Abstract
Objectives
We translated and modified an ambiance scale for use by (in)formal caregivers in Dutch nursing homes. We tested validity and reliability of the modified Ambiance Scale.
Method
Convenience sampling was used to enrol (in)formal caregivers in three nursing homes in the Netherlands. 104 questionnaires were filled in; 45 by informal caregivers, 46 by formal caregivers. Ten caregivers filled in the questionnaire twice for test-retest purposes. Three original items were used, and seven newly were added to form the modified Ambiance Scale. Each item consisted of an adjective pair assessing an aspect of ambiance on a scale of 1 (homelike) to 5 (institutional). Caregivers filled in the questionnaire on two different days to assess intra rater reliability. Differences in scoring between formal and informal caregivers and between original and new items were analyzed.
Results
The questionnaire was easy to comprehend and fill in. Internal consistency was good (a = 0.93). Validity was found to be good. Factor analysis demonstrated that eight items identified as one factor. No differences in scoring between the first and second assessment were found (p<.001). Formal caregivers scored ambiance more chaotic than informal caregivers did (p<.01). No differences in scoring between original and new items were found (p =.06).
Conclusion
This study demonstrated that the modified Ambiance Scale had good internal consistency, moderate replicability and both informal and formal caregivers’ overall ratings were comparable. The modified Ambiance Scale is a valid, reliable and easy to use tool to assess ambiance in nursing home settings.
Introduction
The overall effect of physical and social features of a perceived environment on feelings, moods, behaviour, actions, and reactions of individuals, is commonly described with the term ambiance (Brawley, Citation1992). It has been shown that ambiance has a great impact on health and psychosocial well-being (Anderberg & Berglund, Citation2010; Ulrich, Citation1992). It is thus crucial to shape the environment as adequately as possible to people’s needs. In the context of nursing homes, this can be challenging.
The environment and ambiance in nursing homes are mainly controlled and shaped by staff members. As a result, nursing homes are sometimes more suitable as a working space than as a home environment for the residents. Staff is likely to tolerate (unconsciously) more and different sounds (Southwell & Wistow, Citation1995). These imperfect ambiances can adversely influence feelings, behaviour, actions, moods, and quality of life of the residents (Southwell & Wistow, Citation1995; Van Vracem, Spruytte, Declercq, & Van Audenhove, Citation2016). Since residents have cognitive and often physical impairments, they can do little to change or control the environment. Nursing home residents depend on the caregivers to adjust the environment according to their needs to make them feel safe and at home (Brawley, Citation1992).
In recent decades, long-term care has become more and more person-centered and aimed at the well-being of the individual. This approach led to recognition of the importance of the design of the physical environment for nursing home residents (Day, Carreon, & Stump, Citation2000). Nursing homes need to be built more homelike and be adapted to the patients’ needs and preferences (Devlin & Arneill, Citation2003). In that context, an ambiance scale to measure ambiance in long-term care was first developed by Pastalan (Struble, Citation1995). This original version consisted of ten adjective pairs that described home-like features of the nursing home environment for example peaceful – chaotic. In a subsequent study by Algase et al. (Citation2007), the scale was modified to capture the effect or impact of the immediate environment or surrounds as a gestalt, and not to characterize the extent to which it corresponded with a particular ideal or preferred environment. This version of the ambiance scale consisted of nine adjective pairs. The scale was scored with a semantic differential scaling model (+2 to −2), where +2 represented a homelike environment and −2 represented an institutional environment (Algase et al., Citation2007).
However, two aspects are missing in the two versions of the ambiance scale. The first aspect relates to the type of observer filling in the scale. The two scales were intended for use by research staff. This does not recognize that nursing home residents are usually best represented by persons who know them well (Anderberg & Berglund, Citation2010; Ulrich, 1992). Family members and other informal caregivers who know the resident longest provide a focal representation of the patients’ wishes. In addition, nurses and nursing assistants are the ones who spend most time with the residents and monitor their behavior all day (Lyons & Zarit, Citation1999). Therefore, both informal and formal caregivers are predesignated persons to evaluate the ambiance of a nursing home.
