Abstract
Objective: This study aims to investigate the effect of an integrated intervention of art activities and Qigong exercise on the well-being of older adults in nursing homes in Indonesia.
Method: We employed a randomized controlled trial with 4 specific groups, i.e. art, Qigong, integration of art and Qigong, and control group. A total of 267 participants aged 50 years or older were recruited from 9 nursing homes in Jakarta, Indonesia. The participants were randomly allocated to one of the four groups, attending two intervention sessions per week for eight weeks (16 sessions), lasting 90 minutes each. Measurements were administered at baseline (T0) and post-intervention (T1). The primary outcome was well-being (WHOQOL-Bref) and secondary outcomes were satisfaction with life (SWLS), depression (BDI-II), and health status (SF-36).
Results: The art intervention had a significant positive effect on well-being, in particular in the domain of social relations. It also led to a decrease in depressive symptoms, as did the integration intervention. No significant effects were visible in the Qigong group nor in the integrated intervention compared to either art or Qigong alone.
Conclusion: Interventions such as art programs and an integration of art and Qigong may give psychological benefits to older adults. Yet, results of the study need to be interpreted with caution and need to be replicated. A qualitative approach would be welcome to get an in-depth understanding of why art intervention is especially beneficial. (Trial registration: Clinicaltrials.gov NCT02957773, registered 28 September 2016).
Introduction
There is a large and increasing number of older adults in Indonesia (Kadar, Francis, & Sellick, Citation2013; Mustari, Rachmawati, & Nugroho, Citation2015). The percentage of older adults in the population increased from 4.5% in 1971 to 9.8% in 2010 and is estimated to increase to 11.34% in 2020 (United Nations, Citation2011). This means that Indonesia has made a significant improvement in general health status (World Health Organization, Citation2017b). For example, the Indonesian government has successfully implemented programs for strengthening health services in underdeveloped islands, improving the services of clean drinking water, sanitation, and nutrition (Pusat Kesehatan Masyarakat), and optimization of the National Health Insurance program (Jaminan Kesehatan Nasional). As a result of these programs, the life expectancy of Indonesian people continues to increase and this in turn has an impact on the increasing number of elderly people in Indonesia (Badan Pusat Statistik, Citation2018).
Our study targets older adults in nursing homes in Indonesia because the prevalence of depression in the nursing home population is very high (42.5%), and there is high demand for appropriate nursing homes programs to accommodate both physical and mental health of the older adults (Djernes, Citation2006; Etemadi & Ahmadi, Citation2009; Jongenelis, et al., Citation2004; Pramesona & Taneepanichskul, Citation2018; United Nations, Citation2007). Currently, the programs available in nursing homes in Indonesia do not specifically address older adults’ needs (Arifianto, Citation2013; Nasir, Citation2015), which are to adapt successfully to age-related mental and physical decline, to prevent or delay disabilities and chronic diseases, and to maintain their level of well-being. There are not many health care programs available in Indonesian nursing homes (Arifianto, Citation2006), and the quality of those mental health programs are insufficient (United Nations, Citation2017). The existing activities for Indonesian nursing home residents are, for example, spiritual guidance and related activities, regular meals and medical check-ups, hosting guests or watching movies. These activities tend to be monotonous and not to be meaningful (Choi, Ransom, & Wyllie, Citation2008; Djernes, Citation2006; Sriyanto, Citation2012). Indonesian nursing home residents currently are not supported by programs that could influence their well-being (Arifianto, Citation2006; Sriyanto, Citation2012). As an activity for older adults, art activities and Qigong exercise could be promising to improve older adults’ well-being.
Well-being refers to optimal psychological functioning (Ryan & Deci, Citation2001). It involves high levels of positive affect, low levels of negative affect, a high degree of overall life satisfaction, and the belief that life is worth living since one is able to realize one’s own potential (Lambert, Passmore, & Holder, Citation2015). The terms well-being and quality of life are practically synonymous and are used interchangeably (Peplau, Citation1994). Maintaining one’s well-being by active aging is believed to prevent or delay disabilities and chronic diseases (Bowling, Citation2008; Ryff, Citation2014). Active aging is defines as “the process of optimizing opportunities for health, participation, and security to enhance the quality of life as people age” (World Health Organization, Citation2015, p.5). Active aging that includes participating in activities and exercise could address many challenges such as costs related to medical treatment and health care services. It could also prevent premature deaths and lead to fewer disabilities associated with chronic diseases in older age (Djernes, Citation2006). Furthermore, it could help avoid mental health problems, particularly depression, which is under-diagnosed and prevalent in older adults (World Health Organization, Citation2002).
Previous studies have shown promising effects of participation in activities or exercise such as art or Qigong (Im & Lee, Citation2014; Jones, Warren, & McElroy, Citation2006; Kim, Citation2013; Kuan, Chen, & Wang, Citation2012; Tsang et al., Citation2013; Wang et al., Citation2010, Citation2013). Specifically, art activities aim to help older adults express their feelings and personal problems and engage in socialization processes and to facilitate communication (Buchalter, Citation2011; Johnson & Sullivan-Marx, Citation2006; Jones et al. Citation2006; Liebmann, Citation2004). The socialization process that is elicited during art activities could increase satisfaction in life (Mair & Thivierge-Rikard, Citation2010; Wikström, Citation2002). Qigong is a form of exercise that is safe and cost-effective (Horowitz, Citation2009). It is a suitable daily activity for older adults in nursing homes because it consists of slow gentle meditative movements that are low-impact and low-intensity, it is easy to learn, and it can be practiced at almost any location and at any time by all age groups (Chang & Chen, Citation2016; Kuan et al. Citation2012; Wang et al., Citation2013). Qigong exercise has been found to reduce depression and to improve self-efficacy and well-being in older adults, also in those with a chronic physical illness (Tsang, Fung, Chan, Lee, & Chan, Citation2006; Tsang et al., Citation2013).
