ABSTRACT
Objectives: Over the last 10 years there has been a multitude of studies of psychosocial interventions for people with dementia. However, clinical services face a dilemma about which intervention should be introduced into clinical practice because of the inconsistency in some of the findings between different studies and the differences in the study qualities and trustworthiness of evidence. There was a need to provide a comprehensive summary of the best evidence to illustrate what works.
Methods: A review of the systematic reviews of psychosocial interventions in dementia published between January 2010 and February 2016 was conducted.
Results: Twenty-two reviews (8 physical, 7 cognitive, 1 physical/cognitive and 6 other psychosocial interventions) with a total of 197 unique studies met the inclusion criteria. Both medium to longer-term multi-component exercise of moderate to high intensity, and, group cognitive stimulation consistently show benefits. There is not sufficient evidence to determine whether psychological or social interventions might improve either mood or behaviour due to the heterogeneity of the studies and interventions included in the reviews.
Conclusion: There is good evidence that multi-component exercise with sufficient intensity improves global physical and cognitive functions and activities of daily living skills. There is also good evidence that group-based cognitive stimulation improves cognitive functions, social interaction and quality of life. This synthesis also highlights the potential importance of group activities to improve social integration for people with dementia. Future research should investigate longer-term specific outcomes, consider the severity and types of dementia, and investigate mechanisms of change.
Introduction
The importance of timely psychosocial interventions to reduce disability in dementia is widely acknowledged (Prince, Bryce, & Ferri, Citation2011; WHO, Citation2015). An extensive review of nonpharmacological interventions for people with Alzheimer's disease (Olazaran et al., Citation2010) found robust evidence for the benefits of cognitive training, cognitive stimulation, activities of daily living (ADL) training, behavioural interventions, and caregiver support and training. Since this review of 2010 (Olazaran et al., Citation2010), systematic reviews evaluating psychosocial interventions for dementia have grown. However, conclusions from different reviews evaluating similar types of interventions are not always consistent and the qualities of the reviews are also varied. Furthermore, classification of various psychosocial interventions for dementia can differ between the reviews. There was a need to provide a comprehensive summary of the best evidence on the range of psychosocial interventions using explicit inclusion and exclusion criteria.
A review of systematic reviews is one way of providing a ‘high level’ understanding of the range of psychosocial interventions available. It allows comparison of findings of separate reviews and can bring together in one place a synthesis of trustworthy evidence (Smith, Devane, Begley, & Clarke, Citation2011). Reviews of systematic reviews conducted to date have evaluated a wide range of the effects of health interventions such as those for chronic illness (Ouwens, Wollersheim, Hermens, Hulscher, & Grol, Citation2005), people with dementia in care homes (Vernooij-Dassen, Vasse, Zuidema, Cohen-Mansfield, & Moyle, Citation2010), and carers of people with dementia (Dickinson et al., Citation2017). The aim of this review was to investigate the research question: which psychosocial interventions have adequate evidence to demonstrate they are able to maintain or improve wellbeing of people with dementia?
Methods
For the purpose of this review, we will define psychosocial interventions as those physical, cognitive or social activities that may maintain or improve ‘functioning, interpersonal relationships and well-being in people with dementia’ (Moniz-Cook, Vernooij-Dassen, Woods, Orrell, & INTERDEM Network, Citation2011). The term ‘psychosocial interventions’ is sometimes used synonymously with the term ‘non-pharmacological intervention’. The difficulty with using this term is that it describes what an intervention is not (non-pharmacological) but does not explain what it is. It also has a strong sense of symptom management. Interventions to improve psychological, social and everyday functional abilities of people with dementia should go beyond basic problem-management, thus the term ‘psychosocial intervention’ is used for this review.
Search strategy
The initial electronic searches on MEDLINE, PubMed, Cochrane Library, PsycINFO and EMBASE were conducted in December 2014. Two reviewers (OM, CS) conducted further electronic searches in December 2015 and February 2016 to update the list of potential reviews. Google Scholar was also used to identify additional potentially relevant reviews. Potentially eligible reviews were searched with ‘systematic review’, review, or ‘literature review’ in combination with the following search terms. Population search terms included: dement*, Alzheimer*. Intervention search terms included: psycholog*, behavio*, social, psychosocial, leisure activit*, cognit*, physical, life style. References of the potentially eligible reviews were also checked.
Inclusion criteria
We included systematic reviews on physical, cognitive, psychological or social interventions for people with dementia published in English in a peer-reviewed journal between January 2010 and February 2016. Further inclusion criteria were: (1) clear definition of interventions and components of interventions described in the review, (2) clear search strategies and explicit inclusion and exclusion criteria, and (3) statistical report on the included studies. The study participants were both from the community and the residential settings and had diagnosis of dementia.
Exclusion criteria
We excluded systematic reviews on: (1) interventions to reduce risks of dementia, (2) pharmacological interventions for dementia, (3) neurological or biological factors in dementia, (4) screening or diagnosis for dementia, (5) health service interventions (e.g. case management), (6) interventions for family and paid carers only (not including people with dementia).
