Abstract
Objective: There is limited understanding about how people in the severe stages of Alzheimer’s disease (AD) experience and demonstrate awareness. We synthesised all available evidence with the aim of understanding how awareness is preserved or impaired in severe AD and what evidence there is for different levels of awareness according to the levels of awareness framework.
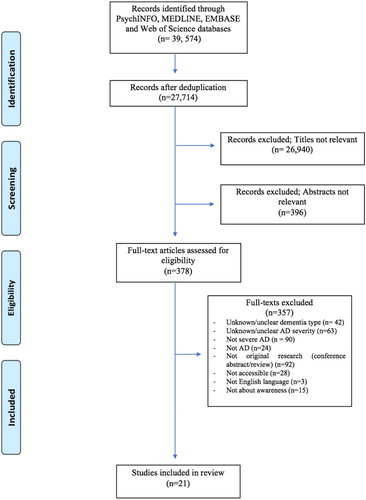
Method: A systematic search of the following databases: Embase, PsycINFO, MEDLINE and Web of Science was carried out. A narrative synthesis and analysis was conducted of all included studies. All studies were assessed for quality using the AXIS and CASP tools.
Results: Our findings suggest that lower level sensory awareness is relatively maintained in severe AD. Findings for higher level awareness are variable and this may be related to the diversity of methods that have been used to explore awareness in these circumstances.
Conclusion: Awareness is complex, heterogeneous and varies significantly between individuals. Environmental and contextual factors have a significant impact on whether awareness is observed in people with severe AD. Adaptation of the environment has the potential to facilitate the expression of awareness while education of caregivers may increase understanding of people with severe AD and potentially improve the quality of care that is received.
Introduction
It is estimated that 12.5% of people with Alzheimer’s disease (AD) are in the severe stages of the dementia (The World Alzheimer Report, Citation2013). At this stage, severe cognitive and functional deficits mean independent living is no longer possible and full time professional care is usually required. One of the observed impairments relates to a lack of awareness. Awareness has been defined as the ‘ability to hold a reasonable or realistic perception or appraisal of, and/or respond accordingly to, a given aspect of one’s environment, situation, functioning or performance’ (Clare, Citation2010). Awareness is a multidimensional construct, proposed to exist on a number of hierarchically operating levels (Stuss, Picton, & Alexander, Citation2001). To conceptualise this hierarchy, Clare and colleagues (2011) developed the ‘levels of awareness framework’ with reference to the structure of existing models of consciousness, where levels of awareness are differentiated by complexity. The framework contains four levels of awareness phenomena, from lower level awareness, sensory registration, to higher level awareness including: performance monitoring, evaluative judgement and meta-representation. A strength of this framework is that it attempts to categorise different aspects of awareness according to complexity (e.g. awareness of being touched versus being aware of changes in ability due to dementia). Importantly, it also takes into account of cognitive, psychosocial and environmental influences on awareness. This holistic approach has been considered to be an important component when developing tailored and effective interventions (Sunderaraman & Cosentino, Citation2017).
Sensory registration
Sensory registration is the lowest form of awareness in the framework requiring only the acknowledgement of, and response to, sensory stimuli (e.g. sound and touch). Sensory awareness is most commonly assessed by self-reports or subjective accounts (Clare, Marková, Verhey, & Kenny, Citation2005). However, these methods are often inappropriate for people with severe AD, who have impaired cognition and verbal communication abilities. Instead, alternative methods that incorporate non-verbal indicators of awareness are employed in people with severe dementia. These include facial expressions (e.g. Magai, Cohen, Gomberg, Malatesta, & Culver, Citation1996), body language (e.g. Pöllänen & Hirsimäki, Citation2014) and physiological responses (e.g. Beach, Huck, Miranda, & Bozoki, Citation2015).
Performance monitoring/self-recognition
This level of awareness is concerned with the ability to monitor ongoing performance or events with a degree of accuracy (Clare, Citation2010). This has been measured by asking participants to estimate their performance on a task and comparing the predicted score with the actual score. These paradigms assume that accurately estimating performance is only possible if the ability to monitor, or be aware of current abilities, is intact (Clare, Citation2004). Examining performance monitoring in severe AD is challenging as verbal estimations are often not possible. It has been suggested that tasks examining the ability to self-recognise or demonstrate self-awareness require similar cognitive abilities as the tasks used to examine performance monitoring in less severe AD (Clare, Citation2010; Clare, Rowlands, Bruce, Surr, & Downs, Citation2008). Studies using methods such as mirror recognition or the mirror-mark task (Gallup, Citation1970) may therefore be suitable to establish the extent to which awareness at this level is disturbed or maintained in severe AD.
Evaluative judgement
This level of awareness requires the ability to make realistic judgements regarding one’s functioning or situation. It is distinct from performance monitoring as it involves making global judgements about impairments, symptoms or changes of one’s abilities or functioning, rather than monitoring performance of an ongoing task (Clare, Marková, Roth, & Robin, Citation2011). It requires an understanding of current abilities and being able to recall and make comparisons against previous abilities, memories or expected standards. In mild to moderate AD, investigation of evaluative judgement usually involves comparing the discrepancy in ratings between an individual and his/her caregiver, with a higher discrepancy score indicating less awareness of specific impairments. However, little is known about evaluative judgement in severe AD since self-report measures cannot often be completed.