A recent review on the integration of art activities and physical exercise found no existing studies into the direct effect of such an integration in comparison with the single interventions (Roswiyani, Kwakkenbos, Spijker, & Witteman, Citation2017). Thus, it is still unknown whether the integration of art activities and Qigong exercise is beneficial for older adults.
The present study aims to investigate the effect of an intervention integrating art and Qigong on the well-being, depression, satisfaction in life, and health status of older adults in nursing homes in Indonesia. The primary hypothesis is that both the integrated intervention and the single interventions (art and Qigong) will be more beneficial than no intervention. The secondary hypothesis is that the integrated intervention will be more beneficial than the single interventions, i.e. either art activities or Qigong exercise alone.
Method
Study design
This study is a randomized controlled trial (RCT) with four groups: (1) a group with Qigong and art activities as an integrated intervention, (2) a group with art activities, (3) a group with Qigong, and (4) a control group that gets no intervention. Participants will be randomly allocated to one of the groups. Randomizing the participants into the four groups was done through a sealed-envelopes selection process where people were randomly handed out envelopes, which contained a card labeled with the information about the intervention (the number of sessions and time period). The study was approved by the Tarumanagara University Human Research Ethics Committee (TUHREC), Institute for Research and Academic Publication, Jakarta, Indonesia (PPZ20162005).
Participants
Eligibility for participation was based on the following criteria: A participant (1) was aged 50 years or older and had been admitted to the nursing home at least 3 months earlier; (2) was deemed to be cognitively capable of participating in the intervention based on a score of 18 or above on the Mini-Mental State Examination (MMSE); (3) was able to communicate based on an understanding of the information and instruction during the screening process; (4) was in healthy physical condition, which was judged by the ability to walk and do daily activities without assistance; (5) was able to see and hear well enough to participate in the group; (6) consented to randomization and follow-up; (7) showed no psychotic disorders and no alcohol/drug misuse based on MINI Neuropsychiatric Interview; and (8) suffered no severe physical illness/disability that could affect participation.
Study settings and procedures
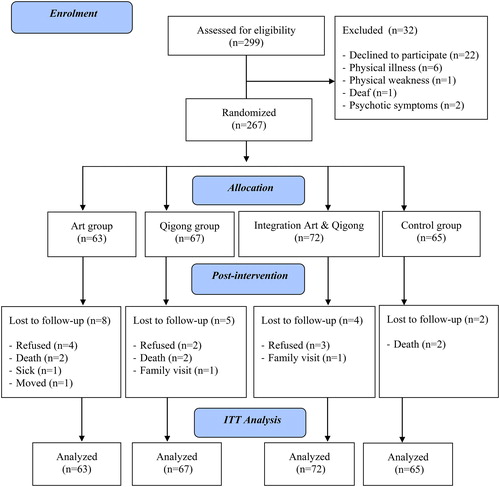
Participants were Indonesian older adults recruited from nine nursing homes in Jakarta, Indonesia through advertisements posted at nursing home offices. Participants meeting the inclusion criteria were contacted individually for the baseline measure and the randomization process to one of the intervention groups or control group, and also for post-measures at the end of the intervention (8th week). Written informed consent was obtained from all participants who were enrolled in the study. The flow diagram of the participants is presented in .
Intervention
The following is a brief explanation of the content of the art and qigong programs.
Art activities
The art program was based on study from Roswiyani, Satiadarma, Spijker, and Witteman (Citation2016) and adapted from Landgarten (Citation1981) and Buchalter (Citation2011). The program is composed of six phases, and aims to make older adults explore their selves, become familiar with the activities, express their feelings and perception, evaluate their interpersonal relationships, and express their perception of being old. Each of these phases has its own theme and detailed description of the activities for the participants. The activities include drawing, coloring, picture completion, mandala, and collage. Materials such as A3-size sketch paper, oil pastels, bright color markers, 2B art pencils, magazines, glue sticks, and scissors are provided. Group discussions were conducted at the end of each session.
Qigong exercise
The program of Qigong exercise was adapted from the work of Dr. Chok Hiew, i.e. Wisdom Heart Qigong (WHQ), which is a mind-body therapeutic technique using a gentle set of meditative movements that has benefits for physical and mental health. The Qigong exercise for older adults consists of nine movements with three main features—body postures and movement, meditation, and breathing (Tsang, Mok, Au Yeung, & Chan, Citation2003; Wang et al., Citation2013). The exercise is intended to achieve body balance and strength, better fluids circulation in the body, and physical and mental relaxation (Johnson, Stewart, & Howell, Citation2000; Wang et al., Citation2013). Each of the movements has specific benefits, for example, to enhance blood flow from the pelvic area to the brain by moving the hips, or to increase memory and brain functioning by moving the head up and down and to the left and right.
