to educate and empower individuals, providing them with the knowledge, skills, and attitudes required to independently sustain health promoting behaviors in a community setting.
Aerobic fitness
The findings highlight the potential benefits of the HaWC program in enhancing cardiorespiratory fitness, physical strength, and self-reported quality of life. Notably, the 6MWT, a widely administered field test for evaluating functional exercise capacity (Eden et al., Citation2018; Enright, Citation2003), and known for its inverse association with chronic disease progression and mortality (Pinto-Plata et al., Citation2004), revealed a substantial improvement. The longer average distance recorded at transition was maintained to final review, indicating that the program led to a sustained improvement in aerobic fitness. Importantly, the increased distance observed exceeded both expected learning effects (Singh et al., Citation2014) and thresholds of clinical significance reported (Bohannon & Crouch, Citation2017), suggesting that the HaWC program meaningfully enhanced participants’ functional exercise performance.
Researchers have established reference 6MWT values in healthy adult cohorts and those with illness, serving as a performance benchmark. A sample of 335 healthy Canadians aged ≥40 years of age achieved an average 6MWT distance of 541 ± 98 m (Delbressine et al., Citation2023). In a study of 51 elderly participants (50 to 85 yrs) without disease, the average distance was 631 ± 93 m (Troosters et al., Citation1999). A large-scale multinational study (40 to 80 yrs) reported 571 ± 90 m (Casanova et al., Citation2011). By comparison, the participants in this study commenced the program with a much lower 6MWT distance (382 ± 95.6 m), comparable to individuals with pulmonary arterial hypertension (PAH), at 329 to 378 m (McGoon et al., Citation2013), albeit higher than in individuals with moderate-to-severe chronic obstructive pulmonary disease, at <300 m (Pinto-Plata et al., Citation2004).
Accordingly, although the HaWC program demonstrated benefits in exercise capacity, with the 6MWT distance increasing to 439.3 m at 12 months, there remains a considerable gap when compared to both healthy and elderly population benchmarks. This suggests that further gains in performance may be possible with appropriate exercise prescription, albeit tailored to individual capabilities, established guidelines, and clinical needs and risks. Continual monitoring and programming are advised.
Grip strength
Grip strength significantly increased from intake to transition and exhibited little change from transition to program completion, indicating sustained strength gains. Statistical effect sizes were large, with 21.4% and 19.5% of the variability in grip strength for the dominant and non-dominant hand explained by program progression, respectively. This result is encouraging as weaker handgrip strength is linked to various chronic physical conditions (Leong et al., Citation2015), even when accounting for socioeconomic, lifestyle-related, and dietary factors (Celis-Morales et al., Citation2018).
In drawing on the scientific literature, our grip strength findings fall within the intermediate (male 26 to 31.9 kg; female 16 to 19.9 kg) to normal (male ≥32.0 kg; female ≥20.0 kg) categories based on the National Institutes of Health Sarcopenia Project (Alley et al., Citation2014), and others (de Souza Vasconcelos et al., Citation2016). Thus, HaWC participants did not, on average, exhibit weakness as it relates to reduced mobility, especially when assessed at program transition. The strength improvements from intake to transition, and onwards to 12-month review, also bode well when compared to heavy hand task performance findings (Wang & Chen, Citation2010), and the range of values reported for younger, healthier cohorts (Bohannon et al., Citation2012). Given these outcomes, the IPECP program appears to have produced a genuine improvement in grip strength, a clinically validated marker of health, as well as morbidity and mortality risk (Vancampfort et al., Citation2019).
Quality of life
Findings suggest that the HaWC program conferred a significant benefit on quality-of-life outcomes, assessed using the AQoL-8D instrument (Richardson, Iezzi, et al., Citation2014; Richardson, Sinha, et al., Citation2014). Overall AQoL scores demonstrated an increase from 0.57 ± 0.18 at intake to 0.69 ± 0.20 at program transition, which despite declining by 0.04 by 12 months, remained significantly higher than the intake value. The magnitude of effect for these differences was large (ηp2 = 0.202). A similar pattern was observed for the physical and psychosocial super-dimensions, where the average AQoL score increased by 8.4 and 6.0 from intake to transition, respectively, and remained stable though to program completion. Given that the AQoL-8D evaluates quality of life in several interrelated physical and mental health areas, these findings are encouraging from the perspective of preventing and living with chronic disease in older age.