Meta-representation
At the most complex level of awareness, meta-representation requires the ability to consider alternative perspectives and engage in self-reflection. Objects of awareness are abstract concepts and are often closely interlinked with social and cultural factors (Clare et al., Citation2011), for example, the ability to reflect on one’s situation and consider the impact this may have on oneself and others. In the milder stages of dementia, meta-representation is often examined by in-depth interviews. This, however, is often not possible in severe AD. Consequently, relatively little is known about this level of awareness in severe AD.
As outlined above, awareness is usually assessed by verbal self-reports or subjective accounts in mild to moderate AD. However, these methods are often inappropriate for people with severe AD, who have significantly impaired cognition and verbal communication abilities. It can therefore be difficult to know what people with severe AD are able to experience or how aware they are of themselves and their environment. Additionally, studies examining awareness often exclude people with severe dementia due to practical challenges. Therefore, relatively few studies have specifically examined awareness in severe dementia, where this faculty may be most impaired and can have the most substantial impact on a person’s life. There is also evidence to suggest that environmental factors (e.g. level of noise, or specific use of music, as well the sensitivity of caregiver’s approach) mediate the expression of awareness (Clare et al., Citation2013). Clare and colleagues (2013) conducted an intervention study to train caregivers in assessing awareness in people with severe AD by observing non-verbal cues (e.g. facial expression, eye movement and posture) in response to environmental stimuli, such as physical contact, conversation or use of personal objects. Training caregivers to be more sensitive to the expression of awareness in severe dementia patients was associated with significant improvement in the quality of life of people with severe dementia, as rated by family members, and caregivers reporting to have a better understanding of the needs of severe dementia patients (Clare et al., Citation2013). Improving our understanding of awareness in severe dementia may therefore help to inform the education of caregivers who may otherwise assume people with severe AD are not aware, leading to negative consequences such as neglectful care (Clare et al., 2012).
A previous systematic review (Clare, Citation2010) highlighted the absence of research into awareness at this stage in AD. Included studies used a range of methodologies, often utilising observational methods and caregiver opinions that may be susceptible to potential bias. The review also showed that evidence for maintained awareness was dependent on the research methods used and the environment in which the research was conducted. The current review serves to update the review conducted by Clare (Citation2010) by exploring whether more research has been carried out in the past decade. It has two objectives:
Establish to what extent awareness is impaired or maintained in severe AD.
Explore the evidence for lower and higher levels of awareness in severe AD according to the levels of awareness framework (Clare et al., Citation2011).
Methods
Search strategy and study selection
This systematic review followed PRISMA guidelines and a review protocol was registered on PROSPERO (CRD42018104952). A systematic search of the literature was conducted using the electronic databases PsycINFO, Embase, MEDLINE and Web of Science to identify relevant studies from inception up to 29th June, 2018, using search terms in . The search was limited to studies published in the English language in peer-reviewed journals.
Table 1. Search terms.
Studies were eligible for inclusion if they directly examined awareness or a construct considered to be indicative of awareness (e.g. reactions to pain) in adult human participants with a validated diagnosis (e.g. DSM or ICD) of Alzheimer’s disease dementia. AD severity must have been in the severe or advanced stages of disease as confirmed by a validated assessment tool ( e.g. CDR, Huges, Berg, Danziger, Coben, & Martin, Citation1982; GDS, Reisberg, Ferris, de Leon, & Crook, Citation1982; MMSE, Folstein, Folstein, & McHugh, Citation1975). In instances where studies included participants with a range of disease stages, severity had to be clearly defined and clear distinctions made between levels of cognitive impairment (e.g. mild; moderate; severe) in results. Exclusion criteria included studies where participants had a diagnosis with a co-morbid neurological or psychiatric condition which may have impaired cognitive abilities and/or levels of awareness (e.g. traumatic brain injury or moderate-severe depression); papers which were not from peer reviewed journals; studies which did not clearly state types of dementia; studies which did not make clear distinctions in analyses with regard to severity or type of dementia and studies where full texts were not available in English language.
Titles and abstracts were screened against the inclusion criteria by four reviewers (RB, JH, NJO & HZ) to exclude irrelevant papers. Full texts were obtained for all potentially relevant studies and examined to determine whether they met the specified inclusion criteria by two authors independently (PG & NJO). Any discrepancies were resolved by a third reviewer (JH).
Data extraction
Information regarding sample characteristics, setting, study design, aims, outcome measures, key findings and conclusions were collected and presented in separate tables (see and Appendices B and C).
Table 2. Study findings and conclusions (Data is organised by ascending levels of awareness).
Quality assessment
A quality assessment was carried out for all eligible studies. Quantitative, cross-sectional studies were assessed using the Appraisal tool for Cross-Sectional Studies (AXIS; Downes, Brennan, Williams, & Dean, Citation2016) while qualitative studies were assessed against the Critical Appraisal Skills Programme Qualitative tool (CASP, 2018). Study quality was based on the clarity of the study objectives, appropriateness of methodology and study design, ethical considerations and validity of results. Appendix A provides more information on the appraisal tools.
Data synthesis and analysis
A narrative summary and review of each study was chosen due to methodological heterogeneity. The results have been presented following each of the four levels of awareness detailed in the theoretical framework proposed by Clare and colleagues (2011).