In particular, the three groups received 16 sessions of the intervention with each session lasting 90 minutes. The intervention was conducted twice a week for 8 weeks. The sessions were led by the first author and by junior psychologists who are experienced in providing art therapy and were trained as Qigong practitioners. Subsequent to the composition of the four respective groups, the intervention process was carried out.
In the integrated intervention group, an instructor provided guidance for participants to do Qigong for 30 minutes followed by 60 minutes of art activities. Both were done in a group setting in the same room.
In the art intervention group, participants were guided through art activities for 60 minutes. In the remaining 30 minutes participants could do their daily activities or discuss their artwork with their group members. In the Qigong intervention group, two Qigong practitioners guided participants to do Qigong exercises for 30 minutes, then in the remaining 60 minutes the participants could do their daily activities or share their experience during the Qigong exercise with the other group members.
In the control group, the participants were engaged in their regular daily activities and did not receive any therapeutic intervention. The researchers observed these daily activities for 90 minutes.
Outcome measures
All outcome measures were collected at baseline (T0) and after 8 weeks of participating in the intervention programs (T1). Well-being was the primary outcome and was assessed using the WHOQOL-Bref. This scale was developed by World Health Organization to determine subjective and psychological well-being (The WHO Group, Citation1998). It contains 26 statements which are rated on a five-point Likert scale using response categories from 1 (very poor) to 5 (very good). The instrument covers four domains, namely: psychological health, physiological health, social relationships, and environmental health. The test-retest reliability for the WHOQOL-BREF lies between 0.80 and 0.90 (Saxena, Carlson, Billington, & Orley, Citation2001).
The secondary outcomes were satisfaction with life, depression, and health status. Satisfaction with life was measured with the Satisfaction With Life Scale (SWLS; Diener, Citation1984). The SWLS is a 5-item scale to assess global judgments of satisfaction with one's life. Items are rated on a 7-point scale (from 1, representing strongly disagree, to 7, representing strongly agree), with higher scores indicating higher life satisfaction. It has strong internal reliability (Cronbach’s alpha 0.87) and correlates with 10 other measurements of subjective well-being, r = .50 (Diener, Emmons, Larsen, & Griffin, Citation1985).
Depression was assessed using the Beck Depression Inventory-II for the Indonesian general population which contains 21 self-report items ( BDI-II; Beck, Steer, & Brown, Citation1996; Ginting, Näring, van der Veld, Srisayekti, & Becker, Citation2013 ). All items were rated on a 4-point Likert-type scale ranging from 0 (not at all) to 3 (extreme form of each symptom) to indicate the degree of severity of depression within the previous two weeks. Cronbach’s alpha of the BDI-II was .90 for healthy participants and .91 for depressed patients. The test-retest correlation of the BDI-II was significant with r = .55, p < .01 (Ginting et al., Citation2013).
Assessment of health status was done using the SF-36 health survey with 36 questions that are widely used for measuring self-reported physical and mental health status (Perwitasari, Citation2012; Ware, Citation1993). Estimates of reliability in the physical and mental components are above 0.90 (Ware, Citation1993).
We examined the participants’ sociodemographic characteristics (i.e. age, gender, ethnicity, education, marital status, duration of stay in a nursing home, and the reason for staying in a nursing home) and clinical information (i.e. cognitive functioning and symptoms of depression). The clinical information was gathered using the Mini-Mental State Exam (MMSE; Folstein, Folstein, & McHugh, Citation1975), a brief indicator of cognitive functioning. The MMSE is an 11-question measure that specifically tests five areas of cognitive function, i.e. orientation, registration, attention and calculation, recall, and language. The maximum score on an MMSE is 30. A score between 23 and 18 indicates mild cognitive impairment, and a score below 18 indicates severe cognitive impairment. In this study, we included participants with MMSE score 18 or above who are capable of participating in the intervention. The MMSE has a test-retest reliability ranging from 0.80 to 0.98 (Folstein et al. Citation1975). To assess symptoms of depression, we used the Geriatric Depression Scale 15 items (GDS-15; Sheikh & Yesavage, Citation1986), consisting of 15 questions, with a yes or no answer where yes is treated as 0 and no treated as 1. An example of the question: “Do you feel happy most of the time?”. A score of above 5 points is suggestive of depression. All the questions in the questionnaires were read out to the participants who then responded verbally. The answers were written down by research assistants for further analyses. In this study, adherence to the intervention was established based on participants’ attendance at the intervention sessions.
Analysis
Chi square tests and analyses of variance were utilized to look at the data of the participants in all four groups (integration, art, Qigong, and control) and to compare their baseline data (sociodemographic characteristics and clinical information, MMSE and GDS-15). All participants who were included in the randomization process were analyzed (intention to treat analyses). A multivariate analysis of variance (MANOVA) was used to compare changes in the outcome measures over time (T0 to T1) and between the four groups. Group differences were further tested with planned contrasts (Warner, Citation2008). Statistical analyses were performed with SPSS 23. Missing data were deemed to be missing at random and calculated using the missing value analysis option of SPSS, EM (expectation-maximization) method (Rubin, Witkiewitz, Andre, & Reilly, Citation2007).