The second aspect that is missing in the available versions of the ambiance scale relates to the fact that they were developed for rating the immediate (visually accessible) environment. Ambiance is however the overall effect of the entire perceived environment and not only the visually accessible environment. The perceived audible part of an environment, also called soundscape, has been recognised as a highly important factor in a person’s core affect, the feeling of safety, and motivation of behaviour (Van den Bosch, Welch, & Andringa, Citation2018; Russel, Citation2003). Appraisal of soundscapes is described with two main dimensions: pleasant – unpleasant and eventful – uneventful (Axelsson, Nilsson, & Berglund, Citation2010). These dimensions are closely related to those of core affect, which are basic affective feelings that are always present (Van den Bosch et al., Citation2018). Therefore, ambiance also includes soundscape (Andringa & Van Den Bosch, Citation2013; Brawley, Citation1992).
Study aims
Given the importance of ambiance for the well-being of residents in nursing homes and to our knowledge – the lack of a Dutch ambiance scale, the main aim of the present study was to translate the original ambiance scale for use in Dutch nursing homes, and modify it to account for the aspects that had been missed. Furthermore, we tested the following psychometric properties of the modified Ambiance Scale (m-AS):
its validity, including construct, face validity and the factor structure; and
its reliability, including internal consistency, test-retest reliability and interrater reliability.
Method
Design
We used a cross-sectional correlation study design to evaluate the m-AS.
Questionnaire construction
The m-AS contains 10 adjective pairs. The pairs and origin of these pairs are shown in . Five items were taken from the modified version of the original ambiance scale (Algase et al., Citation2007). We slightly modified two of these items to account for language differences (see ). To acknowledge the influence of soundscape on ambiance and to acknowledge the importance of feeling safe in homelike environments, five item-pairs were added to form the m-AS. These pairs are in line with the proposed soundscape approach by Van den Bosch et al. (Citation2018) and Axelsson et al. (Citation2010). The items were translated following the golden standard of questionnaires: it was first translated to Dutch and then back again to English.
Table 1. Items of the m-AS and origin of the items.
The pairs on the m-AS are scored with a 5-point Likert scale from 1 (homelike) to 5 (institutional). The words on the left (e.g. informal, lively, pleasant) belong to the homelike category and the words on the right (e.g. formal, lifeless, unpleasant) belong to the category institutional. The format is the same as the one used by Algase et al. (Citation2007).
Participants and setting
Convenience sampling was used to include participants in three nursing homes situated in the Eastern part of the Netherlands. These nursing homes offered care to elderly patients with and without dementia. The first nursing home dates back from 2007, had 106 patients, and had 200 formal caregivers. The second nursing home consisted of 3 locations. The first location was built in 1954 (renovated in 2009). The second location was built in 1980 (renovated in 2010). Both locations housed 110 residents and had around 400 formal caregivers. The third location of this nursing home was built in 2015, housed 72 patients, and had 120 formal. The third nursing home was built in the mid ‘90 s and housed 150 patients. Number of caregivers however is unknown for this nursing home.
To account for the focal representation of nursing home patients by formal and informal caregivers, we included both groups as observers. We investigated whether these groups scored ambiance similarly. Informal and formal caregivers that visited or worked in the nursing home during data collection days were asked to fill in the scale. They gave informed consent before participation. Informal caregivers were also asked to provide the following demographic data: age, gender, and relation to the patient. Formal caregivers were asked to fill in their age, and gender. Overall, there were 104 sampled ratings. The ratings were collected at the three nursing homes (n is 8, 45, and 57 respectively).
Next to the m-AS, four statements evaluating face validity were presented to the caregivers. The four statements evaluating face validity were (1) The questionnaire was clear, (2) The questions capture all aspects of ambiance, (3) I can describe ambiance in the nursing home unit well with these questions, and (4) It took me a lot of effort to answer the items. Participants were asked to rate the statements using a 5-point Likert scale (1 completely disagree to 5 completely agree).
