Abstract
Objectives
To provide prevalence estimates of needs of people with dementia living at home, and to determine sources of variation associated with needs for this population.
Method
A systematic review and meta-analysis was performed searching CINAHL, MEDLINE, PsycINFO and ASSIA databases. Following quality checks, random effects meta-analysis produced prevalence estimates for needs reported by people with dementia and by their informal caregivers. Fixed effects models were undertaken to compare caregiver and person with dementia reported needs. Heterogeneity was explored through sensitivity analysis. The study protocol was registered with Prospero #CRD42017074119
Results
Six retrieved studies published between 2005 and 2017 including 1011 people with dementia and 1188 caregivers were included in the analysis. All data were collected using Camberwell Assessment of Need for the Elderly. Prevalence estimates are provided for 24 needs reported by participants in The Netherlands, United Kingdom, Poland, Ireland, Germany, Norway, Portugal, Italy and Sweden. Most prevalent needs reported by people with dementia were Memory 0.713 [95% CI 0.627, 0.791]; Food 0.706 [95% CI 0.547, 0.842]; Household activities 0.677 [95% CI 0.613, 0.738]; and Money 0.566 [95% CI 0.416, 0.711]. Caregivers reported greater prevalence than people with dementia did for 22 of 24 needs, although the priority ranking of needs was similar. Exploration of heterogeneity revealed that people with young onset dementia were the major source of variation for 24 out of 48 analyses.
Conclusion
Increased understanding of prevalence of needs of people with dementia and associated heterogeneity can assist in planning services to meet those needs.
Introduction
It is known that people with dementia experience a wide range of intense care needs (Prince et al., Citation2015), which vary depending on many factors including the type and severity of cognitive impairment, functional dependencies, multi-morbidities and neuropsychiatric symptoms. These needs, which can be defined as capacity to benefit from services (NHS Health Scotland, Citation2019), are therefore specific to the individual and strongly affect health outcomes. Also, needs are interrelated with risks (Seden, Citation2016), and unmet needs can result in adverse consequences such as falls, dehydration, lower quality of life, caregiver burden, institutionalisation and death (Black et al., Citation2013; Gaugler, Kane, Kane, & Newcomer, Citation2005).
In order to provide appropriate care and support for the increasing number of people with dementia (Prince et al., Citation2015), consideration of information about the complexity of individuals’ needs can enable clinicians to provide services tailored towards their goals and priorities (Farmer, Fenu, O'Flynn, & Guthrie, Citation2016; Morrisby, Joosten, & Ciccarelli, Citation2018). However, there is a gap between the required intervention and care, and the services provided for people with dementia (World Health Organization, Citation2017). One research study examining the needs of older people with severe mental illness including dementia, found that most (70%) people were not receiving the interventions indicated by their assessed needs (Cummings & Kropf, Citation2009). This may be due to the assessed needs not being specific enough to link to particular interventions (Schmid, Eschen, Rüegger-Frey, & Martin, Citation2012), for example, mobility needs may require physiotherapy or wheelchair repair services. Alternatively, this may result from a failure to develop services that meet the needs of people with dementia (Knapp et al., Citation2007).
In order to reorganise care to account for the needs of people with dementia, further knowledge is required to facilitate understanding of the burden of dementia and its co-morbidities, and how this burden relates to intervention. To this end, individual studies have presented data regarding the frequency and range of needs of people with dementia (Morrisby et al., Citation2018). However, this data have not been synthesised and the universality of these results is unknown. Quantitative synthesis of data enables exploration of any associated heterogeneity (Song, Sheldon, Sutton, Abrams, & Jones, Citation2001). This can provide information regarding sources of variation in the needs of people with dementia, and contribute to understanding of characteristics associated with increased frequency of reported needs.
Further, research regarding variation in reported needs will assist in targeting services and resources to where they are most required (Gitlin, Maslow, & Khillan, Citation2018). Informing the efficient organization and delivery of health and social care to manage the complex and diverse requirements of people with dementia can lead to more integrated and person-centred support, addressing actual needs of people with dementia and their caregivers, thereby reducing adverse outcomes including institutionalisation (Banerjee, Citation2015).
Therefore, in order to enhance understanding regarding the needs of people with dementia, the authors conducted a systematic review and meta-analysis of existing studies following Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Electronic Supplementary Material 1) (Liberati et al., Citation2009).
The objectives of this review and meta-analysis were to (a) establish prevalence estimates of needs reported by people with dementia living at home, and by their informal caregivers; (b) compare the prevalence estimates of needs reported by people with dementia to those reported by informal caregivers of people with dementia; (c) quantify and explore heterogeneity associated with these prevalence estimates.
Methods
The review protocol was registered a priori and published online in the PROSPERO database of systematic reviews (www.crd.york.ac.uk/Prospero. registration number #CRD42017074119).
Inclusion and exclusion criteria
Studies were included if; (a) they reported empirical prevalence data regarding the frequency of needs for people with dementia; (b) participants had a diagnosis of dementia; (c) participants were living at home in the community; (d) needs were measured using a validated assessment instrument; (e) needs were identified as concerning the person with dementia and not their caregiver or other significant person; (f) needs were reported by the person with dementia or by their informal caregiver; and (g) the study was reported in English. All study designs and methodologies were included. To allow for exploration of factors that may affect needs, all age groups and dementia diagnoses were included, as were all publication dates and all geographical areas.
Studies that were reviews or conference proceedings or reported only qualitative data were excluded. Articles providing further information on studies selected for inclusion in the analysis were used in the assessment of the quality of the selected studies.