Review screening and selection
Two reviewers (OM, CS) screened titles and abstracts of potentially eligible reviews. Full-text articles were obtained for the potential reviews and those that need further investigations before confirming their eligibility. Reviewer discrepancy was checked and moderated by a third reviewer (MO).
Quality assessment
The ‘assessment of multiple systematic reviews’ (AMSTAR) is an 11-item validated measurement tool to assess the methodological quality of systematic reviews (Shea et al., Citation2007; Shea et al., Citation2009). It is the recommended and commonly used quality measure for conducting a review of systematic reviews of healthcare interventions. The AMSTAR items are scored as ‘Yes’ (1 point), ‘No’ (0), ‘Can't Answer’ (0), or ‘Not Applicable’ (0). The maximum AMSTAR score is 11. Scores of 0-4 is regarded as low quality, 5-8 as medium quality, and 9-11 as high quality (Jaspers, Smeulers, Vermeulen, & Peute, Citation2011). For this review, systematic reviews of medium or high quality (AMSTAR scores 5-11) were included. Two reviewers (OM, CS) independently conducted the quality assessment of the initially included reviews. Discrepancies over AMSTAR scores were resolved by discussion.
Data analysis and synthesis
First, the characteristics of the included reviews were summarised. Second, the outcomes of the interventions were tabulated according to the domain of the effects: physical functioning, cognitive functions, mood, behaviour, ADL, social interaction and Quality of Life. Third, the effects of the interventions in each domain were examined by the experts in the field (EH, AS, GC, EMC, EC). Finally, the outcome of the expert's analysis was brought together in the discussion to contextualise the findings.
Results
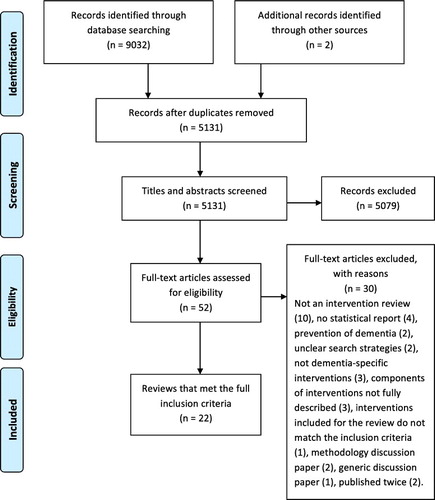
The initial electronic searches on MEDLINE, PubMed, PsycINFO, EMBASE and Cochrane Library yielded 9032 results (). Searches on Google Scholar identified 2 additional reviews. Duplicates were removed leaving 5131 articles for further evaluation. After screening review titles and abstracts, 5079 articles were removed. Full-text articles were obtained for the remaining 52 potential reviews. Thirty reviews were excluded. Reasons for exclusion were: not dementia-specific interventions (3 reviews), components of interventions not fully described (3), interventions included for the review did not match the inclusion criteria (1), unclear search strategies (2), no statistical report on the outcomes of interventions (4), prevention of dementia (2), not an intervention efficacy review (10), methodology discussion paper (2), generic discussion paper (1), and two were published twice (Aguirre, Woods, Spector, & Orrell, Citation2013; Orgeta, Qazi, Spector, & Orrell, Citation2015).
Quality assessment of the included reviews
Quality assessment of the 22 reviews that met the full inclusion criteria was conducted. Level of agreement between the two reviewers was good (k = 0.79). All the 22 reviews were of medium or high quality (AMSTAR score range 5-11) and were therefore included in this review. shows the AMSTAR scores of the 22 reviews. The mean score was 7.5. AMSTAR scores for four Cochrane reviews were 100% that is a score of 11. All reviews but one provided a priori design (AMSTAR item 1). The extent of documenting the review methods varied greatly between the reviews. Only 13 reviews explicitly stated that there were both duplicate study selection and data extraction (item 2). All the reviews conducted electronic searches but two reviews did not specify if they searched beyond electronic databases (item 3). Ten reviews conducted some degree of grey literature search and only the four Cochrane reviews and one other provided full accounts of grey literature search and publication status (item 4). Similarly, only the Cochrane reviews and one other review provided a list of excluded studies (item 5). All the reviews but one provided tables of the characteristics of the included studies, but five reviews provided only selected information (e.g. not providing sufficient demographic information) (item 6). Although all the 22 reviews referred to the scientific quality of the included studies to formulate their conclusions (item 8), four did not document the scientific quality of the included studies (item 7). Meta-analysis (item 9) was conducted in ten reviews. The rest of the reviews did not consider pooling the results was appropriate due to the heterogeneity of the interventions. Only twelve reviews assessed publication bias (item 10). Four reviews did not include conflict of interest (item 11).
Table 1. AMSTAR scores of the 22 reviews.