Procedure
The informal and formal caregivers were approached in the nursing homes in March 2018. Informal caregivers were asked to participate when they visited the patient, and formal caregivers were approached during working hours. Caregivers were informed that participation was entirely voluntary, they had the right to withdraw from the study at any time, and that data was anonymized. The research team explained the aim of the study and distributed the questionnaires. Caregivers were instructed to rate the ambiance at the given moment. After completion of the first questionnaire, a random sample of formal and informal caregivers was approached for an appointment for a second completion of the questionnaire a week later to check test-retest (intra-rater) reliability. Nine-teen formal and informal caregivers completed the questionnaire twice. Ethical approval of the local committee was received.
Analysis
Descriptive statistics for the sample and each item of the m-AS were calculated. A confidence interval of 95% was used. Distribution of scores was checked to verify that caregivers used the full range of possible scores and data was not skewed (asymmetrical around the mean).
To estimate the validity of the questionnaire, we tested face validity, construct validity and the factor structure. To check face validity, we calculated the mean and standard deviation of the four statements about face validity. To determine the construct validity of the m-AS, a preliminary analysis was performed to ascertain that the data was suitable for factor analysis. The average of the communalities should be around .60 or higher (MacCallum, Widaman, Zhang, & Hong, Citation1999) and the ratio of participants to items should be at least 10:1 (Nunnally, Citation1978). Kaiser-Meyer-Olkin measures were calculated and should all be the acceptable level of .5 (Kaiser & Rice, Citation1974). Barlett’s test of sphericity was used to check the correlations between items. If the data was found to be suitable for factor analysis, an exploratory factor analysis (EFA), using a principal component analysis with varimax rotation, was used. Our expectation was that all items would score on one factor representing the concept “ambiance.” A model was considered adequate whenever it met the criteria of a statistical item fit (r ≥ .40, and for each item a contrast with other factor loadings of ≥ .20) and if all items fitted the factor that they were assigned to on conceptual grounds.
Reliability was estimated by investigating overall reliability and test-retest reliability. The overall reliability was investigated by determining the internal consistency (Cronbach’s alpha) of the final scale. A Cronbach’s alpha between .70 and .90 was considered adequate (Terwee et al., Citation2007).
Internal consistency was checked by evaluating item-total correlations and analyzing the contribution of the items to the total score. Correlations between items were analyzed using Pearson’s correlation coefficient. Magnitude of the correlation was defined as small (r = 0.2 to 0.5), moderate (r = .50 to .80) or strong (r > .80) (Cohen, Citation1988). An item with a Pearson’s correlation coefficient of less than .20 was considered to contribute too little. If the Pearson’s correlation between two items was .80 or higher, it was assumed that one of them could be removed.
To see whether ambiance ratings differ between first and second time of filling in the questionnaire, intraclass correlation coefficients (ICC) was used for the 10 caregivers who completed the second questionnaire twice within one week. ICC estimates and their 95% confident intervals were calculated based on a mean-rating (k = 2), absolute-agreement, 2-way mixed-effects model. Values less than .5, between .5 and .75, between .75 and .9, and greater than .90 were considered indicative of poor, moderate, good, and excellent reliability, respectively (Koo & Li, Citation2016).
Alterations to the scale were checked by comparing scores of the original and newly developed items, informal and formal caregivers and evaluating the added soundscape approach to the ambiance scale.
To examine the scores of the original and newly developed items, scores of the original items and newly developed items were compared using a paired samples t-test. A CI of 95% was used. This was done to check the internal consistency of the scale.
To see whether ambiance ratings differ between informal and formal caregivers, an independent samples t-test was calculated. In addition, informal and formal caregivers´ scores were also compared at individual item level with a multivariate analysis of variance (MANOVA). Dependent variables are the ambiance items that were still included after factor analysis.
The addition of the soundscape approach to ambiance was summarized by the factor analysis and pearson correlates for single items.
Statistical data analyses were performed using SPSS 23 (IBM Corp, Citation2015).
Results
Sample and ambiance scores
In total 104 sampled ratings were received, of which 91 different caregivers filled in the m-AS. 10 caregivers filled in the m-AS twice, and 3 questionnaires could not be included in analysis because of missing data. Formal and informal caregivers were equally represented (n = 45, respectively n = 46) (see ). Females (60% of informal caregivers, 93% of formal caregivers) filled in the majority of the ratings. Mean age of informal caregivers was 59.8 years (SD = 13.5), which is higher than the mean age of formal caregivers which was 39.0 years (SD = 14.4).
