Abstract
Objectives: This paper reports on the acceptability and effectiveness of the FITS (Focussed Intervention Training and Support) into Practice Programme. This intervention was scaled up from an earlier cluster randomised-controlled trial that had proven successful in significantly decreasing antipsychotic prescribing in care homes.
Method: An in depth 10-day education course in person-centred care was delivered over a three-month period, followed by six supervision sessions. Participants were care-home staff designated as Dementia Care Coaches (DCCs) responsible for implementing interventions in 1 or 2 care homes. The course and supervision was provided by educators called Dementia Practice Development Coaches (DPDCs).
Effectiveness data included monitoring antipsychotic prescriptions, goal attainment, knowledge, attitudes and implementation questionnaires. Qualitative data included case studies and reflective journals to elucidate issues of implementation.
Results: Of the 100 DCCs recruited, 66 DCCs completed the programme. Pre-post questionnaires demonstrated increased knowledge and confidence and improved attitudes to dementia. Twenty per cent of residents were prescribed antipsychotics at baseline which reduced to 14% (31% reduction) with additional dose reductions being reported alongside improved personalised goal attainment. Crucial for FITS into Practice to succeed was the allocation and protection of time for the DCC to attend training and supervision and to carry out implementation tasks in addition to their existing job role. Evaluation data showed that this was a substantial barrier to implementation in a small number of homes.
Discussion and conclusions: The FITS into practice programme was well evaluated and resulted in reduction in inappropriate anti-psychotic prescribing. Revisions to the intervention are suggested to maximise successful implementation.
Introduction
Banerjee (Citation2009) estimated that as few as 36,000 of the 180,000 people with dementia being prescribed antipsychotics in the UK were receiving any benefit from them, while inappropriate prescribing was leading to up to 1800 extra deaths each year. Anti-psychotic medication is often prescribed as a reaction to behavioural and psychological symptoms of dementia (BPSD) which are very common in dementia. Given that much of this prescribing is for people living in care homes, benefits to health can only be achieved by ensuring that care homes have the necessary skills and knowledge to deliver good quality care without excess sedation. Many BPSDs are the result of untreated delirium, untreated pain, poor nutrition and hydration, boredom, unmet emotional needs, the care provider's lack of understanding of cognitive capacity, poor communication, malignant social psychology, lack of knowledge about the person's history, and poor general care. Unless staff are skilled in this area there is a danger that staff seek to ‘manage’ behaviour through medication without really understanding why it is occurring.
Person-centred care (Brooker, Citation2012; Kitwood, Citation1997) provides a proactive means of helping care home staff to find ways of caring and supporting people with dementia without excess sedation. However, lack of skills at all levels and unsupportive cultures of care (Killett et al., Citation2014) are frequently cited as barriers to implementation. In addition, the implementation of psychosocial approaches to enable people living with dementia in care homes to connect with others and to have a good quality of life relies on a wide range of factors such as staff skills, job roles, tailored interventions, staff time and attitudes (Lawrence, Fossey, Ballard, Moniz-Cook, & Murray, Citation2012). Skills training in care homes is given high priority in many policy guidelines and reports but there is limited availability of an evidence base for training interventions. Fossey et al. (Citation2014) conducted a qualitative review which identified 170 training programmes to improve dementia care of which only four had RCT evidence of benefit for residents. There is no evidence-based process for the effective roll-out of skills based training on a national scale within the care-home sector that focusses on providing staff with the skills to care for people with dementia and complex needs.
The original FITS (Focussed Intervention Training and Support) programme (Fossey et al., Citation2006) was implemented as a research intervention to enable care home staff to deliver effective person-centred care for people with dementia. The aim was to reduce the inappropriate prescription and use of anti-psychotic medications, by providing person-centred approaches and evidence-based psycho-social interventions to support people experiencing BPSD. A cluster randomised-controlled trial demonstrated that, compared with usual care, the FITS programme reduced the prescribing of antipsychotics for people with dementia by over 40% (Fossey et al., Citation2006). Crucially, this was achieved without any increase in BPSD (Ballard et al., Citation2009). However, this original intervention was resource intensive and experimental. Therefore, the current study translated the intervention into an approach that remained true to the intention and outcomes of the original programme but that could be delivered nationally across a large number of care homes. The FITS into Practice Programme was developed as a means of achieving this. This paper reports on the experience and outcomes of this scaled up intervention that was rolled out within the UK during 2012–2014.