Search strategy
A systematic search of four databases, ASSIA, CINAHL, MEDLINE and PsycINFO was conducted (EC) to identify studies in which the needs of people with dementia living at home were quantitatively examined. The CINAHL, MEDLINE and PSYCinfo databases were searched through EBSCOhost using the following terms as Medical Subject Headings (MESH) and keywords; (1) Dementia OR Frontotemporal Dementia OR Dementia, Vascular OR Delirium, Dementia, Amnestic, Cognitive Disorders OR Dementia, Multi-infarct OR AIDS Dementia Complex OR Dementia, Senile OR Dementia, Presenile OR Lewy Body Disease OR Parkinson Disease OR Alzheimer’s disease, AND (2) Needs Assessment OR Health services needs and demand. The ASSIA database was searched through PROQUEST using the above terms as main subjects. Further relevant studies were identified through hand searching reference lists (EC).
Study selection
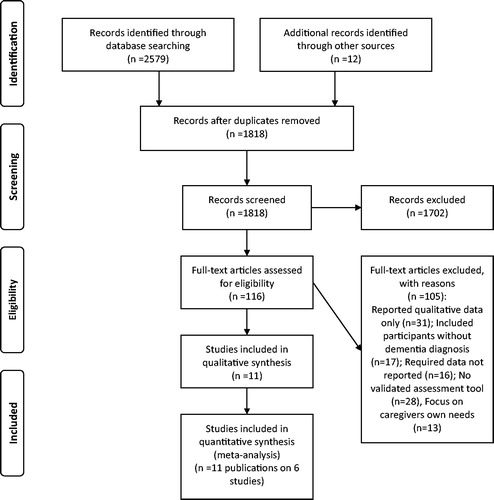
Following removal of duplicates, titles of the returned articles were examined and irrelevant titles were excluded. Abstracts, then full text of the remaining articles were reviewed to find studies that met the inclusion criteria. Two researchers (EC, SA) selected studies independently to minimise selection bias, results were compared and disagreements were resolved through discussion and with reference to inclusion criteria. If no agreement could be reached it was planned a third team member (DM) would decide, but this was unnecessary. The screening process is described in .
Data extraction
A data extraction sheet was developed and pilot tested. Two research team members independently extracted the following data from included studies; (a) characteristics of the study participants including age, diagnosis, living situation; (b) study details including author, title, date of publication; (c) setting; (d) methodological characteristics; (e) outcome measurement tool; (f) outcome data; (g) ethical approval; and (h) data analysis. (EC, SA). Results were compared and inconsistencies were resolved through discussion between the two research team members, and discussion with a third team member (DM) was again unnecessary. Data originating from the same study was included as one study even if reported in more than one paper, to prevent bias. Corresponding authors were contacted where required data were not present, for example when the paper reported only met or unmet need rather than total need. Three authors responded to this request and two provided further data regarding the frequency of reported needs.
Quality assessment
Studies included in this analysis were assessed for risk of bias using the Prevalence Critical Appraisal Instrument (Munn, Moola, Riitano, & Lisy, Citation2014). This assessment focused on (a) the instrument used to assess the needs of the person with dementia and (b) the sampling of the population within the study, as these are issues particularly relevant to prevalence studies. To minimise bias two research team members completed the tool independently for each study (EC, SA) then compared and discussed results. Disagreements were to be resolved through discussion with a third team member (DM) but this was unnecessary. All studies were included in the meta-analysis, and leave1out sensitivity analysis was undertaken to explore heterogeneity (Stroup et al., Citation2000). Details of information considered in the quality appraisal instrument is included in Electronic Supplementary Material 2.
Statistical analyses
The primary measure of prevalence was proportion of people with dementia reporting a specific need. Needs frequency data presented as percentages were recalculated as proportions. Where needs were reported as unmet and met needs, these data were combined to create total need. Proportions were pooled for meta-analysis, using a double arcsine square root transformation, to normalise the sampling distribution and stabilise variation (Barendregt, Doi, Lee, Norman, & Vos, Citation2013; Freeman & Tukey, Citation1950; Wang, Citation2017). The double arcsine square root transformation was selected due to the small sample sizes and extreme proportions involved (Wang, Citation2017). Following analysis, the final pooled estimates with 95% confidence intervals (95% CI) were back-transformed for ease of interpretation (Miller, Citation1978).
Data on each of the 24 needs reported by people with dementia and 24 needs of people with dementia reported by informal caregivers were analysed separately. DerSimonian Laird random-effects models (DerSimonian & Laird, Citation1986) were performed as they are recommended for the meta-analysis of prevalence data to allow for between-study variation and to increase the generalizability of conclusions (Munn, Moola, Lisy, & Riitano, Citation2014).
In order to determine if data on the needs of people with dementia reported by the person themselves differed from data on their needs as reported by their caregivers, it was necessary to compare the results of the random-effects meta-analyses for each need type. Fixed-effects models were fitted to allow comparison of the two estimates for each of the 24 need types, as the residual heterogeneity within each subset had already been accounted for through fitting the random-effects model (Viechtbauer, Citation2010).
Risk of bias across studies
Publication bias refers to the number of statistically non-significant studies remaining unpublished. However, studies included in meta-analysis of proportions are observational, non-comparative, and do not calculate significance levels for their results. Therefore, statistical non-significance was unlikely to result in publication bias (Wang, Citation2017).
Additional analyses
Heterogeneity is expected in prevalence studies and can arise for a number of reasons including: different instruments used to determine the presence of a variable, geographical variation, and differences in the study population (Higgins, Citation2008; Munn, Moola, Riitano, et al., Citation2014). Whilst meta-analysis is used to pool effects, another important benefit is the investigation and description of heterogeneity (Higgins, Citation2008; Song et al., Citation2001; Thompson, Citation1994). Following inspection of the meta-analysis output, heterogeneity was formally tested using the inconsistency index I2 to measure the proportion of the observed variation due to its sensitivity to true heterogeneity (Higgins, Thompson, Deeks, & Altman, Citation2003), and insensitivity to number of studies (Wang, Citation2017). Leave1out sensitivity analyses were performed to identify sources of variation (Higgins, Citation2008; Ryan & Cochrane Consumers & Communication Review Group, Citation2016; Viechtbauer, Citation2010). All analyses were conducted using the Metafor package in R Studio software (R Core Team, Citation2017; Viechtbauer, Citation2010).