The AQoL-8D norming project, which analyzed data from 2,731 Australians (46.6 ± 16.1 yrs), determined that for the age group 55-to-64 years, the AQoL physical score was 0.77 ± 0.22, and the AQoL psychosocial score was 0.51 ± 0.25 (Maxwell et al., Citation2016). Other investigations have used the AQoL-8D to evaluate changes in progressive disease. For example, in 157 individuals with idiopathic pulmonary fibrosis, the average AQoL utility score was 0.69 ± 0.20 (Cox et al., Citation2023), and in 917 persons with depression, the average score was 0.45 ± 0.19 (95% CI: 0.44 to 0.46; Engel et al., Citation2018). In four large longitudinal studies, the mean AQoL utility change score was identified at 0.06 (95% CI: 0.03 to 0.08; Hawthorne & Osborne, Citation2005). While caution should be taken when interpreting this MID, given the different calculation methods and sample characteristics, a 0.12 increase in the overall AQoL score in this study from intake to transition points to a meaningful change. AQoL scores were maintained to final review suggesting a lasting intervention effect.
Anthropometrics
Weight, BMI, waist circumference, fat mass, and muscle mass did not change significantly over the course of the program. Participants, categorized as obese class II at intake (BMI ≥35 kg/m2), had an average waist circumference indicating a high risk of obesity-related diseases (Australian Institute of Health and Welfare, Citation2023c). At transition, modest reductions were recorded, with body weight falling by 2.3 kg, BMI by 0.9 kg/m2, and waist circumference by 4.8 cm. The large (ηp2 = 0.106) change for waist circumference approached the p value cutoff of 0.05, suggesting a potentially positive trend achievable in a larger or longer-term study. Fat and muscle mass, essential markers of metabolic functioning and overall health, also remained somewhat stable from intake to 12 months.
Although our study fell short of a ≥ 5% clinically protective weight loss target (Horn et al., Citation2022), recommended to be achieved following a 1-year treatment period (Jensen et al., Citation2014), it is noted that the HaWC program primarily aims to promote overall biopsychosocial health and wellness. Therefore, the body weight, BMI, and waist circumference results are encouraging given the shorter intervention period and the older age group of the majority of our participants who face physiological changes making weight loss more challenging (Coker & Wolfe, Citation2018). Maintaining weight is essential for older adults to preserve muscle mass, strength, and overall health, which was consistent with health goals among a number of our participants. Close monitoring of changes in these measures will continue henceforth, and modifications may need to occur based on the above findings.
The role of IPECP on health outcomes and insights from the clinic
Through this work, we have contributed to the IPCP literature generally (Körner et al., Citation2016; Wei et al., Citation2022), and specifically to work that has focused on student-led clinics as an IPE service-learning model (Hopkins et al., Citation2022; Kent & Keating, Citation2015), including in an Australian context (Forbes et al., Citation2021; Gustafsson et al., Citation2016; Kent et al., Citation2016; Lai et al., Citation2015). Although individuals with chronic conditions report positive experiences with IPCP (Lawrence et al., Citation2015), research directly linking IPCP to health outcomes and patient-centered care continues to emerge (Lutfiyya et al., Citation2019; Reeves et al., Citation2017). There is a need for longitudinal studies to quantify the connection between IPECP and individual health outcomes (Kent & Keating, Citation2015), and how together IPE and IPCP may support chronic disease prevention and management (Pascucci et al., Citation2021). We have, therefore, contributed important knowledge to that gap, albeit in a specific setting and regional location, and given several logistical and operational challenges outlined elsewhere (Walker et al., Citation2024).
Embedding IPE in a clinical context may enhance the learning experiences of students on university placements, equipping them for effective IPCP. Despite this, there is considerable heterogeneity in terms of how IPE is delivered and implemented in student-led clinics (Hopkins et al., Citation2022). Understanding the specific setting, the diversity of student and health professions, the type of interprofessional activities on offer, placement length, and IPE deliverables is essential for discerning how these components contribute to various outcomes. In the case of the HaWC program, students actively engage as members of an interprofessional healthcare team and consistently participate in both individualized and collective formal education, including behavior change, health management, and food preparation sessions. The comprehensive program schedule delivers content across a diverse range of both IPCP and general health topics, with other students joining remotely online from outlaying rural areas to broaden the educational experience. This bespoke model of IPECP service delivery thus tackles both the increasing chronic disease rates facing regional Australia (Australian Institute of Health and Welfare, Citation2022), including in this specific community (Darling Downs and West Moreton PHN, Citation2018), as well as the workforce shortages experienced (Colman, Citation2022). As the literature indicates that positive student placement experiences are linked to student intentions of returning to the location post-qualification (Martin et al., Citation2022), service-leaning models such as the one described in this study may influence workforce recruitment into the future for Southern Queensland, and other surrounding regions.