Methods
The FITS into practice intervention key attributes
The Dementia Practice Development Coach. Two university-based educators designated Dementia Practice Development Coaches (DPDCs) were employed to deliver an intensive nine month education and supervision programme to Dementia Care Coaches (DCCs) to enable them to safely reduce antipsychotic medication and to put in place evidence-based best practice to reduce BPSD. The person specification for the DPDC role included in-depth experience of working with people living with dementia in care homes and excellent skills in training. 2 part time (three days per week) DPDCs were employed. They received five days coaching on the FITS approach from the original authors as part of their induction.
Dementia Care Coache.The main vehicles for change within the care home were members of staff designated as DCCs. The DCCs were existing members of care home staff selected by their managers to undertake this role, with one DCC per care home. In addition, 50 care homes were included with the expectation that they could be covered by a DCC in a neighbouring home. A key requirement to becoming a DCC was a keen interest in improving well-being of residents. It was suggested that this role would be suitable for a care assistant, senior care assistant, registered nurse or activity co-ordinator. The full role specification is available from the authors.
The person undertaking this role was expected to attend training and supervision sessions and implement the learning within the care home setting between sessions. It was recommended to care homes that DCCs have dedicated time (1–2 days a week), separate from other roles and duties, to attend training sessions and implement changes in practice. In addition to the implementation of person-centred care interventions, DCCs were also responsible for supporting other staff and external healthcare professionals by sharing best practice in reviewing anti-psychotic drug prescriptions (Alzheimer's Society, Citation2011).
The FITS into Practice Education Programme. DCCs from participating homes were trained in cohorts of ten by a DPDC. The DCCs received a free-to attend, 10-day, standardised face-to-face education programme held in two-day blocks across a three-month period. Learning outcomes were based on the original programme (Fossey & James, Citation2008). The training provided DCCs with: tools to assess their home's strengths and areas for development; a framework for understanding and responding to behaviour as unmet needs (Fossey & James, Citation2008); knowledge of psycho-social interventions such as strengths-based care planning, life story work, supportive environments, meaningful activity using the Cohen-Mansfield toolbox and personalised music (Cohen-Mansfield, Citation2001); along with an understanding of learning styles and basic training skills in order to teach skills to others. Teaching material was updated to include additional content on communication strategies, the VIPS framework, (Brooker, Citation2007) and supporting family members. In addition, DPDCs supported DCCs to build confidence in promoting care practices that reduced distress and disability. They were also coached to initiate reviews of antipsychotic drug prescriptions with GPs and other healthcare professionals (Alzheimer's Society, Citation2011).
All training and supervision was directly facilitated by a DPDC in consecutive cohorts of participants at different geographic locations. DCCs were expected to put into practice new skills from the course between training days. Training was followed by a six-month supervision period in which DCCs implemented the learning fully in their own care home (and a second home if allocated). DCCs attended half-day group supervisions each month facilitated by the DPDC. Teaching and supervision sessions took place in locations to suit the participating DCCs. The focus of supervision was on critical reflection, peer support and continued implementation and improvement. DCCs were encouraged to take an active role in providing reflection, ideas, advice and support to each other. The expectation was that DCCs should attend all training days and supervision. A minimum requirement of 8/10 training days and 4/6 supervision sessions was set as the cut-off for certification of completion.
Care homes recruitment
The aim was to recruit 150 care homes across the UK with a mix of size and ownership. 100 care homes were initially included from a single large for-profit provider, with the intention that a single DCC would implement FITS across two care homes, (their existing workplace and another local home in which they did not usually work). Other care homes were recruited via national networks. Altogether 170 care homes expressed an interest. Expressions of interest were followed up by further information by e-mail and a telephone discussion. The subsequent selection of care homes was based on getting a range of provider types, having residents who were on antipsychotic medication and clustering geographical location (so that travelling to group training and supervision could be organised).