Characteristics of the included reviews
Eight reviews were on physical activities, seven on cognitive activities, one on combined physical and cognitive activities and six on other psychosocial interventions (). From the 22 reviews a total of 197 unique studies were identified and a total of 31 (16 physical, 13 cognitive and 2 for other psychological/social) were included more than three times across similar systematic reviews (Supplementary material). This suggests that 31 studies provide trustworthy evidence. Seven domains of intervention outcome were reported in the 22 reviews (). These were: physical outcomes, cognitive outcomes, mood, behaviour, ADL, social interaction and Quality of Life. The impact of the interventions according to these domains are summarised below. All the effect sizes reported in this section are the outcomes of meta-analyses in the individual reviews. They are not effect sizes of individual studies nor pooled results of separate reviews.
Table 2. Characteristics of included reviews.
Table 3. Effects of the interventions according to key domains.
Physical outcomes
Of the eight reviews on exercise interventions (Blankevoort, van Heuvelen, Boersma, Luning, de Jong, and Scherder (Citation2010); Burton et al., Citation2015; Farina, Rusted, & Tabet, Citation2014; Forbes, Thiessen, Blake, Forbes, & Forbes, Citation2013; Ohman, Savikko, Strandberg, & Pitkala, Citation2014; Pitkälä, Savikko, Poysti, Strandberg, & Laakkonen, Citation2013; Potter, Ellard, Rees, & Thorogood, Citation2011; Rao, Chou, Bursley, Smulofsky, & Jezequel, Citation2014) and a study on a combined treatment of exercise and cognitive stimulation (Law, Barnett, Yau, & Gray, Citation2014), that included 68 unique studies between them, five reviews investigated physical outcomes and all but one found improvements, with effect sizes that were small (d = 0.14) to large (d = 1.76). Some reported overall positive effects of exercise on walking speed (Blankevoort et al., Citation2010; Potter et al., Citation2011), balance (Potter et al., Citation2011), and reduced falls risk; whereas others did not find overall effects on the step test (Burton et al., Citation2015) and balance (Blankevoort et al., Citation2010). One review mentioned optimal benefits of multicomponent exercise of walking, stretching and other strength exercises, for a minimum of 12 weeks, 3 times a week for 45-60 min (Blankevoort et al., Citation2010). Two other reviews mentioned the importance of sufficient intensity of exercise needed for improvement (Pitkälä et al., Citation2013; Potter et al., Citation2011) but no difference was found between home-based vs. group exercises (Burton et al., Citation2015).
Cognitive outcomes
There were seven reviews on cognitive interventions (Alves, Magalhaes, Thomas, Goncalves, Petrosyan, and Sampaio (Citation2013); Bahar-Fuchs, Clare, & Woods, Citation2013; Carrion, Aymerich, Bailles, & Lopez-Bermejo, Citation2013; García-Casal, Loizeau, Csipke, Franco-Martín, Perea-Bartolomé, and Orrell (Citation2017); Huntley, Gould, Liu, Smith, & Howard, Citation2015; Spector, Orrell, & Hall, Citation2012; Woods et al., Citation2012) focusing on cognitive outcomes. Further five reviews on physical interventions (Farina et al., Citation2014; Forbes et al., Citation2013; Law et al., Citation2014; Ohman et al., Citation2014; Rao et al., Citation2014) looked at the impact of their interventions on cognitive functions. Thus, the total of 12 reviews covering a total of 87 unique studies looked at effects of the interventions on cognitive functions. The size and scope of reviews varied greatly, ranging between four to 23 RCTs. Cognitive interventions were broken down into the subcategories of cognitive stimulation, cognitive training, cognitive rehabilitation, reality orientation, combined cognitive and exercise programs, or computer-based cognitive interventions. We will use the following definitions proposed by Clare and Woods (Citation2004) and been summarised in Woods, Aguirre, Spector, and Orrell (Citation2012) to classify types of cognitive interventions: ‘Cognitive stimulation is engagement in a range of activities and discussions aimed at general enhancement of cognitive and social functioning. Cognitive training is guided practice on a set of standard tasks designed to reflect particular cognitive functions. Cognitive rehabilitation is an individualised approach where personally relevant goals are identified and the therapist works with the person and his or her family to devise strategies to address these (Woods et al., Citation2012).’.
Effects of physical interventions (30 studies): Evidence for exercise interventions on cognitive function was promising in all five reviews but substantial heterogeneity and the inclusion of poor quality studies was noted by the authors. Three reviews investigated global cognition with Mini Mental State Examination (MMSE) and reported moderate (Forbes et al., Citation2013) (d = 0.55) to large (Farina et al., Citation2014) (d = 1.12) effect sizes. Another review which did not use a meta-analysis (Ohman et al., Citation2014), showed global effects on cognition and in five of its eight studies. Combined cognitive and exercise interventions (Law et al., Citation2014) resulted in significant improvement in general cognitive function, although this review only included three RCTs.
