ABSTRACT
Thousands of young children die or sustain life changing disabilities every year because of unintentional child injury (UCI) at home. Many injuries could be prevented if parents and caregivers were more aware of risks and accident-avoidance strategies. The aim of this review was two-fold. First, we explored whether health education modified parent or caregiver knowledge, attitudes, or behaviour related to injury awareness and prevention. Our secondary aim was to describe strategies used when delivering health education. Intervention studies using quantitative methods published after 2010 were included. The participants were caregivers or parents of children younger than six years of age. A systematic search of multiple databases yielded twelve studies. The risk of bias (ROB) was assessed using the Cochrane ROBINS-I for non-randomised and ROB-2 for randomised studies. Data synthesis was performed following the steps described in the SWiM guideline. We followed PRISMA guidelines to report the process and results. Interventions were usually one-off, multifaceted, and interactive using printed materials, discussion, didactic teaching, video, and games. Improvement of knowledge ranged from 12.5% to 85%. Attitude improvement was noted in five studies and ranged from 6.6% to 28%. Self-reported behavioural change was noted in six studies. Follow up duration varied from less than one month to six months. The observed changes have not been linked to the numbers or severity of UCI. Health education is beneficial, but the true long-term impact has yet to be fully explored. Studies that provided the greatest improvements used theories of behaviour change and interventions that were designed for the specific needs of the target population. Our review provides health care professionals with evidence of the potential benefits of health education in enhancing parents’ awareness regarding preventing UCI and information about how to deliver health education, that can guide the review of prevention practices of UCI.
Introduction
Unintentional child injury (UCI) in children under five years of age is considered one of the most disturbing public health issues globally (Peden et al., Citation2009). It causes the death of thousands of children daily (Hyder & David, Citation2012; Sleet, Citation2018) and the hospitalisation of millions (Adeloye et al., Citation2018; Hogan et al., Citation2018). The time and resources needed for rehabilitation (Polinder et al., Citation2010) and management of psychological consequences (De Young et al., Citation2014; van Meijel et al., Citation2020) place a social and economic burden on the family (Dalal & Svanström, Citation2015).
The financial consequences impact health systems. The United States of America (USA) has a population of more than 23 million under-fives. It costs more than 15 billion US Dollars per year to manage the consequences of 1.6 million injuries in children between 0–4 years (CDC, Citation2020). The United Kingdom (UK) has a population of 3.7 million children under 5 years with 100,000 annual admissions due to UCI costing £150 million per year (Patel et al., Citation2017). A rapidly developing country such as Oman, a country in the Middle East with a population of 382,000 children under 5 years, has observed a significant number of UCI, reporting 86 deaths and 2614 hospital admissions in 2018 (Mehmood et al., Citation2018; MOH, Citation2018).
Nearly three-quarters of UCI occur at or close to home (Hashemi et al., Citation2017; Mehmood et al., Citation2018; Wynn et al., Citation2016). Socio-economic, environmental, and behavioural factors influence the rate of UCI at home (Baron-Epel & Ivancovsky, Citation2015). Good child supervision and maintenance of a safe environment reduce the risk of UCI (Falcone et al., Citation2016; Kendrick et al., Citation2016; Schnitzer et al., Citation2015; Watson & Errington, Citation2016). Caregiver knowledge, attitudes, beliefs, and behaviours influence their approach to UCI prevention (Al-Hajj et al., Citation2020; İnce et al., Citation2017; Younesian et al., Citation2016) increasing the complexity and challenge of promoting adherence to preventive practices (İnce et al., Citation2017; Lafta et al., Citation2014; Sutchritpongsa et al., Citation2013).
Health professionals have a considerable role in educating and raising caregiver awareness of child safety (Hanna et al., Citation2022) through health education; a health promotion approach using different strategies and models to enhance knowledge and attitudes (Glanz et al., Citation2008). Health education can take place in the community, primary care centre, or home (Habermehl et al., Citation2019; Silva et al., Citation2016) and may involve individual, group, or online training. High-income countries such as the UK and US have well-developed programmes with demonstrable impact on rates of injury (Duffee et al., Citation2017; Kendrick et al., Citation2013; Patel et al., Citation2017). However, in rapidly developing countries like Oman (Al Rumhi et al., Citation2020) and other neighbouring countries (Alkhamis & Abdulkader, Citation2020), where there is no established parenting programme or home visit, an alternative context-related programme, needs to be considered. Countries that look forward to establishing or developing the UCI prevention programme need evidence to guide their decision on approaches. Pooled knowledge concerning its effectiveness and ability to influence caregiver knowledge, behaviour and attitudes is lacking. Health practitioners who want to start health education programmes need to be able to evaluate the different approaches so that they can choose the suitable method for their population.
Aim
The purpose of our review was to identify the effect of health education on parental knowledge, attitudes, and behaviour towards UCI prevention. We identify the methods used to undertake and evaluate health education, including settings, length of the intervention, tools, and assessments to provide evidence toward developing educational guidelines for child safety and injury prevention by healthcare practitioners.
Methods
Review process and design
The review is reported according to PRISMA guidelines (Page et al., Citation2021), and conducted according to Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., Citation2008). The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO 2020 CRD42020200183).
Information source
A preliminary search was undertaken to identify keywords through indexed terms, text words and controlled vocabularies in each database. A systematic search was undertaken in September 2020 and updated in June 2022 using CINAHL Plus, MEDLINE, Cochrane Library, PsycINFO, ProQuest Central, ERIC, SCOPUS and Embase. In addition, the reference lists of each eligible paper were hand-searched for relevant research reports. Search operators were used to broaden the search, including truncation, stemming, wildcards, exact phrase searching, and word adjacency proximity strategies. Keywords were combined or excluded for advanced search using “Boolean operators” such as “and”, “or”, and “not”. An example search was undertaken in Medline (Ovid) and is presented in .
Table 1. Example search using Medline.
Eligible studies for inclusion were defined as any interventional primary research study conducted after 2010 and published in English or Arabic. The eligibility concerning population was limited to parents or caregivers of children under the age of six years. Studies conducted on disabled children and children of parents with mental illnesses were excluded from the review to provide a homogenous population for the synthesis.
Assessment of risk of bias
Each study was assessed independently by MJ and BD for risk of bias using ROBINS-I for non-randomised studies of interventions (Sterne et al., Citation2016) and RoB2 for randomised trials (Sterne et al., Citation2019). The results were collated, and discussion was used to achieve consensus. Additional reviewers were available to mediate should consensus not be readily achieved but this was not needed.
Data extraction
Data extraction was carried out using a tool adapted by the reviewers from “Cochrane data collection tool” (Li et al., Citation2019). It included two parts: first, for the study information necessary to determine the study’s eligibility for final analysis. Second, to collect details about publication, researchers, study purposes, design, participants, settings, context, interventions, outcome measures, outcomes, and results. Our review focused specifically on changes in the caregivers’ knowledge, attitudes, behaviour relating to UCI prevention and health education approaches. An Excel spreadsheet (Microsoft Corporation, Citation2021) was used to record and organise the extracted data.