Measures
The evaluation was intended to explore not only the impact of the FITS programme on residents and DCCs but also the experience of implementing such a programme across a wide range of care homes. Quantitative and qualitative evaluation measures were used.
Residents in all participating homes. Comparisons were made pre-training and post-supervision (approximately nine months apart). This included:
total number of people with dementia, and number/type of anti-psychotic prescriptions;
a modified Goal Attainment Scaling (GAS) (Rockwood, Fay, Song, Macknight, & Gorman, Citation2006) was developed as a method to evaluate personalised outcomes. DCCs set individual goals related to residents' quality of life and selected one or more pre-specified goals linked to behavioural issues that were expected to change as part of the programme.
Experience of DCCs. The following measures were used to capture the impact and experience of the intervention:
Training evaluations after each block of training comprising a combination of Likert rating scales for: content, pace, learning methods, standard of presentation and open questions addressing expectations, possible changes, anticipated benefits and implementation difficulties.
A Role Confidence Likert Scale was developed for this project (available from authors) completed pre-training, post-training and post-supervision.
Approaches to Dementia Questionnaire (ADQ) and Dementia Knowledge Questionnaire (Macdonald & Woods, Citation2005) completed pre-training, post-training and post-supervision. The ADQ provides an overall score and two subscales to measure respondents' ‘person-centredness’ and ‘hope’ in relation to dementia care.
Adherence to Implementation Questionnaire developed for this project and available from the authors was completed by DCC's at the end of the supervision phase. This comprised Likert scales of confidence in being a DCC and percentage of implementation of learning into practice as well as open comments to contextualise ratings.
DPDC experience. The following were used to capture the experience of DPDCs throughout the programme:
In-depth, semi-structured interviews at the start and end of the programme addressing: experience of the DPDC role; training design and delivery; supervision delivery; the DCC role, impact and experiences.
Monthly reflective diaries, based on Gibbs' reflective cycle (Gibbs, Citation1988) reporting on their own experiences and gathering qualitative experiences of the groups and DCCs.
All interview and diary data were anonymised and uploaded into NVivo 10 software and analysed using inductive thematic analysis, (Braun & Clarke, Citation2013). The same researcher who conducted the interviews also undertook the analysis. Data were descriptively coded within NVivo by a single researcher.
Case studies
Fourteen care home were recruited as case studies to explore in-depth the impact and experience of FITS participation. This included semi-structured interviews with DCCs post-training and post-supervision about their experience of training and implementation of the intervention. The care home manager and other care home staff were also interviewed post-supervision. In addition case studies utilised job satisfaction (Russell et al., Citation2004) and stress (Stanton, Balzer, Smith, Parra, & Ironson, Citation2001) questionnaires completed by DCCs pre-training, post-training and post-supervision.
External steering group
In order to ensure that the intervention remained true to the original programme an external steering group consisting of the original FITS authors and the Alzheimer's Society met monthly with the evaluation and development team to guide the FITS into Practice Programme. Additional members included senior clinicians, care home management staff, family carers and inspection and regulation (Care Quality Commission) representation to ensure that the programme and its evaluation was grounded in practice.
Results
Care homes completion
In total, 106 homes were recruited with 67 (63%) completing through to the end of supervision.
The lower number than the initial 150 target was due to the substantial challenges faced by DCCs allocated to work in more than one home. In reality, only six homes were included that were a ‘second home’ covered by a DCC who primarily worked in a different care home. Homes were located throughout England (n = 54), Wales (n = 5) and Scotland (n = 8). shows the characteristics of homes by size, ownership and registration.
Table 1. Characteristics of the 67 care homes that completed.
Dementia care coaches
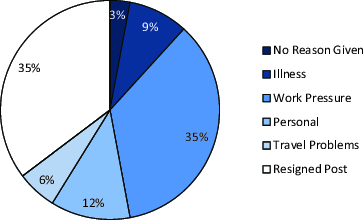
The majority of DCCs had worked with people with dementia for over five years (77%) and 56% put themselves in the 31–49 age range. summarises the numbers of participants who completed or withdrew at each phase of the programme. Two of the cohorts had significantly higher attrition rates which coincided with workload pressures exacerbated by poor communication within their organisation regarding training requirements and travel distances. Reasons for attrition are summarised in . Approximately, 65% of those who withdrew were from registered manager or deputy manager positions.
