Abstract
Objectives: The quality of the relationship between people with dementia and their informal caregiver maybe an important determinant of life satisfaction and well-being for both members of the dyad. Taking a dyadic perspective, the aim of this study was to examine whether self- and partner-rated relationship quality influences life satisfaction and well-being for both people with dementia and their caregivers.
Design and methods: Using data from 1283 dyads in the Improving the Experience of Dementia and Enhancing Active Life (IDEAL) cohort, we examined the impact of current relationship quality on life satisfaction and well-being in dementia caregiving dyads. Data were analysed using the Actor–Partner Interdependence Model (APIM) framework.
Results: Self-rated relationship quality was associated with own life satisfaction and well-being for both people with dementia and caregivers. Partner-rated relationship quality did not influence own life satisfaction or well-being for either member of the dyad.
Conclusion: This study is the first to use the APIM framework to explore the dyadic associations between relationship quality and life satisfaction and well-being in a large cohort of dementia caregiving dyads. The obtained findings suggest that the individual perception of the quality of the caregiving relationship held by each member of the caregiving dyad is an important factor for that member’s life satisfaction and well-being, while the partner’s perception of relationship quality is not. The findings highlight the importance of considering the individual perspective of both the person with dementia and the caregiver and enabling each to maintain positive perceptions of relationship quality.
Introduction
People with dementia are often cared for by people with whom they have a pre-existing relationship, particularly spouses or adult children (Schulz & Martire, Citation2004). Dementia can alter a previous relationship between two people, as one member of the dyad adopts the role of the ‘caregiver’, who increasingly has to provide care for the other member of the dyad, changing previously established roles (Quinn, Clare, & Woods, Citation2009). Consequently, the relationship dynamics may change in unpredictable ways, and caregivers have described changes such as reduction in companionship and mutual support (Quinn, Clare, & Woods, Citation2015). Nevertheless, qualitative studies of dementia caregiving dyads have demonstrated how people with dementia and caregivers try to maintain a sense of ‘couplehood’ or ‘togetherness’ despite threats arising from the shifts in the balance of the relationship (Wadham, Simpson, Rust, & Murray, Citation2016). In turn, preserving the quality of the relationship is an important determinant of the quality of life and well-being of people with dementia (Clare, Woods, et al., Citation2014;; Woods et al., Citation2014) and their caregivers (Quinn et al., Citation2009). However, only a few studies have explored perceptions of relationship quality from the perspective of both the person with dementia and the caregiver (Clare et al., Citation2012; Spector, Orrell, Charlesworth, & Marston, Citation2016; Wright, Citation1991).
More generally, relationship quality is an important determinant of well-being for people across the adult lifespan (Bookwala, Citation2012; Litwin & Shiovitz-Ezra, Citation2006; Proulx, Helms, & Buehler, Citation2007; Walker & Luszcz, Citation2009) as well as when the partners form a caregiving/care receiving dyad (Hellström, Nolan, & Lundh, Citation2007; Wadham et al., Citation2016). For example, older couples who have a positive marital relationship have better psychological well-being, whilst a negative relationship may result in poorer mental health (Walker & Luszcz, Citation2009), and for older married couples, relationship satisfaction is significantly associated with own life satisfaction and well-being (Carr, Freedman, Cornman, & Schwarz, Citation2014). The transformation of a relationship into a caregiving one may alter perceptions of relationship quality and subsequently impact on well-being. Equity theory may offer one explanation for how relationship quality may link to well-being in caregiving dyads (Hinde, Citation1997; Kulik, Citation2002). Equity theory proposes that dyads strive to maintain balance between help given and help received, and that imbalance leads to distress for both dyad members, while a more equitable relationship is linked with greater marital or relationship satisfaction (Kulik, Citation2002). For example, McPherson and colleagues (McPherson, Wilson, Chyurlia, & Leclerc, Citation2011) demonstrated that imbalance in terms of give and take in the relationship led to greater caregiver burden in comparison with dyads who viewed the relationship as more balanced or equal.
The present study focuses on perceived relationship quality from the perspectives of both the person with dementia and the caregiver. Traditionally studies that have explored the association between relationship quality and well-being have focused solely on the perspective of the caregiver or the person with dementia, with relatively few studies eliciting the view of the person with dementia or including both perspectives (Clare et al., Citation2012; Spector et al., Citation2016). A review by Quinn et al. (Citation2009) found that the quality of the relationship between the caregiver and person with dementia could have an impact on the well-being of the caregiver. With regards to the perspective of people with dementia, a more recent review by Martyr et al. (Citation2018) reported that better relationship quality is associated with higher quality of life in people with dementia. Some studies have explored the reciprocal influence of relationship quality. For example, Woods et al. (Citation2014) demonstrated that higher perceived relationship quality among caregivers was positively correlated with better ratings of quality of life by people with dementia. However, the study only focused on factors associated with quality of life in people with dementia and did not consider factors linked to caregiver quality of life. Further, higher ratings of relationship closeness by spousal caregivers are associated with slower rates of functional and cognitive decline in people with Alzheimer’s disease (Norton et al., Citation2009), and where people with dementia report negative interactions with caregivers, this is predictive of poorer self-ratings of quality of life for people with dementia (Menne, Judge, & Whitlatch, Citation2009). This same study found that self-rated quality of life was not associated with positive dyadic interactions or the level of communication between the person with dementia and caregiver.
