Abstract
Objectives
This study investigates specialist healthcare visits of older people with intellectual disability ID having affective and anxiety diagnoses in comparison with the general population, as well as across different levels of ID, behavioural impairment, and living in special housing in Sweden.
Method
The study is a retrospective national-register-based study from 2002–2012 of people with ID 55 years and older (n = 7936) and a control group the same size matched by birth year and sex from the general population at the end of study. The study groups comprised those with affective (n = 918) and anxiety (n = 825) diagnoses who visited specialist healthcare, including data about living in special housing at the end of study in 2012.
Results
Older people with ID and with affective and anxiety diagnoses have a higher risk of inpatient and unplanned visits to psychiatric and somatic healthcare than the general population. The average length of stay in inpatient psychiatric healthcare was higher in older people with ID and anxiety diagnoses than in the general population. Within the ID group, more inpatient and unplanned visits were made by those with moderate and severe levels of ID, behavioural impairment, and living in special housing.
Conclusion
Older people with ID and affective and anxiety diagnoses are more likely to have inpatient and unplanned visits for specialist healthcare than the general population. Future research should explore the quality of healthcare services delivered by healthcare providers to older people with ID and with affective and anxiety diagnoses.
Background
Affective and anxiety diagnoses have a higher occurrence in older people with intellectual disability (ID) than the general population (Axmon et al., Citation2018; Hermans, Beekman, & Evenhuis, Citation2013; McCarron et al., Citation2013). Also, a recent study (El Mrayyan et al., Citation2019) confirms the high morbidity and frailty in older people with ID, with results showing that the occurrence of psychiatric comorbidities was 11 times higher in those with ID and with affective and anxiety disorders than the general population. Most of the psychiatric comorbidities were unspecified diagnoses, which reflect the difficulty of diagnosing in older people with ID. In contrast, lower rates of somatic comorbidities to affective and anxiety disorders were reported in older people with ID than the general population (El Mrayyan et al., Citation2019). Despite knowledge of the higher occurrence of psychiatric disorders, the healthcare utilisation patterns in older people with ID with affective and anxiety diagnoses have not yet been studied.
Affective and anxiety diagnoses are reliant to a great extent on the self-report of symptoms. People with little or no communication skills, such as people with ID, are therefore more difficult to diagnose. This means that people with a mild level of ID can more easily report affective and anxiety symptoms than people with severe ID. The diagnostic criteria used for affective and anxiety diagnoses in the general population are more appropriate for people with mild ID (Hermans, Beekman, & Evenhuis, Citation2014; Hermans & Evenhuis, Citation2013) than for people with more severe ID. Furthermore, the literature reports that affective and anxiety diagnoses in people with a severe level of ID are more complicated since the symptoms are usually overshadowed by behavioural impairment (Ji & Findling, Citation2016; Lunsky & Balogh, Citation2010; McBrien, Citation2003; Myrbakk & von Tetzchner, Citation2008).
As a result of increased life expectancy, the number of people with ID and complex diseases has increased (Cooper, Smiley, Morrison, Williamson, & Allan, Citation2007; Hermans & Evenhuis, Citation2014; McCarron et al., Citation2013). In parallel with ageing, the increased number of complex disease problems has led to adverse health outcomes such as longer hospitalisation, higher health cost, increased risk of hospitalisation, and decreased quality of life (Emerson & Baines, Citation2011; Lunsky & Balogh, Citation2010; Wu, Desarkar, Palucka, Lunsky, & Liu, Citation2013). In the general population, affective and anxiety diagnoses have been associated with higher healthcare utilisation and cost among individuals with diabetes (Huang et al., Citation2015; Kyung Lee & Hee Lee, Citation2014), cancer (Mausbach & Irwin, Citation2017), spinal cord injury (Ullrich, Smith, Blow, Valenstein, & Weaver, Citation2014), and chronic obstructive pulmonary disease (COPD) (Albrecht et al., Citation2017). Similarly, in older people with ID, several studies have reported longer hospitalisation with psychiatric diagnoses, diabetes, cancer, and vision problems but also inadequate healthcare access compared to the general population (Axmon et al., Citation2016; Lunsky & Balogh, Citation2010; McCarron, Cleary, & McCallion, Citation2017; Perkins & Moran, Citation2010)
Staff and managers in intellectual disability services have expressed in interview studies having limited knowledge regarding how to identify when decreased physical or mental abilities are due to the ageing process or to the disability itself (Alftberg et al., Citation2019; Holst et al., Citation2018; Johansson et al., Citation2017). This uncertainty among staff and managers can contribute to inadequate healthcare access in addition to the decreased ability of people with ID to express the symptoms and problems they experience (Axmon et al., Citation2016; Sandberg et al., Citation2016). Previous studies of older people with ID in comparison to the general population have shown that younger people with ID were found to utilise more inpatient and outpatient healthcare (Axmon et al., Citation2016; Sandberg et al., Citation2016). Also, these studies showed longer stays in psychiatric inpatient services and higher risk of somatic healthcare utilisation in younger than older age groups in people with ID than in the general population. Among people with ID, living in residential housing services or group homes was associated with fewer psychiatric inpatient visits (Axmon et al., Citation2016). However, although affective and anxiety disorders are more common in older people with ID than the general population, we have not been able to identify any study of healthcare utilisation specifically for these diagnoses. A deeper understanding of the healthcare utilisation patterns of people with ID and with affective and anxiety disorders is needed, as we might expect this group to be a more vulnerable group than others with ID. Therefore, the aim of this study was to investigate specialist psychiatric and somatic healthcare utilisation in older people with ID having affective and/or anxiety diagnoses in comparison with the general population, and moreover, within the ID cohort, to investigate healthcare utilisation regarding different levels of ID, behavioural impairment, and type of living situation.