Data synthesis
There was heterogeneity in the outcome measures used in the studies that prevented meta-analysis. Therefore, descriptive analysis and synthesis were undertaken and reported following the Synthesis Without Meta-analysis (SWiM) reporting guidelines (Campbell et al., Citation2020). This guidance has been developed to provide a robust reporting method for synthesis when meta-analysis is not possible and can be used as an extension to PRISMA. There are nine reporting items included in this method that ensure that authors provide a rationale for grouping the studies, selection of a standardised metric across the studies and how transformation were conducted, description of the synthesis methods used, prioritisation of studies in creating results and drawing conclusions, methods used to explore heterogeneity, assessment of the certainty of the findings, description of data presentation methods, reporting or results and limitations.
In our review grouping allowed comparison of the method of health education delivery, the use of health psychology models, and knowledge, attitudes, and behaviour outcomes according to the authors definitions. Mean and standard deviation were extracted as provided when possible. In one case the overall mean and standard deviation for knowledge, attitudes and behaviours were created from the individual items reported in the results (Ihalahewage et al., Citation2018) using an online statistics tool. We also calculated the percentage change in knowledge, attitude, and behaviours using the formula (post-measure – pre-measure/pre-measure)*100. The results for knowledge, attitude and behaviours were tabulated for each study and then presented as a descriptive summary and identification of notable examples such as greatest and least change. These results are considered in terms of the approach to development of the intervention, the method of delivery of the intervention and the context including cultural factors.
Risk of bias
The risk of bias was moderate to severe in most studies (). The most significant issue was participant selection. Two RCTs were included, one of which had no description of the randomisation process (Cheraghi et al., Citation2014) and the other used cluster randomisation with the unit being pre-schools (Ning et al., Citation2019). Participants were recruited using convenience methods and often from a health centre in all other studies.
Table 2. Risk of Bias (ROB) summary.
Most studies relied on parents’ self-reports to assess knowledge, attitudes and behaviour changes, potentially biasing outcome quality and overestimating the interventions’ effect. Additionally, most reports made no discussion of engagement with educational materials following the introductory session, meaning that the dose of education and compliance was not identified.
Many studies evaluated the impact of the intervention using a self-designed questionnaire that was piloted and provided validity and reliability data (Afshari et al., Citation2017; Cheraghi et al., Citation2014; El Seifi et al., Citation2018; Fardazar et al., Citation2016). In some cases, a validated questionnaire was used (Kahriman & Karadeniz, Citation2018; Ning et al., Citation2019; Silva et al., Citation2016). However, some studies used self-designed questionnaires and did not report validity of reliability data (Amini et al., Citation2021; Furman et al., Citation2020; Habermehl et al., Citation2019; Ihalahewage et al., Citation2018; Setien et al., Citation2014). A lack of psychometric data introduces a high risk of bias (Paterson & Britten, Citation2005; Scott, Citation1997).
Some studies used psychological health theories in the design of questionnaires and interventions. This provides a transparency and theoretical basis for decision-making relating to data collection and reporting of results that can reduce bias in interpretation and help to avoid other forms of bias such as those resulting from social pressure leading to reporting bias (van der Steen et al., Citation2019).
Duration of follow-up ranged from immediately after the intervention (Silva et al., Citation2016) to six months (Ning et al., Citation2019). Loss to follow up ranged from zero (Afshari et al., Citation2017; Cheraghi et al., Citation2014; Ihalahewage et al., Citation2018; Setien et al., Citation2014) to 40% (Furman et al., Citation2020; Ning et al., Citation2019), but some studies did not provide data about this and it was not possible to infer the loss to follow up from the data presented in the report (Amini et al., Citation2021; El Seifi et al., Citation2018; Fardazar et al., Citation2016; Kahriman & Karadeniz, Citation2018).
Results
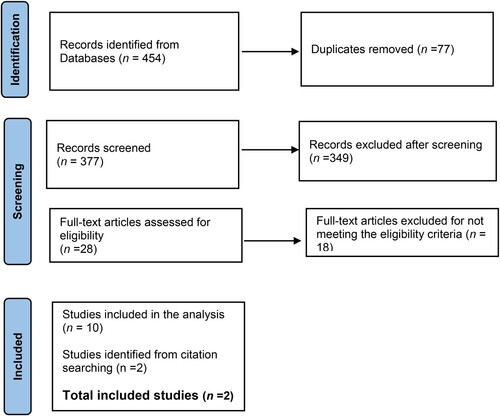
Four hundred and fifty-four research papers were retrieved () and exported to reference management software (EndnoteTM 20, Clarivate), where 77 duplicates removed. A further 377 papers were exported for inclusion-exclusion screenings to the Rayyan online systematic review platform (Ouzzani et al., Citation2016). Two reviewers (MJ/BD) independently screened the papers by title and abstract, which resulted in identification of 28 papers. Full-text screening led to a final total of ten articles. Scrutiny of reference lists identified a further two papers.
All were published in English between 2010 and 2020 and were conducted in Iran (n = 4), the United States of America (n = 3), Turkey (n = 1), Egypt (n = 1), Sri Lanka (n = 1), Brazil (n = 1), and China (n = 1) (). There was a mix of urban and rural settings, and most studies focused on low-income families and education interventions delivered in the community (El Seifi et al., Citation2018; Furman et al., Citation2020; Ihalahewage et al., Citation2018; Kahriman & Karadeniz, Citation2018).
Table 3. Summary of included studies.
The interventions were delivered to families, caregivers or parents. In several studies, the gender of the caregiver(s) or parent(s) were not provided (Furman et al., Citation2020; Habermehl et al., Citation2019; Ihalahewage et al., Citation2018; Ning et al., Citation2019; Setien et al., Citation2014). However, most studies only recruited mothers (Afshari et al., Citation2017; Amini et al., Citation2021; Cheraghi et al., Citation2014; El Seifi et al., Citation2018; Fardazar et al., Citation2016; Kahriman & Karadeniz, Citation2018; Silva et al., Citation2016).
The time spent on education varied between ten minutes (Habermehl et al., Citation2019) to four hours (Afshari et al., Citation2017; Amini et al., Citation2021; Cheraghi et al., Citation2014). The delivery method was not well described in any of the studies () but usually included some form of information delivery and a discussion or question and answer session. Most studies provided the participants with materials to take home in the form of written pamphlets. Two studies also provided the participants with child safety equipment such as socket protectors and cabinet clips (Furman et al., Citation2020; Habermehl et al., Citation2019).
Table 4. Summary of Education Intervention
Change in knowledge, attitudes, and behaviours in response to health education.
Pre- and post-measurement of knowledge, attitudes, and behaviours () were conducted using structured questionnaires with some also using a checklist.
Table 5. Change in parent/caregiver knowledge, attitudes and behaviours associated with health education intervention.
Changes in knowledge
Eight studies reported a statistically significant increase in caregivers’ knowledge relating to child safety and injury prevention in the intervention group but not the control group (Afshari et al., Citation2017; Amini et al., Citation2021; Cheraghi et al., Citation2014; El Seifi et al., Citation2018; Furman et al., Citation2020; Setien et al., Citation2014; Silva et al., Citation2016) (). The greatest change in knowledge was a 110% improvement (Ihalahewage et al., Citation2018) who used the framework of the Health Beliefs Model (Rosenstock et al., Citation1988) to design their intervention as well as using a co-production approach with caregivers. The intervention took the form of a practitioner-facilitated discussion group where caregivers identified poor safety practices and ways to reduce injury. The least change in knowledge was 4% (Setien et al., Citation2014) where the researchers designed the intervention alone based on risks associated with each developmental stage of the child. The intervention was a two-hour training session delivered by trained members of the Latino community (promotoras).