Results
Demographic and clinical characteristics
displays the characteristics of the participants. The participants in the four groups were similar in sociodemographic and clinical characteristics. The participants’ ages ranged from 50 to 96 years, they were mostly women, of Javanese ethnic origin and Christian religious background, finished primary school or below, and almost half were married or widowed. They had been living in a nursing home for more than one year and the main reason that they chose to live in a nursing home was a friend/family recommendation. At screening, the MMSE and GDS-15 were administered and it was found that 54% of the participants had no cognitive impairment and 66% had no symptoms of depression. Although participants in this study had different clinical characteristics (symptoms of depression and cognitive functioning), these clinical characteristics of the participants did not influence the main effects of the interventions.
Table 1. Sociodemographic and clinical characteristics of the participants.
Primary outcome: well-being
shows the change scores in well-being from T0 to T1 measured with the WHOQOL-Bref. A MANOVA was conducted to test whether the interventions had an effect over the time (T0, T1) with difference scores on four domains of well-being as dependent variables (domain 1: physiological health; domain 2: psychological health; domain 3: social relationship; domain 4: environment health) and with group (integration, art, Qigong and control) as between-subject factor. The result showed no significant main effect of group over the time, F(12, 688) = 1.544, p = .104. Between-subject tests showed a significant group effect on well-being, yet only on domain 3, with F(3, 263) = 2.971, p = .032, ηp2 = .033.
Table 2. Well-being scores on four domains before (baseline, T0) and after (T1) the four interventions.
Hypothesis 1
Comparing (any) intervention to the control group, the results of the analysis using a Helmert contrast showed that there were no significant differences on the four domains of well-being (domain 1: p= .262; domain 2: p= .902; domain 3: p= .344; and domain 4: p= .620). When comparing all groups separately using Simple contrasts (integration group versus control group; art group versus control group; and Qigong group versus control group) on the four domains of well-being, there was a significant increase in well-being on domain 3 (social relationship) especially in the comparison of the art group to the control group (p= .019). This finding indicates that well-being in social relationships increased more for participants in the art group than for those in the control group.
Hypothesis 2
Looking at the integration group versus the two other intervention groups, we found no significant differences on the four domains of well-being (domain 1: p= .634; domain 2: p= .816; domain 3: p= .342; and domain 4: p= .722). Comparing the single intervention groups to the integration group using Simple contrasts (integration group versus art group; and integration group versus Qigong group) on the four domains of well-being, we saw a significant increase on the well-being domain 3 (social relationship), specifically in the comparison of the integration group with the art group (p= .030). This finding also indicates that participants’ well-being in social relationships increased more in the art group than in the integration group.
Secondary outcomes: satisfaction in life, depression, and health status
Our secondary outcomes were satisfaction in life (SWLS), depression (BDI-II), and health status (SF-36). shows the scores on T0 and T1 on the SWLS, BDI-II, and SF-36. A MANOVA was conducted to test whether the interventions had an effect on the scores on the SWLS, the BDI-II, and eight domains of the SF-36 (physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health), with group (integration, art, Qigong, and control) as between-subject factor. The resultant findings are described for each outcome measure separately.
Table 3. Scores on Satisfaction In Life (SWLS), Depression (BDI-II), and Health Status (SF-36) before (baseline, T0) and after (T1) the four interventions.
Satisfaction with life scale (SWLS)
There was no significant effect of group on the SWLS, F(3, 263) = 1.288, p = .279. Subsequent planned contrasts were performed to test the hypotheses whether both the integrated intervention and the single interventions (art and Qigong) are more beneficial than no intervention (hypothesis 1) and whether the integrated intervention is more beneficial than the single interventions, i.e. either art activities or Qigong exercise (hypothesis 2) on the SWLS. Results of the analyses for hypothesis 1 and 2 displayed that there was no difference between the intervention groups and the control group (p = .131), nor between the integration group and the art group (p = .213) or between the integration group and the Qigong group (p = .375).
Beck depression inventory-II (BDI-II)
Overall, there was a significant effect of group on the BDI-II, F(3, 263) = 3.523, p = .016, ηp2 = .039.
Hypothesis 1
Using Helmert contrast, the result indicated that there was a significant difference between the intervention groups and the control group (p = .003) on the BDI-II. Additionally, a simple contrast was calculated to compare each group with the control group, and it was confirmed that there were significant differences between the integration group and the control group (p= .005) and between the art group and the control group (p = .005). These findings suggest that depression decreased more in the integration group and in the art group than in the control group. No difference was found between the Qigong group and the control group on the BDI-II (p= .102).
Hypothesis 2
There was no difference between the integration group and the single groups on the BDI-II using Helmert contrast (p= .546). When using simple contrasts to compare the integration group to the single groups separately, there was still no difference between the integration group and the art group (p= .920) or between the integration group and the Qigong group (p= .252).
Health status (SF-36)
There were no effects of group on the eight domains of the SF-36 (physical functioning: p= .616; role physical: p= .081; bodily pain: p= .739; general health: p= .606; role emotional: p= .297; vitality: p= .401; mental health: p = 588; and social functioning: p = 721). The planned contrast was further performed to test the hypotheses on SF36 but also with no significant result.
Adherence rate
Adherence to the intervention was calculated by counting how often the participants attended the sessions of the intervention. We defined high adherence as attending at least 75% of all sessions (12 out of 16 sessions). In this study, adherence to the intervention was high for around half of the participants (52%), moderate for 19% of the participants (attending 8–11 sessions), and low for 29% of the participants (attending fewer than 8 sessions). A MANOVA was performed to test whether the adherence rate (high, moderate or low) had an effect on the outcome measures but no main effect of adherence on any of the outcome measures was found.