Results
The database search returned 2579 articles. A further 12 papers were identified through hand searching and review of citation lists. Review of title and abstracts resulted in 116 potentially relevant papers being identified for full text review. Of these, 11 papers describing six studies met the inclusion criteria and were retained for review. Ineligible studies included studies that failed to report the frequency of needs, included participants without a dementia diagnosis, or did not use a validated needs assessment tool. Retrieved papers were published between 2005 and 2017 (). The databases were last accessed on 04/06/2019.
Table 1. Study characteristics.
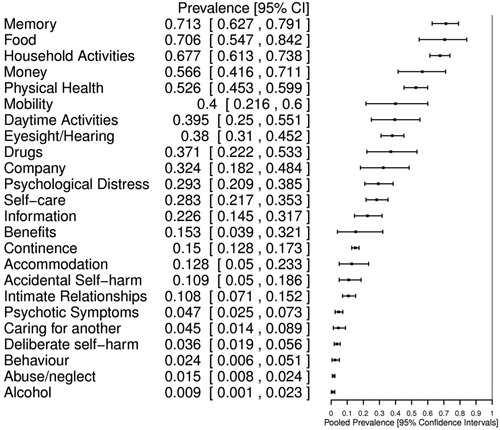
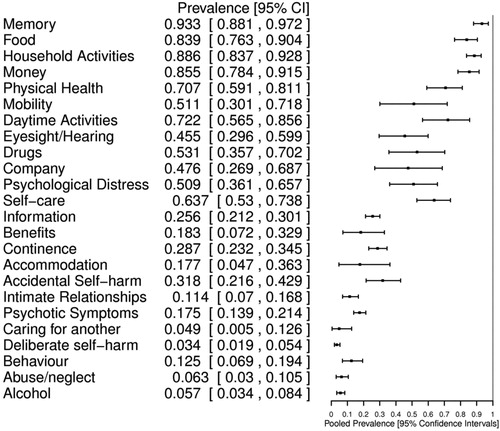
Results of the meta-analyses were based on data relating to twenty-four needs of people with dementia, as reported by 1011 people with dementia and 1188 informal caregivers. Data were extracted from reports of six studies undertaken in The Netherlands, UK, Poland, Ireland, Germany, Norway, Portugal, Italy and Sweden. The forty-eight needs prevalence estimates ranged from 0.933 [95% CI 0.881, 0.972] for caregiver reported memory needs, to 0.009 [95% CI 0.001, 0.023] for person with dementia reported alcohol related needs, and varied depending upon need type and the person reporting the needs ().
Table 2. Prevalence estimates of reported needs.
Study characteristics
Characteristics of retrieved studies are presented in . Non-randomized sampling methods were employed in all studies, and two studies used convenience sampling methods. All retrieved studies collected needs data using validated versions of the Camberwell Assessment of Need for the Elderly (CANE) (Reynolds et al., Citation2000), although three different language versions; English, Dutch and Polish. The need domains of the original (English language) version of the CANE are presented in Electronic Supplementary Material 3. Other needs assessment tools were identified in the literature, but studies did not meet the inclusion criteria for this analysis as either reported data were incomplete and authors could not be contacted, or there was no available validation information for the needs assessment tool used within the study.
Prevalence of needs
Prevalence estimates for the 24 CANE need domains, reported by people with dementia, and by caregivers of people with dementia, are presented as proportions, together with 95% confidence intervals (CI) (). The combined estimated prevalence with 95% confidence intervals are visualised for each need reported by people with dementia (), and by caregivers ().
Comparison of needs reported by people with dementia and needs reported by caregivers
Caregivers of people with dementia reported higher levels of need for people with dementia in 23 out of 24 needs. These two sets of effects sizes were compared in twenty-four fixed effects models (). Results were significantly different for Household Activities (−0.255, p < .001), Memory (−0.297, p < .001), Self-care (−0.361, p < .001), Continence (−0.166, p < .001)), Psychotic Symptoms (−0.210, p < .001), Money (−0.324, p < .001), Alcohol (−0.137, p < .001), Abuse/neglect (−0.125, p = .002), Accidental Self-harm (−0.259, p = .001), Daytime activities (−0.332, p = .004) and Behaviour (−0.202, p < .001). People with dementia and caregivers reported a similar level of need for Deliberate Self-harm (0.0, p = .989).
In one study 27.3% of participants with dementia were unable to answer CANE questions (Bakker et al., Citation2014a). Another study found 17.8% of their participants with dementia were unable to understand CANE questions, and that this group was significantly more cognitively and functionally impaired than the rest of the sample (Miranda-Castillo, Woods, & Orrell, Citation2013). Hence, the needs of this group of people with dementia could only be reported by caregivers, and therefore dementia severity or the inability to comprehend the CANE questions may have contributed to the heterogeneity between the needs reported by people with dementia and by caregivers.
Heterogeneity
Meta-analyses showing very low heterogeneity (I2 = 0%) (Ryan & Cochrane Consumers & Communication Review Group, Citation2016) included two needs reported by people with dementia: Continence I2 = 0% [95% CI 0, 0] ; and Abuse/neglect I2 = 0% [95% CI 0, 82.469] . Notably, these needs had very low prevalence ( < 0.05). As prevalence estimates are reported with 95% confidence intervals, the degree of heterogeneity of these results remains uncertain (Wang, Citation2017). Seventeen of the 24 meta-analyses examining the needs reported by people with dementia, exhibited considerable heterogeneity (I2 > 75%) (Alba et al., Citation2016; Higgins et al., Citation2003). Eighteen of the 24 meta-analyses examining the needs of people with dementia reported by caregivers also exhibited high heterogeneity. Heterogeneity (I2) is reported in .
As it is important to explore and quantify heterogeneity and always bearing in mind that heterogeneity may be due to chance (Thompson, Citation1994), sensitivity analyses were employed to determine the study that was the major source of heterogeneity for each of the meta-analyses (Higgins, Citation2008) (). Following sensitivity analysis, 12 of 24 person with dementia reported needs, and nine of 24 caregiver reported needs showed unimportant or moderate heterogeneity (I2 ≤ 60%) (Koletsi, Fleming, Michelaki, & Pandis, Citation2018).
