Abstract
Objectives
We investigated the 2-week prevalence and correlates of very frequent physical aggression (PA) and vocalizations in nursing home (NH)-residents with dementia.
Method/Design
This cross-sectional study used combined data of 2074 NH-residents from four studies, collected from 119 dementia special care units in 26 Dutch NH. Very frequent PA was defined as scoring 6 or 7 on the items ‘hitting’, pushing’, ‘biting’ and ‘kicking’ of the Cohen Mansfield Agitation Inventory; very frequent vocalizations as scoring 6 or 7 on ‘screaming’ and ‘making strange noises’. We compared NH-residents with very frequent PA or vocalizations with residents with less frequent PA or vocalizations, assessing correlates using univariate and multivariate multilevel logistic regression analyses.
Results
We found a 2-week prevalence of 2.2% (95% confidence interval (CI): 1.63–2.89) of very frequent PA and 11.5% of very frequent vocalizations (95% CI: 10.23–12.98). Very frequent PA was only associated with apathy (odds ratio (OR)=1.93, 95% CI: 1.04–3.61). Correlates of very frequent vocalizations were age (OR = 0.97, 95% CI: 0.951–0.998), dementia severity (overall p-value 0.020), antipsychotic drug use (OR = 1.56, 95% CI: 1.08–2.26), antiepileptic drug use (OR = 2.75, 95% CI: 1.34–5.68) and euphoria (OR = 2.01, 95% CI: 1.22–3.31).
Conclusion
Characteristics of NH-residents with very frequent PA or very frequent vocalizations differ from those of NH-residents with less frequent PA or vocalizations. Frontal lobe damage, boredom, pain and/or external factors may explain several of the found associations, but further research is necessary. Our findings may contribute to better care for these residents and thereby to improving their quality of life.
Introduction
Physical aggression (PA) and vocalizations are behaviors of nursing home (NH)-residents with dementia that are experienced as challenging and complex. They cause distress and burden in the NH-resident self, other residents and (informal) caregivers (Bourbonnais & Ducharme, Citation2010; Cohen-Mansfield & Werner, Citation1997; Holst & Skar, Citation2017; Voyer et al., Citation2005; Zwijsen, Kabboord, et al., Citation2014). PA (e.g. hitting, pushing, scratching) (Voyer et al., Citation2005) can be directed towards nursing staff (Bridges-Parlet, Knopman, & Thompson, Citation1994) or other NH-residents (Bridges-Parlet et al., Citation1994; Ferrah et al., Citation2015). Previous cross-sectional studies have suggested that causes of (physical) aggression or vocalizations (e.g. screaming, excessively loud and/or repetitive verbal utterances) (Cohen-Mansfield & Werner, Citation1997; Yusupov & Galvin, Citation2014) could be internal (i.e. physical, cognitive/neurobiological or psychological) (Algase et al., Citation1996; Beck et al., Citation2011; Bourbonnais & Ducharme, Citation2010; Gotovac, Nikolac Perkovic, Pivac, & Borovecki, Citation2016; Nagaratnam, Patel, & Whelan, Citation2003) ; or external (i.e. environmental) (Bourbonnais & Ducharme, Citation2008; Bridges-Parlet et al., Citation1994; Stutte, Hahn, Fierz, & Zuniga, Citation2017). However, these studies were mostly small and did not focus on very frequent PA or vocalizations. The multifactorial etiology and complexity mean that treatment and care for NH-residents with PA or vocalizations are challenging. These behaviors may result in the prescription of psychotropic drugs (Cariaga, Burgio, Flynn, & Martin, Citation1991; Isaksson, Graneheim, Astrom, & Karlsson, Citation2011) and PA has been shown to lead to the use of physical restraints (Isaksson et al., Citation2011). Prevalence rates of 6–21% (PA) (Isaksson et al., Citation2011) and 11–30% (vocalizations) (Beck et al., Citation2011) have been reported in nursing homes. Several correlates have been described for PA and vocalizations, such as higher age (Beck et al., Citation2011; Voyer et al., Citation2005), more dementia severity (Liljegren, Landqvist Waldo, & Englund, Citation2018; Voyer et al., Citation2005), psychotropic drug use (PDU) (Isaksson et al., Citation2011; Voyer et al., Citation2005), and positive associations with other neuropsychiatric symptoms, e.g. depression and psychotic disorders (Bourbonnais & Ducharme, Citation2008; Leonard, Tinetti, Allore, & Drickamer, Citation2006), whereas conflicting results have been found for sex (Beck et al., Citation2011; Isaksson et al., Citation2011; Voyer et al., Citation2005).
PA and vocalizations in NH-residents can be extremely severe and very frequent. Although suggested prevalence rates of NH-residents with very frequent PA or very frequent vocalizations are low (Brodaty, Draper, & Low, Citation2003; Voyer et al., Citation2005), anecdotal information from daily practice shows that these extreme behaviors cause suffering in the pertaining residents, have a great impact on people involved including co-residents, and lead to difficulties in managing the behaviors among NH-staff. Resident-to-resident aggression is considered a widespread but disregarded phenomenon (Goergen et al., Citation2020) and can result in serious injuries and even death in co-residents (Caspi, Citation2016; Ferrah et al., Citation2015). Furthermore, NH-staff can get injured and experience mental distress as a consequence of very frequent PA or very frequent vocalizations (Hazelhof, Schoonhoven, van Gaal, Koopmans, & Gerritsen, Citation2016; Zeller et al., Citation2009).
Acquiring insight into the prevalence and characteristics of residents with these extreme behaviors is highly relevant; on the one hand to obtain points for improvement in the care and quality of life for these residents, on the other hand to diminish the impact of these behaviors on the people involved. We reported data about NH-residents with dementia and very frequent agitation in a previous paper describing the WAALBED (WAAL Behavior in Dementia)-III study (Veldwijk-Rouwenhorst et al., Citation2017). Agitation, however, encompasses several types of behavior which may differ in prevalence and relevant associated characteristics. Therefore, in this paper, we focus on two specific behaviors often considered to be part of agitation (Cummings et al., Citation2015) and regarded as especially challenging (Bourbonnais & Ducharme, Citation2010; Holst & Skar, Citation2017; Zwijsen, Kabboord, et al., Citation2014).
