Abstract
Objectives
Behavioural and psychological symptoms of dementia (BPSD) are common in patients with dementia. In the elderly population, comorbidities frequently coexist with dementia and mortality in dementia is high. The aim of this study was to investigate the impact of BPSD on mortality in severe dementia.
Methods
This study of 11,448 individuals was based on linked information from the Swedish BPSD registry, the National Patient Register and the Cause of Death register. BPSD was assessed with the Neuropsychiatric Inventory (NPI). Cox proportional hazards regressions were performed for survival analysis. To study different degrees of BPSD, data was categorized into groups: no (NPI, 0 points), mild (NPI, 1–3 points on ≥1 item), moderate (NPI, 4–8 points on ≥1 item) and severe (NPI, 9–12 points on ≥1 item) BPSD based on the highest score on any of the BPSD assessed (NPI items).
Results
The presence of moderate or severe BPSD was associated with a stepwise increased risk of mortality (hazard ratio (HR), 1.31; 95% confidence interval (CI), 1.08–1.60 and HR 1.74; 95% CI 1.44–2.12, respectively) compared with individuals with no BPSD. In addition, there was an association between total NPI score and mortality (HR 1.01; 95% CI 1.007–1.010). The results remained significant after multivariable adjustment for age, sex, dementia diagnosis, medication, previous myocardial infarction, hip fracture and stroke.
Conclusions
The results show a stepwise increase in mortality risk with increased BPSD, highlighting the importance of adequate management of BPSD to reduce mortality in dementia.
Introduction
Dementia is one of the major health problems of our time and is a condition characterized by impaired cognitive abilities resulting in a reduction in daily functioning. It often also leads to changes in personality (Robins Wahlin & Byrne, Citation2011; World Health Organization, Citation2019). Most individuals with dementia experience not only progressive cognitive decline but also non-cognitive symptoms such as various behavioural and psychological symptoms of dementia (BPSD) (Steinberg et al., Citation2008). BPSD comprise a large number of different symptoms, which may be expressed at all stages of the dementia disorder but increase with deterioration in cognition (Siafarikas et al., Citation2018) and are more common in severe dementia (Lopez et al., Citation2003; Selbaek, Kirkevold, & Engedal, Citation2007). There is a strong correlation between BPSD and degree of functional and cognitive impairment and hence, BPSD is regarded as clinically relevant as the cognitive deficits (Cerejeira, Lagarto, & Mukaetova-Ladinska, Citation2012). Agitation, hallucinations, altered sleep patterns and delusions are all examples of BPSD. Other common BPSD are apathy, depressive behaviour and aberrant motor behaviours (Wood et al., Citation2000). BPSD cause considerable suffering for the individuals with dementia and their caregivers (Kamiya, Sakurai, Ogama, Maki, & Toba, Citation2014; Shin, Carter, Masterman, Fairbanks, & Cummings, Citation2005), and are a frequent reason for institutionalization (Toot, Swinson, Devine, Challis, & Orrell, Citation2017). In addition, dementia and BPSD constitute a considerable societal burden socially and economically (Banerjee, Citation2012; World Health Organization, Citation2019). This fact, in combination with the numbers of people affected by dementia, highlights the importance of minimizing BPSD to improve dementia care.
Dementia often coexists with several other medical conditions commonly seen in the elderly (Bunn et al., Citation2014). Studies have reported an increased risk of stroke in Alzheimer disease (AD) dementia (Liu et al., Citation2013), and a prevalence of stroke between 16 and 29% in people with dementia (Bunn et al., Citation2014). Hip fractures are also common in individuals with dementia (Seitz, Adunuri, Gill, & Rochon, Citation2011). AD has been identified as a strong risk factor for sustaining a hip fracture and is also associated with an increase in mortality after hip fracture (Tolppanen, Taipale, Tanskanen, Tiihonen, & Hartikainen, Citation2016). Cardiovascular diseases such as myocardial infarction (MI) are associated with increased mortality and frequently coexist with dementia (Cermakova et al., Citation2015). Dementia and AD without any comorbidity has also been found to be associated with increased mortality (Todd, Barr, Roberts, & Passmore, Citation2013). The associations between dementia, different comorbidities and mortality have thus been explored in previous studies. However, it is unclear how the presence of BPSD relates to mortality.
The aim of this study was to examine whether there is an association between BPSD and mortality in a population with dementia and various degrees of BPSD. We hypothesize that higher degrees of BPSD are associated with an increase in mortality in patients with dementia.
Materials and methods
Study design
This registry study is based on data from the Swedish BPSD registry, the Swedish National Patient Register (NPR) and the Swedish Cause of Death Register (CDR). The register datasets were merged based on personal identification numbers and included information on a total of 11,448 individuals who were registered in the BPSD registry between 15 May 2010 and 31 December 2013.
The BPSD registry
Sweden has a long tradition of using quality registries in health care. The Swedish BPSD registry (http://www.bpsd.se) was started in 2010 with the aim of improving the care of patients with dementia by focusing on non-pharmacological interventions to manage BPSD, based on recommendations from the national guidelines for dementia care (The National Board of Health and Welfare, Citation2017).