In 24 of 46 meta-analyses demonstrating heterogeneity, removal of the Bakker (Bakker et al., Citation2014a) study data produced the greatest reduction in variation indicating that a characteristic of this study or its sample population was the source of this variation. This study reported data on the needs of people with young onset dementia, with a mean age of 61.1 years. The other studies included in this analysis had populations with mean ages ranging from 76.6 to 79.8 years. Notably, heterogeneity in Daytime activity and Accommodation needs reported by people with dementia, reduced by 95.43% and 94.07% respectively, to 0% following removal of Bakker study data from the analysis. Removal of Bakker study data resulted in reduced prevalence estimates indicating higher levels of need associated with young onset dementia. The greatest reduction occurred in the prevalence estimates of Daytime activities and Accommodation needs for people with later onset dementia which decreased to 0.317 [95% CI 0.286, 0.349] and 0.090 [95% CI 0.071, 0.110] respectively. Similarly, variation in caregiver reported need domains of Food; and Deliberate self-harm, reduced by 68.47% and 49.98%, respectively, when this data were removed from the analysis. Resultant prevalence estimates obtained following removal of the study which was identified as the major source of variation are presented in Electronic Supplementary Materials 4.
Discussion
Despite global challenges associated with meeting care needs of people with dementia living at home, the authors believe that this meta-analysis is the first to establish prevalence of needs for this population. It has produced 48 prevalence estimates that reflect the pooled burden of need experienced by the dementia populations of six research studies conducted in The Netherlands, UK, Poland, Ireland, Germany, Norway, Portugal, Italy and Sweden. These outcomes are of interest as needs can lead to someone being put at risk of adverse outcomes including increased multi-morbidity (Levene et al., Citation2017; Seden, Citation2016). Therefore, greater understanding of these needs and the priority placed upon them by people with dementia and their informal caregivers, can inform the design of services to ensure they are person-centred, rather than disease focused. Accurate, descriptive information regarding the needs of people with dementia and differences in their dementia care trajectories, together with details of characteristics which impact care needs, will inform effective service plans (Gitlin et al., Citation2018). This will result in these needs being more effectively managed (Morrisby et al., Citation2018) which, in turn, may reduce the detrimental effects of unmet needs.
As indicated by Munn, Moola, Riitano, et al. (Citation2014) the needs assessment instrument and the sampling of the population within the study are quality issues particularly relevant to prevalence studies. Overall, the quality of the studies included in this meta-analysis was mixed. Importantly, all studies used a validated instrument for the assessment of needs, and used established criteria for dementia diagnosis. Two studies recruited small purposive samples. Four studies described multiple recruitment approaches of which two reported comparisons of their study population with wider populations. Comparison indicated that these samples contained mainly people with mild or moderate dementia. Two further studies recruited small purposive samples, which were not compared with the wider population, and therefore the representativeness of these samples is unknown. The small number of studies restricted subgroup analysis opportunities, but sensitivity analysis did not indicate that study quality influenced the prevalence reported within these studies.
Resultant prevalence estimates indicate that caregivers believe that over 90% of people with dementia experience at least one need. This study also confirms that people with dementia and caregivers identified similar need priorities for the person with dementia living at home. The most prevalent needs for people with dementia and their caregivers (Food, Household activities, Memory and Money) matched, although they differed in order of presentation. Previous research indicates that distinct populations such as people with dementia living in care homes, and elderly people without dementia reported different need priorities (Orrell et al., Citation2008; Stein, Luppa, König, & Riedel-Heller, Citation2015)
Due to a limited number of studies reporting prevalence data on the needs of people with dementia, and the different ways in which data are reported, it is difficult to directly relate the results of this meta-analysis with other prevalence estimates. However, in order to enhance their credibility and validity, results are compared with available published prevalence data derived from alternative methods. As the literature does not consider prevalence of all the needs of people with dementia living at home this ‘will focus upon self-care; continence; mobility and falls; drugs; abuse/neglect; and psychological distress needs.
A study, which used CarenapD needs assessment tool found people with dementia, reported high levels of self-care needs (Meaney, Croke, & Kirby, Citation2005). CarenapD domains do not directly overlap with CANE need domains and Meaney et al. (Citation2005) found 80% of people with dementia reported dental care needs, 79% had bathing needs, and 68% identified toileting needs, all of which can be considered self-care needs. Similarly, people with dementia living in Hong Kong reported prevalence estimated at 29.6%, 59% and 76.9% for bathing needs for people who are at the early, middle or late stage of dementia respectively, using the CarenapD needs assessment instrument (Chung, Citation2006). Hence, the prevalence estimates for person with dementia reported self-care needs from the current study are similar to Chung’s estimate for people in the early stages of dementia, whereas prevalence of the current study’s caregiver reported self-care needs is closer to the estimate provided by Meaney et al. (Citation2005), and Chung’s estimate for people in the middle stages of dementia.
There are no prevalence studies of people with dementia living at home with incontinence needs (Drennan, Cole, & Iliffe, Citation2011). However, 31% of home-dwelling people over the age of 75 in the UK have urinary incontinence problems (Rait et al., Citation2005), and 31% of caregivers of people with dementia in Australia manage incontinence and pads (Drennan et al., Citation2011). These estimates are higher than the prevalence estimate for continence needs in the current study. In addition, Chung (Citation2006) reports prevalence of continence needs ranged from 11.3% to 46.2% for people at different stages of dementia. Again, the current study’s prevalence estimate for people with dementia reported needs is convergent with the estimate for people who are at an early stage of dementia from the Chung study.
The estimated prevalence of mobility and fall related needs from the current study is comparable with data on the number of falls experienced by people with Alzheimer’s disease. Allan, Ballard, Rowan, and Kenny (Citation2009) found a history of falls within the previous year for 51.4% of people with Alzheimer’s disease.