This is a small number of studies and so it is difficult to tell whether the use of a theoretical framework makes a difference to the outcomes. Two studies used the Health Beliefs Model and produced a 56% improvement in knowledge (Cheraghi et al., Citation2014) and a 110% improvement in knowledge (Ihalahewage et al., Citation2018). One study used the Theory of Planned Behaviour and identified a nine percent improvement in knowledge (Amini et al., Citation2021).
Changes in attitudes
When attitude was measured, an improvement was demonstrated. A statistically significant improvement was identified in six studies (Afshari et al., Citation2017; Amini et al., Citation2021; El Seifi et al., Citation2018; Ihalahewage et al., Citation2018; Ning et al., Citation2019; Setien et al., Citation2014) (). Ihalahewage et al. (Citation2018) created the greatest improvement with their small group discussion process. El Seifi et al. (Citation2018), also demonstrated a large improvement in attitudes, with a mean difference of 98%. Their intervention was a 45-minute lecture and discussion with a booklet to take home for groups of 8–10 women who lived with or near each other in a rural village setting. The intervention was based on 2016 guidelines from the Centers for Disease Control and Prevention (CDC, Citation2019) and no theoretical framework was described.
Generally, the change in attitudes was smaller than the changes in knowledge. Four of seven studies providing attitude change scores described improvements less than 15% (Afshari et al., Citation2017; Kahriman & Karadeniz, Citation2018; Ning et al., Citation2019; Setien et al., Citation2014). There was no consistent difference in approach between that group and those who saw a change of more than 30%.
Changes in behavior
Safety practice behaviour was reported in seven studies (Afshari et al., Citation2017; Fardazar et al., Citation2016; Ihalahewage et al., Citation2018; Kahriman & Karadeniz, Citation2018; Ning et al., Citation2019; Setien et al., Citation2014) (). Safety modifications made at home in response to the knowledge gained were confirmed through home visits (Ihalahewage et al., Citation2018; Kahriman & Karadeniz, Citation2018), phone follow up (Furman et al., Citation2020; Habermehl et al., Citation2019; Setien et al., Citation2014) or self-administered questionnaire (Ning et al., Citation2019). In the Habermehl et al. (Citation2019) study, 60% of the participants’ used the products provided by the researchers, and 40% of them bought new child safety items. Similarly, in the study of Furman et al. (Citation2020), a free safety device was distributed to study participants, and they responded positively and installed the devices at their homes.
The greatest improvement in behaviour was seen in Fardazar et al. (Citation2016) who used the Protection Motivation Theory (Rogers & Prentice-Dunn, Citation1997) as their framework. Their intervention was delivered in two 45-minute sessions spaced one week apart with five mothers in each group session. In the first session perceived vulnerability and perceived severity of accidents in children aged younger than five years was the focus. The second session focused on self-efficacy, response-efficacy and prevention behaviours of the mothers.
Discussion
This review aimed to identify health education interventions and their effects on caregivers’ knowledge, attitudes, and behaviours of preventing unintentional child injury (UCI) in and around the house. Twelve interventional studies were identified, analysed and synthesised. This review shows that a range of approaches to health education positively affect caregivers’ knowledge, attitudes, and behaviours towards UCI prevention. There are too few studies to determine whether one approach is better than another and the choice of how to deliver education will depend on the target population and local factors. The review suggests that the interventions that make the greatest contribution to positive change use of behavioural change theories to guide interventions and ensure that the intervention is designed with the target population in mind in terms of materials, environment and education strategies.
The use of behavioural change theories
Behavioural change depends on personal knowledge and attitudes, which are usually influenced by social and cultural norms. For example, parental child safety behaviours such as inadequate supervision (Schnitzer et al., Citation2015) may happen due to socioeconomic factors such as parents’ age and level of knowledge (Mayes et al., Citation2014; Morrongiello et al., Citation2006). Low education attainment in caregivers is an often-cited risk factor in unintentional injury (Eren et al., Citation2019; Morrongiello et al., Citation2006; Morrongiello & House, Citation2004; Nour et al., Citation2018; Thein et al., Citation2005; Villalba-Cota et al., Citation2004). The strong links between poverty and education (Liu et al., Citation2021) make it unsurprising that low income is also a common risk factor, cited alone or in conjunction with education (Chowdhury et al., Citation2009; Karb et al., Citation2016; Vecino-Ortiz et al., Citation2018). Young mothers, especially those with low educational levels (Morrongiello et al., Citation2006; Nour et al., Citation2018), and those of low or moderate socioeconomic status, were identified as a high-risk group (Campbell et al., Citation2019).
It is difficult to draw conclusions from such a small number of studies, some of which have limitations due to the lack of validation of their data collection instruments and reliance on self-reported improvement by the participants. However, the strategies demonstrating the greatest change tended to make use of theoretical frameworks. The Health Beliefs Model (Rosenstock et al., Citation1988) emerged from the work of a group of social psychologists in the 1950s and 60s who were looking for solutions to public health problems (Rosenstock, Citation1974). The focus of this work was to develop an understanding of preventive health behaviour. It was rooted in the principle that to avoid an illness the person must believe that they are personally susceptible to it, that having the disease was worth avoiding due to the likely negative impact of it, and that taking action would be beneficial despite the costs in terms of pain, embarrassment, or convenience. The appropriateness of this model is clear. The two studies that used this model (Cheraghi et al., Citation2014; Ihalahewage et al., Citation2018) focused their education on perceived severity, perceived barriers, cues to action and self-efficacy. The application of the HBM to the educational intervention and questionnaire was more transparent in the Cheraghi et al. study, and improvements in all areas were seen.
Two studies (Amini et al., Citation2021; Ning et al., Citation2019) use the Theory of Planned Behaviour (Ajzen, Citation1985, Citation1991). The principle behind this theory is that most volitional human behaviour is goal directed such that actions are largely governed by intentions. There are causal links between beliefs, attitudes, intentions, and behaviours, which Ajzen terms a theory of reasoned action. This theory is extended by a second component of the model which explores goal-directed behaviours that are influenced by internal and external factors. This is termed the theory of planned behaviour which considers perceived and actual control an individual may have over their behaviour. It allows consideration of constraints on action and models why intentions do not always lead to actions (Armitage & Conner, Citation2001). Like the HBM this model allows the researchers to examine the relationship between knowledge, attitudes, and actions and the two studies included in this review that used this model evaluated behavioural changes by parental self-report.
Fardazar et al. (Citation2016) used Protection Motivation Theory in their design and evaluation. This theory, developed by Rogers (Citation1975) explains how fear of the consequences of ill-health can act as a motivation to alter behaviour. Similar to HBM and TPB this model explains a relationship between the perceived severity of the threat, the probability of its occurrence and the efficacy of the recommended coping response (Maddux & Rogers, Citation1983). The training in the reviewed paper comprised of two 45-minute sessions. In the first the mothers were educated about the severity of injury and vulnerability of children. In the second session the focus was on effective prevention strategies and involved an attempt to increase their self-efficacy in preventative behaviours.