Results
The search strategy identified 39,574 studies. After deduplication, 27,714 results remained, of which 27,336 articles were excluded following the initial screening of titles and abstracts. We further excluded 357 papers after reviewing the full texts, resulting in a total of 21 papers included in the review. More information on study selection is delineated in . The 21 identified studies were published from 1988 to 2016 and were conducted in 8 countries: USA (n = 7); France (n = 3); Spain (n = 3); Sweden (n = 3); Italy (n = 2); Argentina (n = 1); Finland (n = 1); and Japan (n = 1). The number of participants varied considerably across studies, with a median sample size of 11 (range 3–77). Nine studies were defined as high quality (Avondino & Antoine, Citation2016; Beach et al., Citation2015; Conde-Sala et al., Citation2013, Citation2014, Citation2016; Magai et al., Citation1996, Pöllänen & Hirsimäki, Citation2014; Starkstein, Jorge, Mizrahi, & Robinson, Citation2006; Swall, Ebbeskog, Lundh, & Fagerberg, Citation2015), seven as moderate quality (Asplund, Jansson, & Norberg, Citation1995; Asplund, Norberg, Adolfsson, & Waxman, Citation1991; Biringer, Anderson, & Strubel, Citation1988; Biringer & Anderson, Citation1992; Bologna & Camp, Citation1997; Mayhew, Acton, Yauk, & Hopkins, Citation2001; Tappen, Williams, Fishman, & Touhy, Citation1999) and five as low quality (Grewal, Citation1994; Lancioni et al., Citation2013, Citation2015; Mangone et al., Citation1991; Yokoi, Haraguchi, Hashimoto, & Okamura, Citation2012).
Sensory registration
Nine of the 21 studies provided evidence for awareness at the level of sensory registration (Asplund et al., Citation1991, Citation1995; Beach et al., Citation2015; Lancioni et al., Citation2013, Citation2015; Magai et al., Citation1996; Pöllänen & Hirsimäki, Citation2014; Swall et al., Citation2015; Yokoi et al., Citation2012). All nine examined behavioural responses to stimuli while two had the addition of physiological measures (Asplund et al., Citation1991; Beach et al., Citation2015). A summary of each study is provided in .
The majority of studies provided evidence to suggest that sensory registration is maintained in people with severe AD. Listening to familiar music was associated with increased behavioural responses compared to periods of no music (Lancioni et al., Citation2013, Citation2015). These responses extended beyond bodily expressions and involved the use of hand-held switches to actively control the music played. Similarly, painful and unpleasant stimuli (e.g. stretching) were found to increase behavioural responses in people with severe AD indicated by facial expressions (Asplund et al., Citation1991), vocalizations and body language (Beach et al., Citation2015). Conversely, pleasant stimuli (e.g. rocking in a chair) were accompanied by reductions in facial expressions assumed to indicate comfort and relaxation (Asplund et al., Citation1991), implying people with severe AD are able to differentiate between pleasant and unpleasant stimuli. People with severe AD demonstrated a variety of facial responses that correspond to emotional expressions, including anger, disgust, happiness, sadness, and surprise (Asplund et al., Citation1995), although the ability to interpret such responses remains equivocal. While Asplund and colleagues (1991) concluded that only simple facial reactions can be observed in people with severe AD, Magai and colleagues (1996) contended that meaningful emotional expressions can be identified. There is some evidence that certain expressions are more (e.g. fear and disgust; Magai et al., Citation1996) or less (e.g. joy; Magai et al., Citation1996) likely to be observed in severe AD compared to earlier stages. Importantly, one study compared two methods for examining facial expressions (Asplund et al., Citation1995). Overall, agreement between the two measures was low (48%) suggesting that interpretation of sensory awareness using facial expressions in severe AD is challenging. In one study, family members reported higher levels of interest and joy whilst nursing assistants reported more frequent expressions of anger (Magai et al., Citation1996), which may reflect the different interactions each group has with the individuals.
A qualitative study showed that memory triggers were associated with non-verbal indicators of sensory awareness, including signs of relaxation and happiness, as well as efforts to explore objects through touch and smell (Pöllänen & Hirsimäki, Citation2014). Similarly, facial expressions and body language indicative of happiness, relaxation and joy were evident during animal therapy sessions in people with moderate to severe AD (Swall et al., Citation2015).
One study provided evidence of impaired awareness at this level (Yokoi et al., Citation2012). Participants were often not able to demonstrate awareness of food being placed in their mouths; however interpretation of behavioural responses in these studies remains unreliable, as motivational factors including lack of hunger, dislike of food or unwillingness to interact with care staff may play a role rather than a lack of sensory registration.
Two studies (Asplund et al., Citation1991; Beach et al., Citation2015) assessed physiological responses to pleasant, unpleasant or painful stimuli. Both studies revealed unpleasant and painful stimuli were associated with increased heart (Asplund et al., Citation1991; Beach et al., Citation2015) and respiratory rates (Asplund et al., Citation1991). Contrastingly, pleasant stimuli were accompanied with reduced physiological activity suggesting relaxation. These findings are consistent with the behavioural studies reported above. Importantly, compared to people with mild or moderate AD, people with severe AD exhibited blunted physiological responsivity (Beach et al., Citation2015). This observation was posited to be a result of autonomic dysfunction rather than an impaired awareness of pain.
Performance monitoring/self-recognition
Seven studies examined performance monitoring in severe AD (Biringer & Anderson, Citation1992; Biringer et al., Citation1988; Bologna & Camp, Citation1997; Grewal, Citation1994; Mayhew et al., Citation2001; Tappen et al., Citation1999; Yokoi et al., Citation2012). Studies utilised various methods to explore simple self-recognition and self-awareness. Overall, the studies provided mixed evidence, suggesting that some aspects of self-recognition are retained whereas others are impaired. Awareness at this level appears to vary between people with similar AD severities and its manifestation may also be related to environmental cues. A summary of each study is provided in .