Methods
Study design
This study was designed as a retrospective register-based study from three Swedish national registries, covering 11 years from 2002–2012.
The Swedish welfare and healthcare setting
The Swedish healthcare system is funded by public taxes and is mainly operated by the county councils and municipalities. The National Board of Health and Welfare ensures that everyone has equal access to good health and social care in Sweden. This authority is responsible for health data and social service registries that allow trends in health and social care to be followed by producing statistics, knowledge about health and social care, and regulations from the government (The National Board of Health & Welfare, Citation2019). The law that regulates the Swedish healthcare system is the Health and Medical Services Act. County councils are required by this act to promote and ensure equal access to healthcare to all residents based on healthcare needs (SFS 2017:30, 2017). Good health and social care should be based on the best available knowledge, provided with respect to the specific need of individuals, and should be accessible and safe, efficient, and equally distributed for all individuals (SFS 2018:347, 2018). In addition, the Social Service Act also gives older people and those with disabilities the right to receive public services and enjoy good living conditions in everyday life (SFS 2018:347, 2018). People with disabilities are also eligible for support under an act concerning support and services for persons with certain functional impairments (LSS Act) (SFS 1993:387, 1993). The LSS Act (SFS 1993:387) gives people with permanent functional impairment or disabilities the right to receive social support services to ensure equal living conditions to the general population.
Registers used in the study
LSS register
The services provided according to the criteria of the LSS Act are recorded in the LSS Register. The LSS services and support include eight measures for adults, such as personal assistance, companion service, and relief services in home and daily activities. In this study, the data are from the LSS Register for Person Group 1, which includes those individuals having intellectual disability, autism, or autism spectrum disorders.
TPR
The Swedish Total Population Register (TPR) contains information such as age, sex, civil status, address, and personal identity numbers for Swedish citizens. The TPR is administered by the Swedish Tax Agency and maintained by Statistics Sweden, which is the authorised source of population statistics in Sweden.
NPR
The National Patient Register (NPR) includes all inpatient and outpatient psychiatric and somatic specialist healthcare in Sweden, public as well as private. The register does not contain information about primary healthcare. The NPR provides information about health and healthcare utilisation in the population to improve the ability to prevent and treat diseases and monitor the healthcare system (Ludvigsson et al., Citation2016). The information in the NPR is divided into four parts: Personal data (e.g. age, gender, personal identity number), geographical data (e.g. county, hospital/clinic), administrative inpatient and outpatient data (e.g. date of admission and discharge, if the visit was planned or unplanned), and medical data (e.g. primary and up to 21 secondary diagnosis). The diagnosis is based on the ICD-10 code classification and the diagnosis is registered at discharge for inpatients. The National Board of Health and Welfare is the responsible authority for both the LSS Register and NPR.
Study population
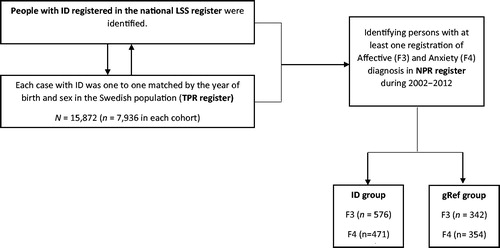
The study population was selected from two national populations (). The first population group, all people with at least one of the support measures according the LSS Act, were identified through the national LSS Register and consisted of 7,936 older people with ID, autism, and autism spectrum disorders (ID-group) aged 55 or older and alive at the end of the year 2012. The reason for choosing 55 or older as an inclusion criterion is based on previous research acknowledging that people with ID age earlier than those in the general population (Coppus, Citation2013). The second population group consists of 7,936 people from the Swedish total population who were matched with each case in the ID cohort (1:1) by year of birth and sex in the TPR. Thus, the total population of 15,872 consisted of 7,936 in the ID group and an equal number in the general population group ().
Study groups
Two study groups, the ID group and the general population reference group (gRef), were drawn from the two study population groups above based on the criterion that the included persons should have been diagnosed with at least one affective disorder (F3) and/or anxiety disorder (F4) as primary or secondary diagnosis (). The diagnoses were based on the International Classification of Diseases ICD-10 codes from the NPR during 2002–2012. Thus, in the study groups () the proportion of identified individuals diagnosed with at least one affective (F3) diagnosis was 66% in those with ID and 61% in the gRef. Moreover, those with at least one anxiety (F4) diagnosis made up 54% of ID and 64% of gRef.
