The world-wide prevalence of dementia still keeps rising, keeping pace with the unabated urgency to find truly supportive strategies for all those who are affected by this condition in our society. One of the main challenges for caregivers of people with dementia (PwD) is to cope with what has been called ‘ambiguous loss’ (Boss, Citation2011; van Wijngaarden, van der Wedden, Henning, Komen, & The, Citation2018): the loss that occurs without closing or understanding of what is going on. After a period of uncertainty, a diagnosis of dementia heralds a new phase in which the dyad of PwD and caregiver constantly must adjust to the cognitive, emotional and behavioral changes that come with this condition. This phase may cause a high level of psychological distress – not only for those with a diagnosis but also for the caregiver – and can have large implications for the care process. Boots et al. have stressed the importance of acceptance as an essential prerequisite for adaptation to the ongoing changes in dyadic relationships, but particularly in the early phase of the disease there may be a lack of knowledge, difficulty in acknowledging changes and a strong focus on what is, or will be lost (Boots, Wolfs, Verhey, Kempen, & de Vugt, Citation2015). In their view, a positive reappraisal of the dyadic relationship and a revitalized perspective for the common future could initiate a psychological healing process. Mindfulness training can support this process in several ways, including a direct neuroprotective effect (Kurth, Cherbuin, & Luders, Citation2017).
Mindfulness, a non-judgmental attention to present moment experience, is a quality of awareness typically developed in an 8-week training with weekly group sessions. Training consists of meditative exercises with a shifting focus of attention (breathing, bodily sensations, arising feelings and thoughts), exchange of experiences during practice and daily homework assignments. In a recent review, preliminary but promising results were reported for mindfulness-based interventions (MBIs) to benefit the well-being of PwDs and their caregivers (Berk, Warmenhoven, van Os, & van Boxtel, Citation2018). There is substantial evidence that MBIs improve psychological well-being, presumably by positive reappraisal of moment-by-moment experience (Berk, van Boxtel, & van Os, Citation2017). This process of ‘adaptive coping’ has previously been described in the ‘mindful coping model’ (Garland, Gaylord, & Park, Citation2009) ().
Figure 1. Mindful coping model (adapted from Garland et al., Citation2009).
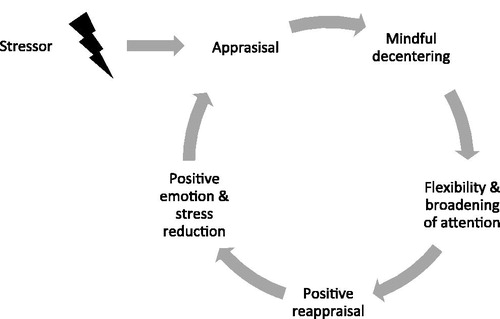
This model states that when primary appraisal of a stressful event is perceived as harmful or going beyond ones coping capacity, decentering from the source of stress into a ‘mindful mode’ may invoke more attentional flexibility and a broadening of awareness. From this perspective new meaning can be attributed to the stressful event, which may generate less defensive, more neutral or even positive emotions, including trust, confidence and compassion and can result in a different appraisal of challenging experiences in the future. On a physiological level, this process is reflected in a reduced sympathetic activation (Gross & Levenson, Citation1997). Functional imaging research recently provided us with a neurocognitive underpinning of this model, by showing that the ability to reappraise negative events is directly associated with increased activity in prefrontal brain regions that are related to cognitive control, areas which typically are compromised in older adults but also were shown to be sensitive to mindfulness training (Prakash, De Leon, Patterson, Schirda, & Janssen, Citation2014). Also other aspects of cognitive ability in older adults, including memory, verbal fluency and mental flexibility were shown to benefit from meditation practice (being a core component of mindfulness training) (Marciniak et al., Citation2014). Several mechanisms have been put forward to explain how meditation practice may influence the rate of decline in age-related cognitive function: 1) it can mitigate the effect of risk factors for cognitive decline or dementia (for example of blood cholesterol and elevated blood pressure); 2) increase regional brain perfusion; 3) provide neuroprotection via increased regional cortical thickness; and 4) reduce stress-reactivity, thereby driving back neuronal damage due to hyperactivity of the HPA-axis (Marciniak et al., Citation2014). No matter how theoretically appealing such neuroprotective action of MBIs may appear, systematic application of this protective potential in a clinical context to date still is scarce. Preliminary studies in PwDs or people with mild cognitive impairment (MCI) have shown that MBIs in such groups are feasible, but so far the evidence of slowing down cognitive decline has been inconclusive (Berk et al., Citation2017; Citation2018). In one recent controlled study (RCT) in 120 PwDs on donezepil it was found that mindfulness practice as adjuvant therapy maintained cognitive function over a period of two years, compared to muscle relaxation, cognitive stimulation therapy or care as usual (Quintana-Hernández et al., Citation2016). Given this paucity of studies, future research in this field needs to address in more detail the potential of MBI’s on cognitive decline and dementia in well-designed studies with sufficient follow-up duration.