Studies observing simple mirror usage demonstrated that the ability to self-recognise becomes increasingly impaired with the progression of AD (Biringer et al., Citation1988; Biringer & Anderson, Citation1992; Grewal, Citation1994). Consistent with this finding, studies using the mirror-mark task found participants with severe AD were less able to demonstrate awareness of the mark than participants with moderate or moderate-severe AD (Biringer et al., Citation1988; Biringer & Anderson, Citation1992). A similar result was found with the use of a video recognition task, in which only one moderately-severe AD participant was able to identify a video of themselves, compared to all moderate participants (Biringer & Anderson, Citation1992). Importantly, all participants reported seeing ‘a face’ which suggests that it was unlikely that visual deficits could account for the inability to self-recognise. Using an alternative approach, Grewal (Citation1994) asked participants to identify parts of their body (e.g. show me your elbow). It was found that all moderate AD participants retained this ability compared to only 25% of people with severe AD. Interestingly, one study using the visible mark paradigm found all moderately-severe participants demonstrated mark awareness compared to one severe participant and 50% of moderate participants (Biringer et al., Citation1988), suggesting that the relationship between performance monitoring and AD severity is not straightforward when using this paradigm.
Two qualitative studies explored the ability to demonstrate self-awareness (Mayhew et al., Citation2001; Tappen et al., Citation1999). Both studies found people with severe AD were able to correctly use personal pronouns (e.g. ‘I’, ‘me’) to refer to themselves during conversations.
One study explored whether awareness could be re-established through an intervention and whether the effects could be maintained (Bologna & Camp, Citation1997). Awareness at the performance monitoring level could be restored in people with moderately-severe and severe AD by using environmental cues. However, in the absence of environmental prompts the ability was not maintained. These findings suggest environmental factors are important for facilitating or preventing the expression of awareness at the performance monitoring/self-recognition level.
Evaluative judgement
Eleven papers provided evidence for evaluative judgement in people with severe AD (Avondino & Antoine, Citation2016; Conde-Sala et al., Citation2013, Citation2014, Citation2016; Mangone et al., Citation1991; Mayhew et al., Citation2001; Pöllänen & Hirsimäki, Citation2014; Starkstein et al., Citation2006; Swall et al., Citation2015; Tappen et al., Citation1999; Yokoi et al., Citation2012) (). While overall these studies suggest that awareness at this level is impaired in severe AD, there is some variability, which may be due to differences in methodology and domain of awareness being evaluated.
Four studies provided evidence for evaluative judgement using the Anosognosia Questionnaire-Dementia scale (AQ-D). All studies demonstrated that awareness at this level became increasingly impaired as AD progressed to the severe stages, as demonstrated by higher AQ-D scores (Conde-Sala et al., Citation2013, Citation2014, Citation2016; Starkstein et al., Citation2006). One study reported that the presence of anosognosia increased from 10% in people with mild AD to 57% in severe AD (Starkstein et al., Citation2006). Interestingly, another study found mean AQ-D scores decreased from baseline to follow-up in the moderately-severe AD group (Conde-Sala et al., Citation2016). However, this result may be explained by participants lost to follow-up having more severe cognitive impairments than those who remained in the study. One study used items from the physical self-maintenance and instrumental activities of daily living scales to assess evaluative judgement (Mangone et al., Citation1991). Results showed that anosognosia increased alongside the progression of AD, with GDS staging being the strongest predictor of impaired evaluative judgement out of all the measures in this study.
Five qualitative studies provided evidence for evaluative judgement. In all studies some participants were able to show awareness of their cognitive decline and current needs (Mayhew et al., Citation2001; Pöllänen & Hirsimäki, Citation2014; Swall et al., Citation2015; Tappen et al., Citation1999; Yokoi et al., Citation2012). One study found people with severe AD were able to give verbal accounts of how they often found speaking difficult and struggled to find words to express themselves (Mayhew et al., Citation2001). The authors also noted the speech of these individuals was often muddled but could be understood when time was spent to understand what they were trying to communicate. Pöllänen and Hirsimäki (Citation2014) also noted that participants could compare earlier and current skill levels, acknowledging that their skills were not as proficient as before. Swall and colleagues (2015) found participants acknowledged their deficits and these realisations were often accompanied by indicators of anxiety and fear, although it is unclear if this occurred in participants with more severe AD. While Tappen and colleagues (1999) demonstrated that participants were aware of their deficits, they struggled to find explanations for why this may have happened, suggesting unawareness of their illness. Similarly, Yokoi and colleagues (2012) noted that all but one severe AD participant were unaware of their cognitive decline.
Meta-representation
There were no studies that specifically aimed to examine meta-representation, although three qualitative studies provided information relating to this level of awareness (Mayhew et al., Citation2001; Swall et al., Citation2015; Yokoi et al., Citation2012), summarised in . One study observed behaviours and verbal responses during animal therapy sessions (Swall et al., Citation2015) while another observed unusual words and actions that were expressed during dining scenes (Yokoi et al., Citation2012). The third study analysed conversations between people with severe AD and nursing staff (Mayhew et al., Citation2001). Two studies found that some participants were able to empathise with and consider the perspectives of others (Mayhew et al., Citation2001; Swall et al., Citation2015). Mayhew and colleagues (2001) also found that people with severe AD were able to consider the social implications of their behaviour. Yokoi and colleagues (2012), however, noted that most participants lacked the ability to adhere to the dining etiquette rules of their society.