Outcome measures
The healthcare utilisation data in the NPR were classified for each individual having at least one visit concerning an F3 or F4 diagnosis during 2002–2012 in the two study groups. The healthcare utilisation regarding psychiatric or somatic healthcare was identified based on the clinic which the individuals visited. Data about inpatient and outpatient specialist healthcare, planned/unplanned visits, and inpatient length of stay (LOS) in days were included. Moreover, information on the individual level with at least one visit was considered for all outcome measures with at least one F3 and F4 diagnosis during the study period. This was done for all outcomes as well as within the ID group.
Regarding the individuals diagnosed with at least one F7 (Intellectual disability) diagnosis, the third digits of the ICD-10 codes were used to identify the levels of ID as mild (F70), moderate (F71), or severe and profound (F72, F73). These levels were then used to investigate the healthcare utilisation at different levels of ID. Individuals with other/unspecified levels of ID (F78, F79) were excluded from this analysis. Moreover, we identified healthcare utilisation concerning the presence of behavioural impairment in individuals with ID based on ICD-10 four digits codes such as F70.1 (Mild intellectual disability with significant impairment of behaviour requiring attention or treatment) with F3 and F4 diagnoses. Furthermore, data from the LSS Register about living in special housing was included for those in the ID group.
Statistical analysis
Data were analysed using IBM SPSS software version 25.0 program. Descriptive data about healthcare utilisation visits were presented using frequencies and percentages. Chi-square analysis was used to test the relationship of categorical outcome variables between the two study groups. For continuous variables with a skewed distribution, the median and quartiles and the Mann-Whitney U-test were used. The healthcare utilisation pattern with affective (F3) and/or anxiety (F4) diagnoses in the ID group were compared with those in gRef using logistic regression analysis to estimate the odds ratio with 95% confidence intervals (CIs). Differences in the inpatient healthcare and LOS of visits were assessed using the Mann-Whitney U-test with median and quartiles, as the data were skewed. Within the ID group, logistic regression analysis was performed regarding behavioural impairment, severity level of ID, and living in special housing on healthcare utilisation. The adjustment was performed in the multivariate analysis for the differences in age at the end of 2012 and sex with the outcomes in ID-group vs gRef, and within the ID group. Within the ID group, the analysis of differences in inpatient healthcare and LOS was performed using the Mann-Whitney U-test and described by median and quartiles, as the data were skewed. p-Values less than 0.05 were considered statistically significant.
Results
Characteristics of healthcare utilisation
The ID group with at least one healthcare visit in the period 2002–2012 was composed of 52% (n = 297) women with at least one affective diagnosis, and the corresponding figure for anxiety diagnosis was 48% (n = 224), with somewhat higher figures for gRef (n = 117, 52% for affective and n = 204, 58% for anxiety) ().
Regarding the total healthcare visits (), there were 10% more women who (p < 0.05) visited healthcare than men and most healthcare visits in younger older age (median age 61 and 60 in ID and 62 and 61 in the gRef group, p < 0.05) with at least one affective and anxiety diagnosis. The total number of specialist healthcare visits for those with affective and anxiety diagnoses were 17,998 and 16,119, respectively, during the study period 2002–2012 (). The proportions of healthcare visits were 70% in ID group and 75% in the gRef group with at least one affective diagnosis. In contrast, there were healthcare visits with the presence of at least one anxiety diagnosis in the ID group, 63%, and gRef group, 67% ().
Table 1. Characteristics of healthcare utilisation in the study groups based on visit level.
Furthermore, there were more psychiatric healthcare visits, 52% (p < 0.05), than somatic healthcare visits, 48%, in the ID group with at least one affective diagnosis (). However, the opposite was found for the ID group with at least one anxiety diagnosis, which visited 8% more somatic healthcare than psychiatric healthcare. In addition, there were significantly (p < 0.05) more planned and outpatient healthcare visits than unplanned and inpatient healthcare visits in both the ID group and the gRef with at least one affective or anxiety diagnosis. Furthermore, among those with at least one anxiety diagnosis, there were 9% more unplanned healthcare visits in the ID versus the gRef group. Finally, within the ID group, there were more visits among older people with a mild level of ID, without behavioural impairment, and living in special housing (). The same pattern was found for the number of individuals with affective and anxiety diagnoses in ID and gRef group (Appendix).
Psychiatric and somatic healthcare utilisation
The results revealed that the ID group had a significantly higher risk of visiting psychiatric versus somatic healthcare than gRef (). The ID group was more likely to have inpatient visits as well as unplanned visits in psychiatric healthcare than the gRef. The same pattern was found regarding somatic healthcare, which showed a higher risk for inpatient and unplanned visits ().
Table 2. Comparison between the study groups psychiatric and somatic healthcare utilisation pattern.
Regarding the inpatient healthcare visits, the total average length of stay (LOS) was slightly higher in the ID group with at least one affective diagnosis than gRef (p < 0.05) (). However, the gRef group had a significantly higher average LOS in somatic healthcare than the ID group with at least one anxiety diagnosis. When assessed on the individual level, the average total inpatient LOS during the study period, we noted a significantly higher median per visits with affective and anxiety diagnoses in individuals of the ID group than gRef (). In addition, there was a higher median for individuals’ LOS in psychiatric healthcare (p < 0.05) with at least one affective diagnosis, and in somatic healthcare LOS (p < 0.05) with at least one anxiety diagnosis, in the ID group than gRef.