The BPSD registry provides a systematic method for use by the multidisciplinary team working with patients with dementia. Before joining the registry, a selected group of staff members from the nursing home receive a 2-day training course. The training includes the following parts; (1) dementia as an illness, (2) assessment of BPSD and common causes thereof, and (3) establishment of an action plan. After completion of the training course, a certification of ‘Administrator’ is provided. Then all involved nursing home staff members receive a web-based instruction on how to use the registry.
Severity and frequency of BPSD is assessed with a modified version of the Neuropsychiatric Inventory – Nursing Home version (NPI-NH) (Cummings et al., Citation1994). The action plan is determined at a multidisciplinary discussion meeting. Components of the action plan are focused on unmet needs of the patient and non-pharmacological person-centred interventions such as activity, physical activity, calm environment, massage, and music/song. A reassessment of BPSD is repeated after a pre-defined time interval to evaluate the performed intervention and the action plan can be revised when needed.
The BPSD-registry has been launched mainly to nursing home staff in routine dementia care. At the time of the present data extraction (31 December 2013) there were 11,448 registered patients, and all were included in the study.
Assessments of BPSD in the BPSD registry
The BPSD assessments with NPI-NH described above, are based on information given by a caregiver familiar with the behaviour of an individual. The NPI items address delusions, hallucinations, agitation, depression, anxiety, euphoria, apathy, disinhibition, irritability, aberrant motor behaviour, sleep disturbances and eating changes.
A total score of 0–12 points is obtained for each NPI item by multiplying the severity score (1–3 points) by the frequency score (1–4 points) for the item (Cummings, Citation2005–2017, Citation2009). The severity score is rated as (1) mild (produces little distress in the patient), (2) moderate (more disturbing for the patient but can be redirected by the caregiver), (3) severe (very disturbing for the patient and difficult to redirect). The frequency score is rated as (1) rarely (less than once per week), (2) sometimes (about once per week), (3) often (several times per week but less than every day) and (4) very often (once or more per day/essentially continuously present/nearly always present/once or more per day or every night) (Cummings, Citation2009). The 12 NPI item scores are added to create the total NPI score ranging from 0 to 144 points.
Medication and dementia diagnoses
Information on medication and dementia diagnoses are added to the registry by caregivers based on information from medical records. In this study, data on medication was missing for 143 individuals.
The Swedish national patient register
The Swedish NPR includes information on all in-patient hospital care. Data registration started in the 1960s and is maintained by The Swedish National Board of Health and Welfare. The register contains patient information such as gender and age and medical data including main and secondary diagnoses (https://www.socialstyrelsen.se/en/statistics-and-data/registers/alla-register/the-national-patient-register/). NPR information on MI, stroke and hip fracture was used in this study.
The Swedish cause of death register
Data have been registered in the Swedish CDR since 1961 and includes information on all events of death that occurs in Sweden. The register is updated continuously and contains information on the date and cause of death (https://sdb.socialstyrelsen.se/if_dor/val_eng.aspx.). Date of death was used as an outcome variable in this study.
Classification of data
BPSD
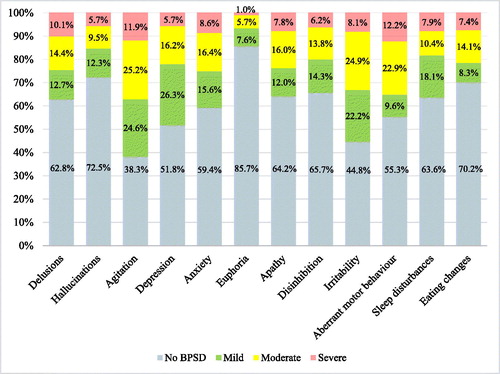
Initially, analyses were performed using the total baseline NPI score. The study population was then divided into four different groups based on baseline NPI scores. Individuals with a total NPI score equalling 0 were categorized into a group named no BPSD and those with a total NPI score above 0 were further divided into three groups: individuals with 0–3 points on ≥1 separate NPI item were categorized as mild BPSD, those with 4–8 points on ≥1 separate NPI item as moderate BPSD, and those with 9–12 points on ≥1 separate NPI item as severe BPSD. Hence, 4 different groups defining different degrees of BPSD were created according to the highest score on any of the 12 NPI items assessed. Finally, we analysed the data with all 12 NPI items categorized into no/mild/moderate/severe based on the criteria above.
Statistical analyses and data processing
Statistical analyses were performed using SPSS version 24.0 (SPSS, Citation2016). A p value <0.05 was considered statistically significant for all analyses. One-way ANOVA was used to test the significance of continuous variables between groups and the chi-squared test was used for categorical variables.
Hazard ratios (HR) and 95% confidence intervals (CI) were calculated using multivariable-adjusted Cox regression models examining mortality associated with BPSD. We used four different models with the different BPSD measures as the main predictor (total NPI score; degree of BPSD; total NPI item score; and the number of mild, moderate and severe NPI items). All models were adjusted for the following covariates: age, sex, dementia diagnosis, medication (analgesics, antiepileptics, antipsychotics, anxiolytics, hypnotics, antidepressants, acetylcholinesterase inhibitors [AChEI] and N-methyl-D-aspartate [NMDA] antagonist), previous hip fracture, MI and stroke.