Table 2. DCC completion and attrition.
Feedback on the training and supervision
Training evaluations demonstrated an overwhelmingly positive response to the training phase of the programme. illustrates the high percentage of respondents who rated the training positively.
Table 3. Percentage of respondents rating training as 4 or 5 (on a 5-point scale where 1 is poor and 5 is good).
On each set of training days participants were asked to state what they would change about the training. In total, 92% (325/355 total responses) stated that no changes were necessary. Changes suggested mostly related to location and venue issues. When asked what barriers there would be to implementing new practice 211 responses were received across all cohorts and training days, with the most frequently (41% of responses) barrier cited as ‘lack of time’. The Role Confidence Likert Scales provided DCCs the opportunity to reflect on their work with people living with dementia pre- and post-training and post-supervision. Non-parametric statistics (sign test) demonstrated a significant positive shift in self-ratings at 95% confidence on the following items:
‘I feel wholly confident in my role with people with dementia’.
‘I feel able to explain the skills I have in working with people with dementia’.
‘I feel able to teach other people how to work with people with dementia’.
‘Other people look to me as a role model in how I work with people with dementia’.
‘Working with people living with dementia is a high status job’.
‘I feel proud of the work I do with people with dementia’.
The largest shifts occurred between pre- and post-training and were maintained or slightly improved post-supervision.
Most useful topics in training course
DCCs were asked to list the three most useful things from their FITS training that they had used. A wide variety of answers were provided, but there were common themes as summarised in
Table 4. DCC rating of most useful things from the FITS training.
Supervision sessions
No evaluations were gathered about the supervision sessions, due to their varied and participant-responsive nature. However, qualitative interview data indicated that DCCs experienced supervision positively, citing the supportive and nurturing environment created by the DPDCs and the peer support and practice sharing provided by other DCCs as important. Notably, within each cohort there was evidence of successful implementation ideas cascading between cohort members. In addition, three issues emerged which influenced recommendations for future delivery of the intervention. First, some cohorts were initially designated to have teleconference supervisions, but these were disliked and eventually rejected by DCCs. Second, the DCCs experiences of supervision prior to the FITS into Practice Programme were often in the context of line management/disciplinary experiences and thus negative. As such, supervision sessions were viewed with some caution. Both DPDCs emphasised the support aspect, re-naming them ‘support’ sessions for some later cohorts. Finally, both the DCC and DPDC interviews reflected that the length of the supervision period was too long, with most progress and implementation having been achieved by the fourth meeting.
Attitudes to residents with dementia
Fifty-one DCCs completed the ADQ showing a significant improvement overall and on subscale factors of ‘Hope’ and ‘Person-Centredness’ (see ).
Table 5. ADQ scores at different time points (n = 51 DCCs).
Knowledge of dementia
Fifty-one DCCs completed the Dementia Knowledge Questionnaire showing a significant improvement (CI = 0.05, p = –0.02) from pre-to post-training and from pre-training to post-supervision (CI = 0.05, p = –0.003).
Impact on practice
Opportunity to implement FITS into Practice
In total, 48 of 57 (84%) DCCs who completed the Adherence to Implementation Questionnaire at the end of the project, agreed or strongly agreed with the statement
I feel confident about being a dementia coach in my care home.
Antipsychotic prescribing
Data were provided by 53 homes. The main reason for data being excluded was either that homes did not provide the total number of residents with dementia in their returns (only the number on antipsychotics) or that homes did not return their forms at the end of the data collection. This was often where the DCC no longer worked at the home and no one was available to complete the submission form. Overall, the percentage of residents prescribed antipsychotics decreased from 20% at baseline (301 out of 1500 residents with dementia) to 14% (216 out of 1558 residents) following the intervention. This represents a 31% reduction in antipsychotic use (χ2= 20.4; p < 0.0001).
Antipsychotic data from the current study were re-analysed by splitting care homes in to quartiles based on the antipsychotic prescription rate at baseline. The greatest reductions were seen in homes with the highest antipsychotic use at baseline (). In 47 out of 53 care homes in the study, the percentage of residents on antipsychotic use decreased or stayed the same.