Discussion
We examined 21 papers to establish the extent to which awareness is maintained or disturbed in severe AD, and to determine the evidence for different levels of awareness according to the levels of awareness framework (Clare et al., Citation2011). We found evidence that sensory level awareness is relatively maintained in severe AD. There was mixed evidence for awareness at the level of Performance Monitoring/Self-recognition. Overall the evidence suggests that awareness is impaired at the levels of evaluative judgement and meta-representation; however there remains some individual variability in higher-level awareness in people with severe AD, indicating that awareness is not completely absent.
Overall, the existing literature highlights that environmental contexts play a significant role in facilitating or preventing the expression of awareness in severe AD. Several studies reported that various environmental stimuli effected the expression of lower level sensory awareness in severe AD patients, such as listening to music (Lancioni et al., Citation2013, Citation2015) and sitting in a rocking-chair (Asplund et al., Citation1991). Environmental cues, including name tags and labels, also appeared to influence self-recognition in individuals who could not independently demonstrate this ability (Bologna & Camp, Citation1997).
These findings are consistent with research in mild AD, which has shown that contextual factors can have a positive or negative impact on awareness (Clare et al., 2012). People with severe AD are also able to differentiate between positive and negative stimuli and respond accordingly. Taken together, it is appropriate to suggest that people with severe AD may not demonstrate awareness, not because they are unable to but rather because the environmental factors are not conducive to expressing awareness. Therefore, caregivers should foster a positive, supportive and stimulating environment to facilitate the expression of awareness. This is reinforced by studies that have found environments, which are over-stimulating (e.g. noisy environments) or under-stimulating, reduce communication and increase withdrawal (Norberg, Melin, & Asplund, Citation1986). Accordingly, it is more likely that carers will assume that reduced responsivity is indicative of unawareness. Caregivers may then reduce interactions with these individuals and in doing so limit their opportunities to demonstrate awareness. Thus, a vicious cycle of assumed unawareness, under-stimulation and withdrawal begins (Clare et al., 2012). Consequently, educating caregivers on how to detect signs of awareness and provide suitable levels of stimulation may enable people with severe AD to express awareness. In support of this, Clare and colleagues (2013) demonstrated that training professional caregivers to identify signs of awareness in people with severe dementia is associated with improved family member-rated quality of life for people with dementia. However, more research examining caregiver training is needed to fully understand its potential benefits, as well as to help guide caregivers and clinicians in choosing suitable activities to stimulate the expression of awareness.
This review highlights several limitations within the existing evidence base. Firstly, many studies do not consider additional factors that may influence the expression of awareness. It is well-recognised that the prevalence of behavioural and psychological symptoms (BPSD) is common in AD including apathy (Burns & Iliffe, Citation2009; Livingston et al., Citation2017) and depression (Ballard, Bannister, & Oyebode, Citation1996). BPSD are also known to be more prevalent in severe dementia (Mukherjee et al., Citation2017) and exacerbate cognitive and functional deficits (Greenwald et al., Citation1989). Accordingly, it would be appropriate to assume that these may also negatively impact awareness. While some studies did consider these symptoms (e.g. Conde-Sala et al., Citation2013, Citation2014, Citation2016), they did not provide sufficient evidence for the relationship with awareness in severe AD. Reasons for this include: exclusion of people in the most severe stages, providing only information about moderately-severe AD (Conde-Sala et al., Citation2013, Citation2014, Citation2016); measurement of BPSD but no subsequent discussion on how this relates to awareness (Lancioni et al., Citation2013); and exclusion of participants on the basis of high BPSD scores (Beach et al., Citation2015). One study examined this relationship (Starkstein et al., Citation2006), demonstrating that people with severe AD were less aware of their own depressive symptoms. However, no definitive conclusions can be drawn from one study.
Secondly, the investigation of awareness in severe AD is heavily reliant on subjective, caregiver and observer reports or observations of behaviour. It is therefore probable that biases have been introduced into these findings, especially since indicators of awareness in severe AD are often subtle and ambiguous. Moreover, studies using more than one method or observer to code behaviours have found low levels of agreement (Asplund et al., Citation1995; Magai et al., Citation1996), highlighting the risk of misinterpretation particularly when no formal coding protocol is implemented. Furthermore, studies observing task performance (e.g. mirror-mark task) to infer awareness may underestimate the complexity of this phenomenon. Notably, the mirror-mark task, devised to be used on non-human primates (Gallup, Citation1970), underestimates the complexity of human self-awareness. The paradigm assumes the absence of behavioural indicators of self-recognition corresponds to no underlying self-awareness. However, considering the requirements of the task it may be more complex than it actually assumes. For example, to pass the task individuals must understand themselves from an alternative perspective, which differs from how they normally see themselves (Merleu-Ponty, 1964, cited in Rochat & Zahavi, Citation2011). Furthermore, the paradigm is unable to differentiate between multiple levels of self-awareness, in this case self-recognition and meta-representation. False negatives may therefore occur when a failure in the task is interpreted as an inability to self-recognise whereas the person may be impaired at the meta-representation level but retains the level of self-recognition. More objective measures to assess awareness may facilitate a more accurate understanding of how different levels of awareness is experienced in severe AD.