The final model employed in the reviewed studies was the PRECEDE-PROCEED model (Green, Citation1974; Green & Kreuter, Citation2005). The use of this model requires the development of an understanding of the community in which the eventual intervention will be used. Thus Afshari et al. (Citation2017) based their intervention on a study undertaken in a similar population (Rezapur-Shahkolai et al., Citation2017) and a preintervention collection of data in the study. In keeping with the behavioural health theories already mentioned, this model makes use of our understanding that beneficial behaviour change is influenced by several factors that enable, predispose, or reinforce behaviours that may or may not be preventative. One of the ways of maximising the effect of education using this model is to show concern for the needs of the target audience and structure communications so that they agree with their motivations. In one of the early descriptions of this model Green (Citation1974, p. 44) identifies one of the motivational factors as fear, one the fundamental factors that appear across all the models described thus far.
The theoretical basis of behaviour change is explicit in the studies we have discussed so far. While others have not been explicit, they all use strategies that are likely to bring about positive change. One of the common features of all interventions in the reviewed studies was the use of discussion in small homogenous groups. The degree of participant generation of discussion topics and problem solving is difficult to tell from most studies. However, Fardazar et al. (Citation2016); Ihalahewage et al. (Citation2018) emphasised the role of the participants in setting the agenda and this will lead to a focus on the most relevant issues for those groups. Both studies produced high levels of change as might be expected when education content is tailored to the needs of the community where change is desired. Social networking and learning in a group have a positive impact as this allows the exchange of expertise and concerns and can add social pressure to motivate change (Khanom et al., Citation2013; Machin et al., Citation2018).
In some of the populations that were targeted in the reviewed research fatalism has an influence. Fatalism is defined as a sense that the person has a lack of control over events, and there is a connection between fatalism and a lack of tacking preventative action (Perfetti, Citation2018). Fatalism is associated with an increased risk of UCI (Santagati et al., Citation2016) and may be resistant to change. Fatalism contributes to low self-efficacy for injury prevention and a behavioural health model can help to target the components of fatalism such as low self-efficacy, helplessness, meaninglessness, and inevitability.
Materials and design of education delivery
The content delivered to improve knowledge was usually identified from research or policy relevant to the local population. Previous research studies conducted to explore UCI causal factors recognised inadequate caregiver knowledge of child safety at a baseline (Akturk & Erci, Citation2016; Lafta et al., Citation2014). Inadequate knowledge of UCI prevention can be a risk factor that may lead to poor anticipation of injury risks and increase the risk of injury (Simpson et al., Citation2009) and low levels of pre-intervention knowledge were identified in this review.
One study in this review used a mobile phone application (app) to deliver the educational strategy (Ning et al., Citation2019). Phone apps have been used widely for different health education purposes (Jeffrey et al., Citation2019; Kang et al., Citation2019; Taki et al., Citation2019), and can positively change child safety attitudes and behaviour (McKenzie & Roberts, Citation2016; Ning et al., Citation2019; Omaki et al., Citation2017). However, clinicians’ opinions must be sought when designing a relevant app (Fitzgerald & McClelland, Citation2017).
The use of apps is attractive given the interactive nature and immediacy of the messaging. However, there are a few accessibility and inclusivity issues with many people unable to access the hardware or broadband to make good use of the app, which can exacerbate health inequalities (Bol et al., Citation2018; Borg et al., Citation2019). The design of the app must also skilfully take into consideration the multitude of platforms used to access the app and the attributes of the target population including learning disabilities and digital literacy (Galinski & Giraldo Perez, Citation2017) and inclination to use an app for health purposes (Powell & Deetjen, Citation2019).
The settings for education delivery were designed with the local population in mind and were community rather than hospital based. Home visits have the advantage that they allow assessment of behavioural changes as well as equipment installation and other home safety modifications. Many studies in this review used primary health care centres to deliver education interventions. When combined with other visits, for example, immunisation clinics, this can be a way to reach the target population. However, while Furman et al. (Citation2020) found mobile centres were effective and helped the researchers to reach an otherwise inaccessible urban population, this increases the cost of the intervention considerably.
Two studies included safety equipment in their intervention (Furman et al., Citation2020; Habermehl et al., Citation2019). Equipment is considered a passive health promotion intervention compared to health education. The systematic review by Abbassinia et al. (Citation2019) suggested that the use of safety equipment did not lead to a greater effect size of the intervention; the greatest effect was made by changing attitudes and knowledge, which led to changes in behaviour in terms of vigilance and self-efficacy.
Strengths and limitations
The findings of this study are relevant and applicable to children under the age of six and can be cautiously extrapolated beyond that age. We reviewed studies from different countries, which allowed some comparison of methods and results in different cultures. The outcome measures and data presented in the report did not allow for more than narrative synthesis and this means that comparison between studies is incomplete.
A lack of detail about educational intervention in most of the reports does not allow us to comment fully on the value of theoretical frameworks to guide interventions nor the method the researchers used to derive the content and delivery method of the sessions. In many cases the cultural and spiritual profile of the community may have influences their baseline and response to education and this was not well described in the studies. The review also included studies reported in English, if other languages were considered it could add additional knowledge.
Implication for practice and research
Education interventions can improve knowledge, attitudes, and behaviours in unintentional child injury prevention. The interventions can be simple and inexpensive and will work best when they are developed with a specific community in mind. The review’s findings can be used as supporting evidence to assist primary health care workers on issues to be considered when initiating or reviewing UCI health education programmes. Current health education initiatives can be reviewed and updated to develop a new health education guide on child injury prevention. By implementing relevant and resourceful health education initiatives, child safety culture will be sustainable in the long term. This in turn will help to spread safety awareness within the community.
Many of the studies in this area used self-designed questionnaires based on behavioural and health beliefs models. Further work is required to create robust questionnaires that can be across different studies to allow greater comparison of results and meta-analysis.
Conclusion
Health education interventions delivered in various ways and settings will improve knowledge, attitudes, and behaviours. Simple and replicable methods are used to deliver information and answer the questions of caregivers. The published studies tended to be conducted in low-income areas where it is likely that the educational attainment of the caregivers contributes to the baseline problem. There is a cost associated with delivering health education to reduce unintentional child injury. Well conducted studies that include larger samples and cover geographical areas would determine the impact of the improvements in knowledge, attitudes, and behaviours on the incidence of injury.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Muna Al Mushaikhi
Muna Al Mushaikhi is a PhD researcher in the School of Nursing at the University of Birmingham, UK.
Julie Taylor
Julie Taylor is Director of Research and Professor of Child Protection.
Ben Donagh
Ben Donagh is a doctoral researcher in the School of Nursing at the University of Birmingham, UK.
Amelia Swift
Amelia Swift is a Reader in Health Professional Education and Head of Education for Nursing and Midwifery.