Table 2. Participant characteristics.
The mean and standard deviation of each item is presented in . The data was visually checked on skewness. Item number 5 (stimulating – demotivating) was skewed to the left. The remaining data showed a normal distribution.
Table 3. Descriptive statistics per item and summary of exploratory factor analysis results.
Validity
Face validity questions were answered by caregivers on a scale of 1, completely disagree, to 5, completely agree. The caregivers indicated that the scale is clear (item 1: M = 3.74, SD = 1) and captures all aspects of ambiance (item 2: M = 3.73, SD = 0.8). They agreed that the m-AS describes ambiance well (item 3: M = 3.65, SD = 0.87), and are neutral with regard to the effort it takes to answer the items of the scale (item 4: M = 2.31, SD = 1.01).
Construct validity was assessed using a principal component analysis (PCA) for the 10 items with varimax rotation. The Kaiser-Meyer-Olkin measure confirmed the sampling adequacy for the analysis (KMO = 0.9). All KMO values for individual measures were > 0.8, which is well above the acceptable level of .5 (Kaiser & Rice, Citation1974). Barlett’s test of sphericity indicated that correlations between items were sufficiently large for PCA (χ2 (45) = 621.14, p = .000).
Next, an exploratory analysis was run to obtain eigenvalues for each component in the data. Two components had eigenvalues over Kaiser’s criterion of 1 and in combination explained 70.64% of the variance. The scree plot showed an inflexion which would justify retaining only component 1. Based on the Kaiser’s criterion and the scree plot, only the first component was retained in the final analysis. shows the factor loadings after rotation. Item 2 and item 5 were eventually excluded from the factor structure because both items were considered conceptually deviant from the main contents of the factor that they were assigned to. The items suggested that component 1 represented the concept ambiance.
Reliability
The internal consistency of the m-AS with all items had a Cronbach’s alpha of 0.92. Taking into account the results of the factor analysis, Cronbach’s alpha of the scale without item 2 and 5 was 0.93. In addition, the corrected item-total correlations were all above the threshold of 0.4 (Cohen, Citation1988).
Most items correlated well with each other (see ). Only the correlations between item 1 and 2, 2 and 4, 1 and 5 and 4 and 5 were lower than the acceptable level of 0.4 (Cohen, Citation1988).
Table 4. Pearson correlations for each item.
Test-retest reliability showed satisfactory reliability estimates, as evidenced by inter-item correlations ranging between .399 and .777. A moderate degree of reliability was found between the first and second ratings with the m-AS. The average Intraclass correlation was 0.67 with a 95% CI from 0.324 to 0.859 (F(18,18) = 5.09, p<.001).
Alterations to the scale
Differences in scoring between the already existing items and the newly added items were checked with a paired samples t-test. There was no significant difference between the scores of the original items (M = 2.00, SD = 0.79) and the new items (M = 2.08, SD = 0.76); t(109) = −1.9, p = 0.06. Which indicates a good internal consistency.
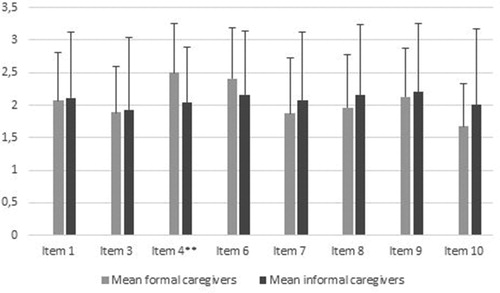
To see whether ambiance ratings differ between informal and formal caregivers, an independent samples t-test was performed. No significant difference between the SUM scores of the informal (M = 2.13, SD = 0.92) and formal caregivers (M = 2.00, SD = 0.56) was found; t(108)= −0.86, p = 0.41. However, on a single item level the MANOVA showed, that there was a significant difference between informal and formal caregivers, Λ = .79, F(8,82) = 2,699, p < .011. The univariate results showed that this was due to a significant group difference for item 4 (calm – chaotic), with F (7,318) = 4.721, p = .008, and ηp 2 = .076 (the other items did not differ significantly between the two observer groups). As can be seen in , formal caregivers scored the ambiance in the nursing homes as more chaotic than informal caregivers did.