The primary aim of this article was to explore the 2-week prevalence of NH-residents with very frequent PA or very frequent vocalizations in a sample of NH-residents. Furthermore, this article is a first attempt to investigate whether NH-residents with very frequent PA or very frequent vocalizations are different from those with less frequent presentations of these behaviors by exploring if there are distinctive correlates for these very frequent behaviors. This would provide NH-staff insight into which NH-residents will be at risk of very frequent PA or vocalizations. We hypothesize that these groups have distinct characteristics compared to NH-residents with less frequent PA and less frequent vocalizations.
Methods
Study design and subjects
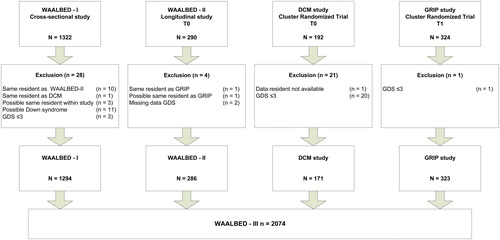
As previously described (Veldwijk-Rouwenhorst et al., Citation2017) we combined data from four studies in NH-residents with dementia: WAALBED-I study (cross-sectional study, n = 1319, 2003) (Zuidema, Derksen, Verhey, & Koopmans, Citation2007), WAALBED-II study (longitudinal study; n = 290, 2006–2008) (Wetzels, Zuidema, de Jonghe, Verhey, & Koopmans, Citation2010), Dementia Care Mapping (DCM) study (randomized controlled trial, cluster randomized; n = 434, 2010–2012) (van de Ven et al., Citation2013) and GRIP on challenging behavior study (randomized controlled trial, stepped wedge design; n = 659, 2011–2012) (Zwijsen, Smalbrugge, et al., Citation2014). All studies were conducted according to the principles of the Declaration of Helsinki (version 2013, www.wma.net). The regional Medical Ethics Committees for Arnhem/Nijmegen and Amsterdam reviewed the study protocols. Informed consent was obtained from the primary legal representative or legal guardian in all studies.
We considered residents for inclusion if they: (a) met the criteria for dementia according to the Diagnostic and Statistical Manual of Mental Disorder, Fourth edition (American Psychiatric Association, Citation1994, Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Arlington, VA: American Psychiatric Publishing, (b) had no life-threatening disease at the time of inclusion; and (c) had resided in the NH for at least 4 weeks. The sole/baseline measurement was used from the first three studies. We only included data from residents in the control condition at the second measurement from the GRIP study. In another part of our study we aim to examine data on quality of life of NH-residents with dementia and very frequent behavior. Because data on quality of life were not collected at baseline in the GRIP study, we used the second measurement of that study (Zwijsen, Smalbrugge, et al., Citation2014). Where residents had participated in more than one of the four studies we only included data from the most recent study. Residents with a Global Deterioration Scale (GDS) (Reisberg, Ferris, de Leon, & Crook, Citation1988) score of 3 or lower, or a missing GDS score, were excluded as well as residents who had Down syndrome. In addition, we excluded one resident because the majority of data was missing. These criteria resulted in the exclusion of 54 residents from the original merged data set, leaving a data set of 2074 residents (see ) from 119 different dementia special care units in 26 NH situated throughout the Netherlands. Because of this large sample, it was possible to perform logistic regression analyses applying multiple possible confounders.
Data
Operationalization of very frequent physical aggression and very frequent vocalizations
We assessed PA and vocalizations with the Dutch version of the Cohen Mansfield Agitation Inventory (CMAI) (de Jonghe & Kat, Citation1996). The CMAI is the most widely used instrument for measuring the frequency of agitation and aggression in nursing home residents (Cohen-Mansfield, Marx, & Rosenthal, Citation1989). It consists of 29 items, each rated on a 7-point frequency scale (1–7) ranging from ‘never’ to ‘several times an hour’ and can be summed into a total score with a possible range from 29 to 203 (Cohen-Mansfield et al., Citation1989). In all four studies, the care staff members most involved in the daily care of the resident completed the CMAI. In three studies this were licensed vocational nurses who had been specifically assigned to individual residents and thus knew them well (Wetzels et al., Citation2010; Zuidema et al., Citation2007; Zwijsen, Smalbrugge, et al., Citation2014). In the DCM study these data were not available (van de Ven et al., Citation2013). In that study the CMAI was administered using a web-based application. In all four studies, the 2-week period before the assessment date was used as reference period for their observations.
Very frequent PA was defined as having a score of 6 (several times a day) or 7 (several times an hour) on the items ‘hitting’, ‘pushing’, ‘biting’ and ‘kicking’ of the CMAI. In order to interpret correlates, we decided to only include items which in terms of content could be unambiguously labeled as PA and directed towards other people. Therefore, the items ‘spitting’, ‘hurting self or others’, ‘tearing things or destroying property’ and ‘scratching’ were not included. Very frequent vocalizations were defined as having a score of 6 or 7 on the items ‘screaming’ and ‘making strange noises’ of the CMAI. Like with PA, we decided to only include items which in terms of content could be clearly labeled as vocalizations. The choice of selecting items for the definition of very frequent vocalizations was based on the first type of vocalizations described in in the article of von Gunten, Alnawaqil, Abderhalden, Needham, & Schupbach (Citation2008), but without the prerequisite that the vocalizations caused disruption as this is very difficult to operationalize. Additionally, we did not include the item ‘cursing or verbal aggression’ of the CMAI because this item may regard aggression more than vocalizations. If it was not possible to determine to which group a NH-resident belonged due to missing relevant CMAI items, we excluded that resident from the analyses.