Ethics
The study was performed after approval by the Regional Ethics Committees of Lund University and Umeå University, Sweden.
Results
Participants
The study population consisted of 11,448 individuals with a BPSD registry baseline registration. The mean age and standard deviation (SD) of the study participants at baseline was 83.2 (7.8) years. There were 7485 (65.4%) women and 3963 (34.6%) men included in the study; 87.3% of the individuals were nursing home residents; 31.4% had AD, 13.6% had vascular dementia (VaD), 8.6% had mixed AD and VaD (mixed), 1.2% had dementia with Lewy bodies (DLB), 1.2% had Parkinson disease dementia (PDD), 2.1% had frontotemporal dementia (FTD), 16.8% had other dementia diagnosis (ODD) and 25% had an undefined dementia diagnosis (UDD). The ODD category represented more uncommon dementia disorders such as alcohol-related dementias and corticobasal degeneration. The UDD group represented individuals for whom information on dementia diagnosis was undefined in the registry. Baseline characteristics are presented in .
Table 1. Baseline characteristics of the study population.
Survival
The observation time for all Cox proportional hazards models extended from the first BPSD assessment and until 31 December 2013. The mean (SD) observation time was 250.3 (191.6) days and the median (min–max) observation time was 224 (0–1326) days. A total of 11,303 (98.7%) individuals were included in the Cox regression analyses and 2370 individuals died during the observation period. One hundred forty-five cases were excluded from the Cox regressions due to missing information about medication (n = 143) or observation time (n = 2).
Measures of BPSD
The mean (SD) and median (min–max) total NPI score in the population was 25.2 (22.5) and 19.0 (0–144), respectively; 6.5% had no BPSD, 16.4% had mild BPSD, 37.4% had moderate BPSD and 39.7% had severe BPSD (). The most prevalent BPSD were agitation (61.7%), irritability (55.3%) and depression (48.3%) and the least common BPSD was euphoria (14.3%). The distribution of NPI item scores of different degrees (no, mild, moderate, and severe) for all 12 NPI items is presented in . The mean (SD) number of mild, moderate and severe items for an individual was 1.8 (1.6), 1.9 (1.8) and 0.9 (1.6) respectively.
Total NPI score
Initially, a Cox regression model was performed with death as a dependent variable and age, sex and total NPI score as covariates. There was a statistically significant association between total NPI score and mortality (HR 1.01; 95% CI 1.007–1.010). The results remained significant after multivariable adjustment, introducing all covariates in . Other variables that were significantly associated with increased mortality were age, male sex, previous MI, hip fracture and stroke. VaD and medication with anxiolytics, antidepressants and AChEIs were associated with a decrease in mortality ().
Table 2. Association between BPSD and mortality in 11,303 individuals with dementia; total NPI score was used as measure of BPSD.
Degree of BPSD
When using the log rank test to test the robustness of the model before adjustment for any variables, there was a significant difference in estimated survival time between the BPSD groups (p < 0.001). The median (CI) estimated survival time was 1124 days (95% CI 690–1558) for individuals with mild BPSD, 893 days (95% CI 785–1001) for those with moderate BPSD and 682 days (95% CI 618–746) for those with severe BPSD. shows survival curves stratified by degree of BPSD.
Figure 2. Survival curves showing the cumulative survival in patients with different degrees of BPSD (n = 11,303). 2370 individuals died. The survival curves were adjusted for sex, age, dementia diagnosis, use of antipsychotics, acetylcholinesterase inhibitors, NMDA (N-methyl-D-aspartate) antagonists, analgesics, antiepileptics, anxiolytics, sedatives, antidepressants, hip fracture, stroke and myocardial infarction. BPSD groups: no BPSD (total NPI score, 0 points), mild BPSD (NPI, 1–3 points on ≥1 item), moderate BPSD (NPI, 4–8 points on ≥1 item), severe BPSD (NPI, 9–12 points on ≥1 item). Proportional hazards assumption with Schoenfeld residuals with a global p value of 0.3575 for the whole model.
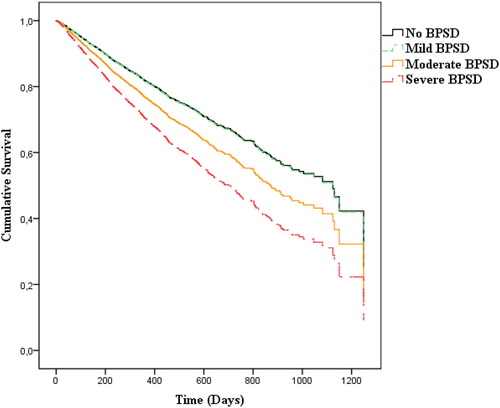
A Cox regression was then performed with the categorized BPSD groups. In the fully adjusted model, the increased risk of death compared with the group with the no BPSD group was 31% (HR 1.31; 95% CI 1.08–1.60) for the moderate BPSD group and 74% (HR 1.74; 95% CI 1.44–2.12) for the severe BPSD group (). No statistically significant difference was found between mild BPSD and the group with no BPSD. In addition to age, male sex, all the comorbidities as well as medication with antipsychotics were significantly associated with an increased mortality risk in this model (). Antidepressants and AChEIs were still associated with a decreased risk of death. There was a tendency towards a decrease in mortality for VaD (HR 0.87; 95% CI 0.76–1.00) ().