Table 3. Comparison between the study groups regarding length of stay in psychiatric and somatic inpatient healthcare.
Healthcare utilisation within the ID group
Within the ID group with affective and anxiety diagnoses (), a consistent pattern was found of a significantly higher risk of inpatient healthcare and a lower risk of planned healthcare visits with behavioural impairment, moderate/severe level of ID, and living in special housing ( and ). Furthermore, as shown in , all significant results remained statistically significant after adjustment within the ID group. On the other hand, mild and moderate/severe level of ID (with affective diagnoses) and behavioural impairment (with anxiety diagnoses) became statistically significant after adjustment in planned compared to unplanned healthcare visits.
Table 4. The number of visits in healthcare utilisation by behavioural impairment, severity level of ID, and living in special housing within the ID group.
Table 5. Odds ratio (OR) and with 95% confidence intervals (CIs) regarding behavioural impairment, severity level of ID, and living in special housing within the ID group.
Within the ID group, the average LOS of healthcare visits was higher among those with behavioural impairment (p < 0.05) than without in both affective and anxiety, and in women (p < 0.05) compared to men with affective diagnoses (). Moreover, the average LOS was higher among those living in special housing (p < 0.05) and with moderate/severe (p < 0.05) than mild levels of ID with at least one anxiety diagnosis ().
Table 6. Length of stay in inpatient healthcare visits within the ID group.
Discussion
In this study, older people with ID and affective and anxiety diagnoses were found to have more inpatient and unplanned healthcare visits in psychiatric and somatic healthcare than the general population. Another important finding was that older people with ID and with anxiety diagnoses have a longer average length of stay in psychiatric healthcare than the general population. Furthermore, increased length of stay in inpatient healthcare can be expected in cases of severe ID and the presence of behavioural impairment, which is in line with the present results. In addition, the results of this study indicate that anxiety combined with more severe levels of ID and behavioural impairment, there is a longer length of stay in inpatient healthcare. However, the finding was unexpected that older people with ID and with anxiety diagnoses living in special housing would have a longer stay in inpatient healthcare. This can be explained by the fact that those with ID who live in special housing such as a group home are in fact more severely ill and are therefore hospitalised longer. Moreover, older people with ID who live in special housing have a higher risk of inpatient and unplanned healthcare visits with affective and anxiety diagnoses. As our data are based on specialist healthcare visits, it is expected to include people with ID with more severe and/or complex problems. This frailty could explain our results about more inpatient and unplanned visits than in the general population with affective and anxiety diagnoses. Furthermore, these results further support the idea that people with ID with more comorbid and complex problems have difficulties in communicating their symptoms properly, which leads to diagnostic overshadowing and increased healthcare utilisation (Mason & Scior, Citation2004; Myrbakk & von Tetzchner, Citation2008). Also, it has been reported that communication difficulties are considered as a barrier to health care utilisation for people with ID (Ali et al., Citation2013; Williamson, Contreras, Rodriguez, Smith, & Perkins, Citation2017). For example, difficulties in understanding the information from healthcare providers lead to decreased knowledge about the healthcare services (Williamson et al., Citation2017). Also, difficulties in expressing their thoughts and needs leads to fear and anxiety, which further limits their ability to communicate effectively with healthcare providers (Raymaker et al., Citation2017; Williamson et al., Citation2017).
A recently published systematic review (van den Bogaard, Lugtenberg, Nijs, & Embregts, Citation2019) focused on reasons for challenging behaviour that people with ID have described in qualitative studies. The results show that interpersonal factors (e.g. staff), environmental factors (e.g. group home and/or health care ward), and intrapersonal factors (e.g. anxiety and/or depression) can be seen as triggers that maintain challenging behaviour (van den Bogaard et al., Citation2019). The role of staff and the environment illustrates the importance of knowledge and awareness of what is needed to provide supportive care to people with ID. The quality of care is a fundamental aspect of care for people with complex and long-term care needs and depends mainly on staff help and support in daily life ( Scheffelaar et al., Citation2019). The staff has to show understanding, patience, and professionalism in providing health care. Furthermore, research shows that people with ID experience significance healthcare disparities, such as high levels of comorbidities and inappropriate medication prescription, compared to people without ID (Axmon et al., Citation2019; Bond et al., Citation2019; Carey et al., Citation2016; Emerson & Baines, Citation2011). A qualitative study on people with mild ID and with anxiety and depression described “feelings of broken” in terms of emotional overwhelmed and physically damaged, fear and uncertainty, rendering them unable to detect warning signs and isolated because of their mental health problems (Tomlinson & Hewitt, Citation2018). Identifying the problem is the first step to addressing their needs and decreasing these healthcare disparities. Therefore, we recommended that staff working in intellectual disability services and healthcare, as well as stakeholders of people with ID and policymakers, work together to identify strategies facilitating an integrated system that meets the needs of people with ID.