Table 1. Demographic data of NH-residents with dementia with very frequent physical aggression (PA) and less frequent PA (Total N = 2072) as well as NH-residents with dementia with very frequent vocalizations and less frequent vocalizations (Total N = 2073).
Other measurements
We included the demographic characteristics: age, sex, marital status and duration of institutionalization. Dementia severity was assessed with the GDS, which ranges from normal cognition (GDS stage 1) to very severe cognitive decline (GDS stage 7) (Reisberg et al., Citation1988).
Neuropsychiatric symptoms were assessed with the Dutch version of the Neuropsychiatric Inventory- Nursing Home version (NPI-NH) (Cummings et al., Citation1994; Kat et al., Citation2002) . With this assessment-instrument, frequency (F) and severity (S) of each symptom are rated on a four-point (1–4) and three-point (1–3) Likert scale, respectively. A separate score (FxS score) can be calculated by multiplying the frequency and severity scores. This results in values ranging from 0 to 12 for each symptom. The NPI-NH was administered in the same way as the CMAI. In the analyses, we used clinically relevant neuropsychiatric symptoms, commonly defined as an FxS score of ≥ 4 (Wood et al., Citation2000). We excluded NPI-items that were conceptually similar to PA or vocalizations. For PA this applied to the items aggression/agitation, irritability and disinhibition, and concerning vocalizations to the item aggression/agitation.
PDU was classified and grouped into several PD-groups (antipsychotics, antidepressants, hypnotics, anxiolytic drugs, antiepileptics and cholinesterase inhibitors) by using the Anatomical Therapeutical Chemical-classification (Guidelines for ATC Classification, Citation1990). We used dichotomous categories of either ‘’present’’ or ‘’absent’’ per drug group in the analyses to quantify PDU and discarded drugs which were taken as needed.
Data analysis
SPSS 22.0 (IBM, Armonk, NY) was used for the analyses. We calculated the 2-week prevalence of very frequent PA and very frequent vocalizations including a 95% (Wilson) confidence interval.
Since we were interested in correlates that can help to identify NH-residents with a risk of very frequent behavior, only those with very frequent (scoring 6 or 7 on the selected CMAI items) and less frequent PA and vocalizations (scoring 2–5 on the selected CMAI items) were included for the analysis. We did not include residents without the behavior (a score of 1 on the selected CMAI items), because, given the generally high prevalence of agitation in NH-residents, comparing NH-residents with very frequent behavior with residents without PA or vocalizations would not result in finding correlates that are specifically relevant for identifying those with very frequent behavior.
To take the hierarchical structure of the data into account (NH-residents within care units), we used multilevel modeling with a mixed model including a random intercept varying across the care unit level. For selecting variables for multivariate analysis, univariate multilevel logistic regression analysis was used to exploratively assess the relationship of characteristics (age, sex, duration of institutionalization, dementia severity, psychotropic drug use (PDU) and other neuropsychiatric symptoms) with very frequent PA and with very frequent vocalizations. To assess the independent relationships of correlates with the outcomes we included variables with p < 0.25 in the univariate analyses in a multivariate logistic model (Hosmer & Lemeshow, Citation2000).
Results
Very frequent physical aggression
Due to missing relevant CMAI items in two residents, the total sample of NH-residents was 2072. We found a 2-week prevalence of 2.2% (95% CI: 1.63–2.89) for very frequent PA (N = 45) and a 2-week prevalence of 24.0%, (95% CI: 22.24–25.92) for less frequent PA (N = 498). The majority of NH-residents with very frequent PA were female (77.8%). Mean age of these residents was 81.6 (SD 8.6) years and ranged from 47 to 93 years. Most NH-residents were in a moderately severe stage of dementia (GDS 6, 48.9%) (see ). Antipsychotic drugs (55.8%) were prescribed most often in these residents. Apathy was the NPI item with the highest prevalence in this group (55.6%) (see ).
Table 2. Psychotropic drug use and Neuropsychiatric symptoms of NH-residents with Dementia with Very Frequent Physical Aggression (PA) and Less Frequent PA (Total N = 2072) as well as NH-residents with Dementia with Very Frequent Vocalizations and Less Frequent Vocalizations (Total N = 2073).
In the univariate multilevel analysis, dementia severity, the use of antipsychotics and having apathy were correlated with very frequent PA, based on a p-value of <0.25 (see ). Multivariate multilevel logistic regression analysis with these variables showed that the odds for very frequent PA were statistically significantly higher in residents who had apathy (OR 1.93, 95% CI 1.04-3.61) (see ).
Table 3. UnivariateTable Footnote† and multivariateTable Footnote‡ multilevel logistic regression analysis of demographic characteristics of NH-residents with very frequent physical aggression compared to NH-residents with less frequent physical aggression.
Very frequent vocalizations
The total sample of NH-residents was 2073, due to missing relevant CMAI items in one resident. We found a 2-week prevalence of very frequent vocalizations (N = 239) of 11.5% (95% CI: 10.23–12.98) compared with a 2-week prevalence of 18.9% (95% CI: 17.28–20.65) for less frequent vocalizations (N = 392). NH-residents with very frequent vocalizations had a mean age of 81.5 (SD 8.4) years. Most of these NH-residents were female (78.7%), were in a moderately severe stage of dementia (GDS 6, 47.3%) (see ) and had the highest prescription rates for antipsychotic drugs (49.1%). Irritability was the NPI item with the highest prevalence in this group (49.4%) (see ).