Discussion
This study aimed to investigate the effect of an integrated intervention of art activities and Qigong exercise on the well-being, depression, satisfaction in life, and health status of older adults in nursing homes in Indonesia. In this randomized clinical trial in which we compared art activities, Qigong exercise, and the integration of both to a control condition, we found that well-being increased significantly in the art group compared to the control group or the integrated intervention group, but only on the domain of social relationships. We also found a decrease of depressive symptoms in the art group and the integrated intervention group compared to the control condition. These findings must be interpreted with caution because the effect sizes were relatively small. No significant result was found in the outcome of satisfaction in life and health status in all interventions group.
Well-being
The results on well-being were only significant in the domain of social relationships. Our finding is in agreement with another study that mentioned that the opportunities for engaging in the intervention in a group setting provides a sense of belonging and attachment to other people (Berkman, Glass, Brissette, & Seeman, Citation2000). This social engagement increased the sense of social identification with others (Gleibs et al., Citation2011) and is perceived as social support that is important for older adults (Berkman et al., Citation2000). Having social relationship has been linked to better mental health (Mair & Thivierge-Rikard, Citation2010).
The significant result on well-being appeared in the art activities group only. Our results reflect those of Hattori, Hattori, Hokao, Mizushima, and Mase (Citation2011), Im and Lee (Citation2014), and (Kim, Citation2013) who also found that art therapy was beneficial to improve well-being. The finding further supports the idea of previous research (Mair & Thivierge-Rikard, Citation2010; Stephenson, Citation2013; Zunzunegui, Alvarado, Del Ser, & Otero, Citation2003) suggesting that through the art making process in a group, sharing with others helps to create a cooperative and encouraging environment. Similarly, the feeling of connection with other people could reduce feelings of isolation and could give hope to the individual (Moon, Citation2016).
The integration intervention was not more beneficial to well-being than the single interventions. This result is not in line with the findings in our previous review on the effectiveness of combining art activities and physical exercise for older adults (Roswiyani, Kwakkenbos, et al., Citation2017). It may be that combining the two activities — Qigong exercise preceding art activities — in the same session was difficult and too demanding for our older population. Furthermore, the Qigong group did not show significant improvements in well-being compared to the control group. Our results are in contrast with other studies showing positive effects of Qigong exercise (Kuan et al. Citation2012; Tsang et al., Citation2003; Citation2006). Our result might be related to the duration and intensity of the exercise (30 minutes per session, with nine movements). Previous studies suggested that a positive result could be achieved when older adults practiced more than two times a week or even every day with the duration of each session being more than 30 minutes (Chan, Yu, & Choi, Citation2017; Oh, Choi, Inamori, Rosenthal, & Yeung, Citation2013; Tsang et al., Citation2003, Citation2006). This suggests that perhaps we need to increase the duration of the exercise or turn it into daily practice to get more benefit from the exercise.
Levels of depression were significantly reduced in the art activities group and the integrated intervention group compared to the control condition. A previous study (Skov, Citation2015) demonstrated that individuals with depression often feel their lives to be meaningless. In order to increase their meaning in life, individuals need to develop competence. Thus, the therapeutic aspects of art can help the individual to gain more meaning in life and lead to a decrease in depression. Besides, the art activity itself allows older adults to express their emotions in a safe way (Johnson & Sullivan-Marx, Citation2006; Stephenson, Citation2013). Self-expression could help older adults to discover and accept themselves, and develop a new perspective on themselves through the art media (Alders & Levine-Madori, Citation2010; Eksell, Citation2015; Stewart, Citation2004). Likewise, it also helps people to express their emotions during the art-making process, which in turn helps to reduce their negative feelings (Skov, Citation2015). In the integration intervention group, the observed reduction in depression could be attributed to the art activities as there was no evidence of significant effect of qigong exercise on depression compared to the control group.
Satisfaction with life and health status
There were no significant improvements in satisfaction with life and health status of participants in any of the intervention groups. However, there does seem to be a positive trend when looking at the scores from T0 to T1 on satisfaction with life and some of the health status outcomes (physical functioning, vitality, and mental health) in all intervention groups compared to the control group. We only investigated the short-term effect of the intervention, and it is possible that a longer duration of the intervention is needed to have an impact on satisfaction with life and health status.
Participant characteristics
We included a naturalistic sample of nursing home residents with different clinical characteristics, for example, no cognitive impairment (54%) and mild cognitive impairment (46%), depressed (34%) and non-depressed (66%), and we did not find an association between these characteristics and outcome. This signifies that the interventions can be applied to a broad range of inhabitants of nursing homes.
There are several strengths to our study. First, we had a large sample. We managed to recruit a large number of residents from different nursing homes in Jakarta. Second, we had a strong study design, with four conditions including a control condition. Third, the adherence of the participants was satisfactory. We found that 71% of our participants adhered to the intervention (moderate to high adherence), which confirms that the interventions are feasible for an older adult population.