Similar to other regional placements that provide increased scope of practice opportunities (Jones et al., Citation2015; Martin et al., Citation2021; Pullon et al., Citation2016), HaWC offers fewer concurrent student placements, allowing each student to make a meaningful contribution to program content and participant progress. Preliminary feedback within the clinic indicates high levels of student satisfaction, pointing to an area of further exploration. Additionally, HaWC incorporates innovative activities such as “escape room” style interprofessional health-related scenarios, adding the benefits of gamification to student learning. Student placements, although varying across disciplines, have been viewed as an extended offering (where possible) to again lengthen the time spent in community and increase the opportunities for students to experience all that regional communities offer. It is these authors’ opinion that the HaWC program and its multifaceted IPECP approach have contributed to particular health improvements – and in line with a primary aim – their maintenance over the longer-term in a community setting.
In summary, the efficacy of an interprofessional chronic disease prevention program, such as that offered at HaWC, is dependent on how education is integrated into practice according to the context, needs, and resources available. In addition, our findings raise questions around possible reasons explaining a lack of participant progress for certain health measures, including the challenges that need to be overcome to achieve optimal outcomes. This includes revaluation of contact time and/or touch-points with clinical educators and students, as the length of time between review points following program transition may need to be reduced, or their frequency increased. Doing so could enhance individual motivation and engagement to support more effective progress. As further work is conducted around the role of IPECP in student-led clinics, and its association with various outcomes, the HaWC program will serve as a valuable piece of evidence within the growing body of IPECP literature.
Limitations and research considerations
The study had limitations and research considerations. The average rate of attrition was 64.5% (range: 53.5 to 75.0%) between intake and 12 months post-transition across the health variables analyzed. By virtue of design, systematic differences between completers and non-completers may exist beyond those discussed. While missing or incomplete data did not fall below 50.0% for those who completed the study, grip strength had limited data points, and so comparisons were made for both males and females combined.
In terms of analyses, statistical power may have been affected by varying sample sizes across variables. In the anthropometric measures, smaller effect sizes and non-significant results were observed despite larger numbers. Conversely, for aerobic fitness and strength, where the effect sizes were relatively large, yet sample sizes were reduced, the results were reasonably robust. Future studies with great numbers are advised. In our case, the global COVID-19 pandemic significantly affected the in-person service delivery forcing us to transition to a telehealth format for services, a process described elsewhere (Walker et al., Citation2022). Despite this, a study strength is the inclusion of follow-up data associated with individuals facing serious health conditions.
In relation to program deliverables, the HaWC intervention is multifaceted and bespoke to individual needs. This approach makes standardizing the intervention particularly challenging for research purposes. As a corollary, it is impractical to objectively measure the student-resourced components and quantify their direct effect on changes in participant health outcomes, particularly within the context described in this study. A controlled experimental environment may negate the capacity to tailor individual programs, such that it would no longer be evaluating an intervention of the type reported here.
Conclusion
We investigated the efficacy of an interprofessional chronic disease prevention program, delivered within a regional student-led nursing and allied health clinic, on individuals either diagnosed with or at risk of developing chronic disease. It is concluded that the HaWC program significantly enhanced aerobic fitness and strength and overall preference-adjusted quality of life. Importantly, the findings suggest that improvements to these health measures were maintained at the 6- and 12-month review post-transition time points. Program adaptations may need to occur to extend the duration, structure, and/or intensity to move closer to accepted clinically protective anthropometric thresholds for high-risk individuals while ensuring compliance and satisfaction for all enrolled.
Acknowledgments
The authors would like to acknowledge staff at Southern Queensland Rural Health (SQRH) and the passionate interprofessional team of clinical educators and students at the Health and Wellness Clinic (HaWC) who have worked tirelessly since 2019 to deliver high-quality healthcare services. Credit is given to Amelia Pearce and Kirsten Waller, Administration Assistants at HaWC, for their ongoing support with clinic coordination, participant management, and logistics. We would also like to show our respect to, and sincerely thank, each and every participant for their efforts to improve their health, having returned multiple times for review and progress checks. We will continue to do our best as a clinic and team and hope to continue to positively impact the lives of people in our regional community.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Adam Hulme
Adam Hulme, BSc Hons (ExSc), MA (Health Promot), PhD (Systems Epidemiol), is an Australian Research Council (ARC) DECRA Fellow at Southern Queensland Rural Health (SQRH). He is Research Chair (SQRH), Deputy Chair of the Australian Rural Health Education Network (ARHEN) Research Staff Network, and serves as an Associate Editor for the Australian Journal of Rural Health (AJRH), a publication of the National Rural Health Alliance (NRHA).