The prevalence estimate for drug related needs is credible given that 49.02% of people with dementia required assistance with medication administration (Bowen, Gonzalez, Edwards, & Lippa, Citation2014), and polypharmacy is observed in 50% of elderly patients (Leelakanok & D'Cunha, Citation2018).
Prevalence estimates of behavioural and psychological symptoms associated with dementia reported in the literature range from 50 to 100% (Devshi et al., Citation2015). The prevalence estimate for caregiver reported psychological distress needs is comparable with the lower end of this range, and this proportion would likely rise when other relevant needs such as accidental self-harm, deliberate self-harm, behaviour, alcohol, and psychotic symptoms were taken into account.
Significant abuse occurs in more than a quarter of people with dementia (Cooper, Manela, Katona, & Livingston, Citation2008). Overall elder abuse is estimated at 15.7% [95% CI 12.8, 19.3] (Yon, Mikton, Gassoumis, & Wilber, Citation2017), therefore the prevalence of abuse/neglect estimate from person with dementia reports and from caregiver reports from the current study are low. This variation may result from the method used to obtain data as rates of abuse detected using objective measures are around 5% (Cooper, Selwood, & Livingston, Citation2008), which is in line with the estimate from the current study.
Overall, the convergence between the results of this study and published data lend them credibility, although it was not possible to identify data for comparison with all of the reported needs. Generally, the needs prevalence estimates produced within this study are low when compared with other published data possibly because they reflect the needs of people with dementia experiencing mild or moderate cognitive and functional impairment.
The present study also revealed variation in needs prevalence was associated with who reported the needs, and fixed effects analyses confirmed that caregivers reported higher levels of need for 23 of the 24 needs. This may be a result of people with more severe cognitive and functional impairment being unable to answer CANE questions. Hence, higher levels of need reported by caregivers may reflect the needs of a population that includes more people with severe dementia. As the CarenapD does not distinguish between caregiver and person with dementia reported needs, this may explain the increased needs frequencies obtained using this assessment tool. Notably, informal caregivers of people with dementia living in care homes (Orrell et al., Citation2008; van der Ploeg, Bax, Boorsma, Nijpels, & van Hout, Citation2013), and of people with dementia attending daycare (van Haeften-van Dijk, Meiland, Hattink, Bakker, & Dröes, Citation2016) also reported greater needs prevalence than people with dementia.
In order to reorganise integrated health and social care services to meet the needs of people living with dementia in a meaningful way, there must be greater understanding of the diversity of needs within this population (Commisso et al., Citation2017; Farmer et al., Citation2016). Sensitivity analysis indicated that data from the study examining the needs of people with young onset dementia was the major source of variation for 12 person with dementia reported needs, and 12 caregiver reported needs. When this data were removed from the analysis, resultant prevalence estimates were reduced indicating that people with young onset dementia and their caregivers both report higher levels of need than other people with dementia and their caregivers. This may reflect the different life stage, and particular clinical characteristics of this population who received a dementia diagnosis prior to the age of 65 and who form 2.2% of people with dementia in the UK (Knapp et al., Citation2007). People with young onset dementia may be coping with lost self-identity, income and socialisation associated with leaving employment, in addition to the psychological burden of an unexpected diagnosis and role changes associated with becoming a dependent family member (Shuman, Hughes, Wiener, & Gould, Citation2017).
People with young onset dementia have particular daytime activity needs which have been previously noted (Harris & Keady, Citation2004; Millenaar et al., Citation2016), and there is a recognised requirement for day care which provides stimulating activities for people who may be more active, or at a different life stage (Millenaar et al., Citation2016). Additionally, a lack of age-appropriate residential facilities may also have an impact upon accommodation needs for this group (Bakker et al., Citation2013). Higher frequency of benefit related needs were reported by both people with young onset dementia and their caregivers perhaps reflecting the impact of young-onset dementia on employment for both people with dementia and their caregivers.
The presented prevalence estimates have particular relevance for service planning. For example, information regarding psychological needs including Psychotic symptoms, Deliberate self-harm and Psychological distress indicate the level of specialist mental health support required by people with dementia as these needs are most likely to be met through formal support services (Cummings & Kropf, Citation2009). Prevalence estimates of environmental needs such as Benefits, Money and Accommodation also have direct implications for social policy and service provision. For other needs, which perhaps require less specialist interventions such as household activities and food, prevalence estimates can indicate sources of difficulty and additional burden often shouldered by informal caregivers. In some cases, CANE domains may be too generic to link to specific interventions or services (Cummings & Kropf, Citation2009; Schmid et al., Citation2012). Therefore, there is a requirement for further work investigating how these needs link with suitable interventions. Exploration of the heterogeneity associated with needs has determined subgroups of people with dementia experiencing specific needs prevalence. It may also be useful to explore associations with variation in met and unmet needs to inform understanding in this regard. This in turn will increase knowledge regarding the provision of interventions that meet the needs of people with dementia.
Limitations
Limitations of this study include the low number of published studies retrieved despite extensive searching. Further, some retrieved studies had small sample sizes and confidence intervals reflect this. All needs data were elicited using CANE, which does not consider educational or vocational needs, however Schmid et al. (Citation2012) found it was the best of the available needs assessment instruments for people with dementia. Results indicate that participants mostly had mild or moderate dementia, and few had severe dementia in part because they were unable to understand CANE questions. Study data were collected from nine European countries. Findings support Morrisby et al. (Citation2018) who claimed that experience is shared across countries and service models. However, data from outside Europe is required to understand the international relevance of results. There was high residual unexplored heterogeneity for a number of the analyses (Ryan & Cochrane Consumers & Communication Review Group, Citation2016).