Effects of cognitive interventions (57 studies): Cognitive stimulation was found to consistently improve cognitive function in three reviews (Huntley et al., Citation2015; Spector et al., Citation2012; Woods et al., Citation2012) (e.g. overall d = 0.41, MMSE g = 0.51, MMSE mean difference 0.64, ADAS-Cog mean difference 2.27, benefits maintained at follow-up). The effects of cognitive training, examined in five reviews (Alex Bahar-Fuchs et al., Citation2013; Alves et al., Citation2013; Carrion et al., Citation2013; Huntley et al., Citation2015; Spector et al., Citation2012), were less favourable and only one RCT of cognitive training reached statistical significance in one review (Carrion et al., Citation2013). A large review (Huntley et al., Citation2015) included evaluation of cognitive rehabilitation (two RCTs) and combined cognitive training/stimulation (seven RCTs). They found no significant improvements in general cognitive outcomes following either approach. In one review (García-Casal et al., Citation2017), a meta-analysis of four studies found computer-based cognitive rehabilitation had moderate effect (d = 0.54), and was more effective than non-computer-based cognitive rehabilitation (d = 0.56).
Mood outcomes
Nine reviews, 3 physical (Forbes et al., Citation2013; Potter et al., Citation2011; Rao et al., Citation2014), 2 cognitive (Bahar-Fuchs et al., Citation2013; García-Casal et al., Citation2017), 4 psychological/social (Leung, Orrell, & Orgeta, Citation2015; Orgeta, Qazi, Spector, & Orrell, Citation2014; Regan & Varanelli, Citation2013; Testad et al., Citation2014), reported the impact of the interventions on mood. A total of 84 unique studies evaluated mood. A total of 6 unique studies were used in both physical and social intervention reviews.
Effects of physical interventions (21 studies): One review conducted meta-analysis but no statistical significance was found in the outcomes of physical interventions on mood (Forbes et al., Citation2013).
Effects of cognitive interventions (10 studies): Computer-based cognitive interventions (García-Casal et al., Citation2017) showed a moderate effect on anxiety (d = 0.55) and depression (d = 0.47). However, the meta-analysis included only three studies (depression) and two studies (anxiety) and the analysis for depression included both cognitive rehabilitation (2 studies) and a cognitive training (1 study) therefore it is difficult to judge the effectiveness. Common (non computer-based) cognitive interventions (cognitive stimulation, cognitive training or cognitive rehabilitation) did not impact on mood.
Effects of psychological/Social interventions (59 studies): Although small effect sizes were reported (e.g. d = range -0.22 – 0.36) all the reviews on psychological and social interventions (Leung et al., Citation2015; Orgeta et al., Citation2014; Regan & Varanelli, Citation2013; Testad et al., Citation2014) concluded that it was not possible to draw a definite conclusion due to the small number of studies included. One review investigating the impact of psychological treatments for depression and anxiety (Orgeta et al., Citation2014) included a wide range of multi-modal interventions (e.g. therapeutic conversation and cognitive interventions combined). It made it difficult to identify potential effects of specific psychological and social interventions on mood. One review (Regan & Varanelli, Citation2013) suggested individual psychotherapy using the problem solving approach or CBT might improve mood in people with mild to moderate dementia and comorbid depression. Another review (Testad et al., Citation2014) indicated that group reminiscence therapy might help reduce depression.
Behaviour outcomes
Two reviews (Livingston et al., Citation2014; Testad et al., Citation2014) covering a total of 68 unique studies investigated the impact of various psychosocial interventions on the levels of agitation. Another review (Forbes et al., Citation2013) concluded that exercise interventions had no significant impact on challenging behaviour based on the outcome of one study. A review without meta-analysis (Testad et al., Citation2014) suggested individualised pleasant activities with or without social interactions reduced agitation amongst care home residents. One review (Livingston et al., Citation2014) found group activities, therapeutic touch and music-based interventions decreased agitation levels. However, evidence of long-term effects was limited. This review (Livingston et al., Citation2014) also highlighted the importance of staff training (e.g. Person Centred Care, communication skills training) to deliver effective interventions.
Activities of daily living (ADL) outcomes
Four reviews (Bahar-Fuchs et al., Citation2013; Blankevoort et al., Citation2010; Forbes et al., Citation2013; Rao et al., Citation2014) were conducted with Activities of Daily Living (ADL) as study outcomes. Three reviews (Blankevoort et al., Citation2010; Forbes et al., Citation2013; Rao et al., Citation2014) covered physical exercise as the intervention, while one review (Bahar-Fuchs et al., Citation2013) focused on cognitive interventions. A total of 15 unique studies evaluated ADL.
Effects of physical interventions (10 studies): Exercise interventions included strength training, aerobic exercise, and walking; with some element of socialising in some of them. Two out of three high-quality studies showed that physical interventions improved ADL across different stages of dementia (d = 0.68) in one review (Blankevoort et al., Citation2010). Another (Forbes et al., Citation2013) found that exercise programmes improved ADLs (d = 0.68), but warned that these findings should be interpreted with caution due to the heterogeneity within subtype and severity of dementia, and the type, duration and frequency of exercise. A review of six RCTs (Rao et al., Citation2014) concluded that the longer duration of exercise (aerobic, balance and strength) had a statistically significant moderate effect size (d = 0.80).