In univariate multilevel analyses, age, severity of dementia and the use of antipsychotics, antidepressants, anxiolytics and antiepileptics were significantly associated with very frequent vocalizations. Furthermore, the odds for very frequent vocalizations were significantly higher in NH-residents who had anxiety, euphoria, aberrant motor behavior or night-time behavior (see ). In multivariate multilevel analyses (see ), a correlate for very frequent vocalizations was age (OR 0.97, 95% CI: 0.951–0.998), which means that NH-residents with a lower age were more likely to develop very frequent vocalizations. Other correlations were the use of antipsychotic drugs (OR 1.56, 95% CI 1.08–2.26), antiepileptic drugs (OR 2.75, 95% CI 1.34–5.68) and having euphoria (OR 2.01, 95% CI 1.22–3.31). Dementia severity was, again, a correlate when considered overall: NH-residents with a GDS score of 6 were less likely to have very frequent vocalizations than those with a GDS score of 4/5 (reference category). NH-residents with a GDS score of 7 were more likely to have very frequent vocalizations than those with a GDS score of 4/5 (GDS 6 OR 0.86, 95% CI 0.49–1.52; GDS 7 OR 1.54, 95% CI 0.85–2.78, the overall p-value was .020).
Table 4. UnivariateTable Footnote† and multivariateTable Footnote‡ multilevel logistic regression analysis of demographic characteristics of NH-residents with very frequent vocalizations compared to NH-residents with less frequent vocalizations.
Discussion
As far as we know, this is the first study to explore the 2-week prevalence and correlates of NH-residents with very frequent PA and very frequent vocalizations in a large sample of NH-residents with dementia. A 2-week prevalence of 2.2% was observed for very frequent PA. NH-residents with apathy were more likely to have very frequent PA. The 2-week prevalence of very frequent vocalizations was 11.5%. NH-residents with a higher age, more severe dementia, having euphoria or using antipsychotics and antiepileptics were more likely to have very frequent vocalizations.
Very frequent physical aggression
The prevalence for very frequent PA is comparable with the findings by Voyer et al. (Citation2005). In that study, fewer than 3% of the older adults in long-term care facilities displayed PA often or always (Voyer et al., Citation2005).
The association with apathy may seem remarkable, because the definition of apathy in the NPI encompasses diminished initiative and indifference, which seem to conflict with the acting out behavior seen in PA (Cummings, Citation1997). A possible explanation for the relationship found could be the executive dysfunction syndrome (Lyketsos, Rosenblatt, & Rabins, Citation2004). In people with the executive dysfunction syndrome, damage in one or more of the three involved brain circuits originating in the frontal lobes (dorsolateral prefrontal circuit, lateral orbitofrontal circuit and anterior cingulum circuit) can lead to co-occurrence of apathy and aggression (Lyketsos et al., Citation2004; Trzepacz et al., Citation2013). In addition, damage to the same structures may also cause disinhibition (O'Callaghan, Hodges, & Hornberger, Citation2013).
A second explanation for the relationship of apathy with PA could be boredom in the NH-resident, which may initially cause apathy followed by PA (Cohen-Mansfield, Dakheel-Ali, Marx, Thein, & Regier, Citation2015).
A third explanation for this association could be pain; chronic pain in a NH-resident may lead to apathy or unexpected outbursts of aggression (van Dalen-Kok et al., Citation2015).
A fourth explanation of the correlation of apathy with physical aggression could lie in external factors, like staff ratio; perhaps a low staff ratio leads to apathy in NH-residents due to insufficient attention for these residents, which consecutively may lead to aggression (Lawton, Citation1989). Unfortunately, we could not include these variables in the analysis because we were limited by the available data of the four studies. Finally, the correlation can be a result of suboptimal validity of the apathy measurement (Gerritsen et al., Citation2019). It may be difficult to observe apathy in more severe dementia.
Associations of PA with older age, male sex, antipsychotic drug use, mild or severe cognitive impairment (Voyer et al., Citation2005), delusions and hallucinations (Leonard et al., Citation2006) have been described in other studies regarding less frequent PA. We did not find these associations for very frequent PA. Perhaps this could partly be explained by the fact that the definition of PA was (slightly) different and prevalences for PA were higher in these studies.
Very frequent vocalizations
Cohen-Mansfield, Werner, & Marx (Citation1990) described a prevalence rate of 15% for residents screaming at least once or twice per day, which is in line with the prevalence rate we found in our study. A higher prevalence of 25% of disruptive vocalizations (> 20 times per day shift) was reported in the study by Cariaga et al. (Citation1991), probably due to the inclusion of more types of vocalizations (e.g. abusive language (profanities) and negativism) compared with our study (Cariaga et al., Citation1991).
Regarding the correlates for very frequent vocalizations, we could only find studies about less frequent vocalizations to compare our results with. Associations with the use of antiepileptic drugs or with euphoria have not been described in the literature.
Again, as with aggression, frontal lobe damage may be a possible explanation for the association of euphoria with very frequent vocalizations. One of the brain circuits involved with executive dysfunction, the anterior cingulum circuit, is important for mood and emotion, especially in the preservation of positive mood (Hornak et al., Citation2003; Lyketsos et al., Citation2004). Additionally, as described above, this anterior cingulate circuit may cause disinhibition (O'Callaghan et al., Citation2013), and has been shown to be involved in voluntary initiation and suppression of vocalizations (Hornak et al., Citation2003; Jurgens, Citation2002).
On the one hand, associations we found for age (Beck et al., Citation2011), the use of antipsychotic drugs (Zeisel et al., Citation2003), and dementia severity (Beck et al., Citation2011; Sloane, Davidson, Knight, Tangen, & Mitchell, Citation1999) are consistent with other studies in NH-residents with less frequent vocalizations. On the other hand, some studies found associations with depression, anxiety and irritability, which we could not confirm (Beck et al., Citation1998; Beck & Vogelpohl, Citation1999; Cohen-Mansfield & Libin, Citation2005; Draper et al., Citation2000; Dwyer & Byrne, Citation2000; Menon et al., Citation2001). Possible reasons for this are the differences in the study populations (like male-female distribution), settings, sample sizes and the use of different measurement instruments.