References
- Abbassinia, M., Barati, M., & Afshari, M. (2019). Effectiveness of interventions in the prevention of home injuries among children under 5 years of age: A systematic review. Archives of Trauma Research, 8(4), 190–197. https://doi.org/10.4103/atr.atr_22_19
- Adeloye, D., Bowman, K., Chan, K. Y., Patel, S., Campbell, H., & Rudan, I. (2018). Global and regional child deaths due to injuries: An assessment of the evidence. Journal of Global Health, 8(2). https://doi.org/10.7189/jogh.08.021104
- Afshari, M., Moghimbeigi, A., Hazavehei, S. M. M., & Rezapur-Shahkolai, F. (2017). Effect of a model-based educational program for mothers, on home-related injury prevention among under-five-year children in rural Twiserkan, Iran. The Turkish Journal of Pediatrics, 59(6), 648–656. https://doi.org/10.24953/turkjped.2017.06.005
- Ajzen, I. (1985). From intentions to action: A theory of planned behaviour. In J. Kuhl & J. Beckman (Eds.), Action-control: From cognition to behaviour (pp. 11–39). Springer.
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. https://doi.org/10.1016/0749-5978(91)90020-T
- Akturk, Ü, & Erci, B. (2016). Determination of knowledge, attitudes and behaviors regarding factors causing home accidents and prevention in mothers with a child aged 0-5 years. Journal of Education and Practice, 7(18), 142–153.
- Al Rumhi, A., Al Awisi, H., Al Buwaiqi, M., & Al Rabaani, S. (2020). Home accidents among children: A retrospective study at a tertiary care center in Oman. Oman Medical Journal, 35(1), e85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6975254/pdf/OMJ-35-01-1900051.pdf https://doi.org/10.5001/omj.2020.03
- Al-Hajj, S., El Haj, R., Chaaya, M., Sharara-Chami, R., & Mehmood, A. (2020). Child injuries in Lebanon: Assessing mothers injury prevention knowledge attitude and practices – A cross sectional study.
- Alkhamis, K. N., & Abdulkader, R. S. (2020). Assessment of unintentional childhood injuries and associated factors in the pediatric clinics of a tertiary care hospital in Riyadh, Saudi arabia. Journal of Family & Community Medicine, 27(3), 168–177. https://doi.org/10.4103/jfcm.JFCM_75_20
- Amini, R., Kalvandi, N., Khodaveisi, M., & Tapak, L. (2021). Investigation of the effect of education based on the theory of planned behavior on the mothers’ preventive practices regarding toddler home injuries. Home Health Care Management & Practice, 33(4), 250–257. https://doi.org/10.1177/10848223211000048
- Armitage, C. J., & Conner, M. (2001). Efficacy of the theory of planned behaviour: A meta-analytic review. British Journal of Social Psychology, 40(4), 471–499. https://doi.org/10.1348/014466601164939
- Barnett, D. J., Balicer, R. D., Blodgett, D., Fews, A. L., Parker, C. L., & Links, J. M. (2005). The application of the haddon matrix to public health readiness and response planning." Environmental Health Perspectives, 113(5), 561–566. https://doi.org/10.1289/ehp.7491
- Baron-Epel, O., & Ivancovsky, M. (2015). A socio-ecological model for unintentional injuries in minorities: A case study of Arab Israeli children. International Journal of Injury Control and Safety Promotion, 22(1), 48–56. https://doi.org/10.1080/17457300.2013.855794
- Bol, N., Helberger, N., & Weert, J. C. (2018). Differences in mobile health app use: A source of new digital inequalities? The Information Society, 34(3), 183–193. https://doi.org/10.1080/01972243.2018.1438550
- Borg, K., Boulet, M., Smith, L., & Bragge, P. (2019). Digital inclusion & health communication: A rapid review of literature. Health Communication, 34(11), 1320–1328. https://doi.org/10.1080/10410236.2018.1485077
- Campbell, M., Lai, E. T., Pearce, A., Orton, E., Kendrick, D., Wickham, S., & Taylor-Robinson, D. C. (2019). Understanding pathways to social inequalities in childhood unintentional injuries: Findings from the UK millennium cohort study. BMC Pediatrics, 19(1), 1–17. https://doi.org/10.1186/s12887-019-1514-7
- Campbell, M., McKenzie, J. E., Sowden, A., Katikireddi, S. V., Brennan, S. E., Ellis, S., Hartmann-Boyce, J., Ryan, R., Shepperd, S., & Thomas, J. (2020). Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 368, 16890. https://doi.org/10.1136/bmj.16890.
- CDC. (2020, December 2, 2021). Web-based Injury Statistics Query and Reporting System. Retrieved May 23, 2022, from https://www.cdc.gov/injury/wisqars/
- Centres for Disease Control and Prevention. (2019). Protect the one's you love: Child Injuries are Preventable. US Department of Health and Human Services. Retrieved January 21, 2022, from https://www.cdc.gov/safechild/publications.html
- Cheraghi, P., Poorolajal, J., Hazavehi, S., & Rezapur-Shahkolai, F. (2014). Effect of educating mothers on injury prevention among children aged< 5 years using the health belief model: A randomized controlled trial. Public Health, 128(9), 825–830. https://doi.org/10.1016/j.puhe.2014.06.017
- Chowdhury, S. M., Rahman, A., Mashreky, S. R., Giashuddin, S. M., Svanstrom, L., Horte, L. G., & Rahman, F. (2009). The horizon of unintentional injuries among children in low-income setting: An overview from Bangladesh health and injury survey. Journal of Environmental and Public Health, 2009, Article 435403. https://doi.org/10.1155/2009/435403
- Dalal, K., & Svanström, L. (2015). Economic burden of disability adjusted life years (DALYs) of injuries. Health, 7(4), 487–494. https://doi.org/10.4236/health.2015.74058
- De Young, A. C., Hendrikz, J., Kenardy, J. A., Cobham, V. E., & Kimble, R. M. (2014). Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. Journal of Child and Adolescent Psychopharmacology, 24(1), 9–17. https://doi.org/10.1089/cap.2013.0066
- Duffee, J. H., Mendelsohn, A. L., Kuo, A. A., Legano, L. A., Earls, M. F., C, C. H. I. L. D. H. O. O. D., Chilton, O. E., Flanagan, L. A., Dilley, P. J., & Green, K. J., & E, A. (2017). Early childhood home visiting. Pediatrics, 140(3), e20172150. https://doi.org/10.1542/peds.2017-2150
- El Seifi, O. S., Mortada, E. M., & Abdo, N. M. (2018). Effect of community-based intervention on knowledge, attitude, and self-efficacy toward home injuries among Egyptian rural mothers having preschool children. PLoS One, 13(6), 1. https://search.proquest.com/docview/2058501785?accountid=8630 https://birmingham-primo.hosted.exlibrisgroup.com/openurl/44BIR/44BIR_Services?genre=article&issn=1932-6203&title=Effect+of+community-based+intervention+on+knowledge%2C+attitude%2C+and+self-efficacy+toward+home+injuries+among+Egyptian+rural+mothers+having+preschool+children.&volume=13&issue=6&date=2018&atitle=Effect+of+community-based+intervention+on+knowledge%2C+attitude%2C+and+self-efficacy+toward+home+injuries+among+Egyptian+rural+mothers+having+preschool+children.&spage=e0198964&sid=ProQ%3Amedline&author=El+Seifi https://doi.org/10.1371/journal.pone.0198964
- Eren, B., Tas, A., Guzey, F. K., Gulec, I., Tufan, A., & Karacan, M. (2019). Television tip-over related head injuries: A particular type of child neglect. Turkish Neurosurgery, 29(3), 349–354. https://doi.org/10.5137/1019-5149.JTN.23279-18.1
- Falcone Jr, R. A., Edmunds, P., Lee, E., Gardner, D., Price, K., Gittelman, M., Pomerantz, W., Besl, J., Madhavan, G., & & Phelan, K. J. (2016). Volunteer driven home safety intervention results in significant reduction in pediatric injuries: A model for community based injury reduction. Journal of Pediatric Surgery, 51(7), 1162–1169. https://doi.org/10.1016/j.jpedsurg.2015.11.020
- Fardazar, E. F., Solhi, M., Mansori, K., Mansouri Hanis, S., & Hashemi, S. S. (2016). Assessment the effect of educational intervention on preventive behaviors of home accidents in mothers with children less than 5-year based on protection motivation theory (PMT). International Journal of Pediatrics, 4(7), 2051–2059. http://ijp.mums.ac.ir/article_6751.html
- Fitzgerald, M., & McClelland, T. (2017). What makes a mobile app successful in supporting health behaviour change? Health Education Journal, 76(3), 373–381. https://doi.org/10.1177/0017896916681179
- Furman, L., Strotmeyer, S., Vitale, C., & Gaines, B. A. (2020). Evaluation of a mobile safety center's impact on pediatric home safety knowledge and device use. Injury Epidemiology, 7(1), 1–9. https://doi.org/10.1186/s40621-019-0228-5
- Galinski, C., & Giraldo Perez, B. S. (2017). The need for information on standards on eAccessibility&eInclusion – Based on the experience of the EU-project IN LIFE. Studies in Health Technology and Informatics, 242, 119–122. https://doi.org/10.3233/978-1-61499-798-6-119
- Glanz, K., Rimer, B. K., & Viswanath, K. (2008). Health behavior and health education: Theory, research, and practice. John Wiley & Sons.