Figure 1. Mean scores and standard deviations of scores per ambiance item for informal and formal caregivers.
** Significance level of the MANOVA p ≤ 0.01, ηp2 = .076. Effect size is only indicated for item 4, which showed the only significant difference in scores of formal and informal caregivers.
Three items acknowledging the soundscape approach were added to the m-AS, which were item 2, item 3 and item 6. Factor analysis showed that item 2 revealed the highest loading on another component. Therefore, item 2 was deleted from the questionnaire. Factor analysis showed that item 3 and 6 loaded on the factor ambiance and these items correlated sufficiently with the other remaining items (). Pearson correlations also showed that item 3 and 6 correlated well with the other ambiance items ().
Discussion
The ambiance scale developed by Algase et al. (Citation2007) was used as the basis for the modified Ambiance Scale (m-AS). The scale was translated into Dutch, and now accommodates items which includes the soundscape approach. The scale was adapted for use by both informal and formal caregivers. This study demonstrated that the m-AS had good internal consistency and a moderate replicability. In addition, both informal and formal caregivers were able to fill in the questionnaire and their overall ratings were mostly comparable. Further analysis showed that the soundscape approach complements the concept of ambiance.
Validity
With regard to the construct validity of the m-AS, this study demonstrated a good face validity as rated by the participants. The scale was rated as being clear, capturing all aspects of ambiance, and providing a good description of ambiance. Caregivers were neutral with regard to the required effort to fill in the m-AS. This indicates that the m-AS was easy to comprehend.
Factor analysis demonstrated eight of ten items of the m-AS identified as one factor (total variance of 60.3%). Algase et al. (Citation2007) tested the ambiance scale and found two factors to account for over 68% of the total variance in nursing homes and over 71% of the total variance in assisted living facilities. However, one factor explained more than 40% of the variance in both samples. Therefore, the author suggested that the concept of ambiance might have only one dimension. Although we combined formal and informal caregivers in the analysis, the current study further supports this initial assumption, because the concept of ambiance is captured as one entity with the m-AS. However, item 5, which originated from the study of Algase et al. (Citation2007) and loaded on the biggest engaging concept, identified with the deleted second factor in our study.
Reliability
The m-AS and subscales demonstrated acceptable internal consistency, which is in line with previous findings by Algase et al. (Citation2007). Comparable high Cronbach’s alphas were found in the study of Algase et al. (Citation2007) and our study. In addition, we noted that most items correlated well with each other with item-total correlations all above the threshold of 0.4 (Cohen, Citation1988). This means that the items are all assessing the same concept, namely ambiance. In addition, moderate correlations (0.408–0.768) indicated sufficient unique variance of the items and lack of isomorphism (Tavakol & Dennick, Citation2011).
Additionally, a moderate degree of reliability was found between the first and second ratings for the m-AS although the CI was rather wide. The width of the CI could be attributed to the mood of the person filling in the m-AS being easily affected by the physical and social features of an environment (Andringa, Citation2013; Russel, Citation2003). Moreover, these features of the environment can be interpreted differently at various times (Russel, Citation2003). The environment in a nursing home is also easily affected by the ongoing activities and number of people present inside, as well as for example the sounds of howling wind or pouring rain outside.
Alterations to the scale
Ratings of the original and newly added items of the m-AS were similar and no significant differences were found in scoring. Scores on all items were, thus, not influenced by the nature of the items, and differences in scored ambiance can therefore be attributed to differences in ambiance in nursing homes. This indicates a good internal consistency.
Ambiance was rated very similar by informal and formal caregivers too. Therefore, both formal and informal caregivers can fill in the scale. However, when looking at single item comparisons we found one significant group difference for item 4 (calm – chaotic). Interestingly, formal caregivers perceived the ambiance in the nursing homes as more chaotic than the informal caregivers. This could be due to perceived work-related pressure. Formal caregivers see the environment as their workplace (Southwell & Wistow, Citation1995) and pressure, created by for example the chaotic work environment, has an influence on mood (Russel, Citation2003). This in turn, influences the appraised ambiance (Andringa, Citation2013). A chaotic environment might affect informal caregivers less, since they are not at work and just visiting family.