Table 3. Association between BPSD and mortality in 11,303 individuals with dementia; degree of BPSD was used as a measure of BPSD.
Total scores for each of the 12 NPI items were then used in a third Cox regression model. Hallucinations (HR 1.02; 95% CI 1.00–1.03), agitation (HR 1.04; 95% CI 1.02–1.05), apathy (HR 1.03; 95% CI 1.02–1.04) and eating changes (HR 1.06; 95% CI 1.05–1.07) were associated with increased mortality, whereas delusions (HR 0.98; 95% CI 0.97–1.00) and euphoria (HR 0.93; 95% CI 0.90–0.95) were associated with decreased mortality (). VaD, treatment with antidepressants and AChEIs remained significantly associated with a decrease in mortality risk. Antipsychotics and anxiolytics showed no significant association with mortality. Increasing age, male sex and all comorbidities were all significantly associated with an increase in mortality ().
Table 4. Association between BPSD and mortality in 11,303 individuals with dementia; total item score for all 12 NPI items was used as a measure of BPSD.
Number of mild, moderate and severe NPI items
To further explore the data, we performed a fourth Cox regression model introducing the number of mild, moderate and severe NPI items as a measure of BPSD. An increase in mortality was observed for each additional moderate item (HR 1.05; 95% CI 1.03–1.08) and each additional severe item (HR 1.10; 95% CI 1.08–1.13) after adjustment for all covariates. There was no association between the number of mild NPI items and mortality (HR 1.00; 95% CI 0.97–1.03). VaD (HR 0.87; 95% CI 0.76–1.00), antidepressants (HR 0.82; 95% CI 0.75–0.89) and AChEI (HR 0.80; 95% CI 0.70–0.91) remained significantly associated with a decrease in mortality. Age (HR 1.05; 95% CI 1.05–1.06), male sex (HR 1.46; 95% CI 1.34–1.59), MI (HR 1.17; 95% CI 1.04–1.31), hip fracture (HR 1.12; 95% CI 1.02–1.23) and stroke (HR 1.35; 95% CI 1.22–1.50) were all significantly associated with increase in mortality. There was no significant association between antipsychotics (HR 1.12; 95% CI 1.00–1.26) or anxiolytics (HR 0.90; 95% CI 0.80–1.00) and mortality in this model.
Discussion
BPSD is a common feature of dementia and is not only the cause of enormous suffering for the individuals and their families, it is also deleterious. In this registry-based study of 11,448 nursing home patients with dementia, we found an increase in mortality associated with the presence and higher severity of BPSD. This finding was independent of age, sex, dementia diagnosis, medication, previous hip fracture, MI and stroke. In addition, we found that categorization of total NPI scores into no/mild/moderate/severe BPSD revealed a stepwise increase in mortality for the moderate and severe categories but not for the mild BPSD category.
The relationship between BPSD and mortality is complex and several factors such as age, gender, dementia diagnosis, dementia severity, other medical conditions and medications need to be considered. There are several studies suggesting increased mortality for antipsychotic treatment, which is used for several neuropsychiatric symptoms such as hallucinations, delusions, agitation and aggression (Kales et al., Citation2012). However, results from studies including the presence of neuropsychiatric symptoms diverge from those without, by not confirming an increase in mortality risk for antipsychotic treatment (Lopez et al., Citation2013; Selbaek et al., Citation2016). In our study, we aimed to include several important covariates to test our hypothesis that the presence of BPSD itself increases mortality risk.
First, we performed fully adjusted multivariable Cox regression, which revealed a 1% increase in mortality risk per 1 point increase in total NPI score. This is in line with previous results (Connors et al., Citation2016). However, even though the direction of the results is similar, they are not fully comparable, because the data in the previous study did not include nursing home patients, indicating less severe dementia than in our study. Another large Norwegian study on 1163 nursing home residents with dementia revealed contradictory results with no independent increase in long-term mortality for BPSD (Selbaek et al., Citation2016). One explanation for these different results might be the accessibility of different covariates in the respective studies. The Norwegian nursing home residents had moderate dementia severity, whereas we did not have access to data of corresponding dementia severity. Another possible explanation for the differences in outcome might be different traditions of medication for BPSD in different countries. In the Norwegian data, 24% had antipsychotic treatment (Selbaek et al., Citation2016). In our study, 16% were on antipsychotics and in a British nursing home study, more than 40% were on antipsychotics (Margallo-Lana et al., Citation2001). On the contrary, the proportion on antidepressants in our study was 41% compared with 16% in the British study and 38% in the Norwegian study (Margallo-Lana et al., Citation2001; Selbaek et al., Citation2016). With regard to anti-dementia treatment, only 2% of the British patients was on cognitive enhancers compared with 11% in the Norwegian study and 26% in our data. Hence, this seems to confirm that pharmaceutical treatments differ among countries.