- Green, L., & Kreuter, M. K. (2005). Health program planning: An educational and ecological approach. McGraw Hill.
- Green, L. W. (1974). Toward cost-benefit evaluations of health education: Some concepts, methods, and examples. Health Education & Behavior, 2(1_suppl), 34–64. https://doi.org/10.1177/10901981740020S106
- Habermehl, N., Diekroger, E., Lazebnik, R., & Kim, G. (2019). Injury prevention education in the waiting room of an underserved pediatric primary care clinic. Clinical Pediatrics, 58(1), 73–78. https://doi.org/10.1177/0009922818806315
- Hanna, J. L., Wright, M. F., & Azar, S. T. (2022). Use of a serious game simulation to build early childhood staff capacity for reducing unintentional childhood injuries. Journal of Safety Research 82, 85–92. https://doi.org/10.1016/j.jsr.2022.04.008
- Hashemi, S. S., Sharhani, A., Lotfi, B., Ahmadi-Juibari, T., Shaahmadi, Z., & Aghaei, A. (2017). A systematic review on the epidemiology of pediatric burn in Iran. Journal of Burn Care & Research: Official Publication of the American Burn Association, 38(6), e944–e951. https://doi.org/10.1097/BCR.0000000000000524 (Erratum in: J Burn Care Res. 2018 Jan 1;39(1):173; PMID: 29931304 [ https://www.ncbi.nlm.nih.gov/pubmed/29931304])
- Higgins, J. P. T., Green, S., & Cochrane, C. (2008). Cochrane handbook for systematic reviews of interventions [electronic resource]. Wiley-Blackwell.
- Hogan, C. M., Weaver, N. L., Cioni, C., Fry, J., Hamilton, A., & Thompson, S. (2018). Parental perceptions, risks, and incidence of pediatric unintentional injuries. Journal of Emergency Nursing, 44(3), 267–273. https://doi.org/10.1016/j.jen.2017.07.017
- Hyder, A. A., & David, B. (2012). Saving 1000 children a day: The potential of child and adolescent injury prevention. International Journal of Child and Adolescent Health, 5(3), 267–280.
- Ihalahewage, N., Fernando, W. M. S., & Weliange, A. A. S. S. (2018). Health promotion approach to reduce unintentional home injuries of young children in rural villages in the north central province of Sri Lanka. Sri Lanka Journal of Child Health, 47(1), 33–39. https://www.scopus.com/inward/record.uri?eid=2-s2.0-85060114017&doi=10.4038%2fsljch.v47i1.8427&partnerID=40&md5=f2ca5ae7322238abe9d0cdfed264950b https://doi.org/10.4038/sljch.v47i1.8427
- İnce, T., Yalçın, S., & Yurdakök, K. (2017). Parents’ attitudes and adherence to unintentional injury prevention measures in Ankara, Turkey. Balkan Medical Journal, 34(4), 335–342. https://dergipark.org.tr/en/pub/bmj/issue/41583/502390
- Jeffrey, B., Bagala, M., Creighton, A., Leavey, T., Nicholls, S., Wood, C., Longman, J., Barker, J., & Pit, S. (2019). Mobile phone applications and their use in the self-management of type 2 diabetes mellitus: A qualitative study among app users and non-app users. Diabetology & Metabolic Syndrome, 11(1), 1–17. https://doi.org/10.1186/s13098-019-0480-4
- Kahriman, I. L., & Karadeniz, H. (2018). Effects of a safety-awareness-promoting program targeting mothers of children aged 0-6 years to prevent pediatric injuries in the home environment: Implications for nurses. Journal of Trauma Nursing: The Official Journal of the Society of Trauma Nurses, 25(5), 327-335. https://search.proquest.com/docview/2105041569?accountid=8630 https://birmingham-primo.hosted.exlibrisgroup.com/openurl/44BIR/44BIR_Services?genre=article&issn=10787496&title=Effects+of+a+Safety-Awareness-Promoting+Program+Targeting+Mothers+of+Children+Aged+0-6+Years+to+Prevent+Pediatric+Injuries+in+the+Home+Environment%3A+Implications+for+Nurses.&volume=25&issue=5&date=2018+Sep%2FOct&atitle=Effects+of+a+Safety-Awareness-Promoting+Program+Targeting+Mothers+of+Children+Aged+0-6+Years+to+Prevent+Pediatric+Injuries+in+the+Home+Environment%3A+Implications+for+Nurses.&spage=327&sid=ProQ%3Amedline&author=Kahriman https://doi.org/10.1097/JTN.0000000000000384
- Kang, Y.-N., Shen, H.-N., Lin, C.-Y., Elwyn, G., Huang, S.-C., Wu, T.-F., & Hou, W.-H. (2019). Does a mobile app improve patients’ knowledge of stroke risk factors and health-related quality of life in patients with stroke? A randomized controlled trial. BMC Medical Informatics and Decision Making, 19(1), 1–9. https://doi.org/10.1186/s12911-018-0723-6
- Karb, R. A., Subramanian, S. V., & Fleegler, E. W. (2016). County poverty concentration and disparities in unintentional injury deaths: A fourteen-year analysis of 1.6 million U.S. Fatalities. PLoS One, 11(5), e0153516. https://doi.org/10.1371/journal.pone.0153516
- Kendrick, D., Mulvaney, C. A., Ye, L., Stevens, T., Mytton, J. A., & Stewart-Brown, S. (2013). Parenting interventions for the prevention of unintentional injuries in childhood. The Cochrane Database of Systematic Reviews (3), CD006020. https://doi.org/10.1002/14651858.CD006020.pub3 (Update of: Cochrane Database Syst Rev. 2007 Oct 17;(4):CD006020; PMID: 17943875 [ https://www.ncbi.nlm.nih.gov/pubmed/17943875])
- Kendrick, D., Zou, K., Ablewhite, J., Watson, M., Coupland, C., Kay, B., Hawkins, A., & Reading, R. (2016). Risk and protective factors for falls on stairs in young children: Multicentre case–control study. Archives of Disease in Childhood, 101(10), 909. https://doi.org/10.1136/archdischild-2015-308486