Conclusion
This study quantifies prevalence estimates of twenty-four needs of people with dementia living at home, as reported by people with dementia and their caregivers, for the first time. Overall, analyses confirm that people with dementia and their caregivers prioritise the same needs, however, caregivers of people with dementia report higher levels of need than people with dementia report themselves, although this may be due to people with severe dementia being unable to complete the needs assessment. Synthesis of results provides evidence of sources of heterogeneity in reported needs including the effects of the person reporting the needs, and age of dementia onset. Understanding prevalence and type of needs experienced by people with dementia, and circumstances in which needs vary can assist in targeting resources to meet the unique range of needs experienced by an individual, hence reducing adverse outcomes for individual patients (Guthrie, Payne, Alderson, McMurdo, & Mercer, Citation2012; Schmid et al., Citation2012).
Supplemental Material
Download MS Word (18.8 KB)Supplemental Material
Download MS Word (13.2 KB)Supplemental Material
Download MS Word (17.7 KB)Supplemental Material
Download MS Word (17.2 KB)Acknowledgements
The authors would like to thank colleagues within Firefly Research, Queen Margaret University, Edinburgh, particularly Stella Arakelyan and Anusua Singh-Roy, for their support and feedback.
Disclosure statement
The authors report no conflict of interest.
References References marked with an asterisk indicate studies included in the meta-analysis
- Alba, A. C., Alexander, P. E., Chang, J., MacIsaac, J., DeFry, S., & Guyatt, G. H. (2016). High statistical heterogeneity is more frequent in meta-analysis of continuous than binary outcomes. Journal of Clinical Epidemiology, 70, 129–135. doi:10.1016/j.jclinepi.2015.09.005
- Allan, L. M., Ballard, C. G., Rowan, E. N., & Kenny, R. A. (2009). Incidence and prediction of falls in dementia: A prospective study in older people. PLoS One, 4(5), e5521. doi:10.1371/journal.pone.0005521
- *Bakker, C., de Vugt, M. E., van Vliet, D., Verhey, F. R. J., Pijnenburg, Y. A., Vernooij-Dassen, M., & Koopmans, R. T. C. M. (2014a). The relationship between unmet care needs in young-onset dementia and the course of neuropsychiatric symptoms: A two-year follow-up study. International Psychogeriatrics, 26(12), 1991–2000. doi:10.1017/S1041610213001476
- *Bakker, C., de Vugt, M. E., van Vliet, D., Verhey, F., Pijnenburg, Y. A., Vernooij-Dassen, M., & Koopmans, R. T. C. M. (2014b). Unmet needs and health-related quality of life in young-onset dementia. The American Journal of Geriatric Psychiatry, 22(11), 1121–1130. doi:10.1016/j.jagp.2013.02.006
- *Bakker, C., de Vugt, M. E., van Vliet, D., Verhey, F. R. J., Pijnenburg, Y. A., Vernooij-Dassen, M., & Koopmans, R. T. C. M. (2013). Predictors of the time to institutionalization in young- versus late-onset dementia: Results from the needs in young onset dementia (NeedYD) study. Journal of the American Medical Directors Association, 14(4), 248–253. doi:10.1016/j.jamda.2012.09.011
- Banerjee, S. (2015). A narrative review of evidence for the provision of memory services. International Psychogeriatrics, 27(10), 1583–1592. doi:10.1017/S1041610215000149
- Barendregt, J. J., Doi, S. A., Lee, Y. Y., Norman, R. E., & Vos, T. (2013). Meta-analysis of prevalence. Journal of Epidemiology and Community Health, 67(11), 974–978. doi:10.1136/jech-2013-203104
- Black, B. S., Johnston, D., Rabins, P. V., Morrison, A., Lyketsos, C., & Samus, Q. M. (2013). Unmet needs of community-residing persons with dementia and their informal caregivers: Findings from the maximizing independence at home study. Journal of the American Geriatrics Society, 61(12), 2087–2095. doi:10.1111/jgs.12549
- Bowen, K. J., Gonzalez, E. W., Edwards, C. Y., & Lippa, C. F. (2014). Needs assessments of memory disorder patients. American Journal of Alzheimer's Disease & Other Dementias, 29(8), 667–672. doi:10.1177/1533317514534952
- Chung, J. C. C. (2006). Care needs assessment of older Chinese individuals with dementia of Hong Kong. Aging & Mental Health, 10(6), 631–637. doi:10.1080/13607860600650532
- Commisso, E., McGilton, K. S., Ayala, A. P., Andrew, M.,K., Bergman, H., Beaudet, L., … Puts, M. T. E. (2017). Identifying and understanding the health and social care needs of older adults with multiple chronic conditions and their caregivers: A protocol for a scoping review. BMJ Open, (7(12), e018247–6. doi:10.1136/bmjopen-2017-018247
- Cooper, C., Manela, M., Katona, C., & Livingston, G. (2008). Screening for elder abuse in dementia in the LASER-AD study: Prevalence, correlates and validation of instruments. International Journal of Geriatric Psychiatry, 23(3), 283–288. doi:10.1002/gps.1875
- Cooper, C., Selwood, A., & Livingston, G. (2008). The prevalence of elder abuse and neglect: A systematic review. Age and Ageing, 37(2), 151–160. doi:10.1093/ageing/afm194
- Cummings, S. M., & Kropf, N. P. (2009). Formal and informal support for older adults with severe mental illness. Aging & Mental Health, 13(4), 619–627. doi:10.1080/13607860902774451
- DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7(3), 177–188. doi:10.1016/0197-2456(86)90046-2
- Devshi, R., Shaw, S., Elliott-King, J., Hogervorst, E., Hiremath, A., Velayudhan, L., … Bandelow, S. (2015). Prevalence of behavioural and psychological symptoms of dementia in individuals with learning disabilities. Diagnostics ( Diagnostics), 5(4), 564–576. doi:10.3390/diagnostics5040564
- Drennan, V. M., Cole, L., & Iliffe, S. (2011). A taboo within a stigma? A qualitative study of managing incontinence with people with dementia living at home. BMC Geriatrics, 11(1), 1–7. doi:10.1186/1471-2318/11/75
- Droes, R., van Hout, H. P. J., & van der Ploeg, E. S. (2004). Camberwell assessment of need for the elderly (CANE), revised version (IV). Retrieved from http://www.ouderenpsychiatrie.nl/sjablonen/1/infotype/news/newsitem/view.asp?objectID%20=%201190.