Perceptions of relationship quality may be influenced by many factors. Characteristics of the person with dementia or the caregiver, such as gender or kin-relationship, can influence perceptions (Quinn et al., Citation2009). In one study caregiver ratings indicated better relationship quality where care-recipients were older, female, and less educated, and had lower levels of behavioural disturbance (Spruytte et al., Citation2002). Further, better relationship quality was reported by children/children-in-law in comparison with spousal/partner caregivers. In a study of married dyads, higher relationship quality was associated with fewer depressive symptoms for the people with dementia, whilst for the caregivers, higher levels of caregiver stress and perceptions of greater extent, severity and impact of neuropsychiatric symptoms in the person with dementia were associated with poorer relationship quality (Clare et al., Citation2012).
To the best of our knowledge, no study has explored the dyadic association between relationship quality and life satisfaction and well-being, in a large cohort of dementia caregiving dyads. Additionally, our sample is significantly larger than has been used in previous studies of relationship quality in dementia caregiving dyads. Further, the study considers the dyadic association between relationship quality and two outcomes, life satisfaction and well-being, and the implications for differences in relationship quality are explored. Prior studies that have considered the perspectives of both members of the caregiving dyad have predominantly focused on factors influencing relationship quality, rather than overall implications for well-being (Clare et al., Citation2012; Spector et al., Citation2016; Wright, Citation1991). Only a few studies have explored the influence of the caregiver ratings of relationship quality on outcomes for the person with dementia or vice versa (Burgener & Twigg, Citation2002; Clare et al., Citation2012; Woods et al., Citation2014). Further, these studies did not examine the dyadic influence of relationship quality rated by both the person with dementia and the caregiver alongside outcomes for both members of the dyad. In addition, no study has included measures of well-being or life satisfaction, which can also serve as important indices of the capability to ‘live well’ as a person with dementia or as a caregiver.
The aim of the current study is to examine the impact of current relationship quality on life satisfaction and well-being in a large community-based sample of caregiving dyads. Firstly, it examines how relationship quality as rated by people with dementia impacts on their own and their respective caregivers’ life satisfaction and well-being. Secondly, it mirrors this investigation by simultaneously exploring the association of caregivers’ ratings of relationship quality with both their own life satisfaction and well-being and that of the person with dementia.
Design and methods
Design and sample
This study analysed data from people with dementia and caregivers who took part in the first wave (2014–2016) of the Improving the experience of Dementia and Enhancing Active Life (IDEAL) cohort study (Clare, Nelis, et al., Citation2014). The aim of the IDEAL programme is to investigate how social and psychological capitals, assets and resources influence the possibility of living well with dementia and to identify changes that could result in improved well-being, life satisfaction and quality of life. Participants with dementia and their respective caregivers were recruited through 29 National Health Service (NHS) sites throughout England, Scotland and Wales. The inclusion criteria required the people with dementia to have a clinical diagnosis of dementia (any sub-type), which was in the mild to moderate stages as indicated by a Mini-Mental State Examination (Folstein, Folstein, & McHugh, Citation1975) score of 15 or over, and to be living in the community at the time of enrolment. Participants were interviewed in their own homes and completed structured interviews at one-year intervals. In total 1547 people with dementia agreed to take part in the IDEAL study. Out of these, 1283 had caregivers who could participate as well, forming the dyads for the present analysis, giving a total number of 2566 individual participants. The analyses are based on version 2.0 of the IDEAL time 1 dataset.
The IDEAL study was approved by the Wales Research Ethics Committee 5 (reference 13/WA/0405), the Scotland A Research Ethics Committee (reference 14/SS/0010) and the Ethics Committee of the School of Psychology, Bangor University (reference 2014 – 11684). The IDEAL study is registered with UKCRN, registration number 16593.
Measures
Current relationship quality
Current perceived relationship quality was assessed using the Positive Affect Index (PAI; Bengston & Schrader, Citation1982). The PAI assesses the extent of positive affect that the respondent has for another person, with five questions addressing communication quality, closeness, similarity of views on life, engagement in joint activities and overall relationship quality. An example of an item is ‘taking everything into consideration, how close do you feel in your relationship with your friend/relative?’. Each item is rated on a six-point scale and responses were summed for a total score. Possible scores range from 5 to 30 with higher scores indicating better relationship quality (Cronbach’s α = 0.80 for people with dementia and 0.83 for caregivers). It has previously been used as a measure of relationship quality in studies of caregivers and people with dementia where it has shown good reliability (e.g. Clare et al., Citation2012; Quinn, Clare, McGuinness, & Woods, Citation2012; Woods et al., Citation2014). The measure was self-completed by both the person with dementia and caregiver, therefore providing information on how both members of the dyad perceive the current quality of their relationship.
Life satisfaction
Life satisfaction in both the people with dementia and the caregivers was measured with the Satisfaction with Life Scale (Diener, Emmons, Larsen, & Griffin, Citation1985). It includes five positively worded statements rated on a seven-point scale from ‘strongly disagree’ to ‘strongly agree.’ An example of a statement is ‘in most ways my life is close to my ideal’. Possible scores ranged from 5 to 35, with higher scores indicating greater satisfaction with life (Cronbach’s α = 0.81 for people with dementia and 0.88 for caregivers).
Well-being
Well-being in both members of the dyad was measured using the World Health Organization-Five Well-Being Index (WHO-5; Bech, Citation2004). Participants were asked how much of the time over the past two weeks they had felt ‘cheerful and good spirits,’ ‘calm and relaxed,’ and ‘active and vigorous’ and how often they ‘woke up feeling fresh and rested’ or found their ‘daily life has been filled with things that interest me.’ Each item is rated on a six-point scale from 0 (at no time) to 5 (all the time) (Cronbach’s α = 0.79 for people with dementia and 0.86 for caregivers). The raw score is transformed into a percentage score where a higher score indicates better well-being.