- Khanom, A., Hill, R. A., Brophy, S., Morgan, K., Rapport, F., & Lyons, R. (2013). Mothers’ perspectives on the delivery of childhood injury messages: A qualitative study from the growing up in Wales, environments for healthy living study (EHL). BMC Public Health, 13(1), 1–9. https://doi.org/10.1186/1471-2458-13-806
- Lafta, R. K., Al-Shatari, S. A., & Abass, S. (2014). Mothers’ knowledge of domestic accident prevention involving children in Baghdad city. Qatar Medical Journal, 2013(2), 17. https://doi.org/10.5339/qmj.2013.17
- Li, T., Higgins, J. P., & Deeks, J. J. (2019). Collecting data. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M. J. Page, V. A. Welch (Eds.), Cochrane handbook for systematic reviews of interventions (pp. 109–141). https://doi.org/10.1002/9781119536604.ch5
- Liu, F., Li, L., Zhang, Y., Ngo, Q.-T., & Iqbal, W. (2021). Role of education in poverty reduction: Macroeconomic and social determinants form developing economies. Environmental Science and Pollution Research International, 28(44), 63163–63177. https://doi.org/10.1007/s11356-021-15252-z
- Machin, A. I., Ngamsuoy, A., & Pearson, P. (2018). Collaborative child home injury prevention in Thailand: An action research study. Nursing & Health Sciences, 20(2), 206-213. https://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed19&AN=625830783.https://birmingham-primo.hosted.exlibrisgroup.com/openurl/44BIR/44BIR_Services?sid=OVID:embase&id=pmid:29349899&id=10.1111%2Fnhs.12403&issn=1442-2018&isbn=&volume=20&issue=2&spage=206&pages=206-213&date=2018&title=Nursing+%26+health+sciences&atitle=Collaborative+child+home+injury+prevention+in+Thailand%3A+An+action+research+study&aulast=Machin&pid=%3Cauthor%3EMachin+A.I.%3C%2Fauthor%3E%3CAN%3E625830783%3C%2FAN%3E%3CDT%3EArticle%3C%2FDT%3E https://doi.org/10.1111/nhs.12403
- Maddux, J. E., & Rogers, R. W. (1983). Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. Journal of Experimental Social Psychology, 19(5), 469–479. https://doi.org/10.1016/0022-1031(83)90023-9
- Mayes, S., Roberts, M. C., & Stough, C. O. (2014). Risk for household safety hazards: Socioeconomic and sociodemographic factors. Journal of Safety Research, 51, 87–92. https://doi.org/10.1016/j.jsr.2014.09.002
- McKenzie, L. B., & Roberts, K. J. (2016). 335 development of the make safe happen app, a home safety mobile application. BMJ Publishing Group Ltd.
- Mehmood, A., Agrawal, P., Allen, K. A., Al-Kashmiri, A., Al-Busaidi, A., & Hyder, A. A. (2018). Childhood injuries in Oman: Retrospective review of a multicentre trauma registry data. BMJ Paediatrics Open, 2(1), 1–8. https://doi.org/10.1136/bmjpo-2018-000310
- Microsoft Corporation. (2021). Microsoft Excel. In (Version Microsoft 365 for Enterprise) https://office.microsoft.com/excel
- MOH. (2018). Annual Health Report. Ministry of Health. https://www.moh.gov.om/en/web/statistics/-/20-69
- Morrongiello, B. A., Corbett, M., McCourt, M., & Johnston, N. (2006). Understanding unintentional injury risk in young children II. The contribution of caregiver supervision, child attributes, and parent attributes. Journal of Pediatric Psychology, 31(6), 540–551. https://doi.org/10.1093/jpepsy/jsj073
- Morrongiello, B. A., & House, K. (2004). Measuring parent attributes and supervision behaviors relevant to child injury risk: Examining the usefulness of questionnaire measures. Injury Prevention, 10(2), 114–118. https://doi.org/10.1136/ip.2003.003459
- Ning, P., Cheng, P., Schwebel, D. C., Yang, Y., Yu, R., Deng, J., Li, S., & Hu, G. (2019). An app-based intervention for caregivers to prevent unintentional injury among preschoolers: Cluster randomized controlled trial. JMIR MHealth and UHealth, 7(8), e13519. https://doi.org/10.2196/13519
- Nour, M., Alharbi, W., Alawneh, S., Al Ansari, A., Al–Luqmani, A. D., Alharbi, A. F., Sonari, M. A., Al–Hassani, H. K., & Al–Malki, A. H. (2018). Knowledge, attitude and practices of mothers towards home accident among children, Makkah, KSA. European Journal of Phamaceuticalans Medical Research, 5(2), 139–147.
- Omaki, E., Rizzutti, N., Shields, W., Zhu, J., McDonald, E., Stevens, M. W., & Gielen, A. (2017). A systematic review of technology-based interventions for unintentional injury prevention education and behaviour change. Injury Prevention, 23(2), 138–146. https://doi.org/10.1136/injuryprev-2015-041740
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—a web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372(71), 1–9. https://doi.org/10.1136/bmj.n71
- Patel, D., Magnusen, E., & Sandell, J. M. (2017). Prevention of unintentional injury in children. Paediatrics and Child Health, 27(9), 420–426. https://doi.org/10.1016/j.paed.2017.05.004
- Paterson, C., & Britten, N. (2005). A narrative review shows the unvalidated use of self-report questionnaires for individual medication as outcome measures. Journal of Clinical Epidemiology, 58(10), 967–973. https://doi.org/10.1016/j.jclinepi.2005.03.012
- Peden, M., Oyegbite, K., Ozanne-Smith, J., Hyder, A. A., Branche, C., Rahman, A., Rivara, F., & Bartolomeos, K. (2009). World report on child injury prevention (Vol. 2008). World Health Organization Geneva.