Two systematic reviews on MBIs in caregivers of PwDs have demonstrated improvements in levels of caregiver depression and experienced burden (Collins & Kishita, Citation2018) and perceived stress levels, albeit only immediately after the training (Kor, Chien, Liu, & Lai, Citation2018). Studies in caregivers of patients with other chronic diseases, such as cancer (Li, Yuan, & Zhang, Citation2016) have shown comparable results. Two small but uncontrolled studies in which MBIs were offered to dyads (PwD and caregiver) showed that the intervention improved quality of life and supported participants in coping with their daily life demands (Berk et al., Citation2018).
Taking the dyad of patient and caregiver as a core entity for intervention can be meaningful for several reasons. Dyadic approaches in interventions for chronic disease have shown to be more effective than those that focused on patients alone (Monin & Schulz, Citation2009). Although caregivers and patients may have different perspectives, they both are in the same taxing situation and may already benefit separately from mindfulness practice (Berk et al., Citation2018). Also, providing care for a loved one with dementia can become an intrinsically positive and rewarding experience, when one is able to adapt to his or her changing role in the relationship (Yu, Cheng, & Wang, Citation2018). There are however several gaps in our current knowledge on mindfulness interventions in dyads that need to be resolved in future research (for a more detailed discussion, see (Berk et al., Citation2018). First, there still is a lack of systematic and rigorously controlled trials into the efficacy of MBIs for dyads, which ideally employ active control groups in which ingredients of the complex intervention are varied. Active control groups may help to identify which ingredient is particularly effective, which could support our understanding of the underlying mechanism. Second, the individual requirements during the training for caregivers and PwDs may differ more than is currently acknowledged. For example, optimizing training intensity and duration for the participants could promote better adherence and perpetuation of their daily practice. Also, at this point it still is unclear at which stage of the disease training will become difficult to deliver, for example due to reduced cognitive ability or disease awareness. Third, there still is insufficient knowledge about the dyadic interaction during the training process, e.g., regarding openness about stress and discomfort of caregivers when the partner is present. Finally, positive self-reports after receiving a training that emerge from qualitative interviews do not always reflect the outcome on more generic outcome scales that aim to capture concepts such as quality-of-life or mental health. Future research could benefit from (newly developed) outcome scales that better capture the essence of mindfulness practice, including factors such as equanimity and (self)compassion as intermediate states that mediate more supportive coping mechanisms. Also, scales that capture ‘acceptance’ may be of interest, as this characteristic of caregivers has been associated with challenging behavior in PwDs (de Vugt et al., Citation2004).
Mindfulness training is currently applied in almost every area of clinical practice (Hempel et al., Citation2014), and interest in its practice has a growing societal and even political momentum (Anonymous, Citation2015). To date, we only have scratched the surface of a promising paradigm that could actuate our outlook on how suffering in dementia care may be addressed in the near future. Based on the evidence so far we may only conclude that there is insufficient knowledge on how MBIs exactly bring about their effect on human behavior, or which adjustments could be beneficial to optimize the training for effective use in dyadic training. These issues need to be addressed in future research, which should take into account the large heterogeneity in the study population, use adequate (controlled) research designs – with sufficient sample sizes and follow-up duration – and focus on ecologically valid study outcomes, while staying mindful of the vulnerability of this population. When further supported by additional scientific evidence, the benefits of MBIs to improve psychological flexibility and personal well-being could prove to be of significant complementary value in providing cost-effective outpatient dementia care.
Department of Psychiatry and Neuropsychology,
Alzheimer Center Limburg, School for Mental Health and Neuroscience, Maastricht University Medical Centre, Maastricht, the Netherlands
[email protected]
Lotte Berk and Marjolein E.de Vugt
Department of Psychiatry and Neuropsychology,
Alzheimer Center Limburg, School for Mental Health and Neuroscience, Maastricht University Medical Centre, Maastricht, the Netherlands
Franca van Warmenhoven
Department of Educational Development and Research, Faculty of Health Medicine and Life Sciences,
Maastricht University, the Netherlands
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Anonymous. (2015). Mindful Nation UK (T. Loughton & J. Morden, Eds.) (p. 200). London, UK: The Mindfulness Initiative. Retrieved from www.themindfulnessinitiative.org.uk
- Berk, L., van Boxtel, M. P. J., & van Os, J. (2017). Can mindfulness-based interventions influence cognitive functioning in older adults? A review and considerations for future research. Aging and Mental Health, 21(11), 1113–1120.