Covariates
Demographic information was collected covering age, sex and education, based on highest qualification achieved (no qualifications, school leaving certificate at age 16, school leaving certificate at age 18, university) for both members of the dyad. Caregiver kin-relationship to the person with dementia was recorded and was subsequently categorised as spouse or partner/other family member or friend. Only twelve caregivers were friends of the person with dementia; due to the small number these were included in the category with other family members. In addition, the specific dementia diagnosis of the person with dementia and time since diagnosis was collected at first interview.
Neuropsychiatric symptoms among the people with dementia were rated by the caregiver using the Neuropsychiatric Inventory Questionnaire (NPI-Q) (Kaufer et al., Citation2000). The total number of symptoms was summed with possible responses ranging from 0 (no symptoms present) to 12 (all behavioural symptoms present). Depressive symptoms were self-rated by the people with dementia using the 10-item Geriatric Depression Scale (GDS-10; Almeida & Almeida, Citation1999), with higher total scores indicating greater depressive symptoms. Caregiver depressive symptoms were self-rated using the 20-item Center for Epidemiologic Studies Depression Scale-Revised (CESD-R) (Eaton, Muntaner, Smith, Tien, & Ybarra, Citation2004). Possible scores range from 0 to 60, with a higher score indicating greater depressive symptoms. Caregiver stress was rated using the Relatives Stress Scale, a 15-item measure assessing the degree of distress and social upset experienced by a relative as the result of caring for a person with physical and/or behavioural difficulties (Greene, Smith, Gardiner, & Timbury, Citation1982). Scores ranged from 0 to 60, with a higher score indicating more severe caregiving stress.
Analytic strategy
Data were analysed using structural equation modelling (SEM). Models estimated actor and partner effects of relationship quality using the Actor–Partner Interdependence Model (APIM) framework (Kenny, Kashy, & Cook, Citation2006; Kenny & Cook, Citation1999). APIM enabled us to test for the influence of relationship quality as reported by both partners on their own life satisfaction and well-being and that of the other member of the dyad. The influence of independent variables or predictors (in this case, relationship quality) on an individual’s own outcomes (life satisfaction and well-being) is referred to as the actor effect and the influence of these predictors on the partner’s outcome is known as the partner effect, as illustrated in . APIM has predominantly been used in areas of family and developmental research to explore interdependence in close relationships (Cook & Kenny, Citation2005).
Figure 1 a. Path diagram of the Actor–Partner Interdependence Model (APIM) with dyadic relationship quality predictors of life satisfaction.
b. Path diagram of the Actor–Partner Interdependence Model (APIM) with dyadic relationship quality predictors of well-being.
Note: PwD = person with dementia
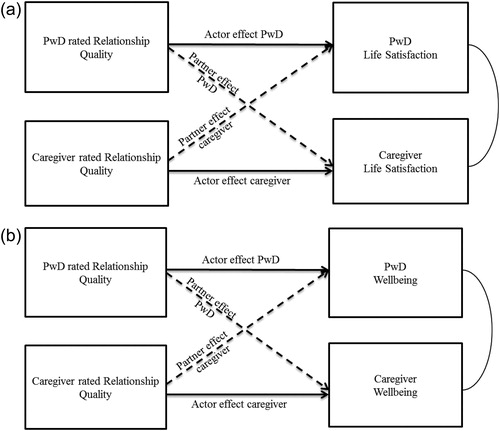
Person with dementia and caregiver life satisfaction and well-being were endogenous variables and relationship quality, rated by both members of the dyad, was an exogenous variable. The first model tested the actor (i.e. own) and partner effects of relationship quality on life satisfaction and well-being. In the second model, socio-demographic characteristics (age, sex, education and kin-relationship), dementia sub-type and time since diagnosis were accounted for. In the third model, either depressive symptoms (GDS-10) and neuropsychiatric symptoms (for people with dementia) or depressive symptoms (CESD-R) and caregiver stress (for caregivers) were added as predictors of own life satisfaction and well-being. The final (fourth) model presents the effect of actor and partner relationship quality on person with dementia and caregiver life satisfaction and well-being with age, sex, education (actor effects), kin-relationship, dementia sub-type, depressive symptoms, neuropsychiatric symptoms and caregiver stress (predictors of both partners’ life satisfaction and well-being) serving as covariates. In order to account for missing data, maximum likelihood with missing values estimation method was applied during dyadic analyses. All data were analysed using Stata 14.2 (TX: StataCorp LP).
Results
sets out the sample characteristics of the 1,283 dyads who took part in the first wave of IDEAL. The mean age of the people with dementia was 76.2 (SD = 8.2), with a higher proportion aged 80 and over (37.6%) compared to 16.8% of caregivers, and over half had a diagnosis of Alzheimer’s disease (55.7%), followed by mixed dementia (20.5%). A higher proportion of caregivers were female (68.7%) in comparison to people with dementia (41.2%). The average age of caregivers was 69.1 (SD = 11.1) and the majority were spouses or partners of the people with dementia (81.0%). The mean relationship quality score for the people with dementia was 25.0 (SD = 3.6) whilst for caregivers it was 23.2 (SD = 4.7). Caregivers reported lower relationship quality in comparison with the people with dementia (p < 0.001). People with dementia reported higher levels of both life satisfaction and well-being in comparison with caregivers (both p < 0.001).