This study confirms that older people with ID have higher psychiatric healthcare utilisation than the general population. One explanation is the increased vulnerability in the ID group with a high occurrence of both psychiatric and somatic diagnoses which lead to health disparities and population-specific differences in access to psychiatric healthcare access in older people with ID (El Mrayyan et al., Citation2019; Axmon et al., Citation2016; Cooper et al., Citation2007, Citation2015; Moss, Bouras, & Holt, Citation2001). Another reason might be that people with ID and with depression and anxiety experience barriers such as fear, distress, and isolation because of the unpredictability of their mental health problem, which could increase the burden on specialist healthcare (Tomlinson & Hewitt, Citation2018). Furthermore, people with ID experience negative self-imagery, such as physical unattractiveness and danger to others, leading to a negative impact on their relationships with others (Tomlinson & Hewitt, Citation2018). These barriers might present more challenges for healthcare providers and special housing staff to meet the needs of people with ID.
In Sweden, people with intellectual disability should, according to the LSS Act, receive support and social services from the municipality if they have significant need due to mental impairment and if the disability causes significant difficulties in their daily life (SFS 1993:387, 1993). According to the LSS, social service staff should provide special services for housing, personal assistance, daily activities, companion services, and personal support and counselling. Therefore, this would be expected to decrease inpatient and unplanned visits to specialist healthcare. However, surprisingly, in this study living in special housing was found to increase the risk of inpatient and unplanned healthcare visits for older people with ID and with affective and anxiety diagnoses. This suggests that the resources for caring for ageing people with ID are unlikely to be met in special housing, which thus would increase the demands on specialist healthcare services. These results raise concerns about the competence of staff working in special housing and whether the care services provided meet the needs of older people with ID (Alftberg et al., Citation2019; Holst et al., Citation2018; Johansson et al., Citation2017)).
Our findings raise an interesting question regarding the difficulties and barriers that healthcare providers encounter with older people with ID and with affective and anxiety diagnoses. Even though the basic needs of people with ID are met at the hospital, such as the right medication, food and drinks, and use of the toilet, many people with ID and communication problems described hospital staff as having negative attitudes and a lack of skills and knowledge regarding their needs (Castles, Bailey, Gates, & Sooben, Citation2014; Iacono, Bigby, Unsworth, Douglas, & Fitzpatrick, Citation2014; Iacono & Davis, Citation2003). Healthcare providers reported a lack of knowledge and training barriers with people with ID (Williamson et al., Citation2017). Such barriers involve calming people and explaining the hospital procedures, which makes healthcare providers more likely to communicate with family members or other caregivers than people with ID (Tyler, Schramm, Karafa, Tang, & Jain, Citation2010; Williamson et al., Citation2017). Obviously, people with ID experience health discrepancies compared to the general population, which makes it an important issue to address and ensure equal health services for people with ID. Furthermore, under the Swedish Health and Medical Services Act (SFS 2017:30, 2017), healthcare services are obligated to promote service quality for people with intellectual disability and address their needs with the best appropriate treatment. Therefore, these results increase the need to identify the challenges that healthcare providers encounter in reaching equitable health outcomes in older people with ID.
Providing care for people with ID is more complex than the general population such as the presence of challenging behaviour, and there is a lack of available resources as time and knowledge about this behaviour as well as about intellectual disability among healthcare professionals. These limits providing a high quality of care and also the accessibility of facilities in primary and community healthcare may contribute to excess utilisation of unplanned (acute) specialist healthcare and longer stay in hospitals. Given this problem may cause high dropouts from primary and community healthcare visits and unmotivated unplanned admissions to hospitals (Cooper et al., Citation2018; Spassiani, Abou Chacra, & Lunsky, Citation2017) . Therefore, different healthcare settings need to be adapted with expertise and collaborate to ensure providing appropriate care and enhance continuity of care for people with ID. As such, this might potentially improve community services and primary care leading to a reduced number of unplanned admission. Future intervention is required to provide accessible resources to caregivers in primary and community healthcare and these parties need to take active responsibility for collaboration in providing care of high quality for people with ID and with health problem.
One strength of this study is the use of the national registers with high population coverage in Sweden. The data registration in the NPR used in the present study has high validity, as it is mandatory in all healthcare settings (Ludvigsson et al., Citation2016). Therefore, the present study includes all inpatient and outpatient visits in older people with ID alive during our study period. However, the information missing from the primary healthcare should be taken in consideration. Affective and anxiety diagnoses are treated most commonly in primary healthcare (Sundquist, Ohlsson, Sundquist, & Kendler, Citation2017). The Swedish primary healthcare physician (General Practitioners) will refer the persons to specialists if needed; therefore, we expect that the people included in this study cohort are those with more severe and complex problems with affective and anxiety diagnoses than those treated in primary healthcare. This is in line with a study of healthcare utilisation in primary healthcare that found that people with ID have shorter consultations and lower continuity of care with the same physician than the general population (Carey et al., Citation2016). This could explain why people with ID with complex problems might have more frequent visits to specialist healthcare.