- Berk, L., Warmenhoven, F., van Os, J., & van Boxtel, M. P. J. (2018). Mindfulness training for people with dementia and their caregivers: Rationale, current research, and future directions. Frontiers in Psychology, 9, 110–123.
- Boots, L. M. M., Wolfs, C. A. G., Verhey, F. R. J., Kempen, G. I. J. M., & de Vugt, M. E. (2015). Qualitative study on needs and wishes of early-stage dementia caregivers: The paradox between needing and accepting help. International Psychogeriatrics, 27(6), 927–936.
- Boss, P. (2011). Loving someone who has dementia: How to find hope while coping with stress and grief. San Francisco CA: Jossey-Bass Wiley.
- Collins, R. N., & Kishita, N. (2018). The effectiveness of mindfulness- and acceptance-based interventions for informal caregivers of people with dementia: A meta-analysis. The Gerontologist, 7, 217–270.
- de Vugt, M. E., Stevens, F., Aalten, P., Lousberg, R., Jaspers, N., Winkens, I., … Verhey, F. R. J. (2004). Do caregiver management strategies influence patient behaviour in dementia? International Journal of Geriatric Psychiatry, 19(1), 85–92.
- Garland, E., Gaylord, S., & Park, J. (2009). The role of mindfulness in positive reappraisal. EXPLORE: The Journal of Science and Healing, 5(1), 37–44.
- Gross, J. J., & Levenson, R. W. (1997). Hiding feelings: The acute effects of inhibiting negative and positive emotion. Journal of Abnormal Psychology, 106(1), 95–103.
- Hempel, S., Taylor, S. L., Marshall, N. J., Miake-Lye, I. M., Beroes, J. M., & Shanman, R. (2014). Evidence map of mindfulness. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK268640/
- Kor, P. P. K., Chien, W. T., Liu, J. Y. W., & Lai, C. K. Y. (2018). Mindfulness-based intervention for stress reduction of family caregivers of people with dementia: A systematic review and meta-analysis, Mindfulness, 9(1), 7–22.
- Kurth, F., Cherbuin, N., & Luders, E. (2017). Promising links between meditation and reduced (brain) aging: An attempt to bridge some gaps between the alleged fountain of youth and the youth of the field. Frontiers in Psychology, 8, 3244–3248.
- Li, G., Yuan, H., & Zhang, W. (2016). The effects of mindfulness-based stress reduction for family caregivers: Systematic review. Archives of Psychiatric Nursing, 30(2), 292–299.
- Marciniak, R., Sheardova, K., Cermáková, P., Hudeček, D., Sumec, R., & Hort, J. (2014). Effect of meditation on cognitive functions in context of aging and neurodegenerative diseases. Frontiers in Behavioral Neuroscience, 8, 17.
- Monin, J. K., & Schulz, R. (2009). Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging, 24(3), 681–695.
- Prakash, R. S., De Leon, A. A., Patterson, B., Schirda, B. L., & Janssen, A. L. (2014). Mindfulness and the aging brain: A proposed paradigm shift. Frontiers in Aging Neuroscience, 6, 120.
- Quintana-Hernández, D. J., Miró-Barrachina, M. T., Ibáñez-Fernández, I. J., Pino, A. S-D., Quintana-Montesdeoca, M. P., Rodríguez-de Vera, B., … Bravo-Caraduje, N., et al. (2016). Mindfulness in the maintenance of cognitive capacities in Alzheimer’s disease: A randomized clinical trial. Journal of Alzheimer’s Disease, 50(1), 217–232.
- Van Wijngaarden, E., van der Wedden, H., Henning, Z., Komen, R., & The, A.-M. (2018). Entangled in uncertainty: The experience of living with dementia from the perspective of family caregivers. PLoS One, 13(6), e0198034–e0198021.
- Yu, D. S. F., Cheng, S.-T., & Wang, J. (2018). Unravelling positive aspects of caregiving in dementia: An integrative review of research literature. International Journal of Nursing Studies, 79, 1–26.