Bahram Sangelaji
Bahram Sangelaji, BSc (PT), MSc (Rehab Manag), PhD (PT), is a Senior Research Assistant at Southern Queensland Rural Health (SQRH). He is an Adjunct Research Fellow at the Centre for Health Research, University of Southern Queensland.
Clara Walker
Clara Walker, MPH, is a Principal Project Officer at Southern Queensland Rural Health (SQRH). She is an Adjunct Research Fellow at the Centre for Health Research, University of Southern Queensland.
Tony Fallon
Tony Fallon, BAppSci, BAppSci (Hons), PhD, is a Senior Research Officer at Southern Queensland Rural Health (SQRH). He is an Adjunct Research Fellow at the Centre for Health Research, University of Southern Queensland.
Joshua Denham
Joshua Denham, BAppSci (Human Movement), Grad Dip, MA (Exercise Rehabilitation), PhD (Biomed), is a Lecturer in clinical Exercise Physiology/Sport and Exercise Science, University of Southern Queensland. He is a Centre for Health Research member and an Accredited Exercise Physiology/Exercise Science (AEP/AES) with Exercise and Sports Science Australia (ESSA).
Priya Martin
Priya Martin, BOT (Hons), MS (Psychotherapy & Counselling), PhD, is a Senior Research Fellow at the Rural Clinical School, University of Queensland. She is a member of the Australasian Interprofessional Practice and Education Network (AIPPEN) steering committee and the ‘Interprofessional.Global’ Global Impact Working Group.
Steve Woodruffe
Steve Woodruffe, BAppSci (HMS), AEP is a Clinical Educator in Exercise Physiology at Southern Queensland Rural Health (SQRH). He has over 20 years’ experience working as an Exercise Physiologist in a variety of clinical settings focused on chronic disease prevention and management.
Kate Bell
Kate Bell, B Education, M Clinical Exercise Physiology, is a Clinical Educator in Exercise Physiology at Southern Queensland Rural Health (SQRH). She has over 10 years’ experience in clinical supervision and education with a professional focus on exercise for chronic disease management, healthy aging, and gastrointestinal conditions.
Michelle Aniftos
Michelle Aniftos, BSc; MEd; MPsych (Clinical); GradCertClinNeurophysiology, is a Clinical Educator in Psychology at Southern Queensland Rural Health (SQRH), and Director of a private mental health practice. She has over 30 years’ experience providing assessment and intervention in the education and mental health sectors.
Jayne Kirkpatrick
Jayne Kirkpatrick, MNutDiet, GDTL, CertIVTA, APD, is a Clinical Educator in Nutrition and Dietetics at Southern Queensland Rural Health (SQRH) and at Darling Downs Health. She has 27 years’ experience working as a Dietitian/Nutritionist in a variety of clinical and community settings.
Nicola Cotter
Nicola Cotter (Physio), is Deputy Director (Darling Downs) at Southern Queensland Rural Health (SQRH). She has 15 years’ experience working as a Physiotherapist and Manager of multidisciplinary and interprofessional healthcare teams.
Dayle Osborn
Dayle Osborn (Nursing), MMHN, is the Health and Wellness Clinic Coordinator and Clinical Educator Nursing and Mental Health Nursing at Southern Queensland Rural Health (SQRH).
Geoff Argus
Geoff Argus (Psych Hons), MPsych (Clinical), is the Director of Southern Queensland Rural Health (SQRH). He is an Associate Professor with The University of Queensland and Adjunct Associate Professor with the University of Southern Queensland. He is a Board Director with Australian Rural Health Education Network (ARHEN) and the National Rural Health Alliance (NRHA).