Furthermore, the LSS register data used in the study is based on the authority decision of support and services in accordance to the LSS Act (SFS 1993:387), which highlights the validity of the data used in the study. One of the issues that emerges from using the LSS Register concerns support and services that do not contain information about the ID diagnoses. However, the LSS Register is the best proxy for people with ID on the national level in Sweden. This is the only way to identify a national cohort of ID. The people in the ID group have their disability since early childhood or before 18 years. The diagnoses of ID became as a registration in the patient register (NPR) only if the healthcare visits were due to the ID diagnosis or if the ID could be a contributing cause of the visits (the diagnoses of the ID could be secondary reason of visit). This weakness needs to be in consideration when interpreting the results. The clinical diagnoses of affective and anxiety disorders registered in the NPR are based on a medical assessment which includes difficulties in diagnoses in people with ID compared with people without cognitive and communicative disabilities. However, the data from the NPR about the diagnosis are the best proxies of clinical diagnosis available on a national level.
Conclusion
This study has shown, first, that older people with ID and with affective and anxiety diagnoses have more inpatient and outpatient visits in specialist healthcare than do older people without ID. The second main finding was that people with ID living in special housing have the same healthcare utilisation pattern in specialist healthcare. In general, healthcare providers working with people with ID and affective and anxiety diagnoses have knowledge barriers to communicating and meeting the needs of older people with ID and with affective and anxiety diagnoses.
Acknowledgements
We would like to thank Anna Axmon, Associate Professor in Statistic, Lund University, Sweden for the assistance of extraction of data from the larger data base.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Albrecht, J. S., Khokhar, B., Huang, T.-Y., Wei, Y.-J., Harris, I., Moyo, P., … Simoni-Wastila, L. (2017). Adherence and healthcare utilization among older adults with COPD and depression. Respiratory Medicine, 129, 53–58. doi:10.1016/j.rmed.2017.06.002
- Alftberg, Å., Johansson, M., & Ahlström, G. (2019). Ambivalence among staff regarding ageing with intellectual disabilities: Experiences and reflections. Journal of Intellectual Disabilities. doi:10.1177/1744629519874997.
- Ali, A., Scior, K., Ratti, V., Strydom, A., King, M., & Hassiotis, A. (2013). Discrimination and other barriers to accessing health care: Perspectives of patients with mild and moderate intellectual disability and their carers. PLoS One., 8(8), e70855. doi:10.1371/journal.pone.0070855
- Axmon, A., El Mrayyan, N., Eberhard, J., & Ahlström, G. (2019). Pharmacotherapy for mood and anxiety disorders in older people with intellectual disability in comparison with the general population. BMC Psychiatry, 19(1). doi:10.1186/s12888-019-2191-7.
- Axmon, A., Björne, P., Nylander, L., & Ahlström, G. (2016). Psychiatric care utilization among older people with intellectual disability in comparison with the general population: a register study. BMC Psychiatry, 16(1). doi:10.1186/s12888-016-1094-0.
- Axmon, A., Björne, P., Nylander, L., & Ahlström, G. (2018). Psychiatric diagnoses in older people with intellectual disability in comparison with the general population: a register study. Epidemiology and Psychiatric Sciences, 27(5), 479–491. doi:10.1017/S2045796017000051.
- Bond, L., Carroll, R., Mulryan, N., O'Dwyer, M., O'Connell, J., Monaghan, R., … McCarron, M. (2019). The association of life events and mental ill health in older adults with intellectual disability: Results of the wave 3 Intellectual Disability Supplement to The Irish Longitudinal Study on Ageing. Journal of Intellectual Disability Research, 63(5), 454–465. doi:10.1111/jir.12595
- Carey, I. M., Shah, S. M., Hosking, F. J., DeWilde, S., Harris, T., Beighton, C., & Cook, D. G. (2016). Health characteristics and consultation patterns of people with intellectual disability: A cross-sectional database study in English general practice. British Journal of General Practice, 66(645), e264–e270. doi:10.3399/bjgp16X684301
- Castles, A., Bailey, C., Gates, B., & Sooben, R. (2014). Experiences of the implementation of a learning disability nursing liaison service within an acute hospital setting: A service evaluation. British Journal of Learning Disabilities, 42(4), 272–281. doi:10.1111/bld.12070
- Cooper, S. A., Hughes-McCormack, L., Greenlaw, N., McConnachie, A., Allan, L., Baltzer, M., … Morrison, J. (2018). Management and prevalence of long-term conditions in primary health care for adults with intellectual disabilities compared with the general population: A population-based cohort study. Journal of Applied Research in Intellectual Disabilities, 31 (Suppl 1), 68–81. doi:10.1111/jar.12386
- Cooper, S.-A., McLean, G., Guthrie, B., McConnachie, A., Mercer, S., Sullivan, F., & Morrison, J. (2015). Multiple physical and mental health comorbidity in adults with intellectual disabilities: Population-based cross-sectional analysis. BMC Family Practice, 16(1), 110. doi:10.1186/s12875-015-0329-3
- Cooper, S.-A., Smiley, E., Morrison, J., Williamson, A., & Allan, L. (2007). Mental ill-health in adults with intellectual disabilities: Prevalence and associated factors. British Journal of Psychiatry, 190(1), 27–35. doi:10.1192/bjp.bp.106.022483
- Coppus, A. M. (2013). People with intellectual disability: What do we know about adulthood and life expectancy? Developmental Disabilities Research Reviews, 18. doi:10.1002/ddrr.1123
- El Mrayyan, N., Eberhard, J., & Ahlström, G. (2019). The occurrence of comorbidities with affective and anxiety disorders among older people with intellectual disability compared with the general population: a register study. BMC Psychiatry, 19(1). doi:10.1186/s12888-019-2151-2.