Effects of cognitive interventions (5 studies): Cognitive training was not associated with an improvement in ADLs (Bahar-Fuchs et al., Citation2013). Self-reported ADL scores improved in a single study on cognitive rehabilitation but the evidence was described as of ‘moderate quality’ by the review (Bahar-Fuchs et al., Citation2013) due to limitation of generalisability from one study.
Social interaction outcomes
One review on Cognitive Stimulation Therapy (Woods et al., Citation2012) included a meta-analysis on social interaction covering 4 studies and reported moderate effect size (d = 0.44).
Quality of life outcomes
A total of 25 unique studies covering a wide range of multi-modal interventions (physical, cognitive, dyadic and social interventions) evaluated Quality of Life (QoL) (Cooper et al., Citation2012; Leung et al., Citation2015; Potter et al., Citation2011; Woods et al., Citation2012). No evidence on benefits of exercise on QoL was found. Meta-analysis of four RCTs (Woods et al., Citation2012) indicated that cognitive stimulation was associated with benefit to QoL compared with no treatment. The largest effect size (d = 0.84) was found in the individually tailored activity interventions delivered by Occupational Therapists for people with dementia and family carers (Cooper et al., Citation2012). Another review (Leung et al., Citation2015) evaluated one study and concluded that structured social support group including carer training might be of benefit.
Discussion
This synthesis of systematic reviews describes the best evidence on psychosocial interventions for people with dementia. The evidence from the 22 reviews evaluating 197 studies of physical, cognitive and other psychosocial interventions suggests that specific interventions including multi-component exercise and cognitive stimulation have discernable benefits.
Physical interventions
Exercise for people with dementia improved overall: physical and cognitive functions and ADL skills, but did not show overall effects on: mood or behavioural and psychological symptoms. Multi-component exercise, including walking, stretching and other strength exercises with sufficient intensity (three times/week, 45-60 min per session for 12-16 weeks) appeared to be most beneficial (Blankevoort et al., Citation2010; Potter et al., Citation2011). No discernable difference between in-home or group-based exercises was noted. Several reviews indicated the need to consider using more specific cognitive tests (e.g. memory, executive and attention tests) in future studies (Blankevoort et al., Citation2010; Burton et al., Citation2015; Farina et al., Citation2014), and to evaluate adherence, objective improvement and type, intensity and duration of exercises (Forbes et al., Citation2013; Ohman et al., Citation2014; Pitkälä et al., Citation2013; Rao et al., Citation2014). Full benefits of physical exercise interventions are still to be explored.
Cognitive interventions
The most consistent evidence for improving cognitive function came from cognitive stimulation (Huntley et al., Citation2015; Spector et al., Citation2012; Woods et al., Citation2012). This finding has stood the test of time since this was also noted in the 2010 review (Olazaran et al., Citation2010) and an international report (Prince et al., Citation2011). Cognitive stimulation also improved quality of life (Woods et al., Citation2012). This may be linked to the fact that group cognitive stimulation encourages participants to provide their opinions and engages them in an optimal learning environment, usually with the social benefits of a group (Spector et al., Citation2012; Woods et al., Citation2012). Recent studies on cognitive interventions include Cognitive Stimulation Therapy delivered in the home setting by family carers (Orgeta et al., Citation2015). Insufficient evidence was found for the impact of cognitive training and rehabilitation on cognitive abilities (Bahar-Fuchs et al., Citation2013; Huntley et al., Citation2015; Spector et al., Citation2012), although no adverse effects were noted. Computer-based cognitive interventions, which incorporated cognitive recreation, cognitive rehabilitation, cognitive stimulation and cognitive training, showed moderate effects on cognition (García-Casal et al., Citation2017).
Other psychosocial interventions
The majority of the 22 reviews included both psychological and social components. Although some interventions were more psychologically oriented (e.g. Cognitive Behavioural Therapy) and others emphasised social elements (e.g. drop-in support group for dyads), it was often not possible to clearly differentiate components between psychological interventions and social interventions.
Three reviews that examined interventions for people with mild or moderate dementia concluded that psychological and social interventions might help improve mood (Leung et al., Citation2015; Orgeta et al., Citation2014; Regan & Varanelli, Citation2013). However, these included a wide range of studies such as modified CBT, Tai Chi, counseling, psycho-education, telephone support (Orgeta et al., Citation2014), and multimodal interventions including: exercise, CBT, educational seminars and communication skills training amongst others (Leung et al., Citation2015; Regan & Varanelli, Citation2013). Although all reviews have shown that interventions with strong social elements are beneficial, it is difficult to identify the best evidence or the mechanism of change since the components of the individual interventions have not been analysed. Furthermore, evaluation of group interventions for people with dementia and their families is complex, due to the difficulty of differentiating between the effects of a formal intervention and of social opportunities to meet other families in similar circumstances.