In line with this, our search of the literature retrieved no studies utilising objective measures to examine possible neurological correlates of awareness in severe AD. Studies with other patient groups, such as people with frontotemporal dementia, have consistently identified areas in the prefrontal cortex (Cosentino & Stern, Citation2005; Cosentino et al., Citation2015; Lau & Rosenthal, Citation2011) as being associated with awareness. Furthermore, studies using neuroimaging techniques have shown neural activation in some people diagnosed as being in a vegetative state as not dissimilar to healthy controls (e.g. Owen et al., Citation2006). These studies demonstrate that neuroimaging techniques are useful for examining levels of consciousness, and so awareness, in people who are no longer able to communicate verbally. To our knowledge, no studies have specifically examined the neural correlates of awareness in severe AD. Future research using these methods could provide a deeper understanding of awareness in severe AD and how it is altered by disease progression. These methods may also help to overcome some of the challenges associated with interpreting non-verbal indicators of awareness.
There is a limited body of evidence for awareness in severe AD. Since the last review in 2010 only 12 new studies were identified. There are several possible explanations for the paucity of new studies. Firstly, obtaining informed consent from people in severe stages of AD is often not possible and strict guidelines are followed to recruit individuals who are unable to provide consent (The World Medical Association, 2013). The difficulty of recruiting people in severe stages of AD is reflected in the identified studies, with the majority having small sample sizes. It is paramount that future studies ensure people with dementia and their caregivers understand the potential benefits of research into awareness in severe AD. Increasing the body of research and improving our understanding of awareness in severe AD could provide more insight into what people with AD are able to experience. This would allow us to improve the provision of person-centred care and provide more meaningful interactions for people with severe AD. Furthermore, it would also eliminate some of the uncertainty experienced by families and caregivers of people with severe AD, which in turn should reduce associated burden and stress. Within institutionalised care settings it would help eliminate the assumption of unawareness and prevent neglectful care practices.
Our review had some limitations. The decision to limit the review to severe AD will limit the generalisability of the findings. In future, research incorporating multiple subtypes of dementia would further our understanding of awareness in severe dementia. It is vital that these studies make distinctions between dementia types in analyses and results. This would facilitate an improved understanding of the possible neural correlates of awareness and how each pathology differentially affects awareness.
It is important to highlight that only 42% of studies included in this review were considered to be of high quality, which may have limited our ability to draw generalisable conclusions. Most studies also used restricted sample sizes, thereby limiting the conclusions that can be made and the generalisability of findings. Moreover, the methods used to explore awareness were heterogeneous and relied heavily on subjective observations, which further limits the conclusions that can be drawn. While the levels of awareness framework (Clare et al., Citation2011) offers a useful tool to conceptualise awareness, it remains challenging to tease apart the higher levels due to the overlap in levels with existing assessment methods. Therefore, it is imperative that more high-quality studies incorporating objective measures are undertaken to elucidate the extent to which awareness is impaired or preserved in severe AD.
Conclusion
In conclusion, awareness is complex, heterogeneous and varies significantly between individuals. Awareness at the level of sensory registration in patients with severe AD is relatively preserved. Performance monitoring or self-recognition is variable and is heavily dependent on environmental factors, while evidence for evaluative judgement is mixed. At the most complex level of awareness (i.e. meta-representation), no inferences can be made due to the limited body of evidence. In other clinical populations, such as minimally conscious states in which awareness is also considerably affected, there have been substantial advances in the objective assessment and understanding of awareness. Comparatively, progress has been limited in AD. Nevertheless, awareness in severe AD remains a significant issue for people with AD, their families and professionals. Therefore, it is paramount that more research is conducted to establish a more coherent account of awareness in this population.
Supplemental Material
Download MS Word (32.1 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Asplund, K., Jansson, L., & Norberg, A. (1995). Facial expression of patients with dementia: A comparison of two methods of interpretation. International Psychogeriatrics, 7(4), 527–534. doi:10.1017/S1041610295002262
- Asplund, K., Norberg, A., Adolfsson, R., & Waxman, H. M. (1991). Facial expression in severe demented patients – A stimulus response study of four patients with dementia of the Alzheimer type. International Journal of Geriatric Psychiatry, 6(8), 599–606. doi:10.1002/gps.930060809
- Avondino, E., & Antoine, P. (2016). Heterogeneity of cognitive anosognosia and its variation with the severity of dementia in patients with Alzheimer’s disease. Journal of Alzheimer's Disease, 50(1), 89–99. doi:10.3233/JAD-150496
- Ballard, C., Bannister, C., & Oyebode, F. (1996). Depression in dementia sufferers. International Journal of Geriatric Psychiatry, 11(6), 507–515. doi:10.1002/(SICI)1099-1166(199606)11:6 < 507::AID-GPS337 > 3.0.CO;2-U
- Beach, P. A., Huck, J. T., Miranda, M. M., & Bozoki, A. C. (2015). Autonomic, Behavioural and Subjective Pain Responses in Alzheimer’s Disease. Pain Medicine, 16(10), 1930–1942. doi:10.1111/pme.12769
- Biringer, F., & Anderson, J. R. (1992). Self-recognition in Alzheimer’s disease: A mirror and Video study. Journal of Gerontology, 47(6), P385–388.