Table 1. Descriptive characteristics of the participants with dementia and caregivers (N = 1283).
Quality of the dyadic relationship and life satisfaction
The results of the APIM analyses for relationship quality and life satisfaction are set out in . In model 1, where we adjusted for both actor and partner rated relationship quality, we observed only an actor effect between relationship quality and life satisfaction for both members of the dyad. The inclusion of socio-demographic factors had a limited effect on the association between relationship quality and life satisfaction (Model 2). The addition of further actor measures (Model 3) reduced the coefficients for the association between relationship quality and life satisfaction for people with dementia to 0.31 (95% CI 0.23, 0.39) and for the association between relationship quality and life satisfaction for caregivers to 0.27 (95% CI 0.20, 0.35). In the final model (Model 4) the actor effects of relationship quality on life satisfaction were reduced but remained significant, indicating that higher self-rated relationship quality was linked with better life satisfaction. The partner effect of relationship quality remained similar. Non-spousal dyads were more likely to report better caregiver life satisfaction and poorer person with dementia life satisfaction than spousal dyads (Supplementary material, ).
Table 2. APIM of the association between relationship quality and life satisfaction using maximum likelihood to account for missing variables (N = 1283 dyads).
Quality of the dyadic relationship and well-being
The results of the dyadic analyses for relationship quality and well-being are set out in . For both the people with dementia and caregivers there was a significant association between own (actor) assessments of relationship quality and own well-being (1.52, 95% CI 1.19, 1.84 and 1.52, 95% CI 1.28, 1.75, model 1), indicating that better relationship quality was related to improved well-being. As was the case for life satisfaction, we did not find evidence of an association between partner-rated relationship quality and own well-being. The addition of socio-demographic factors (Model 2) had a limited impact on the association between actor-rated relationship quality and own well-being. For the people with dementia, adjustment for own depressive and neuropsychiatric symptoms reduced the effect of self-rated relationship quality on own well-being to 0.62 (95% 0.35, 0.89, Model 3). In the final model, relationship quality rated by the person with dementia remained a significant predictor of own well-being (0.61, 95% CI 0.34, 0.88, Model 4). For caregivers, the addition of caregiver stress and depressive symptoms (Model 3) substantially reduced the association by around 72% to 0.41 (95% CI 0.20, 0.61). In the final model (Model 4), the actor effects of relationship quality on own well-being changed little (0.40, 95% CI 0.20, 0.61). Non-spousal caregivers were more likely to report better caregiver well-being than spousal caregivers (Supplementary material, ).
Table 3. APIM of the association between relationship quality and well-being using maximum likelihood to account for missing variables (N = 1283 dyads).
Discussion
The aim of this study was to examine how current relationship quality impacts on life satisfaction and well-being, and how the perceptions of each member of the dyad impact on the experience of the other. To the best of our knowledge, this is one of the few studies to take a dyadic perspective in examining the links between relationship quality, life satisfaction and well-being in caregiving dyads and this is the only large sample study. Perceptions of current relationship quality had a significant effect on own life satisfaction and well-being for each member of the dyad (an actor effect) but had no significant impact on the well-being and life satisfaction of the other member of the dyad (a partner effect). This highlights the importance of considering the individual perspective of both the person with dementia and the caregiver and enabling each to maintain positive perceptions of relationship quality.
Our results indicate that better perceived relationship quality may serve as a protective factor as it was linked to greater life satisfaction and well-being. However, the transition of a relationship to a caregiving/care-recipient one may challenge previously established roles and affect the existing balance in the relationship. Perceptions of current relationship quality may be subject to change and may be influenced by factors such as behavioural symptoms, depression and caregiving stress. We observed that depressive and neuropsychiatric symptoms for the people with dementia, and caregiving stress and depressive symptoms for the caregivers, significantly reduced the observed associations between self-rated relationship quality and own life satisfaction and well-being.
Our finding that perceived relationship quality did not have a significant effect on the well-being and life satisfaction of the other member of the dyad differs from some of the previous dementia caregiving literature which has indicated that partner-rated relationship quality is related to own well-being or quality of life (e.g. Burgener & Twigg, Citation2002; Clare et al., Citation2012; Woods et al., Citation2014) or that quality of life of people with dementia is related to caregiver ratings of relationship quality (Spector et al., Citation2016). It should be noted that these studies used different analytic methods, and did not use a dyadic model which simultaneously accounted for the perceptions held by both people with dementia and caregivers of the quality of the relationship and the implications for the life satisfaction and well-being of each member of the dyad. The APIM method considers the interdependence between dyad members as well as the extent to which our own relationship quality ratings may affect life satisfaction and well-being.
Our results are in line with some previous studies exploring actor and partner effects of marital relationship quality on life satisfaction and subjective well-being. For example, one study found limited evidence of partner effects of spouse-rated marital quality on own well-being in older people (Carr et al., Citation2014). One possible explanation for this finding is that older people may ignore problems with partners because the relationship is an important source of emotional closeness (Carr et al., Citation2014; Luong, Charles, & Fingerman, Citation2011). Similarly, a study examining the relationship between marital satisfaction and depressive symptoms in patients with end-stage renal disease and their spouses observed no cross-partner effects of spouse rated marital satisfaction on depressive symptoms (Pruchno, Wilson-Genderson, & Cartwright, Citation2009). However, partner effects were observed in the opposite direction (i.e. spouse depressive symptoms affected the marital satisfaction of the patient). A study of male heart disease patients and their partners observed only actor effects of greater marital satisfaction on depression during the acute phase (Dekel et al., Citation2014); however, during the chronic phase of the disease, both actor and partner effects were significant, indicating that observed results may be subject to change as different challenges arise. Adjusting to challenges may lead to a change in the balance of the relationship between the person with dementia and caregiver as the condition progresses and thus place greater strain on the quality of the relationship (Wadham et al., Citation2016).