References
- Alley, D. E., Shardell, M. D., Peters, K. W., McLean, R. R., Dam, T. L., Kenny, A. M., Fragala, M. S., Harris, T. B., Kiel, D. P., Guralnik, J. M., Ferrucci, L., Kritchevsky, S. B., Studenski, S. A., Vassileva, M. T., & Cawthon, P. P. (2014). Grip strength cutpoints for the identification of clinically relevant weakness. Journals of Gerontology: Series A, 69(5), 559–566. https://doi.org/10.1093/gerona/glu011
- Australian Government Department of Health and Aged Care. (2023). Rural health multidisciplinary training (RHMT) program. Australian Government. https://www.health.gov.au/our-work/rhmt
- Australian Institute of Health and Welfare. (2022). Rural and remote health. https://www.aihw.gov.au/reports/rural-remote-australians/rural-and-remote-health
- Australian Institute of Health and Welfare. (2023a). Alcohol, tobacco & other drugs in Australia. https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/about
- Australian Institute of Health and Welfare. (2023b). Chronic disease: Overview. https://www.aihw.gov.au/reports-data/health-conditions-disability-deaths/chronic-disease/overview
- Australian Institute of Health and Welfare. (2023c). Overweight and obesity. https://www.aihw.gov.au/reports/overweight-obesity/overweight-and-obesity-an-interactive-insight/contents/measuring-overweight-and-obesity
- Bohannon, R. W., & Crouch, R. (2017). Minimal clinically important difference for change in 6-minute walk test distance of adults with pathology: A systematic review. Journal of Evaluation in Clinical Practice, 23(2), 377–381. https://doi.org/10.1111/jep.12629
- Bohannon, R. W., Magasi, S. R., Bubela, D. J., Wang, Y., & Gershon, R. C. (2012). Grip and knee extension muscle strength reflect a common construct among adults. Muscle and Nerve, 46, 555–558. https://doi.org/10.1002/mus.23350
- Canadian Interprofessional Competency Framework. (2010). A national interprofessional competency framework. The collaborative. https: //phabc.Org/wp-content/uploads/2015/07/CIHC-National-interprofessional-competency-Framework.Pdf extension muscle strength reflect a common construct among adults. Muscle & Nerve, 46(4), 555–558.
- Casanova, C., Celli, B. R., Barria, P., Casas, A., Cote, C., de Torres, J. P., Jardim, J., M V, L., Marin, J. M. de OcaM, M., Pinto-Plata, V., & Aguirre-Jaime, A. (2011). The 6-min walk distance in healthy subjects: Reference standards from seven countries. The European Respiratory Journal, 37(1), 150–156. https://doi.org/10.1183/09031936.00194909.
- Celis-Morales, C. A., Welsh, P., Lyall, D. M., Steell, L., Petermann, F., Anderson, J., Iliodromiti, S., Sillars, A., Graham, N., Mackay, D. F., Pell, J. P., Gill, J. M. R., Sattar, N., & Gray, S. R. (2018). Associations of grip strength with cardiovascular, respiratory, and cancer outcomes and all cause mortality: Prospective cohort study of half a million UK biobank participants. The British Medical Journal, 361, k1651. https://doi.org/10.1136/bmj.k1651
- Centre for Health Economics. (2023). Scoring: Psychometric (unweighted) or utility (weighted)? Monash University, Monash business school. https://www.monash.edu/business/che/aqol/using-aqol/scoring
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge Academic.
- Coker, R. H., & Wolfe, R. R. (2018). Weight loss strategies in the elderly: A clinical conundrum. Obesity (Silver Spring), 26(1), 22–28. https://doi.org/10.1002/oby.21961
- Colman, C. (2022). Rural health is a crisis that can be solved, here and now. The Australian Journal of Rural Health, 30(1), 127–128. https://doi.org/10.1111/ajr.12848
- Cox, I. A., Campbell, J., de Graaff, B., Otahal, P., Corte, T. J., Moodley, Y., Hopkins, P., Macansh, S., Walters, E. H., & Palmer, A. J. (2023). Assessment of health-related quality of life in Australian patients with idiopathic pulmonary fibrosis: A comparison of the EQ-5D-5L and the AQoL-8D. Quality of Life Research, 32(2), 473–493. https://doi.org/10.1007/s11136-022-03205-z
- Darling Downs and West Moreton Primary Health Network. (2018). Health needs assessment. Description of health service use, workforce and consumer need. https://www.ddwmphn.com.au/uploads/images/2017-2018-Health-Needs-Assessment.pdf
- Delbressine, J. M., Jensen, D., Vaes, A. W., Li, P. Z., Bourbeau, J., Tan, W. C., Hajian, B., van ’t Hul, A. J., & Spruit, M. A. (2023). Reference values for six-minute walk distance and six-minute walk work in caucasian adults. Pulmonology, 29(5), 399–409. https://doi.org/10.1016/j.pulmoe.2023.02.014
- de Souza Vasconcelos, K. S., Domingues Dias, J. M., de Carvalho Bastone, A., Alvarenga Vieira, R., de Souza Andrade, A. C., Rodrigues Perracini, M., Oliveira Guerra, R., & Corrêa Dias, R. (2016). Handgrip strength cutoff points to identify mobility limitation in community-dwelling older people and associated factors. The Journal of Nutrition, Health & Aging, 20(3), 306–315. https://doi.org/10.1007/s12603-015-0584-y
- Eden, M. M., Tompkins, J., & Verheijde, J. L. (2018). Reliability and a correlational analysis of the 6MWT, ten-meter walk test, thirty second sit to stand, and the linear analog scale of function in patients with head and neck cancer. Physiotherapy Theory and Practice, 34(3), 202–211. https://doi.org/10.1080/09593985.2017.1390803
- Engel, L., Chen, G., Richardson, J., & Mihalopoulos, C. (2018). The impact of depression on health-related quality of life and wellbeing: Identifying important dimensions and assessing their inclusion in multi-attribute utility instruments. Quality of Life Research, 27(11), 2873–2884. https://doi.org/10.1007/s11136-018-1936-y
- Enright, P. L. (2003). The six-minute walk test. Respiratory Care, 48(8), 783–785.