- Perfetti, A. R. (2018). Fate and the clinic: A multidisciplinary consideration of fatalism in health behaviour. Medical Humanities, 44(1), 59–62. https://doi.org/10.1136/medhum-2017-011319
- Polinder, S., Haagsma, J. A., Toet, H., Brugmans, M. J., & van Beeck, E. F. (2010). Burden of injury in childhood and adolescence in 8 European countries. BMC Public Health, 10(1), 1–8. https://doi.org/10.1186/1471-2458-10-1
- Powell, J., & Deetjen, U. (2019). Characterizing the digital health citizen: Mixed-methods study deriving a New typology. Journal of Medical Internet Research, 21(3), 1–10. https://doi.org/10.2196/11279
- Rezapur-Shahkolai, F., Afshari, M., Moghimbeigi, A., & Hazavehei, S. M. M. (2017). Home-related injuries among under-five-year children and mothers’ care regarding injury prevention in rural areas. International Journal of Injury Control and Safety Promotion, 24(3), 354–362. https://doi.org/10.1080/17457300.2016.1200628
- Rogers, R. W. (1975). A protection motivation theory of fear appeals and attitude change. The Journal of Psychology, 91(1), 93–114. https://doi.org/10.1080/00223980.1975.9915803
- Rogers, R. W., & Prentice-Dunn, S. (1997). Protection motivation theory. In D. S. Gochman (Ed.), Handbook of health behavior research 1: Personal and social determinants (pp. 113–132). Plenum Press.
- Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education & Behavior, 2(4), 328–335. https://doi.org/10.1177/109019817400200403
- Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education Quarterly, 15(2), 175–183. https://doi.org/10.1177/109019818801500203
- Santagati, G., Vezzosi, L., & Angelillo, I. F. (2016). Unintentional injuries in children up to six years of age and related parental knowledge, attitudes, and behaviors in Italy. The Journal of Pediatrics, 177, 267–272. e262. https://doi.org/10.1016/j.jpeds.2016.06.083
- Schnitzer, P. G., Dowd, M. D., Kruse, R. L., & Morrongiello, B. A. (2015). Supervision and risk of unintentional injury in young children. Injury Prevention, 21(e1), e63–e70. https://doi.org/10.1136/injuryprev-2013-041128
- Scott, I. (1997). You can't believe all that you're told: The issue of unvalidated questionnaires. Injury Prevention, 3(1), 5–6. https://doi.org/10.1136/ip.3.1.5
- Setien, M. A., Han, D., Zuniga, G. C., Mier, N., Lucio, R. L., & Treviño, L. (2014). Does injury prevention education initiate household changes in a spanish-speaking minority population? Journal of Community Health, 39(1), 167–172. https://doi.org/10.1007/s10900-013-9755-0
- Silva, E. C. S., de Fátima Fernandes, M. N., Sá, M. C. N., de Souza, L. M., de Araújo Gordon, A. S., de Jesus Costa, A. C. P., de Araújo, T. S., da Silva Carvalho, Q. G., Maia, C. C., & Machado, A. L. G. (2016). The effect of educational intervention regarding the knowledge of mothers on prevention of accidents in childhood. The Open Nursing Journal, 10(1), 113–121. https://doi.org/10.2174/1874434601610010113
- Simpson, J. C., Turnbull, B. L., Ardagh, M., & Richardson, S. (2009). Child home injury prevention: Understanding the context of unintentional injuries to preschool children. International Journal of Injury Control and Safety Promotion, 16(3), 159–167. https://doi.org/10.1080/17457300903135636
- Sleet, D. A. (2018). The global challenge of child injury prevention. In Multidisciplinary Digital Publishing Institute.
- Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., & Boutron, I. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355, i4919. https://doi.org/10.1136/bmj.i4919
- Sterne, J. A., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H.-Y., Corbett, M. S., & Eldridge, S. M. (2019). Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. https://doi.org/10.1136/bmj.l4898
- Sutchritpongsa, S., Sangwisit, S., & Sonjaipanich, S. (2013). Parental awareness of household injury prevention: Adequacy of anticipatory guidance for well childcare. Journal of the Medical Association of Thailand, 96(12), 1531–1535.
- Taki, S., Russell, C. G., Wen, L. M., Laws, R. A., Campbell, K., Xu, H., & Denney-Wilson, E. (2019). Consumer engagement in mobile application (app) interventions focused on supporting infant feeding practices for early prevention of childhood obesity. Frontiers in Public Health, 7, 1–9. https://doi.org/10.3389/fpubh.2019.00060
- Thein, M. M., Lee, B. W., & Bun, P. Y. (2005). Knowledge, attitude and practices of childhood injuries and their prevention by primary caregivers in Singapore. Singapore Medical Journal, 46(3), 122–126. http://www.smj.org.sg/sites/default/files/4603/4603a2.pdf
- van der Steen, J. T., ter Riet, G., van den Bogert, C. A., & Bouter, L. M. (2019). Causes of reporting bias: A theoretical framework [version 1 peer review: 2 approved with reservations]. F1000 Research, 8, 1–20. https://doi.org/10.12688/f1000research.18310.1
- van Meijel, E. P. M., Gigengack, M. R., Verlinden, E., van der Steeg, A. F. W., Goslings, J. C., Bloemers, F. W., Luitse, J. S. K., Boer, F., Grootenhuis, M. A., & Lindauer, R. J. L. (2020). Short and long-term parental posttraumatic stress after a child's accident: Prevalence and associated factors. Child Psychiatry and Human Development, 51(2), 200–208. https://doi.org/10.1007/s10578-019-00924-2
- Vecino-Ortiz, A. I., Jafri, A., & Hyder, A. A. (2018). Effective interventions for unintentional injuries: A systematic review and mortality impact assessment among the poorest billion. The Lancet. Global Health, 6(5), e523–e534. https://doi.org/10.1016/S2214-109X(18)30107-4
- Villalba-Cota, J., Trujillo-Hernandez, B., Vasquez, C., Coll-Cardenas, R., & Torres-Ornelas, P. (2004). Causes of accidents in children aged 0-14 years and risk factors related to the family environment. Annals of Tropical Paediatrics, 24(1), 53-57. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med5&NEWS=N&AN=15005967 https://doi.org/10.1179/027249304225013259
- Watson, M. C., & Errington, G. (2016). Preventing unintentional injuries in children: Successful approaches. Paediatrics and Child Health, 26(5), 194–199. https://doi.org/10.1016/j.paed.2015.12.006
- Wynn, P. M., Zou, K., Young, B., Majsak-Newman, G., Hawkins, A., Kay, B., Mhizha-Murira, J., & Kendrick, D. (2016). Prevention of childhood poisoning in the home: Overview of systematic reviews and a systematic review of primary studies. International Journal of Injury Control and Safety Promotion, 23(1), 3-28. https://doi.org/10.1080/17457300.2015.1032978 (Comment in: Int J Inj Contr Saf Promot. 2016;23(1):1-2; PMID: 26753528 [ https://www.ncbi.nlm.nih.gov/pubmed/26753528])
- Yin, C., Song, Y., Tabata, Y., Ogata, H., & Hwang, G.-W. (2013). Developing and implementing a framework of participatory simulation for mobile learning using scaffolding. Educational Technology & Society, 16(2), 137–150. https://www.jstor.org/stable/10.2307/jeductechsoci.16.2.137
- Younesian, S., Mahfoozpour, S., Shad, E. G., Kariman, H., & Hatamabadi, H. R. (2016). Unintentional home injury prevention in preschool children; a study of contributing factors. Emergency, 4(2), 72–77.