In previous studies, the total NPI score has been used to study BPSD (Steinberg et al., Citation2014; Wu, Low, Xiao, & Brodaty, Citation2009). A disadvantage of this approach is that the total score can comprise low scores for several different NPI items with limited clinical significance and yet result in a high total score indicating the opposite. By separately studying each NPI item and defining the degree of BPSD according to the highest total item score, the prevalence of BPSD could be described more appropriately. Therefore, we categorized the participants into groups based on their highest score on any of the 12 NPI items assessed and introduced four BPSD categories: no/mild/moderate/severe. Cox regression revealed a stepwise increase in mortality risk with a 31% increase for the moderate group and a 74% increase for the severe BPSD group. The mild BPSD category showed no increase in mortality when no BPSD was used a reference. However, the effect size of the described associations can be discussed. The use of relative effect sizes such as the Cohen’s d for measures of risk proposed for binary correlation coefficients has been suggested (Chen, Cohen, & Chen, Citation2010; Olivier, May, & Bell, Citation2017). The levels of HR of 1.22, 1.86, and 3.00 are proposed to correspond to small, medium, and large effect sized, respectively (Olivier et al., Citation2017). Hence, the HR of 1.31 for the moderate BPSD group would be of small effect size and the HR of 1.74 for the severe BPSD group would be of medium effect size, which we consider is of clinical relevance. We believe that, at least individuals with moderate BPSD as previously defined in the methods section are easily identified related to the frequency or severity the symptom(s), and their increased mortality risk should be noted.
Further, we found that the presence of hallucinations, agitation, apathy and eating changes were independently associated with increased mortality risk in the adjusted model. The hypothesis that the presence of psychiatric symptomatology, and not the drug treatment of the same symptoms, was responsible for the negative outcome (Lopez et al., Citation2013) is supported by our data. The highest mortality risk was found for eating changes with 6% increase per 1-point increase. Difficulties with eating, loss of appetite and weight loss are very frequent in patients with advanced dementia (Finucane, Christmas, & Travis, Citation1999). Hence, this may be an indicator of advanced dementia and death (Hanson, Ersek, Lin, & Carey, Citation2013).
The presence of agitation also increased the risk of a negative outcome. Agitation has been defined as inappropriate verbal, vocal or motor activity that does not result directly from a patient’s needs or from confusion (Cohen-Mansfield & Billig, Citation1986). The presence of agitation can lead to greater use of restraints and psychotropic medication (Testad, Ballard, Bronnick, & Aarsland, Citation2010). However, prediction of mortality was stable even after adjustment for medication and comorbidity, but the association with mortality is complex and the direct causality is not clear. Studies on specific BPSD items and mortality are scarce. One study on disruptive behaviour in Alzheimer dementia showed no association between agitation and mortality, however those data were derived from outpatient clinics and consequently represented a population with less severe dementia (Scarmeas et al., Citation2007). Hence, further longitudinal studies are needed to unravel the effect of agitation on the life span in dementia.
Finally, in the Cox regression analysis using the number of mild, moderate and severe NPI items, we found a 5% increase in mortality risk for each additional item of moderate degree and a 10% increase per additional severe item. Thus, the finding that an increase in BPSD is independently associated with an increase in mortality seems stable and remains after relevant multivariable adjustment.
Dementia diagnosis and mortality
The data indicating a 13%−14% reduced mortality risk for the VaD diagnosis was rather unexpected. In a previous Swedish registry-based study, all dementia diagnoses, including VaD, were associated with a higher mortality than AD (Garcia-Ptacek et al., Citation2014). However, that study did not include data on BPSD and involved individuals with less advanced dementia. A possible explanation for the diverging results might also be that cases with severe stroke died and our results represent individuals exposed to a less serious vascular burden.
Medication and mortality
Antidepressant treatment was associated with a reduced mortality risk of 18 − 19%, in accordance with one previous study with the same reduced mortality risk (Enache et al., Citation2016). We also found that AChEI treatment was associated with a 19 − 20% decrease in mortality. This is consistent with the results of a previous Swedish study that linked AChEI to reduced mortality in AD (Nordstrom, Religa, Wimo, Winblad, & Eriksdotter, Citation2013). It was hypothesized that the side effects of AChEI on the cardiovascular system could improve cardiac function, reduce oxygen demands and possibly thereby reduce the risk of MI and death.
Comorbidities and mortality
We found that previous MI increased mortality risk by 16 − 18% and previous stroke by 30 − 35%. Ischemic heart disease together with stroke is the leading cause of death (World Health Organization, Citation2018). Our data are in accordance with that. Finally, we confirmed previous findings of an increased mortality risk for hip fractures (Tarazona-Santabalbina et al., Citation2015; Tolppanen et al., Citation2016; Wang et al., Citation2014; Weller & Schatzker, Citation2004; Zhao, Shen, & Ji, Citation2012). Individuals with dementia have a high risk of falls that can be attributed to visuospatial decline or loss of balance among several other factors.