- Emerson, E., & Baines, S. (2011). Health inequalities and people with learning disabilities in the UK. Tizard Learning Disability Review, 16(1), 42–48. doi:10.5042/tldr.2011.0008
- Hermans, H., Beekman, A. T., & Evenhuis, H. M. (2013). Prevalence of depression and anxiety in older users of formal Dutch intellectual disability services. Journal of Affective Disorders, 144(1-2), 94–100. doi:10.1016/j.jad.2012.06.011
- Hermans, H., Beekman, A. T., & Evenhuis, H. M. (2014). Comparison of anxiety as reported by older people with intellectual disabilities and by older people with normal intelligence. The American Journal of Geriatric Psychiatry, 22(12), 1391–1398. doi:10.1016/j.jagp.2013.04.017
- Hermans, H., & Evenhuis, H. M. (2013). Factors associated with depression and anxiety in older adults with intellectual disabilities: Results of the healthy ageing and intellectual disabilities study. International Journal of Geriatric Psychiatry, 28(7), 691–699. doi:10.1002/gps.3872
- Hermans, H., & Evenhuis, H. M. (2014). Multimorbidity in older adults with intellectual disabilities. Research in Developmental Disabilities, 35(4), 776–783. doi:10.1016/j.ridd.2014.01.022
- Holst, G., Johansson, M., & Ahlström, G. (2018). Signs in People with Intellectual Disabilities: Interviews with Managers and Staff on the Identification Process of Dementia. Healthcare, 6(3), 103.doi:10.3390/healthcare6030103.
- Huang, C. J., Chiu, H. C., Hsieh, H. M., Yen, J. Y., Lee, M. H., Chang, K. P., … Lin, C. H. (2015). Health care utilization and expenditures of persons with diabetes comorbid with anxiety disorder: A national population-based cohort study. General Hospital Psychiatry, 37(4), 299–304. doi:10.1016/j.genhosppsych.2015.04.008
- Iacono, T., Bigby, C., Unsworth, C., Douglas, J., & Fitzpatrick, P. (2014). A systematic review of hospital experiences of people with intellectual disability. BMC Health Services Research, 14(1), 327–342. doi:10.1186/s12913-014-0505-5
- Iacono, T., & Davis, R. (2003). The experiences of people with developmental disability in Emergency Departments and hospital wards. Research in Developmental Disabilities, 24(4), 247–264. doi:10.1016/S0891-4222(03)00041-6
- Ji, N. Y., & Findling, R. L. (2016). Pharmacotherapy for mental health problems in people with intellectual disability. Current Opinion in Psychiatry, 29(2), 103–125. doi:10.1097/YCO.0000000000000233
- Johansson, M., Björne, P., Runesson, I., & Ahlström, G. (2017). Healthy Ageing in People with Intellectual Disabilities from Managers’ Perspective: A Qualitative Study. Healthcare, 5(3), 45.doi:10.3390/healthcare5030045.
- Kyung Lee, H., & Hee Lee, S. (2014). Depression, diabetes, and healthcare utilization: Results from the Korean Longitudinal Study of Aging (KLoSA). Iranian Journal of Public Health, 43(1), 6–15.