Two reviews specifically investigating the impact of psychosocial interventions on behavioural and psychological symptoms of dementia (Livingston et al., Citation2014; Testad et al., Citation2014) met our inclusion criteria. However, some of the interventions that have been identified as effective in reducing agitation were not fully or accurately described; for example as ‘pleasant activities’ (Testad et al., Citation2014) or as ‘music therapy’ which were music activities (Livingston et al., Citation2014). One review (Livingston et al., Citation2014) noted that staff training had an impact in reducing agitation levels and acknowledged the variability of defining agitation between the studies. Another review not included in this synthesis (Moniz-Cook et al., Citation2012) also found that functional analysis-based interventions for challenging behaviour in dementia had positive effects on not only frequency of challenging behaviour but also caregiver reaction to the behaviour. Carer perception of difficult behaviour needs to be targeted first before introducing an intervention to manage what may be considered as dementia symptoms. Changes in carer perception would also impact the delivery methods of interventions (‘how’), which are as equally important as the interventions themselves (‘what’).
Strengths and limitations
This review provides a comprehensive synthesis of high quality evidence from a wide range of interventions to meet physical, cognitive, psychological and social needs of people with dementia. The rigor of synthesis was achieved through standardised literature searches, quality assessment of the initially included reviews, detailed data extraction and experts input into reporting and analyses of the findings for each domain. A review of systematic reviews is a useful approach to develop an overview of currently available best evidence but some limitations of this approach also need to be acknowledged.
First, synthesising evidence from heterogeneous systematic reviews evaluating a wide range of interventions is a challenge. All reviews provided statistical information of the included studies but only 10 out of 24 reviews conducted meta-analysis. We did not attempt to pool the results of the systematic reviews due to the lack of information (outcomes of meta-analysis) and heterogeneity of interventions. It is difficult to compare the effectiveness of different types of interventions. Second, a systematic review does not always take the differences in the contents and the qualities of control groups into consideration. For example, even a ‘high quality’ systematic review, for example Bahar-Fuchs (Citation2013) (AMSTAR score 11/11) reports meta-analyses of the 12 RCTs with different control groups (7 active control groups, 2 wait-list control, 3 treatment as usual/no specific treatment). Analysis of the use of control groups (and absence of control groups) would have been useful for this review, but this requires examining 197 studies individually and synthesise the findings, which is beyond the scope of this review. Third, review of systematic reviews can overgeneralise evidence from individual studies, or may overlook trustworthy evidence from a high quality study. We tried to address this by identifying 31 studies that were frequently included in systematic reviews as trustworthy evidence (Supplementary material). Further exploration of these 31 studies may help articulating methodologically strong study designs and identifying the mechanism of change. Finally, there is no standardised procedure for conducting a review of systematic reviews. The term ‘review of reviews’ is not well defined. Several terms including ‘overview of reviews’, ‘umbrella review’, and ‘evidence synthesis’ are used interchangeably. The lack of methodological rigor in a review of reviews has been criticised (Pieper, Antoine, Mathes, Neugebauer, & Eikermann, Citation2014; Smith et al., Citation2011). A method for systematically extracting the most relevant information from a systematic review should be developed to produce a clinically meaningful evidence synthesis.
Implications for future research and practice
To assist clinically relevant decisions, severity and types of dementia of the study participants and their residency (community-dwelling people or care home residents) needs to be specified. The existing reviews did not provide sufficient evidence to draw a conclusion on the best psychosocial interventions for people living in different settings or those at different stages of dementia. Diagnostic-specific issues also need to be addressed more explicitly in a systematic review. Analyses of multi-component interventions should be outlined in more detail, taking into account the effects of components to identify the mechanism of change and the key active ingredients. Dismantling trial methodology may be one way to achieve this. Pooling the results of multi-components interventions without considering the impact of each intervention should be avoided.
The need for longer-term, methodologically strong studies with larger sample sizes was consistently highlighted in the 22 reviews. Furthermore, the delivery method of an intervention should be considered more carefully. The importance of training people who deliver the intervention (e.g. practitioners, volunteers or care home staff) should not be underestimated. This synthesis highlighted the lack of rigorous studies on psychological and social interventions for people with dementia with many interventions not clearly defining whether the target is psychological (emotional) support or a social intervention or psychological support to encourage a person to maintain or engage in social activity.
This synthesis of evidence covering 197 studies found that multi-component exercise including walking with sufficient intensity and group cognitive stimulation are likely to be beneficial for people with dementia. This synthesis also highlights the potential importance of social integration for people with dementia. For example, interventions to promote social interaction such as peer group activity may also be of value given that dementia can result in social exclusion for some. Further evidence for long-term effects of psychosocial interventions targeting specific outcomes is necessary to understand the mechanism of change and clinical relevance.
Disclosure of interest
Martin Orrell, Aimee Spector and Emese Csipke are authors of specific systematic reviews included in this review.
Acknowledgements
This article presents independent research funded by the Economic and Social Research Council (ESRC): ES/L001802/2. Orii McDermott received funding from Velux Foundation, Denmark.