Several limitations of this study need to be acknowledged. First, the lack of diversity in sociodemographic background is one of our limitations because the nursing homes from which we recruited participants all had a Christian orientation and all were located in the Jakarta area. Furthermore, participants were predominantly of Javanese ethnicity, and had low levels of education. Consequently, our findings cannot be generalized to residents of all nursing homes in Indonesia. Next, most of our participants were women. Therefore, it is unknown whether the results are also valid for male nursing home residents. In addition, the interventions were conducted twice a week and limited by their short duration. Finally, the participants responded verbally to the self-report questionnaires, which might increase a social desirability response bias.
Future studies need to consider a longer duration of especially the Qigong intervention to enhance the effect. It would also be useful to do a follow-up study to see whether the effect of these interventions can extend to 3 or 6 months after the program. Finally, a qualitative approach would be helpful to get an in-depth understanding of the feelings and reactions of the target population to these types of intervention.
Conclusion
To conclude, we found that an art program and, to a lesser extent, a combination of art and Qigong, offers psychological benefits for older adults in nursing homes in Indonesia. More research is needed to evaluate the long-term effects of these interventions and the reason why nursing home residents particularly like art rather than other intervention. Finally, art activities might be considered first for further implementation.
Ethics approval and consent to participate
The Tarumanagara University Human Research Ethics Committee (TUHREC), Jakarta, Indonesia approved the trial protocol (project number: PPZ20162005). The TUHREC will ensure that the study is conducted within appropriate human research ethical guidelines and has a proper data management system. All eligible patients are informed (both written and verbal) about the purpose of the study, the expected duration, and procedure, the right to decline to participate and to withdraw from the research at any given time once participation has begun without any consequences. Written informed consent is obtained from all participants who are enrolled in the study.
Consent for publication
Consent for publication forms a specific part of the consent for participation. It has been obtained from all participants or their legal guardians.
| Abbreviations | ||
| BDI-II | = | Beck Depression Inventory-II |
| GDS-15 | = | Geriatric Depression Scale 15 items |
| MMSE | = | The Mini-Mental State Examination |
| RCT | = | Randomized Controlled Trial |
| SF-36 | = | The 36-item short-form survey |
| SWLS | = | The Satisfaction With Life Scale |
| WHOQOL-BREF | = | World Health Organization Quality of Life |
Acknowledgements
This research was supported by Universitas Tarumanagara, Jakarta, Indonesia, under grant number 128-R.1/UNTAR/IV/2014. We would also like to acknowledge the Behavioural Science Institute, Radboud University, Nijmegen, The Netherlands for the authorship and publication of this study, and its general support on this research. We are thankful to various people for their contribution to this project; all nursing homes in Jakarta, Indonesia for their cooperation, and all participants willing to participate in this study; all research assistants for their help in collecting the data; our colleagues from Faculty of Psychology, Universitas Tarumanagara, Jakarta, Indonesia and colleagues from Department of Experimental Psychopathology and Treatment, Radboud University, Nijmegen, The Netherlands who provided expertise that greatly assisted the research.
Disclosure statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Funding
References
- Alders, A., & Levine-Madori, L. (2010). The Effect of Art Therapy on Cognitive Performance of Hispanic/Latino Older Adults. Art Therapy, 27(3), 127–135. doi:10.1080/07421656.2010.10129661
- Arifianto, A. (March, 2006). Public policy towards the elderly in Indonesia: Current policy and future directions. Jakarta: Smeru Research Institute.
- Badan Pusat Statistik. (2018). Statistik Penduduk Lanjut Usia Indonesia 2018. Subdirektorat Statistik Pendidikan dan Kesejahteraan Sosial, Jakarta-Indonesia. Retrieved March 11, 2019, from https://www.bps.go.id/publication.html/Publikasi%5BtahunJudul%5D=2018&Publikasi%5BkataKunci%5D=lanjut+usia&yt0=Tampilkan
- Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory-II. San Antonio, 78(2), 490–498.
- Berkman, L. F., Glass, T., Brissette, I., & Seeman, T. E. (2000). From social integration to health: Durkheim in the new millennium. Social Science and Medicine, 51(6), 843–857.
- Bowling, A. (2008). Enhancing later life: How older people perceive active ageing? Aging &Amp; Mental Health, 12(3), 293–301.
- Buchalter, S. (2011). Art therapy and creative coping techniques for older adults. Pentonville Road, London: Jessica Kingsley Publishers.
- Chan, A. W. K., Yu, D. S. F., & Choi, K. C. (2017). Effects of tai chi Qigong on psychosocial well-being among hidden elderly, using elderly neighborhood volunteer approach: A pilot randomized controlled trial. Clinical Interventions in Aging, 12, 85–96.
- Chang, M.-Y., & Chen, H.-Y. (2016). Body composition outcomes of a Qigong intervention among community-dwelling aging adults. Western Journal of Nursing Research, 38(12), 1574–1594.
- Choi, N. G., Ransom, S., & Wyllie, R. J. (2008). Depression in older nursing home residents: The influence of nursing home environmental stressors, coping, and acceptance of group and individual therapy. Aging and Mental Health, 12(5), 536–547.
- Diener, E. (1984). Subjective well-being. Psychological Bulletin, 95(3), 542–575.
- Diener, E., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75.
- Djernes, J. K. (2006). Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatrica Scandinavica, 113(5), 372–387.
- Eksell, B. S. (2015). Creativity as a means to expression of emotions by older adults. Walden University: Walden Dissertations and Doctoral Studies.
- Etemadi, A., & Ahmadi, K. (2009). Psychological disorders of elderly home residents. Journal of Applied Sciences, 9(3), 549–554.
- Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198.
- Ginting, H., Näring, G., van der Veld, W. M., Srisayekti, W., & Becker, E. S. (2013). Validating the beck depression inventory-II in Indonesia's general population and coronary heart disease patients. International Journal of Clinical and Health Psychology, 13(3), 235–242.
- Gleibs, I. H., Haslam, C., Jones, J. M., Haslam, S. A., McNeill, J., & Connolly, H. (2011). No country for old men? The role of a ‘Gentlemen's Club’ in promoting social engagement and psychological well-being in residential care. Aging & Mental Health, 15(4), 456–466.
- Hattori, H., Hattori, C., Hokao, C., Mizushima, K., & Mase, T. (2011). Controlled study on the cognitive and psychological effect of coloring and drawing in mild Alzheimer's disease patients. Geriatrics & Gerontology International, 11(4), 431–437.
- Horowitz, S. (2009). Evidence-based health benefits of Qigong. Alternative and Complimentary Therapies, 15(4), 178–183.
- Im, M. L., & Lee, J. I. (2014). Effects of art and music therapy on depression and cognitive function of the elderly. Technology and Health Care: Official Journal of the European Society for Engineering and Medicine, 22(3), 453–458.
- Johnson, C. M., & Sullivan-Marx, E. M. (2006). Art therapy: Using the creative process for healing and hope among African American older adults. Geriatric Nursing, 27(5), 309–316.
- Johnson, J. A., Stewart, J. M., & Howell, M. H. (2000). Chinese medical Qigong therapy: A comprehensive clinical guide. Pacific Grove, CA: International Institute of Medical Qigong
- Jones, F., Warren, A., & McElroy, S. (2006). Home-based art therapy for older adults with mental health needs: Views of clients and caregivers. Art Therapy, 23(2), 52–58.
- Jongenelis, K., Pot, A. M., Eisses, A. M., Beekman, A. T., Kluiter, H., & Ribbe, M. W. (2004). Prevalence and risk indicators of depression in elderly nursing home patients: The aged study. Journal of Affective Disorders, 83(2-3), 135–142.
- Kadar, K. S., Francis, K., & Sellick, K. (2013). Ageing in Indonesia–health status and challenges for the future. Ageing International, 38(4), 261–270.
- Kim, S. K. (2013). A randomized, controlled study of the effects of art therapy on older Korean-Americans’ healthy aging. The Arts in Psychotherapy, 40(1), 158–164. doi:10.1016/j.aip.2012.11.002
- Kuan, S. C., Chen, K. M., & Wang, C. (2012). Effectiveness of Qigong in promoting the health of wheelchair-bound older adults in long-term care facilities. Biological Research for Nursing, 14(2), 139–146.
- Lambert, L., Passmore, H. A., & Holder, M. D. (2015). Foundational frameworks of positive psychology: Mapping well-being orientations. Canadian Psychology/Psychologie Canadienne, 56(3), 311.
- Landgarten, H. B. (1981). Clinical art therapy: A comprehensive guide. New York: Brunner-Routledge.
- Liebmann, M. (2004). Art therapy for groups: A handbook of themes and exercises (2nd ed.). 27 Church Road, Hove, East Sussex BN3 2FA: Brunner-Routledge.
- Mair, C. A., & Thivierge-Rikard, R. (2010). The strength of strong ties for older rural adults: Regional distinctions in the relationship between social interaction and subjective well-being. The International Journal of Aging and Human Development, 70(2), 119–143.
- Moon, B. L. (2016). Art-based group therapy: Theory and practice. Springfield, Illinois, USA: Charles C Thomas Publisher, Ltd.
- Mustari, A., Rachmawati, Y., & Nugroho, S. (2015). Statistik penduduk lanjut usia 2014. Jakarta: Badan Pusat Statistik.
- Nasir, S. (2015). Indonesia at 70: Prepare for aging population. The Jakarta Post. Retrieved from http://www.thejakartapost.com/news/2015/08/15/indonesia-70-prepare-aging-population.html
- Oh, B., Choi, S. M., Inamori, A., Rosenthal, D., & Yeung, A. (2013). Effects of Qigong on depression: A systemic review. Evidence-Based Complementary and Alternative Medicine, 2013, 1.
- Peplau, H. E. (1994). Quality of life: An interpersonal perspective. Nursing Science Quarterly, 7(1), 10–15.
- Perwitasari, D. A. (2012). Development the validation of Indonesian version of sf-36 questionnaire in cancer disease. Indonesian Journal of Pharmacy, 23, 248–253.
- Pramesona, B., & Taneepanichskul, S. (2018). Prevalence and risk factors of depression among Indonesian elderly: A nursing home-based cross-sectional study. Neurology, Psychiatry and Brain Research, 30, 22–27.
- Roswiyani, R., Kwakkenbos, L., Spijker, J., & Witteman, C. L. M. (2017). The effectiveness of combining visual art activities and physical exercise for older adults on well-being or quality of life and mood: A scoping review. Journal of Applied Gerontology. OnlineFirst. doi:10.1177/0733464817743332.
- Roswiyani, R., Satiadarma, M. P., Hiew, C. H., Witteman, C. L., & Spijker, J. (2017). Integration of social art activities and Qigong for the well-being or quality of life of older adults in nursing homes in Indonesia: Study protocol for a randomized controlled trial. Unpublished manuscript. Nijmegen, The Netherlands: Radboud University.