Limitations
There are some limitations of this study. First, there was no control group, but as the BPSD registry contains data on all degrees of BPSD, including individuals with no BPSD, this latter group served as a reference group. Second, there is no indicator of dementia severity in our data, which might have contributed to some of our divergent results compared with other studies. Data in the BPSD registry does not include information on cognitive test scores indicating level of cognitive impairment, or severity of dementia defined by instruments such as the Clinical Dementia Rating Scale (CDR). Nor does it contain information on functional status. Hence, we are not able to control for degree of cognitive impairment/dementia severity. However, 87% of the study participants were nursing home residents and dependent on care to manage their daily lives, which is indicative of a severe dementia stage. In addition, one of the demands for nursing home placement in Sweden is an inability to manage ordinary housing and hence by definition, we are convinced that the great majority of our study participants have a severe dementia status. Further, we have adjusted all regression models with a large number of covariates known to be associated with mortality. Despite this, the lack of information on dementia severity needs to be taken into consideration when interpreting the study results. Third, registry data may not always mirror reality exactly because a large number of assessments are performed and added by many different assessors. Despite this, a systematic and widely used instrument such as the NPI-NH is likely to be satisfactory when studying BPSD.
Conclusions
In summary, our data reveal an association between the risk of mortality and BPSD that was independent of other factors. There was a stepwise increase in mortality risk for moderate and severe BPSD. Furthermore, the specific symptoms eating changes, agitation, apathy and hallucinations were associated with higher mortality risk. The results may be important because better and more directed management of BPSD in dementia care might have the potential to contribute to a reduction in mortality among people with dementia.
Acknowledgments
The authors thank Alicja Wizert for statistical support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Banerjee, S. (2012). The macroeconomics of dementia – Will the world economy get Alzheimer’s disease? Archives of Medical Research, 43(8), 705–709. doi:10.1016/j.arcmed.2012.10.006
- Bunn, F., Burn, A.-M., Goodman, C., Rait, G., Norton, S., Robinson, L., … Brayne, C. (2014). Comorbidity and dementia: A scoping review of the literature. BMC Medicine, 12(1), 192. doi:10.1186/s12916-014-0192-4
- Cerejeira, J., Lagarto, L., & Mukaetova-Ladinska, E. B. (2012). Behavioral and psychological symptoms of dementia. Frontiers in Neurology, 3, 73. doi:10.3389/fneur.2012.00073
- Cermakova, P., Johnell, K., Fastbom, J., Garcia-Ptacek, S., Lund, L. H., Winblad, B., … Religa, D. (2015). Cardiovascular diseases in ∼30,000 Patients in the Swedish Dementia Registry. Journal of Alzheimer's Disease, 48(4), 949–958. doi:10.3233/JAD-150499
- Chen, H., Cohen, P., & Chen, S. (2010). How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics – Simulation and Computation, 39(4), 860–864.
- Cohen-Mansfield, J., & Billig, N. (1986). Agitated behaviors in the elderly. I. A conceptual review. Journal of the American Geriatrics Society, 34(10), 711–721. doi:10.1111/j.1532-5415.1986.tb04302.x
- Connors, M. H., Ames, D., Boundy, K., Clarnette, R., Kurrle, S., Mander, A., … Brodaty, H. (2016). Predictors of mortality in dementia: The PRIME Study. Journal of Alzheimer's Disease, 52(3), 967–974. doi:10.3233/JAD-150946
- Cummings, J. (2005–2017). npiTEST. Retrieved from http://npitest.net/about-npi.html
- Cummings, J. (2009). Neuropsychiatric Inventory Nursing Home Version (NPI-NH). Comprehensive assessment of psychopathology in patients with dementia resicing in nursing homes. Retrieved from http://dementiamanagementstrategy.com/File.axd?id=c9f7405f-3596-4f5f-9f8d-f322e5188678
- Cummings, J. L., Mega, M., Gray, K., Rosenberg-Thompson, S., Carusi, D. A., & Gornbein, J. (1994). The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology, 44(12), 2308–2314. doi:10.1212/WNL.44.12.2308
- Enache, D., Fereshtehnejad, S.-M., Kåreholt, I., Cermakova, P., Garcia-Ptacek, S., Johnell, K., … Eriksdotter, M. (2016). Antidepressants and mortality risk in a dementia cohort: Data from SveDem, the Swedish Dementia Registry. Acta Psychiatrica Scandinavica, 134(5), 430–440. doi:10.1111/acps.12630
- Finucane, T. E., Christmas, C., & Travis, K. (1999). Tube feeding in patients with advanced dementia: A review of the evidence. JAMA, 282(14), 1365–1370. doi:10.1001/jama.282.14.1365