Socio-demographic factors explained little of the association between relationship quality and life satisfaction and well-being for both members of the dyad. In the final fully-adjusted models, the results for socio-demographic factors were mixed. There was some indication that older age was associated with poorer life satisfaction and well-being for people with dementia but not for caregivers, whilst female sex and lower levels of education were associated with poorer well-being for caregivers only. This is consistent with findings from recent systematic reviews, which have found limited evidence for an impact of demographic characteristics on the quality of life of people with dementia and caregivers (Farina et al., Citation2017; Martyr et al., Citation2018).
For the people with dementia, depressive and neuropsychiatric symptoms explained most of the observed association between self-rated relationship quality and both life satisfaction and well-being. Previous research has indicated that greater informant-rated behavioural symptoms are associated with poorer relationship quality for people with dementia and caregivers (Spector et al., Citation2016; Spruytte et al., Citation2002), whilst Clare and colleagues (2012) demonstrated a link between increased depressive symptoms and lower perceived relationship quality for people with dementia.
For caregivers, the inclusion of caregiving stress and depressive symptoms substantially reduced the associations between self-rated relationship quality and their own life satisfaction and well-being. Consistent with previous literature, increased levels of caregiving stress (Alspaugh, Stephens, Townsend, Zarit, & Greene, Citation1999; Pinquart & Sörensen, Citation2004) and depressive symptoms (Schulz, O'Brien, Bookwala, & Fleissner, Citation1995) were linked with poorer caregiver well-being. In turn such factors have also been shown to relate to caregiver ratings of relationship quality (Clare et al., Citation2012; Spector et al., Citation2016) and vice-versa (Fauth et al., Citation2012). Equity theory indicates that a perceived imbalance in the relationship may lead to increased stress (Kulik, Citation2002). There was some evidence to suggest that the mood of the person with dementia affects the caregiver but not the other way round, which has been observed previously (Spector et al., Citation2016; Waite, Bebbington, Skelton-Robinson, & Orrell, Citation2004).
Overall participants with dementia rated the quality of their relationship higher in comparison with their caregivers, which is in accordance with previous studies of relationship quality (Clare et al., Citation2012; Wright, Citation1991). One explanation is that people with dementia may be basing their relationship quality ratings on previous knowledge of the relationship (Morris & Mograbi, Citation2013). This may also partly explain why previous studies have found that relationship quality ratings for caregivers decline over time but not for people with dementia. We found some evidence to suggest that the association between relationship quality, life satisfaction and well-being differed for family or friends in comparison with spouses or partners. For example, a previous meta-analysis demonstrated that spousal caregivers of people with dementia or frail older people are more likely to report depressive symptoms in comparison with adult children or children-in-law serving as caregivers (Pinquart & Sörensen, Citation2011). This difference influenced the relationship between the caregiver and care-recipient. This could suggest that the quality of the caregiving relationship may have different meanings according to the nature of the previous relationship. It will therefore be of importance to examine these relationships longitudinally to learn how the quality of the relationship changes as dementia progresses.
There are several limitations. Firstly, it is not possible to establish causal relationships in this cross-sectional study. Future research using longitudinal data would enable changes in current relationship quality and how this affects well-being and life satisfaction to be observed as dementia progresses. It is plausible that perceived changes to relationship quality over time may have a greater impact on well-being and life satisfaction. It would also enable the direction of the association between relationship quality and life-satisfaction and well-being to be explored further. Previous studies have indicated that caregiver-rated relationship quality or closeness may change or worsen over time impacting on caregiver well-being (Fauth et al., Citation2012) although there is more limited evidence of change from the perspective of people with dementia (Ablitt, Jones, & Muers, Citation2009; Clare et al., Citation2012). Further, as our sample includes only people with mild-to-moderate dementia, the observed associations may differ for people with more advanced dementia and their caregivers. Additionally, as we had a smaller proportion of non-spousal caregivers, we did not distinguish son or daughter caregivers from other family or friends as there was not enough statistical power to examine the differences between these groups. Kin relationship and gender composition of caregiving dyads may play a role and should be explored longitudinally. Similarly, there may be factors relating to existing family or relationship dynamics, not controlled for here, which may influence the quality of the relationship between the person of with dementia and caregiver and which could be considered in future research (Choi & Marks, Citation2006; Walker & Luszcz, Citation2009).
However, to the best of our knowledge this study has used a larger cohort of people with dementia and caregivers than any previous studies investigating relationship quality in caregiving dyads. Further, we have incorporated the perspective of both the person with dementia and the caregiver, and examined how partner effects may influence life satisfaction and well-being. Our study highlights the importance of integrating the perspectives of both people with dementia and caregivers, and supports calls for taking a dyadic perspective.