Table 6. Changes in anti-psychotic prescriptions by quartiles of lowest to highest baseline prescription rates and magnitude of change.
Goal Attainment Scaling
DCCs set individual goals related to residents' quality of life and selected one or more pre-specified goals, linked to BPSD issues. They then set the current level against the goal (score 0) and specified four levels of improvement (1–4), against which they would later rate the performance of the resident. Only goals that were rated at baseline and at least one further follow-up were included in the analysis. Completed data on personal goals were available for 76 participants and 85 participants had data on BPSD. Analysis was undertaken using a binary outcome of improvement (2, 3, 4) or no-change/worsening (0/1) in performance to avoid bias introduced by having more data points reflecting improvement. A significant benefit was seen in personal GAS goals (Pearson χ2= 0.03), but not in BPSD goals (Pearson χ2= 0.823).
Case studies
Fourteen homes initially volunteered as case studies although only ten DCCs (working in nine care homes) completed sufficient data collection. The nine care homes case studies yielded a wealth of information to be reported in a separate paper. Overall they demonstrated that the ways in which DCCs undertook implementation varied depending on their own skills and the needs of their care home. However, case studies showed a number of similar features relating to both substance and style of implementation used by DCCs. These often included:
Medication review; making contact and negotiating with prescribers regarding residents prescribed antipsychotics.
Generalised care planning review for all residents with a particular focus on behavioural analysis.
Education for fellow staff; analysing training needs and supporting development of staff skills.
Consideration of activities and meaningful interaction with residents; introduction of ‘toolboxes’, personalised music and changes in routines.
Review of use of language; role modelling and challenging of negative language use.
Overall, the vast majority of DCCs experienced FITS positively and showed improvements personally and in their care homes. However, DPDC qualitative reflections suggested that a few DCCs (<6) who encountered substantial, insurmountable, organisational barriers to implementation reported that the experience had a negative impact on their own well-being. Increased stress and frustration were reported by DCCs where they were not given time to implement FITS, particularly where they were overloaded by other organisational requirements. DCCs often had to use substantial personal resources to participate and implement FITS. DPDC reflective diaries and case study interviews identified that participation in FITS in these circumstances contributed to at least one DCC's decision to resign their post.
DPDC role
The original DPDC advert, job description and person specification is available from the authors. Two DPDCs were employed on university contracts. Qualitative data revealed five themes relating to the conduct, features and skill set of the DPDC role, which influenced recommendations for future delivery of the FITS programme.
Training design and delivery
Both DPDCs had substantial skills and experience of training, care homes and understanding of people living with dementia. This enabled them to successfully review and develop the original training manual (Fossey & James, Citation2008) and to tailor the content in response to the needs of each cohort. DCCs regularly cited through qualitative and quantitative data that the manner of training delivery was highly supportive and facilitative of implementation.
Supervision delivery
This feature sets FITS apart from other training programmes and managing this supervision role effectively is a key feature of the DPDC. The supportive challenge provided in these sessions was highlighted in the qualitative data as being influential on the implementation work of DCCs.
Relationship building with DCCs
Both DPDCs reflected that the role required special consideration of the relationships they formed with individual DCCs. Successful relationships were built on respect and trust between DPDCs and DCCs and as such required good listening skills and empathy. Crucially, this support was a way in which a person-centred approach could be role-modelled to DCCs that they could then use when challenging staff within the care homes to try innovative approaches.
Organisational negotiation
DPDCs had limited control over barriers to implementation experienced by DCCs. Consideration of how to enable future DPDCs to have influence over organisations in which DCCs are working is therefore incorporated into recommendations for future delivery of the programme.
Support needs of the DPDC role
Both DPDCs reflected that the role was a challenging one, exacerbated by the lone-working and travel required for the role within this project. This indicates that any future delivery of the FITS programme needs to consider the practical capacity of the role and thus the skills, experience and support necessary.