- Farlow, J. L., Goodwin, C., & Sevilla, J. (2015). Interprofessional education through service-learning: Lessons from a student-led free clinic. Journal of Interprofessional Care, 29(3), 263–264. https://doi.org/10.3109/13561820.2014.936372
- Forbes, R., Beckman, E., Tower, M., Mandrusiak, A., Mitchell, L. K., Sexton, C. T., Cunningham, B., & Lewis, P. A. (2021). Interprofessional, student-led community health clinic: Expanding service provision and clinical education capacity. Australian Health Review, 45(2), 255–260. https://doi.org/10.1071/AH20021
- Gustafsson, L., Hutchinson, L., Theodoros, D., Williams, K., Copley, A., Fagan, A., & Desha, L. (2016). Healthcare students’ experiences of an interprofessional, student-led neuro-rehabilitation community-based clinic. Journal of Interprofessional Care, 30(2), 259–261. https://doi.org/10.3109/13561820.2015.1086730
- Haggarty, D., & Dalcin, D. (2014). Student-run clinics in Canada: An innovative method of delivering interprofessional education. Journal of Interprofessional Care, 28(6), 570–572. https://doi.org/10.3109/13561820.2014.916658
- Hawthorne, G., & Osborne, R. (2005). Population norms and meaningful differences for the assessment of quality of life (AQoL) measure. Australian and New Zealand Journal of Public Health, 29(2), 136–142. https://doi.org/10.1111/j.1467-842x.2005.tb00063.x
- Hopkins, S., Bacon, R., & Flynn, A. (2022). Student outcomes for interprofessional education in student led clinics: A rapid review. Journal of Interprofessional Care, 36(2), 234–244. https://doi.org/10.1080/13561820.2020.1858767
- Horn, D. B., Almandoz, J. P., & Look, M. (2022). What is clinically relevant weight loss for your patients and how can it be achieved? A narrative review. Postgraduate Medicine, 134(4), 359–375. https://doi.org/10.1080/00325481.2022.2051366
- Jensen, M. D., Ryan, D. H., Apovian, C. M., Ard, J. D., Comuzzie, A. G., Donato, K. A., Hu, F. B., Hubbard, V. S., Jakicic, J. M., & Kushner, R. F. (2014). AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. Journal of the American College of Cardiology, 63(25 Part B), 2985–3023. https://doi.org/10.1016/j.jacc.2013.11.004
- Jones, D., McAllister, L., & Lyle, D. (2015). Interprofessional academic service-learning in rural Australia: Exploring the impact on allied health student knowledge, skills, and practice. A qualitative study. International Journal of Practice-Based Learning in Health and Social Care, 3(2), 1–16. https://doi.org/10.18552/ijpblhsc.v3i2.217
- Kent, F., & Keating, J. L. (2015). Interprofessional education in primary health care for entry level students: A systematic literature review. Nurse Education Today, 35(12), 1221–1231. https://doi.org/10.1016/j.nedt.2015.05.005
- Kent, F., Martin, N., & Keating, J. L. (2016). Interprofessional student-led clinics: An innovative approach to the support of older people in the community. Journal of Interprofessional Care, 30(1), 123–128. https://doi.org/10.3109/13561820.2015.1070133
- Körner, M., Bütof, S., Müller, C., Zimmermann, L., Becker, S., & Bengel, J. (2016). Interprofessional teamwork and team interventions in chronic care: A systematic review. Journal of Interprofessional Care, 30(1), 15–28. https://doi.org/10.3109/13561820.2015.1051616
- Lai, F. Y. X., Kent, F., & Dodic, M. (2015). Exploring the value of interprofessional student‐led clinics for chronic disease patients. The Medical Journal of Australia, 203(10), 402–402. https://doi.org/10.5694/mja15.00360
- Lavie, C. J., Ozemek, C., Carbone, S., Katzmarzyk, P. T., & Blair, S. N. (2019). Sedentary behavior, exercise, and cardiovascular health. Circulation Research, 124(5), 799–815. https://doi.org/10.1161/circresaha.118.312669
- Lawrence, D., Bryant, T. K., Nobel, T. B., Dolansky, M. A., & Singh, M. K. (2015). A comparative evaluation of patient satisfaction outcomes in an interprofessional student-run free clinic. Journal of Interprofessional Care, 29(5), 445–450. https://doi.org/10.3109/13561820.2015.1010718