The APIM framework used has been developing over the last decade and a half and it has predominantly been used in areas of family psychology and developmental research (Cook & Kenny, Citation2005). There have been few studies exploring actor and partner effects of marital quality, and the results of these have been inconclusive or mixed (Bookwala, Citation2012; Carr et al., Citation2014). In studies of dementia care, the few existing studies to have used this method have predominantly focused on dyadic coping (e.g. Gellert et al., Citation2018), where some partner effects have been observed. However, one of the strengths of this analytical method is that it accounts for the interdependence in the relationship between people with dementia and the caregivers and it enables the relative size of actor and partner effects to be directly tested (Kenny & Cook, Citation1999). Standard statistical methods, such as multiple regression, treat the scores from two linked individuals as if they are independent observations, whilst this framework takes into account the interdependency of the observed scores (Kenny & Cook, Citation1999). The method we have used takes advantage of the IDEAL study design, where data from both the people with dementia and the caregiver are collected, enabling us to explore interdependency and test dyadic effects.
Implications
The present study provides further evidence that relationship quality impacts on the life satisfaction and well-being of people with dementia and their caregivers. If both members of the dyad have a positive view of relationship quality, this can help support their own life satisfaction and well-being. Interventions or strategies that aim to preserve a sense of togetherness following a shift in the balance of the relationship or to maintain the involvement of both members of the dyad may be beneficial (Hellström et al., Citation2007; Wadham et al., Citation2016). Such strategies would need to be tailored to take account of the nature of the relationship between the person with dementia and the caregiver. Spouses or partners may have different needs or issues to caregivers who are children or other family members (Pinquart & Sörensen, Citation2011). Further, as factors such as behavioural symptoms, depression and stress have been shown to predict relationship quality as well as life satisfaction and well-being, support strategies should also take these factors into consideration (Clare et al., Citation2012; Spruytte et al., Citation2002). There is some evidence to suggest that multi-component interventions aimed at caregivers and dyads may be effective in improving quality of life and reducing depressive symptoms of caregivers, along with behavioural and depressive symptoms in people with dementia (Laver, Milte, Dyer, & Crotty, Citation2017).
Our findings indicate that the individual perception of the quality of the caregiving relationship held by each member of the caregiving dyad is an important factor for that member’s life satisfaction and well-being, while the partner’s perception of relationship quality is not. This has implications for practitioners, highlighting the importance of considering the individual viewpoints of people with dementia and their caregivers and not making assumptions based on the perspective of one member of the dyad. For example, we should not rely only on the caregiver for information about how the person with dementia perceives the quality of the relationship or his/her own ability to live well, but rather we should consider the individual experience of both the person with dementia and the caregiver within the context of the dyadic relationship.
Conclusions
This study has demonstrated that the quality of the relationship between people with dementia and their caregivers is an important factor for life satisfaction and well-being for both partners. It has indicated that self-ratings of relationship quality are associated with own life satisfaction and well-being for both people dementia and caregivers, but that the perceptions of relationship quality held by each member of the dyad did not affect life satisfaction and well-being for the other. These associations remained following adjustment for caregiving stress, depressive and neuropsychiatric symptoms. The findings highlight the importance of considering the perspective of both members of the dementia caregiving dyad in future research and of maintaining positive relationship quality for people with dementia and caregivers.
Supplemental Material
Download MS Word (49.6 KB)Acknowledgements
We would like to acknowledge the support of the following research networks: NIHR Dementias and neurodegeneration specialty (DeNDRoN) in England, the Scottish Dementia Clinical Research Network (SDCRN) and Health and Care Research Wales. We are grateful to the IDEAL study participants for their participation in the study and to members of the ALWAYs group and the Project Advisory Group for their support throughout the study. We would also like to thank Prof Fiona Matthews and Dr Yu-Tzu Wu for their statistical advice.
Disclosure statement
None declared.
Data availability statement
The IDEAL data will be deposited with the UK Data Archive upon completion of the study in March 2020. Details on how the data can be accessed after this date will be made available on the project website www.idealproject.org.uk
Additional information
Funding
References
- Ablitt, A., Jones, G. V., & Muers, J. (2009). Living with dementia: A systematic review of the influence of relationship factors. Aging & Mental Health, 13(4), 497–511. https://doi.org/10.1080/13607860902774436
- Almeida, O. P., & Almeida, S. A. (1999). Short versions of the geriatric depression scale: A study of their validity for the diagnosis of a major depressive episode according to ICD‐10 and DSM‐IV. International Journal of Geriatric Psychiatry, 14(10), 858–865. https://doi.org/10.1002/(SICI)1099-1166(199910)14:10<858::AID-GPS35>3.0.CO;2-8
- Alspaugh, M. E. L., Stephens, M. A. P., Townsend, A. L., Zarit, S. H., & Greene, R. (1999). Longitudinal patterns of risk for depression in dementia caregivers: Objective and subjective primary stress as predictors. Psychology and Aging, 14(1), 34–43. https://doi.org/10.1037/0882-7974.14.1.34
- Bech, P. (2004). Measuring the dimensions of psychological well-being by the WHO-5. QoL Newsletter, 32, 15–16.
- Bengston, V. L., & Schrader, S. S. (1982). Parent-child relationship. In D. J. Mangon & W. A. Peterson (Eds.), Research instruments in social gerontology: Social roles and social participation (Vol. 2, pp. 115–185). Minneapolis: University of Minnesota Press.
- Bookwala, J. (2012). Marriage and other partnered relationships in middle and late adulthood. In R. Blieszner & V. H. Bedford (Eds.), Handbook of aging and the family (2nd ed., pp. 91–124). Santa Barbara, CA: ABC-CLIO.