- Garcia-Ptacek, S., Farahmand, B., Kareholt, I., Religa, D., Cuadrado, M. L., & Eriksdotter, M. (2014). Mortality risk after dementia diagnosis by dementia type and underlying factors: A cohort of 15,209 patients based on the Swedish Dementia Registry. Journal of Alzheimer's Disease, 41(2), 467–477. doi:10.3233/JAD-131856
- Hanson, L. C., Ersek, M., Lin, F. C., & Carey, T. S. (2013). Outcomes of feeding problems in advanced dementia in a nursing home population. Journal of the American Geriatrics Society, 61(10), 1692–1697. doi:10.1111/jgs.12448
- Kales, H. C., Kim, H. M., Zivin, K., Valenstein, M., Seyfried, L. S., Chiang, C., … Blow, F. C. (2012). Risk of mortality among individual antipsychotics in patients with dementia. American Journal of Psychiatry, 169(1), 71–79. doi:10.1176/appi.ajp.2011.11030347
- Kamiya, M., Sakurai, T., Ogama, N., Maki, Y., & Toba, K. (2014). Factors associated with increased caregivers’ burden in several cognitive stages of Alzheimer’s disease. Geriatrics & Gerontology International, 14(Suppl 2), 45–55. doi:10.1111/ggi.12260
- Liu, M.-E., Tsai, S.-J., Chang, W.-C., Hsu, C.-H., Lu, T., Hung, K.-S., … Chang, W.-P. (2013). Population-based 5-year follow-up study in Taiwan of dementia and risk of stroke. PLoS One, 8(4), e61771. doi:10.1371/journal.pone.0061771
- Lopez, O. L., Becker, J. T., Chang, Y.-F., Sweet, R. A., Aizenstein, H., Snitz, B., … Klunk, W. E. (2013). The long-term effects of conventional and atypical antipsychotics in patients with probable Alzheimer’s disease. American Journal of Psychiatry, 170(9), 1051–1058. doi:10.1176/appi.ajp.2013.12081046
- Lopez, O. L., Becker, J. T., Sweet, R. A., Klunk, W., Kaufer, D. I., Saxton, J., … DeKosky, S. T. (2003). Psychiatric symptoms vary with the severity of dementia in probable Alzheimer’s disease. The Journal of Neuropsychiatry and Clinical Neurosciences, 15(3), 346–353. doi:10.1176/jnp.15.3.346
- Margallo-Lana, M., Swann, A., O'Brien, J., Fairbairn, A., Reichelt, K., Potkins, D., … Ballard, C. (2001). Prevalence and pharmacological management of behavioural and psychological symptoms amongst dementia sufferers living in care environments. International Journal of Geriatric Psychiatry, 16(1), 39–44. doi:10.1002/1099-1166(200101)16:1<39::AID-GPS269>3.0.CO;2-F
- Nordstrom, P., Religa, D., Wimo, A., Winblad, B., & Eriksdotter, M. (2013). The use of cholinesterase inhibitors and the risk of myocardial infarction and death: A nationwide cohort study in subjects with Alzheimer’s disease. European Heart Journal, 34(33), 2585–2591. doi:10.1093/eurheartj/eht182
- Olivier, J., May, W. L., & Bell, M. L. (2017). Relative effect sizes for measures of risk. Communications in Statistics: Theory and Methods, 46(14), 6774–6781. doi:10.1080/03610926.2015.1134575
- Robins Wahlin, T. B., & Byrne, G. J. (2011). Personality changes in Alzheimer’s disease: A systematic review. International Journal of Geriatric Psychiatry, 26(10), 1019–1029. doi:10.1002/gps.2655
- Scarmeas, N., Brandt, J., Blacker, D., Albert, M., Hadjigeorgiou, G., Dubois, B., … Stern, Y. (2007). Disruptive behavior as a predictor in Alzheimer disease. Archives of Neurology, 64(12), 1755–1761. doi:10.1001/archneur.64.12.1755
- Seitz, D. P., Adunuri, N., Gill, S. S., & Rochon, P. A. (2011). Prevalence of dementia and cognitive impairment among older adults with hip fractures. Journal of the American Medical Directors Association, 12(8), 556–564. doi:10.1016/j.jamda.2010.12.001
- Selbaek, G., Aarsland, D., Ballard, C., Engedal, K., Langballe, E. M., Benth, J. S., & Bergh, S. (2016). Antipsychotic drug use is not associated with long-term mortality risk in Norwegian nursing home patients. Journal of the American Medical Directors Association, 17(5), 461.e1-7. doi:10.1016/j.jamda.2016.01.016
- Selbaek, G., Kirkevold, Ø., & Engedal, K. (2007). The prevalence of psychiatric symptoms and behavioural disturbances and the use of psychotropic drugs in Norwegian nursing homes. International Journal of Geriatric Psychiatry, 22(9), 843–849. doi:10.1002/gps.1749
- Shin, I. S., Carter, M., Masterman, D., Fairbanks, L., & Cummings, J. L. (2005). Neuropsychiatric symptoms and quality of life in Alzheimer disease. American Journal of Geriatric Psychiatry, 13(6), 469–474. doi:10.1176/appi.ajgp.13.6.469
- Siafarikas, N., Selbaek, G., Fladby, T., Šaltytė Benth, J., Auning, E., & Aarsland, D. (2018). Frequency and subgroups of neuropsychiatric symptoms in mild cognitive impairment and different stages of dementia in Alzheimer’s disease. International Psychogeriatrics, 30(1), 103–113. doi:10.1017/S1041610217001879
- SPSS, I. (2016). SPSS (Version 24.0). Chicago: SPSS Inc.