- Ludvigsson, J. F., Almqvist, C., Bonamy, A.-K. E., Ljung, R., Michaëlsson, K., Neovius, M., … Ye, W. (2016). Registers of the Swedish total population and their use in medical research. European Journal of Epidemiology, 31(2), 125–136. doi:10.1007/s10654-016-0117-y
- Lunsky, Y., & Balogh, R. (2010). Dual diagnosis: A national study of psychiatric hospitalization patterns of people with developmental disability. The Canadian Journal of Psychiatry, 55(11), 721–728. doi:10.1177/070674371005501106
- Mason, J., & Scior, K. (2004). Diagnostic overshadowing’ amongst clinicians working with people with intellectual disabilities in the UK. Journal of Applied Research in Intellectual Disabilities, 17(2), 85–90. doi:10.1111/j.1360-2322.2004.00184.x
- Mausbach, B. T., & Irwin, S. A. (2017). Depression and healthcare service utilization in patients with cancer. Psycho-Oncology, 26(8), 1133–1139. doi:10.1002/pon.4133
- McBrien, J. A. (2003). Assessment and diagnosis of depression in people with intellectual disability. Journal of Intellectual Disability Research, 47(1), 1–13. doi:10.1046/j.1365-2788.2003.00455.x
- McCarron, M., Cleary, E., & McCallion, P. (2017). Health and health-care utilization of the older population of Ireland: Comparing the intellectual disability population and the general population. Research on Aging, 39(6), 693–718. doi:10.1177/0164027516684172
- McCarron, M., Swinburne, J., Burke, E., McGlinchey, E., Carroll, R., & McCallion, P. (2013). Patterns of multimorbidity in an older population of persons with an intellectual disability: Results from the intellectual disability supplement to the Irish longitudinal study on aging (IDS-TILDA). Research in Developmental Disabilities, 34(1), 521–527. doi:10.1016/j.ridd.2012.07.029
- Moss, S., Bouras, N., & Holt, G. (2001). Mental health services for people with intellectual disability: A conceptual framework. Journal of Intellectual Disability Research, 44(2), 97–107. doi:10.1046/j.1365-2788.2000.00283.x
- Myrbakk, E., & von Tetzchner, S. (2008). Psychiatric disorders and behavior problems in people with intellectual disability. Research in Developmental Disabilities, 29(4), 316–332. doi:10.1016/j.ridd.2007.06.002
- Perkins, E. A., & Moran, J. A. (2010). Aging adults with intellectual disabilities. JAMA, 304(1), 91–92. doi:10.1001/jama.2010.906
- Raymaker, D. M., McDonald, K. E., Ashkenazy, E., Gerrity, M., Baggs, A. M., Kripke, C., … Nicolaidis, C. (2017). Barriers to healthcare: Instrument development and comparison between autistic adults and adults with and without other disabilities. Autism, 21(8), 972–984. doi:10.1177/1362361316661261
- Sandberg, M., Ahlström, G., Axmon, A., & Kristensson, J. (2016). Somatic healthcare utilisation patterns among older people with intellectual disability: an 11-year register study. BMC Health Services Research, 16(1), 642.
- Scheffelaar, A., Hendriks, M., Bos, N., Luijkx, K., & Van Dulmen, S. (2019). Determinants of the quality of care relationships in long-term care - a participatory study. BMC Health Services Research, 19(1). doi:10.1186/s12913-019-4195-x.
- SFS 1993:387. (1993). Act concerning support and service for persons with certain functional impairments (LSS). Stockholm, Sweden: Swedish Parliament.
- SFS 2017:30. (2017). Hälso- och sjukvårdslag [The Health and Medical Service Act]. Stockholm, Sweden: Ministry of Health and Social Affairs.
- SFS 2018:347. (2018). The Swedish social and services act [Swedish: Socialtjänstlag.] Stockholm, Sweden: Ministry of Health and Social Affairs.
- Spassiani, N., Abou Chacra, M. S., & Lunsky, Y. (2017). Why are you here? Can’t you cope at home?” The psychiatric crisis of people with intellectual disabilities and the community’s response. Journal of Mental Health Research in Intellectual Disabilities, 10(2), 74–92. doi:10.1080/19315864.2016.1278290
- Sundquist, J., Ohlsson, H., Sundquist, K., & Kendler, K. S. (2017). Common adult psychiatric disorders in Swedish primary care where most mental health patients are treated. BMC Psychiatry, 17(1), 235. doi:10.1186/s12888-017-1381-4
- The National Board of Health and Welfare. (2019). https://www.socialstyrelsen.se/.
- Tomlinson, S., & Hewitt, O. (2018). Adults with mild intellectual disabilities’ experiences of mental health problems: A qualitative study using interpretative phenomenological analysis. Journal of Mental Health Research in Intellectual Disabilities, 11(1), 16–29. doi:10.1080/19315864.2017.1370045
- Tyler, C., Schramm, S., Karafa, M., Tang, A. S., & Jain, A. (2010). Electronic health record analysis of the primary care of adults with intellectual and other developmental disabilities. Journal of Policy and Practice in Intellectual Disabilities, 7(3), 204–210. doi:10.1111/j.1741-1130.2010.00266.x
- Ullrich, P. M., Smith, B. M., Blow, F. C., Valenstein, M., & Weaver, F. M. (2014). Depression, healthcare utilization, and comorbid psychiatric disorders after spinal cord injury. The Journal of Spinal Cord Medicine, 37(1), 40–45. doi:10.1179/2045772313Y.0000000137
- van den Bogaard, K. J. H. M., Lugtenberg, M., Nijs, S., & Embregts, P. J. C. M. (2019). Attributions of people with intellectual disabilities of their own or other clients’ challenging behavior: A systematic review of qualitative studies. Journal of Mental Health Research in Intellectual Disabilities, 12(3-4), 126–151.
- Williamson, H. J., Contreras, G. M., Rodriguez, E. S., Smith, J. M., & Perkins, E. A. (2017). Health care access for adults with intellectual and developmental disabilities: A scoping review. OTJR (Thorofare NJ), 37(4), 227–236. doi:10.1177/1539449217714148
- Wu, C.-S., Desarkar, P., Palucka, A., Lunsky, Y., & Liu, S.-K. (2013). Acute inpatient treatment, hospitalization course and direct costs in bipolar patients with intellectual disability. Research in Developmental Disabilities, 34(11), 4062–4072. doi:10.1016/j.ridd.2013.08.035
Appendix.
Characteristics of the study groups and healthcare utilisation at the individual level
Appendix. Characteristics of the study groups and healthcare utilisation at the individual level