- Burgener, S., & Twigg, P. (2002). Relationships among caregiver factors and quality of life in care recipients with irreversible dementia. Alzheimer Disease and Associated Disorders, 16(2), 88–102. https://doi.org/10.1097/00002093-200204000-00006
- Carr, D., Freedman, V. A., Cornman, J. C., & Schwarz, N. (2014). Happy marriage, happy life? Marital quality and subjective well-being in later life. Journal of Marriage and Family, 76(5), 930–948. https://doi.org/10.1111/jomf.12133
- Choi, H., & Marks, N. F. (2006). Transition to caregiving, marital disagreement, and psychological well-being: A prospective U.S. National Study. Journal of Family Issues, 27(12), 1701–1722. https://doi.org/10.1177/0192513X06291523
- Clare, L., Nelis, S. M., Quinn, C., Martyr, A., Henderson, C., Hindle, J. V., … Victor, C. R. (2014). Improving the experience of dementia and enhancing active life – Living well with dementia: Study protocol for the IDEAL study. Health and Quality of Life Outcomes, 12(1), 164. https://doi.org/10.1186/s12955-014-0164-6
- Clare, L., Nelis, S. M., Whitaker, C. J., Martyr, A., Markova, I. S., Roth, I., … Morris, R. G. (2012). Marital relationship quality in early-stage dementia: Perspectives from people with dementia and their spouses. Alzheimer Disease and Associated Disorders, 26(2), 148–158. https://doi.org/10.1097/WAD.0b013e318221ba23
- Clare, L., Woods, R. T., Nelis, S. M., Martyr, A., Marková, I. S., Roth, I., … Morris, R. G. (2014). Trajectories of quality of life in early-stage dementia: Individual variations and predictors of change. International Journal of Geriatric Psychiatry, 29(6), 616–623. https://doi.org/10.1002/gps.4044
- Cook, W. L., & Kenny, D. A. (2005). The Actor–Partner Interdependence Model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29(2), 101–109. https://doi.org/10.1080/01650250444000405
- Dekel, R., Vilchinsky, N., Liberman, G., Leibowitz, M., Khaskia, A., & Mosseri, M. (2014). Marital satisfaction and depression among couples following men’s acute coronary syndrome: Testing dyadic dynamics in a longitudinal design. British Journal of Health Psychology, 19(2), 347–362.
- Diener, E., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. https://doi.org/10.1207/s15327752jpa4901_13
- Eaton, W. W., Muntaner, C., Smith, C., Tien, A., & Ybarra, M. (2004). Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R). In M. E. Maruish (Ed.), The Use of Psychological Testing for Treatment Planning and Outcomes Assessment (3rd ed., pp. 363–377). Mahwah, NJ: Lawrence Erlbaum.
- Farina, N., Page, T. E., Daley, S., Brown, A., Bowling, A., Basset, T., … Banerjee, S. (2017). Factors associated with the quality of life of family carers of people with dementia: A systematic review. Alzheimers & Dementia, 13(5), 572–581. https://doi.org/10.1016/j.jalz.2016.12.010
- Fauth, E., Hess, K., Piercy, K., Norton, M., Corcoran, C., Rabins, P., … Tschanz, J. (2012). Caregivers’ relationship closeness with the person with dementia predicts both positive and negative outcomes for caregivers’ physical health and psychological well-being. Aging & Mental Health, 16(6), 699–711. https://doi.org/10.1080/13607863.2012.678482
- Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. https://doi.org/10.1016/0022-3956(75)90026-6
- Gellert, P., Häusler, A., Gholami, M., Rapp, M., Kuhlmey, A., & Nordheim, J. (2018). Own and partners’ dyadic coping and depressive symptoms in individuals with early-stage dementia and their caregiving partners. Aging & Mental Health, (8), 1014–1022. https://doi.org/10.1080/13607863.2017.1334759
- Greene, J. G., Smith, R., Gardiner, M., & Timbury, G. C. (1982). Measuring behavioural disturbance of elderly demented patients in the community and its effects on relatives: A factor analytic study. Age and Ageing, 11(2), 121–126. https://doi.org/10.1093/ageing/11.2.121
- Hellström, I., Nolan, M., & Lundh, U. (2007). Sustaining `couplehood’: Spouses’ strategies for living positively with. Dementia, 6(3), 383–409. https://doi.org/10.1177/1471301207081571
- Hinde, R. A. (1997). Relationships: A dialectical perspective. Hove: Psychology Press.
- Kaufer, D. I., Cummings, J. L., Ketchel, P., Smith, V., MacMillan, A., Shelley, T., … DeKosky, S. T. (2000). Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. The Journal of Neuropsychiatry and Clinical Neurosciences, 12(2), 233–239. https://doi.org/10.1176/jnp.12.2.233
- Kenny, D. A., & Cook, W. L. (1999). Partner effects in relationship research: Conceptual issues, analytic difficulties, and illustrations. Personal Relationships, 6(4), 433–448. https://doi.org/10.1111/j.1475-6811.1999.tb00202.x
- Kenny, D. A., Kashy, D. A., & Cook, W. L. (2006). Dyadic data analysis. New York: Guildford Publications.