Three items measuring soundscape appraisal were added to the original ambiance scale. With the exception of item 2 (lively – lifeless), 3 (pleasant – unpleasant) and 6 (harmonious – tense), which loaded on the first eigenvalue ambiance. According to the Pearson correlations, these two items fitted with the concept ambiance. This means that soundscape is part of ambiance in a nursing home setting.
Strengths and limitations
This study contributes to the literature by confirming the psychometric properties of a useful measurement tool of caregivers’ perceptions of the ambiance in long-term care. A strength of the m-AS is that both formal and informal caregivers can fill in the questionnaire similarly. The psychometric properties concerning validity and reliability were satisfactory across multiple nursing homes. Another strength is that the m-AS captures ambiance as one entity in a nursing home. The specific items can be used to make more detailed adaptations to the environment to enhance ambiance. For example, if overall ambiance is rated as good, but the environment is rated as more chaotic than calm, this indicates that the environment can still be improved by making the ambiance calmer. In the context of person-centered care and recognition of the importance of the physical environment of nursing homes (Day et al., Citation2000), the m-AS will become more important when measuring the properties of the environment. Because the m-AS can be used to measure ambiance as an entity but also on specific items, it gives the opportunity to gather insights about the ambiance in a flexible way. The insights gathered make it easier to make adaptations to the environment to optimize the environment for the patients.
Several limitations of this study need to be acknowledged when interpreting and using the study results. First, although the caregiver recruitment took place in different nursing homes, all nursing homes were located in the eastern part of the Netherlands. The lack of diversity in terms of geography could cause a lack in cultural diversity. Therefore, this study does not guarantee representativeness of formal and informal caregivers of different cultural backgrounds.
In addition, we could not examine whether the factor structure is invariant across different nursing homes due to the small number of participating nursing homes. It is unclear whether the m-AS assesses the same construct in each nursing home. Therefore, variance across nursing homes in means and correlations involving that construct cannot be interpreted.
Further, the focus of our study was on psychogeriatric wards. Residents of these wards can only verbally express themselves to a limited degree. In the future, we think that it would be useful to test if the instrument can be filled in by nursing home residents with sufficient cognitive abilities. They are in the end the main users of the facilities. This in turn can be used to assess differences in perception between caregivers and residents.
Conclusion
We have developed a valid and reliable ambiance scale that is easy to use for both formal and informal caregivers in nursing homes and captures the entire perceived environment. From the clinical perspective, simple and straightforward items in the m-AS are easy and quick to administer to informal and formal caregivers in nursing homes. Staff could use the m-AS to describe the extent to which the ambiance of their unit is experienced as homelike, and evaluate if an intervention has effects on the ambiance. The m-AS could be used to develop and examine interventions that are aimed at enhancing ambiance in long-term care settings, and in turn the residents’ quality of life.
Disclosure statement
The authors report no conflict of interest
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, J. Kosters. The data are not publicly available due to that they contain information that could compromise the privacy of research participants.
Additional information
Funding
References
- Algase, D. L., Yao, L., Son, G. R., Beattie, E. R. A., Beck, C., & Whall, A. F. (2007). Initial psychometrics of the ambiance scale: A tool to study person-environment interaction in dementia. Aging and Mental Health, 11(3), 266–272. doi:10.1080/13607860600963604
- Anderberg, P., & Berglund, A.-L. (2010). Elderly persons’ experiences of striving to receive care on their own terms in nursing homes. International Journal of Nursing Practice, 16(1), 64–68. doi:10.1111/j.1440-172X.2009.01808.x
- Andringa, T. C. (2013). Soundscape and its relation to core affect, appraisal, and motivation. Paper presented a the Proceedings of the AIA-DAGA, Merano, pp. 1511–1513.