- Farmer, C., Fenu, E., O'Flynn, N., & Guthrie, B. (2016). Clinical assessment and management of multimorbidity: Summary of NICE guidelines. BMJ, 354i, 4843.
- Freeman, M., & Tukey, J. (1950). Transformation related to the angular and the square root. The Annals of Mathematical Statistics, 21(4), 607–611. doi:10.1214/aoms/1177729756
- Freyne, A., Dolan, M., & Cooney, C. (2010). Carer-rated needs assessment of a cohort of people with dementia. Irish Journal of Psychological Medicine, 27(2), 72–76. doi:10.1017/S0790966700001087
- Gaugler, J. E., Kane, R. L., Kane, R. A., & Newcomer, R. (2005). Unmet care needs and key outcomes in dementia. Journal of the American Geriatrics Society, 53(12), 2098–2105. doi:10.1111/j.1532-5415.2005.00495.x
- Gitlin, L. N., Maslow, K., & Khillan, R. (2018). National research summit on care, services and supports for persons with dementia and their caregivers. Report to the national advisory council on Alzheimer's research, care and services. Bethesda, MD: Research Summit on Dementia Care.
- Guthrie, B., Payne, K., Alderson, P., McMurdo, M. E. T., & Mercer, S. W. (2012). Adapting clinical guidelines to take account of multimorbidity. BMJ (Clinical Research ed.), 345, e6341.doi:10.1136/bmj.e6341
- Harris, P. B., & Keady, J. (2004). Living with early onset dementia: Exploring the experience and developing evidence-based guidelines for practice. Alzheimer's Care Today, 5, 111–122.
- Higgins, J. P. T. (2008). Commentary: Heterogeneity in meta-analysis should be expected and appropriately quantified. International Journal of Epidemiology, 37(5), 1158–1160. doi:10.1093/ije/dyn204
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ (Clinical Research ed.), 327(7414), 557–560. doi:10.1136/bmj.327.7414.557
- *Kerpershoek, L., de Vugt, M., Wolfs, C., Woods, B., Jelley, H., Orrell, M., … Verhey, F., & The Actifare Consortium. (2018). Needs and quality of life of people with middle stage dementia and their family carers from the European Actifare study. When informal care alone may not suffice. Aging & Mental Health, 22(7), 897–902. doi:10.1080/13607863.2017.1390732
- Knapp, M., Prince, M., Albanese, E., Banerjee, S., Dhanasiri, S., Fernandez, J., … Stewart, R. (2007). Dementia UK: The full report. London: UK: Alzheimer's Society.
- Koletsi, D., Fleming, P. S., Michelaki, I., & Pandis, N. (2018). Heterogeneity in Cochrane and non-Cochrane meta-analyses in orthodontics. Journal of Dentistry, 74, 90–94. doi:10.1016/j.dent.2018.05.003
- Leelakanok, N., & D'Cunha, R. R. (2018). Association between polypharmacy and dementia - A systematic review and meta-analysis. Aging & Mental Health, 23(8), 932–941. doi:10.1080/13607863.2018.1468411
- Levene, L. S., Baker, R., Wilson, A., Walker, N., Boomla, K., & Bankart, M. J. G. (2017). Population health needs as predictors of variations in NHS practice payments: A cross-sectional study of English General Practices in 2013-2014 and 2014-2015. British Journal of General Practice, 67(654), e10–e19. doi:10.3399/bjgp16X688345
- Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P. A., … Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Medicine, 6(7), e1000100. doi:10.1371/journal.pmed.1000100
- *Mazurek, J., Szczesniak, D., Urbanska, K., Droes, R., & Rymaszewska, J. (2017). Met and unmet care needs of the elderly with dementia living at home: Personal and informal carers' perspectives. Dementia, 0(0), 1–13. doi:10.1177/1471301217733233
- *Meaney, A. M., Croke, M., & Kirby, M. (2005). Needs assessment in dementia. International Journal of Geriatric Psychiatry, 20(4), 322–329. doi:10.1002/gps.1284
- Millenaar, J. K., Bakker, C., Koopmans, R. T. C. M., Verhey, F. R. J., Kurz, A., & de Vugt, M. E. (2016). The care needs and experiences with the use of services of people with young-onset dementia and their caregivers: A systematic review. International Journal of Geriatric Psychiatry, 31(12), 1261–1276. doi:10.1002/gps.4502
- Miller, J. (1978). The inverse of the Freeman-Tukey double arcsine transformation. The American Statistician, 32(4), 138. doi:10.1080/00031305.1978.10479283
- *Miranda-Castillo, C., Woods, B., & Orrell, M. (2010). People with dementia living alone: What are their needs and what kind of support are they receiving? International Psychogeriatrics, 22(4), 607–617. doi:10.1017/S104161021000013X
- *Miranda-Castillo, C., Woods, B., & Orrell, M. (2013). The needs of people with dementia living at home from user, caregiver and professional perspectives: A cross-sectional survey. BMC Health Services Research, 13(1), 43–43. doi:10.1186/1472-6963-13-43
- *Miranda-Castillo, C., Woods, B., Galboda, K., Oomman, S., Olojugba, C., & Orrell, M. (2010). Unmet needs, quality of life and support networks of people with dementia living at home. Health and Quality of Life Outcomes, 8(1), 132. doi:10.1186/1477-7525-8-132
- Morrisby, C., Joosten, A., & Ciccarelli, M. (2018). Do services meet the needs of people with dementia and carers living in the community? A scoping review of the international literature. International Psychogeriatrics, 30(1), 5–14. doi:10.1017/S1041610217001491
- Munn, Z., Moola, S., Riitano, D., & Lisy, K. (2014). The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. International Journal of Health Policy and Management, 3(3), 123–128. doi:10.15171/ijhpm.2014.71
- Munn, Z., Moola, S., Lisy, K., & Riitano, D. (2014). The synthesis of prevalence and incidence data. Philadelphia: Lippincott Williams and Wilkins.