- Leong, D. P., Teo, K. K., Rangarajan, S., Lopez-Jaramillo, P., Avezum, A., Orlandini, A., Seron, P., Ahmed, S. H., Rosengren, A., Kelishadi, R., Rahman, O., Swaminathan, S., Iqbal, R., Gupta, R., Lear, S. A., Oguz, A., Yusoff, K., Zatonska, K. … Li, W. (2015). Prognostic value of grip strength: Findings from the prospective urban rural epidemiology (PURE) study. Lancet, 386(9990), 266–273. https://doi.org/10.1016/S0140-6736(14)62000-6
- Lutfiyya, M. N., Chang, L. F., McGrath, C., Dana, C., Lipsky, M. S., & Oelke, N. (2019). The state of the science of interprofessional collaborative practice: A scoping review of the patient health-related outcomes based literature published between 2010 and 2018. PLOS ONE, 14(6), e0218578. https://doi.org/10.1371/journal.pone.0218578
- Martin, P., Ford, M., Hill, A., Argus, G., Graham, N., & Browne, M. (2023). Comparing outcomes of an innovative interprofessional student placement model to standard placement models in rural healthcare settings. Journal of Interprofessional Care, 37(5), 767–773. https://doi.org/10.1080/13561820.2023.2166906
- Martin, P., Hill, A., Ford, M., Barnett, T., Graham, N., & Argus, G. (2022). A novel interprofessional education and supervision student placement model: Student and clinical educator perspectives and experiences. International Journal of Environmental Research and Public Health, 19(17), 10734. https://doi.org/10.3390/ijerph191710734
- Martin, P., Pighills, A., Burge, V., Argus, G., & Sinclair, L. (2021). Promoting interprofessional education and collaborative practice in rural health settings: Learnings from a state-wide multi-methods study. International Journal of Environmental Research and Public Health, 18(10), 5162. https://doi.org/10.3390/ijerph18105162
- Maxwell, A., Özmen, M., Iezzi, A., & Richardson, J. (2016). Deriving population norms for the AQoL-6D and AQoL-8D multi-attribute utility instruments from web-based data. Quality of Life Research, 25(12), 3209–3219. https://doi.org/10.1007/s11136-016-1337-z
- McGoon, M. D., Benza, R. L., Escribano-Subias, P., Jiang, X., D P, M., A J, P., Pepke-Zaba, J., Pulido, T., Rich, S., Rosenkranz, S., Suissa, S., & Humbert, M. (2013). Pulmonary arterial hypertension. Journal of the American College of Cardiology, 62(25_Supplement), D51–D59. https://doi.org/10.1016/j.jacc.2013.10.023
- Murray, C. J. L. (2022). The global burden of disease study at 30 years. Nature Medicine, 28(10), 2019–2026. https://doi.org/10.1038/s41591-022-01990-1
- National Rural Health Alliance. (2021). Rural health in Australia: Snapshot 2021. https://www.ruralhealth.org.au/rural-health-australia-snapshot
- Olson, R., & Bialocerkowski, A. (2014). Interprofessional education in allied health: A systematic review. Medical Education, 48(3), 236–246. https://doi.org/10.1111/medu.12290
- Pascucci, D., Sassano, M., Nurchis, M. C., Cicconi, M., Acampora, A., Park, D., Morano, C., & Damiani, G. (2021). Impact of interprofessional collaboration on chronic disease management: Findings from a systematic review of clinical trial and meta-analysis. Health Policy, 125(2), 191–202. https://doi.org/10.1016/j.healthpol.2020.12.006
- Pinto-Plata, V. M., Cote, C., Cabral, H., Taylor, J., & Celli, B. R. (2004). The 6‐min walk distance: Change over time and value as a predictor of survival in severe COPD. The European Respiratory Journal, 23(1), 28–33. https://doi.org/10.1183/09031936.03.00034603
- Pullon, S., Wilson, C., Gallagher, P., Skinner, M., McKinlay, E., Gray, L., & McHugh, P. (2016). Transition to practice: Can rural interprofessional education make a difference? A cohort study. BMC Medical Education, 16(1), 154. https://doi.org/10.1186/s12909-016-0674-5
- Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017). Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev, 6(6), Cd000072. https://doi.org/10.1002/14651858.CD000072.pub3
- Richardson, J., Iezzi, A., Khan, M. A., & Maxwell, A. (2014). Validity and reliability of the assessment of quality of life (AQoL)-8D multi-attribute utility instrument. The Patient: Patient-Centered Outcomes Research, 7(1), 85–96. https://doi.org/10.1007/s40271-013-0036-x