- Biringer, F., Anderson, J. R., & Strubel, D. (1988). Self-recognition in senile dementia. Experimental Aging Research, 14(4), 177–180. doi:10.1080/03610738808259745
- Bologna, S. M., & Camp, C. J. (1997). Covert versus overt self-recognition in late stage Alzheimer’s disease. Journal of the International Neuropsychological Society, 3(2), 195–198. doi:10.1017/S1355617797001951
- Burns, A., & Iliffe, S. (2009). Alzheimer’s’ disease: Clinical Review. BMJ, 338, b158. https://www.bmj.com/content/338/bmj.b158
- Clare, L. (2004). Awareness in early‐stage Alzheimer's disease: A review of methods and evidence. British Journal of Clinical Psychology, 43(2), 177–196. doi:10.1348/014466504323088042
- Clare, L. (2010). Awareness in people with severe dementia: Review and integration. Aging & Mental Health, 14(1), 20–32. doi:10.1080/13607860903421029
- Clare, L., Marková, I. S., Roth, I., & Robin, G. M. (2011). Awareness in Alzheimer's disease and associated dementias: Theoretical framework and clinical implications. Aging & Mental Health, 15(8), 936–944. doi:10.1080/13607863.2011.583630
- Clare, L., Marková, I. S., Verhey, F., & Kenny, G. (2005). Awareness in dementia: A review of assessment methods and measures. Aging & Mental Health, 9(5), 394–413. doi:10.1080/13607860500142903
- Clare, L., Nelis, S., Martyr, A., Roberts, J., Whitaker, C., Markova, I. S., … Morris, R. (2012a). The influence of psychological, social and contextual factors on the expression and measurement of awareness in early‐stage dementia: Testing a biopsychosocial model. International Journal of Geriatric Psychiatry, 27(2), 167–177. doi:10.1002/gps.2705
- Clare, L., Rowlands, J., Bruce, E., Surr, C., & Downs, M. (2008). I don't do like I used to do’: A grounded theory approach to conceptualising awareness in people with moderate to severe dementia living in long-term care. Social Science & Medicine, 66(11), 2366–2377. doi:10.1016/j.socscimed.2008.01.045
- Clare, L., Whitaker, R., Quinn, C., Jelley, H., Hoare, Z., Woods, B., … Wilson, B. (2012b). AwareCare: Development and validation of an observational measure of awareness in people with severe dementia. Neuropsychological Rehabilitation, 22(1), 113–133. doi:10.1080/09602011.2011.640467
- Clare, L., Whitaker, R., Woods, R. T., Quinn, C., Jelley, H., Hoare, Z., … Wilson, B. A. (2013). AwareCare: A pilot randomized controlled trial of an awareness-based staff training intervention to improve quality of life for residents with severe dementia in long-term care services. International Psychogeriatrics, 25(1), 128–139. doi:10.1017/S1041610212001226
- Conde-Sala, J. L., Reñe-Ramírez, R., Turró-Garriga, O., Gascón-Bayarri, J., Campdelacreu-Fumadó, J., Juncadella-Puig, M., … Garre-Olmo, J. (2014). Severity of Dementia, Anosognosia, and Depression in Relation to the Quality of Life of Patients with Alzheimer Disease: Discrepancies Between Patients and Caregivers. The American Journal of Geriatric Psychiatry, 22(2), 138–147. doi:10.1016/j.jagp.2012.07.001
- Conde-Sala, J. L., Reñé-Ramírez, R., Turró-Garriga, O., Gascón-Bayarri, J., Juncadella-Puig, M., Moreno-Cord, ´… Garre-Olmo, J. (2013). Clinical Differences in Patients with Alzheimer’s Disease According to the Presence or Absence of Anosognosia: Implications for Perceived Quality of Life. Journal of Alzheimer's Disease, 33(4), 1105–1116. doi:10.3233/JAD-2012-121360
- Conde-Sala, J. L., Turró-Garriga, O., Piñán-Hernández, S., Portellano-Ortiz, C., Viñas-Diez, V., Gascón-Bayarri, J., & Reñé-Ramírez, R. (2016). Effects of anosognosia and neuropsychiatric symptoms on the quality of life of patients with Alzheimer’s disease: A 24-month follow-up study. International Journal of Geriatric Psychiatry, 31(2), 109–119. doi:10.1002/gps.4298
- Cosentino, S., & Stern, Y. (2005). Metacognitive theory and assessment in dementia: Do we recognize our areas of weakness?. Journal of the International Neuropsychological Society, 11(07), 910–919. doi:10.1017/S1355617705050964
- Cosentino, S., Brickman, A. M., Griffith, E., Habeck, C., Cines, S., Farrell, M., … Stern, Y. (2015). The right insula contributes to memory awareness in cognitively diverse older adults. Neuropsychologia, 75, 163–169. doi:10.1016/j.neuropsychologia.2015.05.032
- Critical Appraisal Skills Programme. (CASP). (2018). CASP (Qualitative) Checklist [online]. Retrieved from https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist.pdf.