Discussion
The FITS into Practice Programme provides a robust way to help care homes bring about change to reduce a reliance on anti-psychotic medication for care home residents. However, change only occurred where DCCs were able to implement the approaches they learnt about. The persistence of organisational barriers to implementation within this project suggests that future delivery must raise awareness of and actively combat such barriers to ensure results are achieved from training investment. On the whole, DCCs were highly experienced in working with people living with dementia but still benefitted greatly from an in-depth person-centred training and supervision programme delivered by a skilled facilitator. There was a significant reduction in overall antipsychotic use, which was greatest in the homes that had the highest antipsychotic drug use at baseline. Interestingly the baseline use of antipsychotics (20%) was much lower than that reported by Fossey et al. (Citation2006) (42%) and actually lower than the post intervention prescription rate in the original study (23%). This likely reflects growing appreciation of the harms associated with antipsychotic use and subsequent policy drive to move away from their use (Banerjee, Citation2009; MHRA, Citation2012). In the upper quartile of homes in the current study, the reduction in antipsychotic use was very similar to that of Fossey et al. (Citation2006), suggesting that the efficacy of the scaled up intervention was similar in the two studies. From the case study data and the DPDC diaries, it would appear that the decrease in antipsychotic prescribing was initiated by the DCCs. DCCs also reported improvements in residents' functioning, including improvements in ability to communicate, increased mobility, improvements in appetite and better sleeping patterns following reduction or ceasing of antipsychotics. The majority were supported by the GPs they worked with but the change would not have occurred without being initiated by the FITS into Practice programme.
Managing and synthesising different types of data from so many different sources over time was a challenge and the results are affected by this. One of the limitations with the data collection was that changes in prescriptions were not measured (for instance changes in dose, or switching of drugs prescribed). Anecdotally the DPDCs reported many instances of DCCs working alongside prescribers to successfully bring about reductions in dosage, and PRN antipsychotics no longer being administered. These benefits may have been missed because of the way in which data were collected. A further limitation was that The Goal Attainment Scale results came from a relatively small data set (<5% of the total sample). The qualitative data were all descriptively coded by a single researcher which may have introduced bias.
In total, over a third of DCCs failed to complete the programme. In comparison with other evaluated training programmes where attrition rates of participants are reported, this rate does not appear to be unusual. In studies conducted worldwide using a variety of educational interventions for staff in residential care for people living with dementia, in which the intervention ran for two months or longer, attrition rates were reported to be 32% (Davison et al., Citation2007), 40% (Kuske et al., Citation2009) and 21% (Visser et al., Citation2008). Of those studies cited above which reported rationale for participant withdrawal, lack of time, illness and resignation were the most often cited reasons (Kuske et al., Citation2009; Visser et al., Citation2008). This would suggest that the FITS into Practice Programme did not experience unusual causes of participant withdrawal. The National Care Forum reported that turnover rates of care staff in UK residential care for older people was at 17% in 2012–2013 (National Care Forum, Citation2013). This would suggest that the percentage of staff turnover within the FITS into Practice Programme was higher than expected. However, NCF only surveyed organisations from the not-for-profit sector, whereas FITS homes included a large proportion of for-profit organisations and this could account for the discrepancy. In addition, it is possible that participating in the FITS into Practice Programme prompted DCCs to reconsider their positions and seek employment elsewhere. In one case study the DCC reported that participation in FITS prompted her to challenge the home regarding staffing levels and contributed to her decision to change jobs. She also reported that FITS participation was an advantage in securing a new post.
Throughout the programme and across cohorts, participants reported difficulties in implementing FITS due to insufficient time allocated within their working hours and workplace issues taking precedence over FITS. This was despite initial guidance when recruiting care homes and coaches that it should be considered as equivalent to a half time post. This negative impact is significant because it demonstrates that provision of training and development opportunities to staff, without adequate consideration of implementation requirements, is not only ineffectual but potentially detrimental for those staff who take part. This has implications for future delivery, as it will need to ensure that appropriate organisational planning is in place.
On the basis of the feedback and in order to maximise benefit and minimise risk the following recommendations are made:
Revisions and recommendations for the FITS into Practice Programme
The DPDC is able to provide sufficient teaching and supervision for successful implementation of the programme. Revisions have been made to the job description and person specification of the DPDC to ensure sufficient knowledge, skills and support for this role in practice whether the post is positioned within or external to the care home provider.