- Kulik, L. (2002). Marital equality and the quality of long-term marriage in later life. Ageing & Society, 22(4), 459–481. https://doi.org/10.1017/S0144686X02008772
- Laver, K., Milte, R., Dyer, S., & Crotty, M. (2017). A systematic review and meta-analysis comparing carer focused and dyadic multicomponent interventions for carers of people with dementia. Journal of Aging and Health, 29(8), 1308–1349. https://doi.org/10.1177/0898264316660414
- Litwin, H., & Shiovitz-Ezra, S. (2006). The association between activity and wellbeing in later life: What really matters? Ageing & Society, 26(2), 225–242. https://doi.org/10.1017/S0144686X05004538
- Luong, G., Charles, S. T., & Fingerman, K. L. (2011). Better with age: Social relationships across adulthood. Journal of Social and Personal Relationships, 28(1), 9–23. https://doi.org/10.1177/0265407510391362
- Martyr, A., Nelis, S. M., Quinn, C., Wu, Y.-T., Lamont, R. A., Henderson, C., … Clare, L. (2018). Living well with dementia: A systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychological Medicine, 48(13), 2130–2139. https://doi.org/10.1017/S0033291718000405
- McPherson, C. J., Wilson, K. G., Chyurlia, L., & Leclerc, C. (2011). The caregiving relationship and quality of life among partners of stroke survivors: A cross-sectional study. Health and Quality of Life Outcomes, 9(1), 29. https://doi.org/10.1186/1477-7525-9-29
- Menne, H. L., Judge, K. S., & Whitlatch, C. J. (2009). Predictors of quality of life for individuals with dementia: Implications for intervention. Dementia, 8(4), 543–560. https://doi.org/10.1177/1471301209350288
- Morris, R. G., & Mograbi, D. C. (2013). Anosognosia, autobiographical memory and self-knowledge in Alzheimer's disease. Cortex, 49(6), 1553–1565. https://doi.org/10.1016/j.cortex.2012.09.006
- Norton, M. C., Piercy, K. W., Rabins, P. V., Green, R. C., Breitner, J. C. S., Ostbye, T., … Tschanz, J. T. (2009). Caregiver–recipient closeness and symptom progression in Alzheimer disease. The Cache County Dementia Progression Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64B(5), 560–P568. https://doi.org/10.1093/geronb/gbp052
- Pinquart, M., & Sörensen, S. (2004). Associations of caregiver stressors and uplifts with subjective well-being and depressive mood: A meta-analytic comparison. Aging & Mental Health, 8(5), 438–449. https://doi.org/10.1080/13607860410001725036
- Pinquart, M., & Sörensen, S. (2011). Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging, 26(1), 1–14. https://doi.org/10.1037/a0021863
- Proulx, C. M., Helms, H. M., & Buehler, C. (2007). Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family, 69(3), 576–593. https://doi.org/10.1111/j.1741-3737.2007.00393.x
- Pruchno, R., Wilson-Genderson, M., & Cartwright, F. P. (2009). Depressive symptoms and marital satisfaction in the context of chronic disease: A longitudinal dyadic analysis. Journal of Family Psychology, 23(4), 573–584.
- Quinn, C., Clare, L., McGuinness, T., & Woods, R. T. (2012). The impact of relationships, motivations, and meanings on dementia caregiving outcomes. International Psychogeriatrics, 24(11), 1816–1826. https://doi.org/10.1017/S1041610212000889
- Quinn, C., Clare, L., & Woods, B. (2009). The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: A systematic review. Aging & Mental Health, 13(2), 143–154. https://doi.org/10.1080/13607860802459799
- Quinn, C., Clare, L., & Woods, R. T. (2015). Balancing needs: The role of motivations, meanings and relationship dynamics in the experience of informal caregivers of people with dementia. Dementia, 14(2), 220–237. https://doi.org/10.1177/1471301213495863
- Schulz, R., & Martire, L. M. (2004). Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. The American Journal of Geriatric Psychiatry, 12(3), 240–249. https://doi.org/10.1097/00019442-200405000-00002
- Schulz, R., O'Brien, A. T., Bookwala, J., & Fleissner, K. (1995). Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist, 35(6), 771–791. https://doi.org/10.1093/geront/35.6.771
- Spector, A., Orrell, M., Charlesworth, G., & Marston, L. (2016). Factors influencing the person-carer relationship in people with anxiety and dementia. Aging & Mental Health, 20(10), 1055–1062. https://doi.org/10.1080/13607863.2015.1063104
- Spruytte, N., Audenhove, C., Lammertyn, F., & Storms, G. (2002). The quality of the caregiving relationship in informal care for older adults with dementia and chronic psychiatric patients. Psychology and Psychotherapy: Theory, Research and Practice, 75(3), 295–311. https://doi.org/10.1348/147608302320365208
- Wadham, O., Simpson, J., Rust, J., & Murray, C. (2016). Couples’ shared experiences of dementia: A meta-synthesis of the impact upon relationships and couplehood. Aging & Mental Health, 20(5), 463–473. https://doi.org/10.1080/13607863.2015.1023769
- Waite, A., Bebbington, P., Skelton-Robinson, M., & Orrell, M. (2004). Social factors and depression in carers of people with dementia. International Journal of Geriatric Psychiatry, 19(6), 582–587. https://doi.org/10.1002/gps.1136
- Walker, R. B., & Luszcz, M. A. (2009). The health and relationship dynamics of late-life couples: A systematic review of the literature. Ageing & Society, 29(3), 455–480. https://doi.org/10.1017/S0144686X08007903
- Woods, R. T., Nelis, S. M., Martyr, A., Roberts, J., Whitaker, C. J., Markova, I., … Clare, L. (2014). What contributes to a good quality of life in early dementia? Awareness and the QoL-AD: A cross-sectional study. Health and Quality of Life Outcomes, 12(1), 94. https://doi.org/10.1186/1477-7525-12-94
- Wright, L. K. (1991). The impact of Alzheimer’s disease on the marital relationship. The Gerontologist, 31(2), 224–237. https://doi.org/10.1093/geront/31.2.224