Although we did not include other emotional or environmental factors in our analyses, it is possible that these factors play a role in the occurrence of vocalizations. Namely, several studies describe a relationship of premorbid personality (having a history of introversion, rigidity, emotional control, and (dis)agreeableness) with vocalizations (Holst, Hallberg, & Gustafson, Citation1997; Kolanowski, Strand, & Whall, Citation1997; Zielin & McCabe, Citation2016). Furthermore, associations are reported of vocalizations with the environment in general (Zeisel et al., Citation2003) and specific factors such as temperature (Cohen-Mansfield & Werner, Citation1995). A higher awareness of these associations might positively influence the practice of NH-staff.
Finally, earlier studies show that the way of providing care, NH-staff attitudes and care staff characteristics all influence the behavior of NH-residents (Burshnic, Douglas, & Barker, Citation2018; Gerritsen, van Beek, & Woods, Citation2018). For example, less challenging behavior occurs in NH-residents with dementia when NH-staff has a more hopeful attitude towards them (Gerritsen et al., Citation2018). It would have been interesting if we had data about these factors, to confirm the findings of these studies.
Strengths and limitations
Our study has several strengths. It used a large and representative sample of NH-residents, resulting from the participation of a large number of nursing homes from many regions of the Netherlands. Additionally, since the same assessment instruments were used in the four combined studies, it was straightforward to merge and interpret the data.
This study also has some limitations. First, the 2-week prevalence rates found may be influenced by PDU, which may have weakened the relationships between the correlates and very frequent PA or very frequent vocalizations. Second, because of its cross-sectional design, our findings should not be interpreted as causal relationships. As an example, for PDU, the high frequency of the behavior may lead to the use of psychotropic drugs instead of PDU leading to very frequent behavior. Besides this, possible causes for the behaviors (severity of dementia) and possible consequences of these behaviors (PDU) were combined in the same statistical model, which could have influenced our findings. Third, the most important methodological consideration of our study is the operationalization of very frequent PA and very frequent vocalizations. To begin with, as we used the CMAI to define very frequent PA and very frequent vocalizations, the items of this assessment instrument restricted the operationalization of these behaviors. This way, we have also partly predetermined the prevalence rates of these behaviors by our unambiguous, but consequently narrow definitions. Maybe the prevalence rates we found could be considered an underestimation. Another limitation is the fact that the CMAI only reports frequency and not intensity or severity of distress like the NPI-NH. Behavior which is very frequent but less intense can be well tolerated by people involved, while behavior which is less frequent but intense can have a great impact. Furthermore, although we tried to operationalize very frequent PA and vocalizations by aligning with existing operationalizations in previous studies, this appeared to be more complex than expected. In the current literature, differences in the use of terminology of (physical) aggression (Bridges-Parlet et al., Citation1994; Cohen-Mansfield, Citation2008; Patel & Hope, Citation1993) and vocalizations (Beck et al., Citation2011; Cohen-Mansfield, Citation2008; Cohen-Mansfield & Werner, Citation1997; von Gunten et al., Citation2008) were observed and various measurement instruments were used to operationalize PA and vocalizations (Beck et al., Citation1998; Patel & Hope, Citation1993; Whall et al., Citation2013). In consequence, diverging and overlapping classifications exist for the same behaviors (Cohen-Mansfield & Werner, Citation1997; Gerritsen et al., Citation2019; Patel & Hope, Citation1993). Additionally, the fact that frequencies of the behaviors were not further specified in several articles was another difficulty in operationalizing. As a consequence, these difficulties in aligning with other studies imply difficulties in comparing our findings with those from other studies. As already mentioned earlier in the discussion, a final limitation concerns the fact that comparison with other studies is limited due to differences in study populations (like male-female distribution), settings and sample sizes.
Yet, our definition and operationalization of very frequent PA and vocalizations could facilitate replication and comparison with other studies in future research. Nevertheless, further studies are needed to define and operationalize very frequent PA and vocalizations, especially by incorporating the context in which these behaviors occur. The influence of the care environment as a cause of these behaviors is important, like the interaction with NH-staff. Finally, although further exploring subtypes of PA or vocalizations would have been interesting, it was not possible to perform these analyses because the groups became too small for analysis or comparison.
Conclusion
To conclude, in this study we found a 2-week prevalence of 2.2% for very frequent PA and of 11.5% for very frequent vocalizations. Characteristics of NH-residents with very frequent PA or very frequent vocalizations are different from NH-residents with less frequent PA or vocalizations. Boredom, pain and factors according to environment may be explanations for the association of apathy with very frequent PA. Furthermore, executive dysfunction needs attention in the scientific study of very frequent challenging behavior as it may be a possible explanation for both the association of apathy with very frequent PA and the association of euphoria with very frequent vocalizations. Our findings contribute to gaining insight into these two types of behaviors and may improve the care and quality of life of NH-residents. Simultaneously, it may increase the quality and safety of the working experience of NH-staff.
However, although we could identify correlates for very frequent PA and very frequent vocalizations, further research is needed to confirm and extend our findings. New studies should consider the validity of measurements and fully consider this in their choice for a certain data collection method. Moreover, a straightforward definition of very frequent PA and vocalizations is needed that incorporates the context of the behaviors. This may eventually result in a better understanding, treatment and quality of life of NH-residents with very frequent PA and very frequent vocalizations.
Sponsor’s role
None.
Acknowledgements
We would like to acknowledge Geertje van de Ven and Sandra Zwijsen for making the data of their studies available for our study.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Algase, D. L., Beck, C., Kolanowski, A., Whall, A., Berent, S., Richards, K., & Beattie, E. (1996). Need-driven dementia-compromised behavior: An alternative view of disruptive behavior. American Journal of Alzheimer's Disease, 11(6), 10–19. doi:10.1177/153331759601100603
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders. 4th ed. Arlington, VA: American Psychiatric Publishing.