It is suggested that in larger care home provider organisations that the FITS into Practice Programme could be delivered by DPDCs employed directly by the care home provider organisation (suitable for a dementia lead post). In smaller provider organisations the intervention could be delivered by a suitably qualified external DPDC, acting in a consultancy or practice development role to provider organisations.
The DCC role is able to initiate and model behaviours within the staff team to successfully decrease the need for anti-psychotic prescribing and improve person-centred care, when their management and organisations are supportive of this role in practice. Revisions have been made to the job description and person specification of the DCC to help clarify this for care providers.
A structured recruitment process to the programme, including mandatory management meetings and pre-course contact between the DPDC and organisational representatives may be necessary to ensure that organisational understanding and support is adequate and the training is recognised as effective only in the context of a supportive organisational approach.
In order to pre-empt barriers to implementation, the care home manager could undertake a one-day workshop with the DPDC prior to commencement of the programme and engage with two key sessions of the training and supervision programme.
The course outline has been revised from feedback to suggest that the programme takes place across a 30-week period, with 3–4 weeks between training sessions and an interim supervision session to encourage implementation throughout the whole programme.
Feedback suggests that the main supervision period remains at the end of the programme, although this is shortened to four half-day sessions and re-named as support sessions to better reflect its purpose.
The DCC manual has been revised to include additional content essential for the adequate knowledge base and to adapt to the train-the-trainer format.
The peer support gained by DCCs participating in face-to-face training and supervision significantly contributed to the positive experience and implementation and it is recommended that a face-to-face model be retained to create a community of practice for staff.
The name ‘FITS’ should be changed to better describe both the type of role and the status of this work. This is better described as a suitably qualified DCC who has undergone a dementia care coaching course delivered and supervised by a suitably qualified DPDC. This enables the care home (and those who live there or purchase care) to feel confident that they can deliver person-centred dementia specialist care.
Finally, the FITS into Practice programme was delivered as a ‘free’ intervention. Care homes had to cover the costs of releasing staff and to change their work role to accommodate the new practice. The next stage is to work with the care homes sector and with education and training policy drivers to see how this sort of intervention could be funded more widely. As care homes cater for increasing numbers of frail older people with complex needs, the requirement for skilled care has never been greater. Finding a way of caring for people without resorting to pharmacological or physical restraint is a challenge faced by care homes worldwide. FITS into practice may seem like an intensive programme but without the investment it is difficult to see how a shift to person-centred care will occur.
Acknowledgements
This work is based on original research conducted at King's College London, in association with Oxford University, University of Newcastle and Oxford Health Foundation NHS Trust. Copyright of the original FITS manual is held by Dr Jane Fossey (Oxford Health Foundation NHS Trust) and Dr Ian James (University of Newcastle). With many thanks to the staff at the Alzheimer's Society James Pickett, Anne Corbett, Clive Ballard, Nicola Hart and Keara O'Connor: the independent Steering Group chaired by Jane Fossey that advised on the design and provided helpful comments on early drafts and included Barbara Woodward-Carlton (AS), Robin Jacoby (University of Oxford), Claire Surr (University of Bradford) and Karen Culshaw (CQC). The Biomedical Research Centre for Mental Health and the Biomedical Research Unit for Dementia at King's College London both supported the input of Clive Ballard. Finally, this programme would not have worked at all without the dementia care coaches working in care homes. Our particular thanks go to all of the care homes and dementia care coaches who showed extraordinary commitment to their work on the FITS programme and to improving the lives of all the residents in their care.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
This work was supported by a grant from the Alzheimer's Society [grant number 168] to the University of Worcester with support from the Department of Health and HC-One.
References
- Alzheimer's Society. (2011). Optimising treatment and care for behavioural and psychological symptoms of dementia. www.alzheimers.org.uk/bpsdguide
- Ballard, C., Margallo-Lana, M., O'Brien J., James, I., Howard, R., & Fossey, J. (2009). Reflections on quality of life for people with dementia living in residential and nursing home care: The impact of performance on activities of daily living, behavioral and psychological symptoms, language skills, and psychotropic drugs. International Psychogeriatrics, 21, 1026–1030.