- NHS Health Scotland. (2019). Understanding needs. Retrieved from www.healthscotland.scot/reducing-health-inequalities/understanding-needs.
- Orrell, M., Hancock, G. A., Liyanage, K. C. G., Woods, B., Challis, D., Hoe, J., … Hoe, J. (2008). The needs of people with dementia in care homes: The perspectives of users, staff and family caregivers. International Psychogeriatrics, 20(05), 941–951. doi:10.1017/S1041610208007266
- Prince, M., Wimo, A., Guerchet, M., Ali, G., Wu, Y., & Prina, M. (2015). World Alzheimer report 2015: The global impact of dementia: An analysis of prevalence, incidence, costs and trends. London: Alzheimer's Disease International. doi:10.1016/j.jalz.2016.07.150
- R Core Team. (2017). R: A language and environment for statistical computing. Retrieved from https://www.R-project.org/.
- Rait, G., Fletcher, A., Smeeth, L., Brayne, C., Stirling, S., Nunes, M., … Tulloch, A. J. (2005). Prevalence of cognitive impairment: Results from the MRC trial of assessment and management of older people in the community. Age and Ageing, 34(3), 242–248. doi:10.1093/ageing/afi039
- Reynolds, T., Thornicroft, G., Abas, M., Woods, B., Hoe, J., Leese, M., & Orrell, M. (2000). Camberwell assessment of need for the elderly (CANE) development, validity, reliability. British Journal of Psychiatry, 174, 444–452. doi:10.1192/bjp.176.5.444
- Ryan, R. & Cochrane Consumers and Communication Review Group. (2016). Heterogeneity and subgroup analyses in Cochrane consumers and communication group reviews: Planning the analysis at protocol stage. Retrieved from http://cccrg.cochrane.org.
- Rymaszewska, J., Klad, R., & Synak, A. (2008). CANE- badanie polskiej wersji narzedzia. [CANE- testing the Polish version of the tool]. Psychogeriatria Polska, 2(5), 105–113.
- Schmid, R., Eschen, A., Rüegger-Frey, B., & Martin, M. (2012). Instruments for comprehensive needs assessment in individuals with cognitive complaints, mild cognitive impairment or dementia: A systematic review. International Journal of Geriatric Psychiatry, 27(4), 329–341. doi:10.1002/gps.2724
- Seden, J. (2016). Social work: Risks, needs and balanced assessments. Milton Keynes, UK: Open University.
- Shuman, S. B., Hughes, S., Wiener, J. M., & Gould, E. (2017). Research on care needs and supportive approaches for persons with dementia. (Background Paper).Research Summit on Dementia Care: Building Evidence for Services and Supports. Retrieved from https://aspe.hhs.gov/national-research-summit-care-services-and-supports-persons-dementia-and-their-caregivers.
- Song, F., Sheldon, T. A., Sutton, A. J., Abrams, K. R., & Jones, D. R. (2001). Methods for exploring heterogeneity in meta-analysis. Evaluation & the Health Professions, 24(2), 126–151. doi:10.1177/016327870102400203
- Stein, J., Luppa, M., König, H., & Riedel-Heller, S. G. (2015). The German version of the Camberwell assessment of need for the elderly (CANE): Evaluation of content validity and adaptation to the German-speaking context. International Psychogeriatrics, 27(11), 1919–1926. doi:10.1017/S104161021500054X
- Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D., … Thacker, S. B. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA, 283(15), 2008–2012. doi:10.1001/jama.283.15.2008
- Thompson, S. G. (1994). Why sources of heterogeneity in meta-analysis should be investigated. BMJ, 309(6965), 1351–1355. doi:10.1136/bmj.309.6965.1351
- van der Ploeg, E. S., Bax, D., Boorsma, M., Nijpels, G., & van Hout, H. P. J. (2013). A cross-sectional study to compare care needs of individuals with and without dementia in residential homes in the Netherlands. BMC Geriatrics, 13(1), 51–51. doi:10.1186/1471-2318-13-51
- *van der Roest, H. G., Meiland, F. J. M., Comijs, H. C., Derksen, E., Jansen, A. P. D., van Hout, H. P. J., … Dröes, R.-M. (2009). What do community-dwelling people with dementia need? A survey of those who are known to care and welfare services. International Psychogeriatrics, 21(05), 949–965. doi:10.1017/S1041610209990147
- *van der Roest, H. G., Meiland, F. J. M., van Hout, H. P. J., Jonker, C., Dröes, R., van der Roest, H. G., … Dröes, R. (2008). Validity and reliability of the Dutch version of the Camberwell Assessment of Need for the Elderly in community-dwelling people with dementia. International Psychogeriatrics, 20(06), 1273–1290. doi:10.1017/S1041610208007400
- van Haeften-van Dijk, A. M., Meiland, F. J. M., Hattink, B. J. J., Bakker, T. J. E. M., & Dröes, R. (2016). Community day care with carer support versus usual nursing home-based day care: Effects on needs, behavior, mood, and quality of life of people with dementia. International Psychogeriatrics, 28(4), 631–645. doi:10.1017/S1041610215001921
- Viechtbauer, W. (2010). Conducting meta-analyses in R with the Metafor package. Journal of Statistical Software, 36(3), 1–48. doi:10.18637/jss.v036.i03
- Wang, N. (2017). Conducting meta-analyses of proportions in R. Retrieved from www.wangnaike.com.
- World Health Organization. (2017). Global action plan on the public health response to dementia 2017-2025. Geneva: World Health Organization.
- Yon, Y., Mikton, C. R., Gassoumis, Z. D., & Wilber, K. H. (2017). Elder abuse prevalence in community settings: A systematic review and meta-analysis. Lancet Global Health, 5(2), e147–156. doi:10.1016/S2214-109X(17)30006-2