- Beck, C., Frank, L., Chumbler, N. R., O'Sullivan, P., Vogelpohl, T. S., Rasin, J., … Baldwin, B. (1998). Correlates of disruptive behavior in severely cognitively impaired nursing home residents. The Gerontologist, 38(2), 189–198. doi:10.1093/geront/38.2.189
- Beck, C., Richards, K., Lambert, C., Doan, R., Landes, R. D., Whall, A., … Feldman, Z. (2011). Factors associated with problematic vocalizations in nursing home residents with dementia. The Gerontologist, 51(3), 389–405. doi:10.1093/geront/gnq129
- Beck, C. K., & Vogelpohl, T. S. (1999). Problematic vocalizations in institutionalized individuals with dementia. Journal of Gerontological Nursing, 25(9), 17–26; quiz 48, 51. doi:10.3928/0098-9134-19990901-07
- Bourbonnais, A., & Ducharme, F. (2008). Screaming in elderly persons with dementia: A critical review of the literature. International Journal of Social Research and Practice, 7(2), 205–225.
- Bourbonnais, A., & Ducharme, F. (2010). The meanings of screams in older people living with dementia in a nursing home. International Psychogeriatrics, 22(7), 1172–1184. doi:10.1017/S1041610209991670
- Bridges-Parlet, S., Knopman, D., & Thompson, T. (1994). A descriptive study of physically aggressive behavior in dementia by direct observation. Journal of the American Geriatrics Society, 42(2), 192–197. doi:10.1111/j.1532-5415.1994.tb04951.x
- Brodaty, H., Draper, B. M., & Low, L. F. (2003). Behavioural and psychological symptoms of dementia: A seven-tiered model of service delivery. The Medical Journal of Australia, 178(5), 231–234.
- Burshnic, V. L., Douglas, N. F., & Barker, R. M. (2018). Employee attitudes towards aggression in persons with dementia: Readiness for wider adoption of person-centered frameworks. Journal of Psychiatric and Mental Health Nursing, 25(3), 176–187. doi:10.1111/jpm.12452
- Cariaga, J., Burgio, L., Flynn, W., & Martin, D. (1991). A controlled study of disruptive vocalizations among geriatric residents in nursing homes. Journal of the American Geriatrics Society, 39(5), 501–507. doi:10.1111/j.1532-5415.1991.tb02497.x
- Caspi, E. (2016). Deaths as a result of resident-to-resident altercations in dementia in long-term care homes: A need for research, policy, and prevention. Journal of the American Medical Directors Association, 17(1), 7–11. doi:10.1016/j.jamda.2015.10.003
- Cohen-Mansfield, J. (2008). Agitated behavior in persons with dementia: The relationship between type of behavior, its frequency, and its disruptiveness. Journal of Psychiatric Research, 43(1), 64–69. doi:10.1016/j.jpsychires.2008.02.003
- Cohen-Mansfield, J., Dakheel-Ali, M., Marx, M. S., Thein, K., & Regier, N. G. (2015). Which unmet needs contribute to behavior problems in persons with advanced dementia? Psychiatry Research, 228(1), 59–64. doi:10.1016/j.psychres.2015.03.043
- Cohen-Mansfield, J., & Libin, A. (2005). Verbal and physical non-aggressive agitated behaviors in elderly persons with dementia: Robustness of syndromes. Journal of Psychiatric Research, 39(3), 325–332. doi:10.1016/j.jpsychires.2004.08.009
- Cohen-Mansfield, J., Marx, M. S., & Rosenthal, A. S. (1989). A description of agitation in a nursing home. Journal of Gerontology, 44(3), M77–84. doi:10.1093/geronj/44.3.M77
- Cohen-Mansfield, J., & Werner, P. (1995). Environmental influences on agitation: An integrative summary of an observational study. American Journal of Alzheimer's Care and Related Disorders & Research, 10(1), 32–39. doi:10.1177/153331759501000108
- Cohen-Mansfield, J., & Werner, P. (1997). Typology of disruptive vocalizations in older persons suffering from dementia. International Journal of Geriatric Psychiatry, 12(11), 1079–1091. doi:10.1002/(SICI)1099-1166(199711)12:11<1079::AID-GPS689>3.0.CO;2-P
- Cohen-Mansfield, J., Werner, P., & Marx, M. S. (1990). Screaming in nursing home residents. Journal of the American Geriatrics Society, 38(7), 785–792. doi:10.1111/j.1532-5415.1990.tb01470.x
- Cummings, J., Mintzer, J., Brodaty, H., Sano, M., Banerjee, S., Devanand, D. P., … Zhong, K. (2015). Agitation in cognitive disorders: International Psychogeriatric Association provisional consensus clinical and research definition. International Psychogeriatrics, 27(1), 7–17. doi:10.1017/s1041610214001963
- Cummings, J. L. (1997). The Neuropsychiatric Inventory: Assessing psychopathology in dementia patients. Neurology, 48(5 Suppl 6), S10–S16. doi:10.1212/wnl.48.5_suppl_6.10s
- Cummings, J. L., Mega, M., Gray, K., Rosenberg-Thompson, S., Carusi, D. A., & Gornbein, J. (1994). The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology, 44(12), 2308–2314. doi:10.1212/WNL.44.12.2308
- de Jonghe, J. F., & Kat, M. G. (1996). Factor structure and validity of the Dutch version of the Cohen-Mansfield Agitation Inventory (CMAI-D). Journal of the American Geriatrics Society, 44(7), 888–889. doi:10.1111/j.1532-5415.1996.tb03762.x
- Draper, B., Snowdon, J., Meares, S., Turner, J., Gonski, P., McMinn, B., … Luscombe, G. (2000). Case-controlled study of nursing home residents referred for treatment of vocally disruptive behavior. International Psychogeriatrics, 12(3), 333–344. doi:10.1017/s1041610200006438
- Dwyer, M., & Byrne, G. J. (2000). Disruptive vocalization and depression in older nursing home residents. International Psychogeriatrics, 12(4), 463–471. doi:10.1017/S104161020000658X
- Ferrah, N., Murphy, B. J., Ibrahim, J. E., Bugeja, L. C., Winbolt, M., LoGiudice, D., … Ranson, D. L. (2015). Resident-to-resident physical aggression leading to injury in nursing homes: A systematic review. Age and Ageing, 44(3), 356–364. doi:10.1093/ageing/afv004
- Gerritsen, D. L., Smalbrugge, M., Veldwijk-Rouwenhorst, A. E., Wetzels, R., Zuidema, S. U., & Koopmans, R. T. C. M. (2019). The difficulty with studying challenging behavior. Journal of the American Medical Directors Association, 20(7), 879–881. doi:10.1016/j.jamda.2019.01.148.