- Banerjee, S. (2009). The use of antipsychotic medication for people with dementia: A time for action. A report for the minister of state for care services. London: Department of Health.
- Braun, V., & Clarke, V. (2013). Successful qualitative research. London: Sage.
- Brooker, D. (2007). Person-centred dementia care: Making services better. London: Jessica Kingsley Publishers.
- Brooker, D. (2012). Understanding dementia and the person behind the diagnostic label. International Journal of Person Centered Medicine, 2(1), 11–17.
- Cohen-Mansfield, J. (2001). Non-pharmacological interventions for inappropriate behaviours in dementia – a review summary and critique. American Journal of Geriatric Psychiatry, 9, 361–381.
- Davison, T., Mccabe, M., Visser, S., Hudgson, C., Buchanan, G., & George, K. (2007). Controlled trial of dementia training with a peer support group for aged care staff. International Journal of Geriatric Psychiatry, 22, 868–873.
- Fossey, J., Ballard, C., Juszczak, E., James, I., Alder, N., Jacoby, R., & Howard, R. (2006). Effect of enhanced psychosocial care on antipsychotic use in nursing home residents with severe dementia: A cluster randomised trial. British Medical Journal, 332. 756–758.
- Fossey, J., & James, I. (2008). Evidence-based approaches for improving dementia care in care homes. London: Alzheimer's Society.
- Fossey, J., Masson, S., Stafford, J., Lawrence, V., Corbett, A., & Ballard, C. (2014). The disconnect between evidence and practice: A systematic review of person-centred interventions and training manuals for care home staff working with people with dementia. International Journal of Geriatric Psychiatry, 29(8), 797–807.
- Gibbs, G. (1988). Learning by doing: A guide to teaching and learning methods. Oxford: Further Education Unit.
- Killett, A., Burns, D., Kelly, F., Brooker, D, Bowes, A., La Fontaine, J., … O'Neill, M. (2014). Digging deep: How organisational culture affects care home residents' experiences. Ageing & Society. doi: https://doi.org/10.1017/S0144686X14001111
- Kitwood, T. (1997). Dementia reconsidered: The person comes first. Buckingham: Open University Press.
- Kuske, B., Luck, T., Hanns, S., Matschinger, H., Angermeyer, M., Behrens, J., & Riedel-Heller, S. (2009). Training in dementia care: A cluster-randomized controlled trial of a training program for nursing home staff in Germany. International Psychogeriatrics, 21(2), 295–308.
- Lawrence, V., Fossey, J., Ballard, C., Moniz-Cook, E., & Murray, J. (2012). Making psychosocial interventions work: Improving quality of life for people with dementia in care homes. British Journal of Psychiatry, 201, 344–351.
- Macdonald, A., & Woods, R. (2005). Attitudes to dementia and dementia care held by nursing staff in U.K. ‘non-EMI’ care homes: What difference do they make?’. International Psychogeriatrics, 17(3), 383–391.
- MHRA. (2012). Concerns over recent years about the use of antipsychotics to treat the behavioural and psychological symptoms of dementia (BPSD). http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON152729 accessed 16/04/14
- National Care Forum. (2013). Personnel statistics survey. London: National Care Forum.
- Rockwood, K., Fay, S., Song, S., Macknight, C., & Gorman, M.C. (2006). Attainment of treatment goals by people with Alzheimer's disease receiving galantamine: A randomised controlled trial. CMAJ, 174, 1099–1105.
- Russell, S., Spitzmuller, C., Lin, L., Stanton, J., Smith, P., & Ironson, G. (2004). Shorter can also be better: The abridged job in general scale. Educational and Psychological Measurement, 64, 878–893.
- Stanton, J., Balzer, W., Smith, P., Parra, L., & Ironson, G. (2001). A general measure of work stress: The Stress in general scale. Educational and Psychological Measurement, 61, 866–888.
- Visser, S., Mccabe, M., Hudgson, C., Buchanan, G., Davison, T., & George, K. (2008). Managing behavioural symptoms of dementia: Effectiveness of staff education and peer support. Aging & Mental Health, 12(1), 47–55.