- Downes, M., Brennan, M., Williams, H., & Dean, R. (2016). Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open, 6(12), e011458. doi:10.1136/bmjopen-2016-011458
- Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini Mental State. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. doi:10.1016/0022-3956(75)90026-6
- Gallup, G. (1970). Chimpanzees: Self-recognition. Science, 167(3914), 86–87. doi:10.1126/science.167.3914.86
- Greenwald, B., Kramer-Ginsberg, E., Marin, D., Laitman, L., Hermann, C., Mohs, R., & Davis, K. (1989). Dementia with coexistent major depression. The American Journal of Psychiatry, 146(11), 1472–1478. doi:10.1176/ajp.146.11.1472
- Grewal, R. P. (1994). Self-recognition in dementia of the Alzheimer type. Perceptual and Motor Skills, 79(2), 1009–1010. doi:10.2466/pms.1994.79.2.1009
- Huges, C. P., Berg, L., Danziger, W. L., Coben, L. A., & Martin, R. L. (1982). A new clinical scale for the staging of dementia. British Journal of Psychiatry, 140, 566–572. doi:10.1192/bjp.140.6.566
- Lancioni, G. E., Bosco, A., De Caro, M. F., Singh, N., O’Reilly, M. F., Green, V. A., … Zonno, N. (2015). Effects of response-related music stimulation versus general music stimulation on positive participation of patients with Alzheimer’s disease. Developmental Neurorehabilitation, 18(3), 169–176. doi:10.3109/17518423.2013.802388
- Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Green, V. A., Ferlisi, G., Ferrarese, G., … Zonno, N. (2013). Self-regulated music stimulation for persons with Alzheimer's disease: Impact assessment and social validation. Developmental Neurorehabilitation, 16(1), 17–26. doi:10.3109/17518423.2012.707693
- Lau, H., & Rosenthal, D. (2011). Empirical support for higher-order theories of conscious awareness. Trends in Cognitive Sciences, 15(8), 365–373. doi:10.1016/j.tics.2011.05.009
- Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S. G., Huntley, J., Ames, D., … Mukadam, N. (2017). Dementia prevention, intervention, and care. The Lancet, 390(10113), 2673–2734. doi:10.1016/S0140-6736(17)31363-6
- Magai, C., Cohen, C., Gomberg, D., Malatesta, C., & Culver, C. (1996). Emotional expression during mid to late stage dementia. International Psychogeriatrics, 8(3), 383–395. doi:10.1017/S104161029600275X
- Mangone, C. A., Hier, D. B., Gorelick, P. B., Ganellen, R. J., Langenberg, P., Regina, B., & Dollear, W. C. (1991). Impaired insight in Alzheimer’s disease. Topics in Geriatrics, 4(4), 189–193. doi:10.1177/089198879100400402
- Mayhew, P. A., Acton, G. J., Yauk, S., & Hopkins, B. A. (2001). Communication from Individuals with Advanced DAT: Can it provide clues to their sense of self-awareness and well-being? Geriatric Nursing, 22(2), 106–110. doi:10.1067/mgn.2001.115198
- Mukherjee, A., Biswas, A., Roy, A., Biswas, S., Gangopadhyay, G., & Das, S. K. (2017). Behavioural and Psychological Symptoms of Dementia: Correlates and Impact on Caregiver Distress. Dementia and Geriatric Cognitive Disorders Extra, 7(3), 354–365. doi:10.1159/000481568
- Norberg, A., Melin, E., & Asplund, K. (1986). Reactions to music, touch and object presentation in the final stage of dementia. An exploratory study. International Journal of Nursing Studies, 23(4), 315–323. doi:10.1016/0020-7489(86)90054-4
- Office of National Statistics. (2017). National life tables, UK: 2014 to 2016. Retrieved from https://www.ons.gov.uk/releases/nationallifetablesuk2014to2016
- Owen, A., Coleman, M., Boly, M., Davis, M., Laureys, S., & Pickard, J. (2006). Detecting awareness in the vegetative state. Science, 313(5792), 1402–1402. doi:10.1126/science.1130197
- Pöllänen, S. H., & Hirsimäki, R. M. (2014). Crafts as Memory Triggers in Reminiscence: A Case Study of Older Women with Dementia. Occupational Therapy in Health Care, 28(4), 410–430. doi:10.3109/07380577.2014.941052
- Reisberg, B., Ferris, S. H., de Leon, M. J., & Crook, T. (1982). The Global Deterioration Scale for assessment of primary degenerative dementia. The American Journal of Psychiatry, 139(9), 1136–1139. doi:10.1176/ajp.139.9.1136
- Rochat, P., & Zahavi, D. (2011). The uncanny mirror: A re-framing of mirror self-experience. Consciousness and Cognition, 20(2), 204–213. doi:10.1016/j.concog.2010.06.007
- Starkstein, S. E., Jorge, R., Mizrahi, R., & Robinson, R. G. (2006). A diagnostic formulation for anosognosia in Alzheimer’s disease. Journal of Neurology, Neurosurgery & Psychiatry, 77(6), 719–725. doi:10.1136/jnnp.2005.085373
- Stuss, D. T., Picton, T. W., & Alexander, M. P. (2001). Consciousness, self-awareness, and the frontal lobes. In S. P. Salloway, P. F. Malloy, & J. D. Duffy (Eds.), The frontal lobes and neuropsychiatric illness (pp. 101–109). Arlington, VA, US: American Psychiatric Publishing
- Sunderaraman, P., & Cosentino, S. (2017). Integrating the Constructs of Anosognosia and Metacognition: A Review of Recent Findings in Dementia. Current Neurology and Neuroscience Reports, 17(3), 27. doi:10.1007/s11910-017-0734-1
- Swall, A., Ebbeskog, B., Lundh, H. C., & Fagerberg, I. (2015). Can therapy dogs evoke awareness of one’s past and present life in persons with Alzheimer’s disease? International Journal of Older People Nursing, 10(2), 84–93. doi:10.1111/opn.12053
- Tappen, R. M., Williams, C., Fishman, S., & Touhy, T. (1999). Persistence of Self in Advance Alzheimer’s Disease. Image: The Journal of Nursing Scholarship, 31(2), 121–125. doi:10.1111/j.1547-5069.1999.tb00445.x
- The World Alzheimer Report. (2013). Journey of Caring: An analysis of long-term care for dementia. London: Alzheimer's Disease International.
- World Medical Association. (2013). World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191–2194. doi:10.1001/jama.2013.281053
- Yokoi, T., Haraguchi, E., Hashimoto, T., & Okamura, H. (2012). Investigation of eating actions of people with dementia from the viewpoint of self-awareness. American Journal of Alzheimer's Disease & Other Dementias®, 27(4), 228–237. doi:10.1177/1533317512449728