- Gerritsen, D. L., van Beek, A. P. A., & Woods, R. T. (2019). Relationship of care staff attitudes with social well-being and challenging behavior of nursing home residents with dementia: A cross sectional study. Aging & Mental Health, 23(11), 1517–1523. doi:10.1080/13607863.2018.1506737
- Goergen, T., Gerlach, A., Nowak, S., Reinelt-Ferber, A., Jadzewski, S., & Taefi, A. (2020). Danger in safe spaces? Resident-to-resident aggression in institutional care. In P. A. (Ed.), Advances in elder abuse research: Practise, legistation and policy (pp. 181–192). Dublin: Spinger Nature Switzerland.
- Gotovac, K., Nikolac Perkovic, M., Pivac, N., & Borovecki, F. (2016). Biomarkers of aggression in dementia. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 69, 125–130. doi:10.1016/j.pnpbp.2016.03.002
- Guidelines for ATC Classification (1990).
- Hazelhof, T. J., Schoonhoven, L., van Gaal, B. G., Koopmans, R. T., & Gerritsen, D. L. (2016). Nursing staff stress from challenging behaviour of residents with dementia: A concept analysis. International Nursing Review, 63(3), 507–516. doi:10.1111/inr.12293
- Holst, A., & Skar, L. (2017). Formal caregivers' experiences of aggressive behaviour in older people living with dementia in nursing homes: A systematic review. International Journal of Older People Nursing, 12(4), e12158. doi:10.1111/opn.12158
- Holst, G., Hallberg, I. R., & Gustafson, L. (1997). The relationship of vocally disruptive behavior and previous personality in severely demented institutionalized patients. Archives of Psychiatric Nursing, 11(3), 147–154. doi:10.1016/S0883-9417(97)80038-6
- Hornak, J., Bramham, J., Rolls, E. T., Morris, R. G., O'Doherty, J., Bullock, P. R., & Polkey, C. E. (2003). Changes in emotion after circumscribed surgical lesions of the orbitofrontal and cingulate cortices. Brain: A Journal of Neurology, 126(Pt 7), 1691–1712. doi:10.1093/brain/awg168
- Hosmer, D. W. J., & Lemeshow, S. (2000). In Applied logistic regression (pp. 95). New York: John Wiley & Sons.
- Isaksson, U., Graneheim, U. H., Astrom, S., & Karlsson, S. (2011). Physically violent behaviour in dementia care: Characteristics of residents and management of violent situations. Aging & Mental Health, 15(5), 573–579. doi:10.1080/13607863.2011.556600
- Jurgens, U. (2002). Neural pathways underlying vocal control. Neuroscience & Biobehavioral Reviews, 26(2), 235–258.
- Kat, M. G., de Jonghe, J. F., Aalten, P., Kalisvaart, C. J., Droes, R. M., & Verhey, F. R. (2002). Neuropsychiatric symptoms of dementia: Psychometric aspects of the Dutch Neuropsychiatric Inventory (NPI). Tijdschrift Voor Gerontologie en Geriatrie, 33(4), 150–155. [].
- Kolanowski, A. M., Strand, G., & Whall, A. (1997). A pilot study of the relation of premorbid characteristics to behavior in dementia. Journal of Gerontological Nursing, 23(2), 21–30. doi:10.3928/0098-9134-19970201-08
- Lawton, M. P. (1989). In K. W. S. Schaie, C. (Ed.), Social structure and aging: Psychological processes. New York: Erlbaum.
- Leonard, R., Tinetti, M. E., Allore, H. G., & Drickamer, M. A. (2006). Potentially modifiable resident characteristics that are associated with physical or verbal aggression among nursing home residents with dementia. Archives of Internal Medicine, 166(12), 1295–1300. doi:10.1001/archinte.166.12.1295
- Liljegren, M., Landqvist Waldo, M., & Englund, E. (2018). Physical aggression among patients with dementia, neuropathologically confirmed post-mortem. International Journal of Geriatric Psychiatry, 33(2), e242–e248. doi:10.1002/gps.4777
- Lyketsos, C. G., Rosenblatt, A., & Rabins, P. (2004). Forgotten frontal lobe syndrome or "Executive Dysfunction Syndrome." Psychosomatics, 45(3), 247–255. doi:10.1176/appi.psy.45.3.247
- Menon, A. S., Gruber-Baldini, A. L., Hebel, J. R., Kaup, B., Loreck, D., Itkin Zimmerman, S., … Magaziner, J. (2001). Relationship between aggressive behaviors and depression among nursing home residents with dementia. International Journal of Geriatric Psychiatry, 16(2), 139–146. doi:10.1002/1099-1166(200102)16:2<139::AID-GPS284>3.0.CO;2-5
- Nagaratnam, N., Patel, I., & Whelan, C. (2003). Screaming, shrieking and muttering: The noise-makers amongst dementia patients. Archives of Gerontology and Geriatrics, 36(3), 247–258. doi:10.1016/S0167-4943(02)00169-3
- O'Callaghan, C., Hodges, J. R., & Hornberger, M. (2013). Inhibitory dysfunction in frontotemporal dementia: A review. Alzheimer Disease and Associated Disorders, 27(2), 102–108. doi:10.1097/WAD.0b013e318265bbc9
- Patel, V., & Hope, T. (1993). Aggressive behaviour in elderly people with dementia: A review. International Journal of Geriatric Psychiatry, 8(6), 457–472. doi:10.1002/gps.930080603
- Reisberg, B., Ferris, S. H., de Leon, M. J., & Crook, T. (1988). Global Deterioration Scale (GDS). Psychopharmacology Bulletin, 24(4), 661–663.