Additional information
Funding
References
- Aguirre, E., Woods, R. T., Spector, A., & Orrell, M. (2013). Cognitive stimulation for dementia: A systematic review of the evidence of effectiveness from randomised controlled trials. Ageing Research Reviews, 12(1), 253–262.
- Alves, J., Magalhaes, R., Thomas, R. E., Goncalves, O. F., Petrosyan, A., & Sampaio, A. (2013). Is there evidence for cognitive intervention in Alzheimer disease? A systematic review of efficacy, feasibility, and cost-effectiveness. Alzheimer Disease & Associated Disorders, 27(3), 195–203.
- Bahar-Fuchs, A., Clare, L., & Woods, B. (2013). Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer's disease and vascular dementia. The Cochrane Database of Systematic Reviews, 6. Art.No.: CD003260.
- Blankevoort, C. G., van Heuvelen, M. J., Boersma, F., Luning, H., de Jong, J., & Scherder, E. J. (2010). Review of effects of physical activity on strength, balance, mobility and ADL performance in elderly subjects with dementia. Dementia and Geriatric Cognitive Disorders, 30(5), 392–402.
- Burton, E., Cavalheri, V., Adams, R., Browne, C. O., Bovery-Spencer, P., Fenton, A. M., … Hill, K. D. (2015). Effectiveness of exercise programs to reduce falls in older people with dementia living in the community: A systematic review and meta-analysis. Clinical Interventions in Aging, 10, 421.
- Carrion, C., Aymerich, M., Bailles, E., & Lopez-Bermejo, A. (2013). Cognitive psychosocial intervention in dementia: A systematic review. Dementia and Geriatric Cognitive Disorders, 36(5-6), 363–375.
- Clare, L., & Woods, R. (2004). Cognitive training and cognitive rehabilitation for people with early-stage Alzheimer's disease: A review. Neuropsychological Rehabilitation, 14(4), 385–401.
- Cooper, C., Mukadam, N., Katona, C., Lyketsos, C. G., Ames, D., Rabins, P., … Teri, L. (2012). Systematic review of the effectiveness of non-pharmacological interventions to improve quality of life of people with dementia. International Psychogeriatrics, 24(06), 856–870.
- Dickinson, C., Dow, J., Gibson, G., Hayes, L., Robalino, S., & Robinson, L. (2017). Psychosocial intervention for carers of people with dementia: What components are most effective and when? A systematic review of systematic reviews. International Psychogeriatrics, 29 (1 ), 31–43.
- Farina, N., Rusted, J., & Tabet, N. (2014). The effect of exercise interventions on cognitive outcome in Alzheimer's disease: A systematic review. International Psychogeriatrics, 26(1), 9–18.
- Forbes, D., Thiessen, E. J., Blake, C. M., Forbes, S. C., & Forbes, S. (2013). Exercise programs for people with dementia. The Cochrane Database of Systematic Reviews, 12. Art.No.: CD006489.
- García-Casal, J. A., Loizeau, A., Csipke, E., Franco-Martín, M., Perea-Bartolomé, M. V., & Orrell, M. (2017). Computer-based cognitive interventions for people living with dementia: A systematic literature review and meta-analysis. Aging & Mental Health, 21(5), 454-467.
- Huntley, J., Gould, R., Liu, K., Smith, M., & Howard, R. (2015). Do cognitive interventions improve general cognition in dementia? A meta-analysis and meta-regression. BMJ Open, 5(4), e005247.
- Jaspers, M. W., Smeulers, M., Vermeulen, H., & Peute, L. W. (2011). Effects of clinical decision-support systems on practitioner performance and patient outcomes: A synthesis of high-quality systematic review findings. Journal of the American Medical Informatics Association, 18(3), 327–334.
- Law, L. L., Barnett, F., Yau, M. K., & Gray, M. A. (2014). Effects of combined cognitive and exercise interventions on cognition in older adults with and without cognitive impairment: A systematic review. Ageing Research Reviews, 15, 61–75.
- Leung, P., Orrell, M., & Orgeta, V. (2015). Social support group interventions in people with dementia and mild cognitive impairment: A systematic review of the literature. International Journal of Geriatric Psychiatry, 30(1), 1–9.
- Livingston, G., Kelly, L., Lewis-Holmes, E., Baio, G., Morris, S., Patel, N., … Cooper, C. (2014). Non-pharmacological interventions for agitation in dementia: Systematic review of randomised controlled trials. The British Journal of Psychiatry, 205(6), 436–442.
- Moniz-Cook, E. D., Swift, K., James, I., Malouf, R., De Vugt, M., & Verhey, F. (2012). Functional analysis‐based interventions for challenging behaviour in dementia. The Cochrane Database of Systematic Reviews, 2. Art.No.: CD006929.
- Moniz-Cook, E., Vernooij-Dassen, M., Woods, B., Orrell, M., & INTERDEM Network. (2011). Psychosocial interventions in dementia care research: The INTERDEM manifesto. Aging & Mental Health, 15(3), 283–290.