- Andringa, T. C., & Van Den Bosch, K. A. (2013). Core affect and soundscape assessment: Fore- and background design for quality of life. Paper presented at the Proceedings of the Internoise 2013, Innsbruck, pp. 1–10.
- Axelsson, Ö., Nilsson, M. E., & Berglund, B. (2010). A principal components model of soundscape perception. The Journal of the Acoustical Society of America, 128(5), 2836–2846. doi:10.1121/1.3493436
- Brawley, E. (1992). Alzheimer’s disease: Designing the physical environment. American Journal of Alzheimer's Care and Related Disorders & Research, 7(1), 3–8. doi:10.1177/153331759200700103
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). London: Taylor & Francis.
- Day, K., Carreon, D., & Stump, C. (2000). The therapeutic design of environments for people with dementia: A review of the empirical research. Gerontologist, 40, 397–416. doi:10.1093/geront/40.4.397
- Devlin, A. S., & Arneill, A. B. (2003). Health Care Environments and patient outcomes. A review of the literature. Environment and Behavior, 35(5), 665–694. doi:10.1177/0013916503255102
- IBM Corp. (2015). IBM SPSS statistics for windows, Version 23.0. Armonk, NY: IBM Corp.
- Kaiser, H. F., & Rice, J. (1974). Little jiffy. Educational and Psychological Measurement, 34(1), 111–117. doi:10.1177/001316447403400115
- Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. doi:10.1016/j.jcm.2016.02.012
- Lyons, K. A., & Zarit, S. H. (1999). Formal and informal support: The great divide. International Journal of Geriatric Psychiatry, 14, 183–196. doi:10.1002/(SICI)1099-1166(199903)14:3<183::AID-GPS969>3.0.CO;2-J
- MacCallum, R. C., Widaman, K. F., Zhang, S., & Hong, S. (1999). Sample size in factor analysis. Psychological Methods, 4(1), 84–99. doi:10.1037/1082-989X.4.1.84
- Nunnally, J. C. (1978). Psychometric theory (2nd ed.). New York: McGraw-Hill.
- Russel, J. A. (2003). Core affect and the psychological construction of emotion. Psychological Review, 110, 145–172.
- Southwell, M. T., & Wistow, G. (1995). Sleep in hospitals at night: Are patients’ needs being met? Journal of Advanced Nursing, 21(6), 1101–1109. doi:10.1046/j.1365-2648.1995.21061101.x
- Struble, L. M. (1995). Ambulation behaviors of people with Alzheimer’s disease: Case studies of residents on the facilities along the homelike continuum (Doctoral dissertation). University of Michigan, Ann Arbor, UM. Dissertation Abstract International, AAT 9542963.
- Tavakol, M., & Dennick, R. (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education, 2, 53–55. doi:10.5116/ijme.4dfb.8dfd
- Terwee, C. B., Bot, S. D. M., de Boer, M. R., van der Windt, D. A. W. M., Knol, D. L., & Dekker, J. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60, 34–42. doi:10.1016/j.jclinepi.2006.03.012
- Ulrich, R. S. (1992). How design impacts wellness. Healthcare Forum Journal, 35, 20–25.
- Van den Bosch, V. A. K., Welch, D., & Andringa, T. C. (2018). The evolution of soundscape appraisal through enactive cognition. Frontiers in Psychology, 9, 1129. doi:10.3389/fpsyg.2018.01129
- Van Vracem, M., Spruytte, N., Declercq, A., & Van Audenhove, C. (2016). Nachtelijke onrust bij personen met dementie in woonzorgcentra: Een verkennende veldstudie. Tijdschrift Voor Gerontologie En Geriatrie, 47(2), 78–85. doi:10.1007/s12439-016-0167-3
Appendix A
Modified ambiance scale in Dutch
Op deze lijst kunt u de sfeer van de omgeving beoordelen. Het gaat om uw eigen gevoel, oftewel het gevoel dat de omgeving bij u oproept.
De tien sfeer tegenstellingen in de lijst kunt u beoordelen op een schaal van 1 tot een met 5. 1 is erg huiselijk en komt overeen met het linker woord. 5 is erg institutioneel en komt overeen met het rechter woord.
Graag bij iedere stelling één cijfer omcirkelen.