- Sloane, P. D., Davidson, S., Knight, N., Tangen, C., & Mitchell, C. M. (1999). Severe disruptive vocalizers. Journal of the American Geriatrics Society, 47(4), 439–445. doi:10.1111/j.1532-5415.1999.tb07236.x
- Stutte, K., Hahn, S., Fierz, K., & Zuniga, F. (2017). Factors associated with aggressive behavior between residents and staff in nursing homes. Geriatric Nursing (New York, N.Y.).), 38(5), 398–405. doi:10.1016/j.gerinurse.2017.02.001
- Trzepacz, P. T., Yu, P., Bhamidipati, P. K., Willis, B., Forrester, T., Tabas, L., … Saykin, A. J. (2013). Frontolimbic atrophy is associated with agitation and aggression in mild cognitive impairment and Alzheimer's disease. Alzheimer's & Dementia, 9(5S), S95–S104.e1. doi:10.1016/j.jalz.2012.10.005
- van Dalen-Kok, A. H., Pieper, M. J., de Waal, M. W., Lukas, A., Husebo, B. S., & Achterberg, W. P. (2015). Association between pain, neuropsychiatric symptoms, and physical function in dementia: A systematic review and meta-analysis. BMC Geriatrics, 15, 49. doi:10.1186/s12877-015-0048-6
- van de Ven, G., Draskovic, I., Adang, E. M., Donders, R., Zuidema, S. U., Koopmans, R. T., & Vernooij-Dassen, M. J. (2013). Effects of dementia-care mapping on residents and staff of care homes: A pragmatic cluster-randomised controlled trial. PLoS One, 8(7), e67325. doi:10.1371/journal.pone.0067325
- Veldwijk-Rouwenhorst, A. E., Smalbrugge, M., Wetzels, R., Bor, H., Zuidema, S. U., Koopmans, R., & Gerritsen, D. L. (2017). Nursing home residents with dementia and very frequent agitation: A particular group. The American Journal of Geriatric Psychiatry, 25(12), 1339–1348. doi:10.1016/j.jagp.2017.08.002
- von Gunten, A., Alnawaqil, A. M., Abderhalden, C., Needham, I., & Schupbach, B. (2008). Vocally disruptive behavior in the elderly: A systematic review. International Psychogeriatrics, 20(4), 653–672. doi:10.1017/s1041610208006728
- Voyer, P., Verreault, R., Azizah, G. M., Desrosiers, J., Champoux, N., & Bedard, A. (2005). Prevalence of physical and verbal aggressive behaviours and associated factors among older adults in long-term care facilities. BMC Geriatrics, 5, 13. doi:10.1186/1471-2318-5-13
- Wetzels, R. B., Zuidema, S. U., de Jonghe, J. F., Verhey, F. R., & Koopmans, R. T. (2010). Course of neuropsychiatric symptoms in residents with dementia in nursing homes over 2-year period. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 18(12), 1054–1065. doi:10.1097/JGP.0b013e3181f60fa1
- Whall, A. L., Kim, H., Colling, K. B., Hong, G. R., DeCicco, B., & Antonakos, C. (2013). Measurement of aggressive behaviors in dementia: Comparison of the physical aggression subscales of the Cohen-Mansfield Agitation Inventory and the Ryden Aggression Scale. Research in Gerontological Nursing, 6(3), 171–177. doi:10.3928/19404921-20130321-01
- Wood, S., Cummings, J. L., Hsu, M. A., Barclay, T., Wheatley, M. V., Yarema, K. T., & Schnelle, J. F. (2000). The use of the neuropsychiatric inventory in nursing home residents. Characterization and measurement. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 8(1), 75–83. doi:10.1097/00019442-200002000-00010
- Yusupov, A., & Galvin, J. E. (2014). Vocalization in dementia: A case report and review of the literature. Case Reports in Neurology, 6(1), 126–133. doi:10.1159/000362159
- Zeisel, J., Silverstein, N. M., Hyde, J., Levkoff, S., Lawton, M. P., & Holmes, W. (2003). Environmental correlates to behavioral health outcomes in Alzheimer's special care units. The Gerontologist, 43(5), 697–711. doi:10.1093/geront/43.5.697
- Zeller, A., Hahn, S., Needham, I., Kok, G., Dassen, T., & Halfens, R. J. (2009). Aggressive behavior of nursing home residents toward caregivers: A systematic literature review. Geriatric Nursing (New York, N.Y.).), 30(3), 174–187. doi:10.1016/j.gerinurse.2008.09.002
- Zielin, S., & McCabe, M. (2016). Exploring the relationship between premorbid personality and dementia-related behaviors. Journal of Gerontological Nursing, 42(1), 40–48. doi:10.3928/00989134-20151008-77
- Zuidema, S. U., Derksen, E., Verhey, F. R., & Koopmans, R. T. (2007). Prevalence of neuropsychiatric symptoms in a large sample of Dutch nursing home patients with dementia. International Journal of Geriatric Psychiatry, 22(7), 632–638. doi:10.1002/gps.1722
- Zwijsen, S. A., Kabboord, A., Eefsting, J. A., Hertogh, C. M., Pot, A. M., Gerritsen, D. L., & Smalbrugge, M. (2014). Nurses in distress? An explorative study into the relation between distress and individual neuropsychiatric symptoms of people with dementia in nursing homes. International Journal of Geriatric Psychiatry, 29(4), 384–391. doi:10.1002/gps.4014
- Zwijsen, S. A., Smalbrugge, M., Eefsting, J. A., Twisk, J. W., Gerritsen, D. L., Pot, A. M., & Hertogh, C. M. (2014). Coming to grips with challenging behavior: A cluster randomized controlled trial on the effects of a multidisciplinary care program for challenging behavior in dementia. Journal of the American Medical Directors Association, 15(7), e531. doi:10.1016/j.jamda.2014.04.007