- Roswiyani, R., Satiadarma, M. P., Spijker, J., & Witteman, C. L. (2016). Social art activities in a nursing home: A pilot study in Indonesia. IAFOR Journal of Psychology & the Behavioral Sciences, 2(1), 45–59. doi:10.22492/ijpbs.2.1.
- Rubin, L. H., Witkiewitz, K., Andre, J. S., & Reilly, S. (2007). Methods for handling missing data in the behavioral neurosciences: Don’t throw the baby rat out with the bath water. Journal of Undergraduate Neuroscience Education, 5(2), A71.
- Ryan, R. M., & Deci, E. L. (2001). On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annual Review of Psychology, 52(1), 141–166.
- Ryff, C. D. (2014). Psychological well-being revisited: Advances in the science and practice of eudaimonia. Psychotherapy and Psychosomatics, 83(1), 10–28.
- Saxena, S., Carlson, D., Billington, R., & Orley, J. (2001). The who quality of life assessment instrument (whoqol-bref): The importance of its items for cross-cultural research. Quality of Life Research, 10(8), 711–721.
- Sheikh, J. I., & Yesavage, J. A. (1986). Geriatric depression scale (gds) recent evidence and development of a shorter version. Clinical Gerontology: A Guide to Assessment and Intervention, 5(1–2), 165–173.
- Skov, V. (2015). Integrative art therapy and depression. London, UK: Jessica Kingsley Publishers.
- Sriyanto, E. (2012). Lanjut usia: Antara tuntutan jaminan sosial dan pengembangan pemberdayaan. Jurnal Kawistara, 2(1), 73–86.
- Stephenson, R. C. (2013). Promoting well-being and gerotranscendence in an art therapy program for older adults. Art Therapy, 30(4), 151–158.
- Stewart, E. G. (2004). Art therapy and neuroscience blend: Working with patients who have dementia. Art Therapy, 21(3), 148–155.
- The WHO Group. (1998). Development of the world health organization whoqol-bref quality of life assessment. Psychological Medicine, 28(3), 551–558.
- Tsang, H. W., Fung, K. M., Chan, A. S., Lee, G., & Chan, F. (2006). Effect of a Qigong exercise programme on elderly with depression. International Journal of Geriatric Psychiatry, 21(9), 890–897.
- Tsang, H. W., Mok, C., Au Yeung, Y., & Chan, S. Y. (2003). The effect of Qigong on general and psychosocial health of elderly with chronic physical illnesses: A randomized clinical trial. International Journal of Geriatric Psychiatry, 18(5), 441–449.
- Tsang, H. W., Tsang, W. W., Jones, A. Y., Fung, K. M., Chan, A. H., Chan, E. P., & Au, D. W. (2013). Psycho-physical and neurophysiological effects of Qigong on depressed elders with chronic illness. Aging & Mental Health, 17(3), 336–348.
- United Nations. (2007). Economic and social commission for Asia and the pacific: High-level meeting on the regional review of the Madrid international plan of action on ageing (mipaa). In T. B. W. Rahardjo (Ed.), Review Of Madrid International Plan Of Action On Ageing: Country Report Of Indonesia. Macao, China: United Nations.
- United Nations. (2011). Information of the implementation of general assembly resolution 65/182 entitled “follow-up to the second world assembly on ageing in Indonesia”. Retrieved August 13, 2014, from http://www.ohchr.org/Documents/Issues/OlderPersons/Submissions/Indonesia.pdf.
- United Nations. (2017). Addressing the challenges of population ageing in Asia and the pacific: implementation of the Madrid international plan of action on ageing. Bangkok: United Nations Publication.
- Wang, C., Bannuru, R., Ramel, J., Kupelnick, B., Scott, T., & Schmid, C. H. (2010). Tai chi on psychological well-being: Systematic review and meta-analysis. BMC Complementary and Alternative Medicine, 10(1), 23.
- Wang, F., Man, J. K., Lee, E.-K. O., Wu, T., Benson, H., Fricchione, G. L., … Yeung, A. (2013). The effects of Qigong on anxiety, depression, and psychological well-being: A systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine, 2013, 16.
- Ware, J. E. (1993). Sf-36 health survey: Manual and interpretation guide. Boston, MA: Nimrod Press.
- Warner, R. M. (2008). Applied statistics: From bivariate through multivariate techniques. Thousand Oaks, California 91320: Sage Publication, Inc.
- Wikström, B. M. (2002). Social interaction associated with visual art discussions: A controlled intervention study. Aging & Mental Health, 6(1), 82–87.
- Zunzunegui, M.-V., Alvarado, B. E., Del Ser, T., & Otero, A. (2003). Social Networks, Social Integration, and Social Engagement Determine Cognitive Decline in Community-Dwelling Spanish Older Adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(2), S93–S100. doi:10.1093/geronb/58.2.S93
- World Health Organization. (2002). Active ageing: A policy framework. The Aging Male, 5(1), 1–37.
- World Health Organization. (2015). World report on ageing and health. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World Health Organization Press.
- World Health Organization. (2017). The Republic of Indonesia health system review. Health Systems in Transition, 7(1), i-292. Retrieved from http://apps.who.int/iris/bitstream/10665/254716/1/9789290225164-eng.pdf.