- Steinberg, M., Hess, K., Corcoran, C., Mielke, M. M., Norton, M., Breitner, J., … Tschanz, J. (2014). Vascular risk factors and neuropsychiatric symptoms in Alzheimer’s disease: The Cache County Study. International Journal of Geriatric Psychiatry, 29(2), 153–159. doi:10.1002/gps.3980
- Steinberg, M., Shao, H., Zandi, P., Lyketsos, C. G., Welsh-Bohmer, K. A., Norton, M. C., Breitner, J. C. S., & Tschanz, J. T., Cache County Investigators (2008). Point and 5-year period prevalence of neuropsychiatric symptoms in dementia: The Cache County Study. International Journal of Geriatric Psychiatry, 23(2), 170–177. doi:10.1002/gps.1858
- Tarazona-Santabalbina, F. J., Belenguer-Varea, Á., Rovira Daudi, E., Salcedo Mahiques, E., Cuesta Peredó, D., Doménech-Pascual, J. R., … Avellana Zaragoza, J. A. (2015). Severity of cognitive impairment as a prognostic factor for mortality and functional recovery of geriatric patients with hip fracture. Geriatrics & Gerontology International, 15(3), 289–295. doi:10.1111/ggi.12271
- Testad, I., Ballard, C., Bronnick, K., & Aarsland, D. (2010). The effect of staff training on agitation and use of restraint in nursing home residents with dementia: A single-blind, randomized controlled trial. The Journal of Clinical Psychiatry, 71(01), 80–86. doi:10.4088/JCP.09m05486oli
- Todd, S., Barr, S., Roberts, M., & Passmore, A. P. (2013). Survival in dementia and predictors of mortality: A review. International Journal of Geriatric Psychiatry, 28(11), 1109–1124. doi:10.1002/gps.3946
- Tolppanen, A. M., Taipale, H., Tanskanen, A., Tiihonen, J., & Hartikainen, S. (2016). Comparison of predictors of hip fracture and mortality after hip fracture in community-dwellers with and without Alzheimer’s disease – Exposure-matched cohort study. BMC Geriatrics, 16(1), 204. doi:10.1186/s12877-016-0383-2
- Toot, S., Swinson, T., Devine, M., Challis, D., & Orrell, M. (2017). Causes of nursing home placement for older people with dementia: A systematic review and meta-analysis. International Psychogeriatrics, 29(2), 195–208. doi:10.1017/S1041610216001654
- The Swedish BPSD Registry. (2010). Retrieved from https://bpsd.se/in-english/
- The National Board of Health and Welfare. (2019, May 20). The National patient register. Retrieved from https://www.socialstyrelsen.se/en/statistics-and-data/registers/alla-register/the-national-patient-register/
- The National Board of Health and Welfare. (2017). Nationella riktlinjer för vård och omsorg vid demenssjukdom (Report No 2017-12-2). [National guidelines for dementia care]. The National Board of Health and Welfare, Sweden
- Wang, H.-K., Hung, C.-M., Lin, S.-H., Tai, Y.-C., Lu, K., Liliang, P.-C., … Li, Y.-C. (2014). Increased risk of hip fractures in patients with dementia: A nationwide population-based study. BMC Neurology, 14(1), 175. doi:10.1186/s12883-014-0175-2
- Weller, I., & Schatzker, J. (2004). Hip fractures and Alzheimer’s disease in elderly institutionalized Canadians. Annals of Epidemiology, 14(5), 319–324. doi:10.1016/j.annepidem.2003.08.005
- Wood, S., Cummings, J. L., Hsu, M. A., Barclay, T., Wheatley, M. V., Yarema, K. T., & Schnelle, J. F. (2000). The use of the neuropsychiatric inventory in nursing home residents. Characterization and measurement. The American Journal of Geriatric Psychiatry, 8(1), 75–83. doi:10.1097/00019442-200002000-00010
- World Health Organization. (2019). Dementia. Fact sheet. Retrieved from https://www.who.int/news-room/fact-sheets/detail/dementia
- World Health Organization. (2018). The top 10 causes of death. Fact sheet. Retrieved from https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- Wu, H. Z., Low, L. F., Xiao, S., & Brodaty, H. (2009). A pilot study of differences in behavioral and psychological symptoms of dementia in nursing home residents in Sydney and Shanghai. International Psychogeriatrics, 21(03), 476–484. doi:10.1017/S1041610209008643
- Zhao, Y., Shen, L., & Ji, H. F. (2012). Alzheimer’s disease and risk of hip fracture: A meta-analysis study. Scientific World Journal, 2012, 1–5. doi:10.1100/2012/872173