- Ohman, H., Savikko, N., Strandberg, T. E., & Pitkala, K. H. (2014). Effect of physical exercise on cognitive performance in older adults with mild cognitive impairment or dementia: A systematic review. Dementia and Geriatric Cognitive Disorders, 38(5-6), 347–365.
- Olazaran, J., Reisberg, B., Clare, L., Cruz, I., Pena-Casanova, J., Del Ser, T., … Muniz, R. (2010). Nonpharmacological therapies in Alzheimer's disease: A systematic review of efficacy. Dementia and Geriatric Cognitive Disorders, 30(2), 161–178.
- Orgeta, V., Leung, P., Yates, L., Kang, S., Hoare, Z., Henderson, C., … Orrell, M. (2015). Individual cognitive stimulation therapy for dementia: A clinical effectiveness and cost-effectiveness pragmatic, multicentre, randomised controlled trial. Health Technology Assessment, 19(64), 1–108.
- Orgeta, V., Qazi, A., Spector, A. E., & Orrell, M. (2014). Psychological treatments for depression and anxiety in dementia and mild cognitive impairment. The Cochrane Database of Systematic Reviews, 1. Art.No.: CD009125.
- Orgeta, V., Qazi, A., Spector, A., & Orrell, M. (2015). Psychological treatments for depression and anxiety in dementia and mild cognitive impairment: Systematic review and meta-analysis. The British Journal of Psychiatry, 207(4), 293–298.
- Ouwens, M., Wollersheim, H., Hermens, R., Hulscher, M., & Grol, R. (2005). Integrated care programmes for chronically ill patients: A review of systematic reviews. International Journal for Quality in Health Care, 17(2), 141–146.
- Pieper, D., Antoine, S.-L., Mathes, T., Neugebauer, E. A., & Eikermann, M. (2014). Systematic review finds overlapping reviews were not mentioned in every other overview. Journal of Clinical Epidemiology, 67(4), 368–375.
- Pitkälä, K., Savikko, N., Poysti, M., Strandberg, T., & Laakkonen, M.-L. (2013). Efficacy of physical exercise intervention on mobility and physical functioning in older people with dementia: A systematic review. Experimental Gerontology, 48(1), 85–93.
- Potter, R., Ellard, D., Rees, K., & Thorogood, M. (2011). A systematic review of the effects of physical activity on physical functioning, quality of life and depression in older people with dementia. International Journal of Geriatric Psychiatry, 26(10), 1000–1011.
- Prince, M., Bryce, R., & Ferri, C. (2011). World Alzheimer report 2011: The benefits of early diagnosis and intervention. Alzheimer's Disease International. Retrieved from https://www.alz.co.uk/research/world-report-2011
- Rao, A. K., Chou, A., Bursley, B., Smulofsky, J., & Jezequel, J. (2014). Systematic review of the effects of exercise on activities of daily living in people with Alzheimer's disease. American Journal of Occupational Therapy, 68(1), 50–56.
- Regan, B., & Varanelli, L. (2013). Adjustment, depression, and anxiety in mild cognitive impairment and early dementia: A systematic review of psychological intervention studies. International Psychogeriatrics, 25(12), 1963–1984.
- Shea, B. J., Grimshaw, J. M., Wells, G. A., Boers, M., Andersson, N., Hamel, C., … Bouter, L. M. (2007). Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology, 7(1), 10.
- Shea, B. J., Hamel, C., Wells, G. A., Bouter, L. M., Kristjansson, E., Grimshaw, J., … Boers, M. (2009). AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. Journal of Clinical Epidemiology, 62(10), 1013–1020.
- Smith, V., Devane, D., Begley, C. M., & Clarke, M. (2011). Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Medical Research Methodology, 11(1), 15.
- Spector, A., Orrell, M., & Hall, L. (2012). Systematic review of neuropsychological outcomes in dementia from cognition-based psychological interventions. Dementia and Geriatric Cognitive Disorders, 34(3-4), 244–255.
- Testad, I., Corbett, A., Aarsland, D., Lexow, K. O., Fossey, J., Woods, B., & Ballard, C. (2014). The value of personalized psychosocial interventions to address behavioral and psychological symptoms in people with dementia living in care home settings: A systematic review. International Psychogeriatrics, 26(7), 1083–1098.
- Vernooij-Dassen, M., Vasse, E., Zuidema, S., Cohen-Mansfield, J., & Moyle, W. (2010). Psychosocial interventions for dementia patients in long-term care. International Psychogeriatrics, 22(07), 1121–1128.
- WHO. (2015). Dementia: A public health priority. Geneva: World Health Organization, 2012. Retrieved from http://apps.who.int/iris/bitstream/10665/75263/1/9789241564458_eng.pdf
- Woods, B., Aguirre, E., Spector, A. E., & Orrell, M. (2012). Cognitive stimulation to improve cognitive functioning in people with dementia. The Cochrane Database of Systematic Reviews, 2. Art.No.: CD005562.