- Richardson, J., Sinha, K., Iezzi, A., & Khan, M. A. (2014). Modelling utility weights for the assessment of quality of life (AQoL)-8D. Quality of Life Research, 23(8), 2395–2404. https://doi.org/10.1007/s11136-014-0686-8
- Sangaleti, C., Schveitzer, M. C., Peduzzi, M., Zoboli, E. L. C. P., & Soares, C. B. (2017). Experiences and shared meaning of teamwork and interprofessional collaboration among health care professionals in primary health care settings: A systematic review. JBI Evidence Synthesis, 15(11), 2723–2788. https://journals.lww.com/jbisrir/fulltext/2017/11000/experiences_and_shared_meaning_of_teamwork_and.14.aspx
- Schofield, D., Shrestha, R. N., Cunich, M. M., Tanton, R., Veerman, L., Kelly, S. J., & Passey, M. E. (2016). Economic costs of chronic disease through lost productive life years (PLYs) among Australians aged 45–64 years from 2015 to 2030: Results from a microsimulation model. British Medical Journal Open, 6(9), e011151. https://doi.org/10.1136/bmjopen-2016-011151
- Singh, S. J., Puhan, M. A., Andrianopoulos, V., Hernandes, N. A., Mitchell, K. E., Hill, C. J., Lee, A. L., Camillo, C. A., Troosters, T., Spruit, M. A., Carlin, B. W., Wanger, J., Pepin, V., Saey, D., Pitta, F., Kaminsky, D. A., McCormack, M. C., MacIntyre, N., Culver, B. H. Holland, A. E. (2014). An official systematic review of the European respiratory society/American thoracic society: Measurement properties of field walking tests in chronic respiratory disease. The European Respiratory Journal, 44(6), 1447–1478. https://doi.org/10.1183/09031936.00150414
- Smith, J. A., Canuto, K., Canuto, K., Campbell, N., Schmitt, D., Bonson, J., Smith, L., Connolly, P., Bonevski, B., & Rissel, C. (2022). Advancing health promotion in rural and remote Australia: Strategies for change. Health Promotion Journal of Austtralia, 33(1), 3–6. https://doi.org/10.1002/hpja.569
- Troosters, T., Gosselink, R., & Decramer, M. (1999). Six minute walking distance in healthy elderly subjects. The European Respiratory Journal, 14(2), 270–274. https://doi.org/10.1034/j.1399-3003.1999.14b06.x
- Vancampfort, D., Stubbs, B., Firth, J., & Koyanagi, A. (2019). Handgrip strength, chronic physical conditions and physical multimorbidity in middle-aged and older adults in six low- and middle income countries. European Journal of Internal Medicine, 61, 96–102. https://doi.org/10.1016/j.ejim.2018.11.007
- Walker, C., Forbes, R., Osborn, D., Lewis, P. A., Cottrell, N., Peek, S., & Argus, G. (2022). The transformation of a student-led health clinic in rural Australia from a face-to-face service to a telehealth model: Evaluation of student and client experiences during a COVID-19 driven transition. Focus on Health Professional Education: A Multi-Disciplinary Journal, 23(2), 79–92. https://doi.org/10.11157/fohpe.v23i2.554
- Walker, C., Sangelaji, B., Osborn, D., Cotter, N., Argus, G., & Hulme, A. (2024). Findings, progress and lessons learned during the first three years of a student-resourced interprofessional health clinic in regional Australia. Journal of Interprofessional Care, 38(2), 403–408. https://doi.org/10.1080/13561820.2023.2282084
- Wang, C. Y., & Chen, L. Y. (2010). Grip strength in older adults: Test-retest reliability and cutoff for subjective weakness of using the hands in heavy tasks. Archives of Physical Medicine & Rehabilitation, 91(11), 1747–1751. https://doi.org/10.1016/j.apmr.2010.07.225
- Wei, H., Horns, P., Sears, S. F., Huang, K., Smith, C. M., & Wei, T. L. (2022). A systematic meta-review of systematic reviews about interprofessional collaboration: Facilitators, barriers, and outcomes. Journal of Interprofessional Care, 36(5), 735–749. https://doi.org/10.1080/13561820.2021.1973975
- World Health Organization. (2008). Waist circumference and waist-hip ratio. Report of a WHO expert consultation. https://www.who.int/publications/i/item/9789241501491
- World Health Organization. (2010). Framework for action on interprofessional education and collaborative practice. https://iris.who.int/handle/10665/70185
- World Health Organization. (2023). Noncommunicable diseases. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases