Abstract
Objectives
Older women report lower mental health compared to men, yet little is known about the nature of this sex difference. Therefore, this study investigates time trends and possible risk groups.
Method
Data from the Doetinchem Cohort Study (DCS) and the Longitudinal Aging Study Amsterdam (LASA) were used. General mental health was assessed every 5 years, from 1995 to 1998 onwards (DCS, n = 1412, 20-year follow-up, baseline age 55–64 years). Depressive and anxiety symptoms were assessed for two birth cohorts, from 1992/1993 onwards (LASA cohort 1, n = 967, 24-year follow-up, age 55-65 years,) and 2002/2003 onwards (LASA cohort 2, n = 1002, 12-year follow-up, age 55–65 years) with follow-up measurements every 3–4 years.
Results
Mixed model analyses showed that older women had a worse general mental health (−6.95; −8.36 to 5.53; range 0–100, ∼10% lower), more depressive symptoms (2.09; 1.53–2.63; range 0-60, ∼30% more) and more anxiety symptoms (0.86; 0.54–1.18; range 0–11, ∼30% more) compared to men. These sex differences remained stable until the age of 75 years, where after they decreased due to an accelerated decline in mental health for men compared to women. Sex differences and their course by age were consistent over successive birth cohorts, educational levels and ethnic groups (Caucasian vs. Turkish/Moroccan).
Conclusion
There is a consistent female disadvantage in mental health across different sociodemographic groups and over decennia (1992 vs. 2002) with no specific risk groups.
Introduction
Adult women are twice as often diagnosed with depression and anxiety disorders and report a significantly lower general mental health compared to men (Jalnapurkar, Allen, & Pigott, Citation2018; Kuehner, Citation2003; Maji, Citation2018; Weissman et al., Citation1993). How this sex difference develops by age and whether it persists at old ages remains unclear. Since good mental health is an important determinant of healthy aging, a more detailed understanding of the sex difference in mental health among older adults is needed to inform preventive and treatment strategies of potential target groups to enhance healthy mental aging among older women.
Previous studies have shown that the higher prevalence of poor mental health in women compared to men arises around puberty, remains stable during adolescence but showed mixed results among older adults (Chaplin, Gillham, & Seligman, Citation2009; Derdikman-Eiron et al., Citation2012; Leach, Christensen, Mackinnon, Windsor, & Butterworth, Citation2008). Several empirical studies investigating the changes in the sex difference across the older adult life span showed that it decreased by age at age, 40, 50 or 65, increased by age after age 65 or remained stable among 40–80 years old (Girgus, Yang, & Ferri, Citation2017). All these results however demonstrate that the prevalence of depression in men and women does not completely converge after menopause (Byers, Yaffe, Covinsky, Friedman, & Bruce, Citation2010; Luppa et al., Citation2012); instead the female disadvantage seems to continue into old age (Kuehner, Citation2017). In general, these studies used a cross-sectional approach, with different participants at different ages. As a result, cohort effects cannot be ruled out (Twisk, Citation2011). Long-term longitudinal research is needed to accurately investigate the development of the sex difference in mental health from adulthood to old age (Leach et al., Citation2008).
It has been suggested that persons with a lower educational level form a risk group for a more apparent sex difference in mental health. This was demonstrated by comparing high and low educated men and women separately for depressive and anxiety symptoms (Mwinyi et al., Citation2017; Ross & Mirowsky, Citation2006) and mental health (Vable et al., Citation2018). Here, the educational difference was higher among women than for men. This suggests that the sex difference may be larger among lower educated persons compared to higher educated persons. However, these studies did not statistically compare the sex difference among education groups nor include older adults.
Ethnicity also has been demonstrated to be associated with mental health. Previous research in the United States has found that African Americans, Asian Americans and Hispanic Americans report more depressive symptoms compared to Caucasian ethnic groups in America, independent of socioeconomic status (Hargrove et al., Citation2020; Hooker et al., Citation2019; Liang, Xu, Quiñones, Bennett, & Ye, Citation2011; Sorkin, Pham, & Ngo-Metzger, Citation2009; Xu, Liang, Bennett, Quiñones, & Ye, Citation2010). Recent research in the Netherlands showed that older Turkish/Moroccan immigrants form a risk group for poor (mental) health, since they have two times higher levels of depressive and anxiety symptoms and lower self-rated health compared to the Dutch population (Denktas, Citation2011; Klokgieters, van Tilburg, Deeg, & Huisman, Citation2018; Devillé et al., Citation2006). This might be explained by cultural differences, lower socioeconomic status, unhealthier life style or other health factors (Denktas, Citation2011). These factors might affect men and women differently, but this remains to be investigated.
The literature on the change in mental health over successive birth cohorts is conflicting, suggesting an increase, decrease or stable trend of mental health indicators over time (Girgus et al., Citation2017; Jorm, Patten, Brugha, & Mojtabai, Citation2017; Tampubolon & Maharani, Citation2017). It has been suggested that the prevalence of depression increases in women, but remains stable for men (Spiers et al., Citation2012), which would mean an increase in the sex difference in mental health over time. However, a stable sex difference in depression prevalence has also been demonstrated (Kessler et al., Citation1994). These older studies are derived from cross-sectional designs using retrospective information from different countries and therefore bias could have been introduced (Leach et al., Citation2008). More recent research comparing (sex differences in) mental health across birth cohorts is needed.
This study aims to identify possible demographic risk groups, which will help identify potential target groups for prevention strategies aiming to enhance healthy mental aging in older women (Kaeberlein, Rabinovitch, & Martin, Citation2015). Furthermore, the potential variation of the sex difference over successive birth cohorts may inform us on future trends in mental health. In order to achieve these aims, this study undertakes a longitudinal investigation to answer the following three questions: (1) How does the sex difference in mental health develop during aging; (2) are there risk groups for a more pronounced sex difference with regard to educational level and ethnicity; and (3) does the sex difference differ between different birth cohorts?
Methods
Study samples
Data from two large prospective cohort studies were used, both containing data on a wide variety of indicators for healthy aging. The Doetinchem Cohort Study (DCS) includes (older) adults living in/close to Doetinchem in the Netherlands (Verschuren, Blokstra, Picavet, & Smit, Citation2008). For a more detailed description of DCS see the cohort profile described by Verschuren et al. (Citation2008). The Medical Ethics Committee of the Utrecht Medical Center approved DCS. The Longitudinal Aging Study Amsterdam (LASA) includes older adults of three culturally distinct regions in the Netherlands (Zwolle, Oss and Amsterdam) (Hoogendijk et al., Citation2016). For a more detailed description of LASA see the cohort profile described by Hoogendijk et al. (Citation2016). The Ethical Review Board of the VU University Medical Center approved LASA. All participants gave written informed consent after the nature of the procedures was fully explained. Data of both studies were collected by questionnaires and medical interviews performed by trained staff. The investigation in this study was carried out in accordance with the latest version of the Declaration of Helsinki.
Birth cohort populations
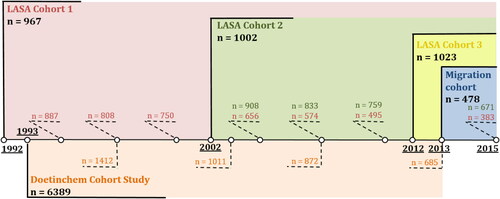
With the emphasis on older adults, participants aged 55 years and older were included from DCS and LASA. General mental health was measured in DCS at baseline in 1993/1997, (n = 1412, aged 55–65 years, 20-year follow-up) with follow-up measurements every 5 years. Two longitudinal birth cohorts of LASA were used, with baseline measurements in 1992/1993 (LASA cohort 1, n = 967, 24-year follow-up) and 2002/2003 (LASA cohort 2, n = 1002, 12-year follow-up) with follow-up measurements every 3–4 years. Data of two additional cross-sectional LASA cohorts were used, with measurements in 2012/2013 (LASA cohort 3, n = 1023) and 2013/2014 (Migration cohort, n = 478). The latter cohort consisted of Turkish and Moroccan immigrants. provides a schematic overview of the different birth cohort samples and their follow-up measurements.
Figure 1. Schematic timeline of different (birth) cohort populations. The longitudinal Doetinchem Cohort (shown in orange, n = 1412) measured general mental health inventory from baseline measurements in 1993–1997 with follow-up measurements every 5 years (dotted lines with adjusted n per follow-up measurement). The Longitudinal Aging Study (LASA) has two longitudinal birth cohorts with baseline measurements in 1992/1993 (LASA cohort 1, shown in red, n = 967) and 2002/2003 (LASA cohort 2, shown in green, n = 1002) both with follow-up measurements every 3–4 years. LASA has two additional cross-sectional cohorts, a Dutch cohort with measurements in 2012/2013 (LASA cohort 3, shown in yellow, n = 1023) and a Turkish/Moroccan cohort with measurements in 2013 (Migration cohort, show in blue, n = 478).
Mental health indicators
This study contained three separate continuous outcome measures for mental health: general mental health, depressive symptoms and anxiety symptoms. Since changes on a population level were of interest in this study, symptoms were studied. General mental health in the past month was assessed using the five-item Mental Health Inventory questionnaire (MHI-5) (Berwick et al., Citation1991). The MHI-5 is a five-item questionnaire with a five-point scale on the frequency of a set of positive and negative feelings, ranging from zero (all the time) to four (never), transformed into a score ranging from 0 to 100. A higher sore indicates better mental health. A score of 60 and higher is most commonly used to indicate good mental health (Kelly, Dunstan, Lloyd, & Fone, Citation2008). The MHI-5 has shown good validity in measuring general mental health on a population level (McCabe, Thomas, Brazier, & Coleman, Citation1996). Depressive symptoms during the past week were measured using the Center for Epidemiologic Studies Depression Scale (CES-D) (Carleton et al., Citation2013). It is a 20-item questionnaire with a four-point scale ranging from zero (rarely or none of the time; less than one day per week) to three (most or almost all the time; 5–7 days per week), transformed into a score ranging from 0 to 60. A higher score indicates more depressive symptoms and a cut-off of 16 is most commonly used as indication for clinically relevant depressive symptoms (Vilagut, Forero, Barbaglia, & Alonso, Citation2016). The CES-D has shown high reliability and good criterion validity in several populations, including older adults (Beekman et al., Citation1997; Van De Rest, Van Der Zwaluw, Beekman, De Groot, & Geleijnse, Citation2009). Anxiety symptoms during the past 4 weeks were assessed using the Hospital Anxiety and Depression Scale-Anxiety sub-scale (HADS-A) (Snaith, Citation2003). The HADS-A is a seven-item questionnaire with a four-point scale ranging from zero (rarely or never) to three (mostly or always), transformed into a score ranging from 0 to 21. A higher score indicates more anxiety symptoms and a score of eight or higher is the most commonly used indication for clinically relevant anxiety symptoms (Snaith, Citation2003). The HADS-A has shown excellent reliability and good validity in older populations (Julian, Citation2011).
Risk groups for a more apparent sex difference in mental health
To test if there are risk groups with regard to age, educational level and ethnicity for which the sex difference is more apparent, the size of the sex difference was compared between these different risk groups. For age it was investigated whether the size of the sex difference significantly changed by age (interaction sex and age). For educational level, the size of the sex difference (interaction sex and educational level) and the course of the sex difference by age (interaction sex, age and educational level) was compared between different educational levels. Education level was categorized into low (elementary education or less), middle (lower vocational education and general intermediate education) and high (intermediate vocational education, general secondary education, higher vocational education, college education and university). For ethnic groups, the size of the sex difference (interaction sex and ethnic groups) was compared between Dutch and Turkish or Moroccan. Data of the migration cohort were used for the Turkish and Moroccan ethnic groups and data of LASA cohort 3 were used for the Dutch ethnic group. Turkish and Moroccan ethnicities were taken together to ensure sufficient statistical power.
Trend of the sex difference in mental health over time (1992 vs. 2002)
To investigate the trend of the sex difference in mental health over time, depressive and anxiety symptoms of two longitudinal birth cohorts were compared (LASA cohorts 1 and 2). First it was investigated whether the size of the sex difference changed over successive birth cohorts (interaction sex and birth cohort) and secondly whether the course of the sex difference by age changed over successive birth cohorts (interaction sex, age and birth cohort). These analyses compared older adults aged 55–65 years from LASA cohort 1 (started in 1992/1993, 25-year follow-up, 8 measurements) with LASA cohort 2 (started in 2002/2003, 15-year follow-up, 5 measurements).
Statistical method
Mixed model analyses with a random intercept for the individual and a random slope for the age of the individual were used to examine the longitudinal data (DCS, LASA cohorts 1 and 2) and linear regression analyses were used to examine the cross-sectional data (LASA cohort 3 and migration cohort). Mixed model analyses included all longitudinal data of the outcome, thereby not losing previous measurements of participants when they drop-out or have missing values on (further) follow-up measurements. This prevents the loss of available data and creates more statistical power (Twisk, Citation2011). The percentage of missing values in all three indicators of mental health was similar between men and women and relatively stable over follow-up measurements (approximately 15% on average). Taking this into account with the fact that there were no missing values for the other baseline variables used (sex, age, educational level and ethnic group) we assumed no implications due to missing values in our analyses and a robust regression coefficient estimate. For the linear regression analyses, full case only analyses were performed. Missing values were again relatively low (approximately 10%), appeared only in the outcome measurements and to be equal over men and women, so it was assumed not to influence our results.
Overview analysis steps
In total, four analysis steps were taken. First, the overall age-adjusted sex difference for the three separate mental health indicators was investigated for all (birth) cohort populations separately (variable ‘sex’ in an age-adjusted model). Second, the longitudinal course of the sex difference in mental health by age was investigated using the longitudinal data of DCS and LASA cohorts 1 and 2. In these analyses the significance of the interaction term of age and sex (‘age * sex’) was determined. If ‘age * age’ improved the model significantly as determined by the likelihood test, the quadratic regression coefficient was additionally included in further analyses steps, since this allowed a better estimation of the decline in mental health measures by age. Third, whether the size of the age-adjusted sex difference in mental health differed by birth cohort, educational level or ethnicity was investigated for each (birth) cohort population (significance of the interaction term with sex in an age-adjusted model: ‘birth cohort * sex’, ‘education * sex’ or ‘ethnicity * sex’). Fourth, whether the course of the sex difference in mental health by age differed between birth cohorts or educational levels was investigated using the longitudinal data DCS and LASA cohorts 1 and 2 (significance of the interaction term with sex * age: ‘birth cohort * sex * age’ and ‘education * sex * age’). To visually depict the longitudinal course of general mental health, depressive symptoms and anxiety symptoms by age and sex, lines were plotted based on the regression coefficients of the statistical model. All analyses were performed using Stata (version 14.0, Stata Inc.).
Results
(Birth) cohort populations
At baseline, all LASA cohort populations had an equal number of men and women a mean age of 60 ranging from 55 to 64/65 years. Overall, women were lower educated, scored lower on all mental health indicators and had more often a poor mental health compared to men ().
Table 1. Baseline characteristics for men and women of the different (birth) cohort populations.
Age-adjusted sex difference in mental health
Adjusted for age, women consistently reported poorer general mental health and more depressive and anxiety symptoms compared to men (). For example, older women scored 6.95 (95% CI: 8.36 − 5.53) points lower on general mental health (ranging from 0 to 100) compared to men. Another example, women from LASA cohort 1 scored 2.09 (95% CI: 1.53 − 2.63) points higher on depressive symptoms (ranging from 0 to 60) compared to men.
Table 2. Age-adjusted mean difference in three mental health indicators between women and men in persons of the different (birth) cohort populations.
Course of sex differences in mental health
In general, for both men and women mental health slightly decreased by age in a non-linear manner ( and ). For all three indicators of mental health, the sex difference narrowed after the age of approximately 75 years, due to an (accelerated) decline in mental health for men compared to women (). This was also demonstrated by the significance of the interaction terms sex * age * age for general health and anxiety symptoms (). Although the interaction term for depressive symptoms did not reach the significance threshold (p = .136), a similar trend was observed from the depicted model (). The sex difference in depressive and anxiety symptoms remained stable for LASA birth cohort 2 (sex * age and sex * age * age; p > .05) (), where the participants did not reach the age of 75 years ().
Figure 2. Longitudinal course of three indicators of mental health by age and sex in older adults. (A) Self-reported general mental health inventory measured by the MHI-5 questionnaire by age for men and women of the Doetinchem Cohort Study (DCS) aged 55–64 years at baseline measurements in 1995/1998. (B) Self-reported depressive symptoms measured by the CES-D questionnaire and (C) anxiety symptoms measured by the HADS-A questionnaire by age for men and women of the Longitudinal Aging Study Amsterdam (LASA) cohort 1 with baseline measurements in 1992/1993 (solid lines) and LASA cohort 2 with baseline measurements in 2002/2003 (dotted lines) aged 55–65 years at baseline. Lines depict results of statistical models.
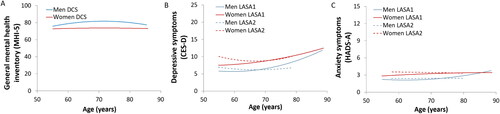
Table 3. Multivariable model of the longitudinal course of the sex difference in three different mental health indicators by age.
Risk groups for a more apparent sex difference in mental health
There was no significant age at which the size of the sex difference was more apparent compared to others ages for all three mental health indicators (). Furthermore, there was no significant difference in the size of the sex difference (nor in the longitudinal course by age) between different educational levels and ethnic groups. So, none of the interaction terms (sex * ethnicity, sex * education and sex * age * education) reached significance levels.
Trend of the sex difference in mental health over time (1992 vs. 2002)
There was neither a significant difference in the size nor the course of the sex difference between LASA birth cohorts 1 and 2 for depressive symptoms and anxiety symptoms. So the interaction terms sex * birthcohort and sex * age * birthcohort did not reach significance.
Discussion
This study demonstrated a consistent sex difference in mental health among older adults; women report lower mental health for three separate indicators: general mental health, depressive symptoms and anxiety symptoms. This finding was independent of age, educational level, ethnic group and birth cohort. Furthermore, there were no risk groups for a more apparent sex difference with regard to these investigated sociodemographic factors. Moreover, the sex difference diminished after the age of 75 years due to an (accelerated) decline of mental health among older men, demonstrated in all three mental health indicators.
The size of the sex difference in depressive symptoms and anxiety symptoms is similar to previous research among older adults (Jalnapurkar et al., Citation2018) but its clinical relevance needs to be considered. Since the current study is population based, the average general mental health inventory score was high, depressive and anxiety symptoms were low and the variation by age was small. Taking this into account, women still scored on average 10% lower on general mental health (dividing the mean score of men by the mean difference between men and women: 78/7) and about 30% higher on depressive symptoms (8/2.5) and anxiety symptoms (3.5/1). Furthermore, the sex difference was higher than the overall variance within men and women across the 25 years of follow-up (sex difference/increase over time) for all three mental health indicators. The sex differences found in this study could suggest a clinical relevance difference in mental health.
The observed sex difference can either be a true difference in mental health status or, alternatively, reflect gender and/or sex differences in the reporting and/or the perception of mental health. An item-separate analyses of the CES-D, HADS-A and MHI-5 questionnaires demonstrated that all items had similar sex differences and trends by age compared to the complete questionnaire (data not shown). It still remains difficult to determine whether these sex differences represent a true health difference, since questionnaires are the tool to identify these outcomes on a population level. Further in-depth research investigating the sex-specific relationship between self-reported mental health and health outcomes is advised.
This study demonstrated that there is a consistent and similar sex difference in mental health across different ages, educational levels and ethnic groups; women report a worse mental health in three separate indicators. In line with previous research, the current study found higher depressive and anxiety symptoms and a lower general mental health inventory in lower educated persons and Turkish/Moroccan ethnic groups compared to higher educated persons and Dutch ethnic group (Bauldry, Citation2015; Bjelland et al., Citation2008; Liang et al., Citation2011; Lorant et al., Citation2003; Xu et al., Citation2010). However, no specific sociodemographic risk groups with regard to age, educational level and ethnicity were identified for which the sex difference in mental health is most apparent.
The observed sex difference in mental health can be explained by various theories. One is the susceptibility theory which describes biological and psychological risk factors (Kuehner, Citation2017). Another theory is based on environmental factors on both the individual and societal level. Both theories are shortly discussed below (Kuehner, Citation2017). For more detailed information, please refer to Kuehner (Citation2017) and Li et al. (2017).
With regard to the biological susceptibility theory, there is limited empirical evidence for a stronger genetic risk for depression among women compared to men (Flint & Kendler, Citation2014), but ovarian hormones have been often demonstrated to modulate various neurotransmitter systems in the brain and the HPA axis activation system, thereby increasing the risk for depression among women (Slavich & Sacher, Citation2019). Here, (social) stress and inflammation-related depressed mood play an important role, especially for women with an already existing higher risk for mood disorders or in the midst of a hormonal transition period, such as puberty or menopause (Slavich & Sacher, Citation2019). In contrast, so far there is inconclusive evidence for an increase in anxiety and depressive symptoms during menopausal transition (Judd, Hickey, & Bryant, Citation2012). In line with these findings, current results showed no spiking increase in mental health symptoms around menopause in women. This suggests that ovarian hormones might not play an (important) role in the higher depression prevalence among older women. Next to biological factors, previous studies suggest that psychological gender factors such as personality and coping styles may also partly explain the observed sex difference in mental health among adolescence (Salk, Hyde, & Abramson, Citation2017). Neuroticism and body shame and dissatisfaction have been demonstrated to have a mediating effect on the sex difference in depression among adolescence, although merely from cross-sectional studies to date (Kuehner, Citation2017; Leach et al., Citation2008). In addition, a ruminative response style (the tendency to passively and repetitively analyzes one’s distress problems and concerns without taking action) has been proposed to account for a substantial part of the sex difference in mental health among adolescences (Goodwin & Gotlib, Citation2004; Kuehner, Citation2017; Parker & Brotchie, Citation2010). Future studies investigating whether these psychological gender factors also (partly) explain the observed sex difference in mental health among older adults is needed.
With regard to the environmental theory, individual common stress exposure and higher stress susceptibility among women has been suggested to partly explain the sex difference in mental health (Hyde & Mezulis, Citation2020). For example, data from the Netherlands Mental Health Survey and Incidence Study showed that paid work was associated with a decreased prevalence of depressive and anxiety disorders for both men and women, but in women, the protective role was restricted to those without children (Plaisier et al., Citation2008). Furthermore, women are more commonly victims to interpersonal violence, such as sexual abuse or intimate physical violence, which has been demonstrated to explain part of the higher prevalence of depression and anxiety among women (Hyde & Mezulis, Citation2020; Li & Graham, Citation2017). Also on a societal level, sex is associated with various mental health determinants such as socioeconomic status, access to resources and social status. Consequently, the degree of gender equality is reversely associated with depressive symptoms (Salk et al., Citation2017; Van de Velde, Huijts, Bracke, & Bambra, Citation2013). Note, the previously discussed theories are mostly based on studies including adolescence. There is much less knowledge about whether this sex difference occurs in older adults, the magnitude of this difference and it’s change by age. In addition, whether this effect occurs in older adults for the same reasons that it occurs at earlier life stages remains unknown. It does seems clear that there is a new set of stressors that arise in old age, such as widowhood/living alone, poor health/chronic illness, cognitive decline and caregiving (Girgus et al., Citation2017). Moreover, the way women respond to these stressors compared to men with regard to coping styles and personality might still explain part of the sex difference in mental health among older adults. Unfortunately, there is not sufficient research to be certain whether any of these new stressors contribute to the sex difference in depression in old age. Future longitudinal research investigating the impact of these stressors on the life course of sex differences in mental health is recommended.
The current study demonstrated a narrowing of the sex difference in mental health after the age of 75 years, due to an accelerated decrease in three indicators of mental health among men. Although the three used indicators describe different aspects of mental health, all showed a similar trend. The age of 75 years as a turning point at which the consistent sex difference decreases, was at higher ages than suggested by previous research indicating menopause (age 50-60 years) (Bebbington et al., Citation2003; Jorm, Citation1987; Portman, Riskind, & Rector, Citation2012; ). This discrepancy is most likely explained by the cross-sectional design or short-term follow-up of previous studies, prohibiting drawing conclusions about potential sex differences during the aging process. Therefore, the findings of the current prospective study provide a more solid estimate. Although a popular belief (Kuehner, Citation2017), the sex difference in mental health is not linked solely to the reproductive life of women. A possible explanation for the accelerated worsening in mental health for older men might be their decrease in coping with regard to loss of a spouse or partner compared to men (younger than 75 years) (Aldwin, Sutton, Chiara, & Spiro, Citation1996; Diehl et al., Citation2014) and greater decrease in seeking social support as compared to older women (Meléndez, Mayordomo, Sancho, & Tomás, Citation2012). Although there is no specific risk group for which the sex difference seems most apparent, the accelerated worsening in mental health in men could suggest that men aged 75 years and older are a specific risk group for a decline in mental health. However, women still score (significantly) poorer in mental health measures in all ages compared to men (Djernes, Citation2006; Girgus et al., Citation2017; Luppa et al., Citation2012; McLean, Asnaani, Litz, & Hofmann, Citation2011; Schaub & Linden, Citation2000; Vink et al., Citation2009; Zunzunegui et al., 2007). Only after the age of 90 the female disadvantage seems to disappear, since at this point the higher decrease in mental health among men has caught up with the lower mental health among women. However, at this age there is a lower statistical power due to a lower number of participants, so additional research is needed to investigate this finding.
A slight increase in depressive or anxiety symptoms among adults aged 50–70 years over successive birth cohorts was observed in this study. This is in line with previous research demonstrating a (slightly) higher number of depressive symptoms among adults aged 50–60 years in more recent compared to older birth cohorts (Abrams & Mehta, Citation2019; Zivin, Pirraglia, McCammon, Langa, & Vijan, Citation2013). In contrast, a study by Tampubolon and Maharani (Citation2017) suggested a decrease in depressive symptoms over successive birth cohorts (Tampubolon & Maharani, Citation2017). This discrepancy might be an artifact of using a quadratic specification for age in the latter study to handle different observed age ranges across the cohorts (Blazer, Citation2017). Moreover, it has been shown that the prevalence of anxiety disorders remains stable over successive cohorts in the Netherlands. However, this was based on a study in adults aged 18–64 years and did not include anxiety symptoms but only anxiety disorder status (De Graaf, Ten Have, Van Gool, & Van Dorsselaer, Citation2012). Although a small cohort effect was found on the absolute levels of depressive and anxiety symptoms in the current study, no significant change in the sex difference across these cohorts was found. Thus, it seems that any cohort effect on mental health affects men and women equally. It is therefore hypothesized that developments in our society (a higher increase in education for women compared to men, for example) do not seem to significantly affect the differences between men and women in mental health.
This study has several strengths. First, it uses data of two large prospective longitudinal cohort studies, includes two successive longitudinal birth cohorts and all cohorts have a low drop-out on each follow-up measurements. Furthermore, it includes three different mental health outcomes, all of which have a high reliability and validity, that all show consistent results in the current study (Beekman et al., Citation1997; Julian, Citation2011; Kelly et al., Citation2008; Van De Rest et al., Citation2009). In addition, this is the first study to investigate various demographic risk groups in relationship to the sex difference in mental health. Finally, the current study was population based, eliminating the possible influence of differences in help-seeking behavior of mental health care between men and women (Mackenzie, Gekoski, & Knox, Citation2006). A possible limitation of this study is the healthy cohort effect, which might affect men and women differently since women live longer (Freedman, Wolf, & Spillman, Citation2016; Minicuci et al., Citation2004). This might have caused an overestimation of the sex difference, since more unhealthy men compared to unhealthy women are die. Furthermore, the influence of ethnicity could only be studied in a cross-sectional design and the mental health questionnaires were not validated for this subpopulation of Turkish and Moroccan older adults. Finally, LGBTQ people are a known risk group for lower mental health compared to cisgender heterosexual people across age (Kaniuka et al., Citation2019). Unfortunately, data on sexual orientation was not available in the current study to investigate whether this this association with mental health differs between men and women. Future research investigating this risk group is recommended.
In conclusion, there is a consistent sex difference in mental health among older adults aged 55 years and older. There are no specific risk groups with regard to age, educational level and ethnicity for which the sex difference is most apparent. The sex difference decreases after the age of 75 years due to an accelerated worsening of all three mental health aspects in men. However, the sex difference in mental health remains at all ages. No target group was identified for preventive strategies and treatments aimed to enhance mental health; older women form a uniform risk group for poorer mental health compared to men. Future research should identify whether this is caused by sex-specific risk factors to be able to divert these preventive strategies toward specific risk factors.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Data cannot be shared publicly because of confidentiality. Data are available from the LASA Institutional Data Access/Ethics Committee (contact via https://www.lasa-vu.nl/index.htm) for researchers who meet the criteria for access to confidential data. The LASA Steering Group will review all requests for data to ensure that proposals for the use of LASA data do not violate privacy regulations and are in keeping with informed consent that is provided by all LASA participants. The authors of this study do not have any special access privileges to the data underlying this study that other researchers would not have.
Additional information
Funding
References
- Abrams, L. R., & Mehta, N. K. (2019). Changes in depressive symptoms over age among older Americans: Differences by gender, race/ethnicity, education, and birth cohort. SSM – Population Health, 7, 100399. doi:https://doi.org/10.1016/j.ssmph.2019.100399
- Aldwin, C. M., Sutton, K. J., Chiara, G., & Spiro, A. (1996). Age differences in stress, coping, and appraisal: Findings from the normative aging study. Journals of Gerontology – Series B, 54(4), 179–188.
- Australian Bureau of Statistics. (2008). Mental health and wellbeing: Summary of results [Internet]. National Survey. Available from: https://www.abs.gov.au/AUSSTATS/[email protected]/Lookup/4326.0Main+Features32007?OpenDocument
- Bauldry, S. (2015). Variation in the protective effect of higher education against depression. Society and Mental Health, 5(2), 154–161.
- Bebbington, P., Dunn, G., Jenkins, R., Lewis, G., Brugha, T., Farrell, M., & Meltzer, H. (2003). The influence of age and sex on the prevalence of depressive conditions: Report from the National Survey of Psychiatric Morbidity. International Review of Psychiatry (Abingdon, England)), 15(1–2), 74–83. doi:https://doi.org/10.1080/0954026021000045976
- Beekman, A. T. F., Deeg, D. J. H., Van Limbeek, J., Braam, A. W., De Vries, M. Z., & Van Tilburg, W. (1997). Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): Results from a community-based sample of older subjects in the Netherlands. Psychological Medicine, 27(1), 231–235. doi:https://doi.org/10.1017/S0033291796003510
- Berwick, D. M., Murphy, J. M., Goldman, P. A., Ware, J. E., Barsky, A. J., & Weinstein, M. C. (1991). Performance of a five-item mental health screening test. Medical Care, 29(2), 169–176. doi:https://doi.org/10.1097/00005650-199102000-00008
- Bjelland, I., Krokstad, S., Mykletun, A., Dahl, A. A., Tell, G. S., & Tambs, K. (2008). Does a higher educational level protect against anxiety and depression? The HUNT study. Social Science & Medicine, 66(6), 1334–1345. doi:https://doi.org/10.1016/j.socscimed.2007.12.019
- Blazer, D. (2017). Do we ever outlive depression? The American Journal of Geriatric Psychiatry, 25(11), 1196–1197.
- Byers, A. L., Yaffe, K., Covinsky, K. E., Friedman, M. B., & Bruce, M. L. (2010). High occurrence of mood and anxiety disorders among older adults: The National Comorbidity Survey Replication. Archives of General Psychiatry, 67(5), 489.
- Carleton, R. N., Thibodeau, M. A., Teale, M. J., Welch, P. G., Abrams, M. P., & Robinson, T. (2013). The center for epidemiologic studies depression scale: A review with a theoretical and empirical examination of item content and factor structure. PLoS One., 8(3), e58067.
- Chaplin, T. M., Gillham, J. E., & Seligman, M. E. P. (2009). Gender, anxiety, and depressive symptoms: A longitudinal study of early adolescents. The Journal of Early Adolescence, 29(2), 307–327. doi:https://doi.org/10.1177/0272431608320125
- De Graaf, R., Ten Have, M., Van Gool, C., & Van Dorsselaer, S. (2012). Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Social Psychiatry and Psychiatric Epidemiology, 47(2), 203–213. doi:https://doi.org/10.1007/s00127-010-0334-8
- Denktas, S. (2011). Health and Health Care Use of Elderly Immigrants in the Netherlands: A comparative study (133 p.).
- Derdikman-Eiron, R., Indredavik, M. S., Bakken, I. J., Bratberg, G. H., Hjemdal, O., & Colton, M. (2012). Gender differences in psychosocial functioning of adolescents with symptoms of anxiety and depression: Longitudinal findings from the Nord-Trøndelag Health Study. Social Psychiatry and Psychiatric Epidemiology, 47(11), 1855–1863.
- Devillé, W., Uiters, E., Westert, G., Groenewegen, P. (2006). Perceived health and consultation of GPs among ethnic minorities compared to the general population in the Netherlands. In G.P. Westert, L. Jabaaij, F.G. Schellevis (Eds.), Morbidity, performance and quality in primary care: Dutch general practice on stage (pp. 85–96). Oxon: Radcliffe Publishing.
- Diehl, M., Chui, H., Hay, E. L., Lumley, M. A., Grühn, D., & Labouvie-Vief, G. (2014). Change in coping and defense mechanisms across adulthood: Longitudinal findings in a European American sample. Developmental Psychology, 50(2), 634–648. doi:https://doi.org/10.1037/a0033619
- Djernes, J. K. (2006). Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatrica Scandinavica, 113(5), 372–387. doi:https://doi.org/10.1111/j.1600-0447.2006.00770.x
- Flint, J., & Kendler, K. S. (2014). The genetics of major depression. Neuron, 81(3), 484–503. doi:https://doi.org/10.1016/j.neuron.2014.01.027
- Freedman, V. A., Wolf, D. A., & Spillman, B. C. (2016). Disability-free life expectancy over 30 years: A growing female disadvantage in the US population. American Journal of Public Health, 106(6), 1079–1085. doi:https://doi.org/10.2105/AJPH.2016.303089
- Girgus, J., Yang, K., & Ferri, C. (2017). The gender difference in depression: Are elderly women at greater risk for depression than elderly men? Geriatrics [Internet], 2(4), 35. Available from: http://www.mdpi.com/2308-3417/2/4/35
- Goodwin, R. D., & Gotlib, I. H. (2004). Gender differences in depression: The role of personality factors. Psychiatry Research, 126(2), 135–142. doi:https://doi.org/10.1016/j.psychres.2003.12.024
- Hargrove, T. W., Halpern, C. T., Gaydosh, L., Hussey, J. M., Whitsel, E. A., & Dole, N. (2020). Race/ethnicity, gender, and trajectories of depressive symptoms across early- and mid-life among the add health cohort. Journal of Racial and Ethnic Health Disparities, 7(4), 619–629.
- Hoogendijk, E. O., Deeg, D. J. H., Poppelaars, J., van der Horst, M., Broese van Groenou, M. I., Comijs, H. C., … Huisman, M. (2016). The longitudinal aging study Amsterdam: Cohort update 2016 and major findings. European Journal of Epidemiology, 31(9), 927–945. doi:https://doi.org/10.1007/s10654-016-0192-0
- Hooker, K., Phibbs, S., Irvin, V. L., Mendez-Luck, C. A., Doan, L. N., & Li, T. (2019). Depression among older adults in the United States by disaggregated race and ethnicity. Gerontologist, 59(5), 886–891.
- Hyde, J. S., & Mezulis, A. H. (2020). Gender differences in depression: Biological, affective, cognitive, and sociocultural factors. Harvard Review of Psychiatry, 28(1), 4–13.
- Jalnapurkar, I., Allen, M., & Pigott, T. (2018). Sex differences in anxiety disorders: A review. Psychiatry, Depression & Anxiety, 4, 1–9.
- Jorm, A. F. (1987). Sex and age differences in depression: A quantitative synthesis of published Research. The Australian and New Zealand Journal of Psychiatry, 21(1), 46–53. doi:https://doi.org/10.3109/00048678709160898
- Jorm, A. F., Patten, S. B., Brugha, T. S., & Mojtabai, R. (2017). Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry, 16(1), 90–99. doi:https://doi.org/10.1002/wps.20388
- Judd, F. K., Hickey, M., & Bryant, C. (2012). Depression and midlife: Are we overpathologising the menopause? Journal of Affective Disorders, 136(3), 199–211. doi:https://doi.org/10.1016/j.jad.2010.12.010
- Julian, L. J. (2011). Measures of anxiety. Arthritis Care & Research, 63(S11), S467–S472. doi:https://doi.org/10.1002/acr.20561
- Kaeberlein, M., Rabinovitch, P. S., & Martin, G. M. (2015). Healthy aging: The ultimate preventative medicine. Science (New York, N.Y.), 350(6265), 1191–1193. doi:https://doi.org/10.1126/science.aad3267
- Kaniuka, A., Pugh, K. C., Jordan, M., Brooks, B., Dodd, J., Mann, A. K., … Hirsch, J. K. (2019). Stigma and suicide risk among the LGBTQ population: Are anxiety and depression to blame and can connectedness to the LGBTQ community help? Journal of Gay & Lesbian Mental Health, 23(6), 1–16.
- Kelly, M. J., Dunstan, F. D., Lloyd, K., & Fone, D. L. (2008). Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: A comparison of five different methods. BMC Psychiatry, 8(1), 10. doi:https://doi.org/10.1186/1471-244X-8-10
- Kessler, R. C., McGonagle, K. A., Nelson, C. B., Hughes, M., Swartz, M., & Blazer, D. G. (1994). Sex and depression in the National Comorbidity Survey. II: Cohort effects. Journal of Affective Disorders, 30(1), 15–26.
- Klokgieters, S. S., van Tilburg, T. G., Deeg, D. J. H., & Huisman, M. (2018). Gezondheidsverschillen onder oudere migranten in Nederland. Demos, 34(9), 4–7.
- Kuehner, C. (2003). Gender differences in unipolar depression: An update of epidemiological findings and possible explanations. Acta Psychiatrica Scandinavica, 108(3), 163–174. doi:https://doi.org/10.1034/j.1600-0447.2003.00204.x
- Kuehner, C. (2017). Why is depression more common among women than among men? The Lancet Psychiatry, 4(2), 146–158.
- Leach, L. S., Christensen, H., Mackinnon, A. J., Windsor, T. D., & Butterworth, P. (2008). Gender differences in depression and anxiety across the adult lifespan: The role of psychosocial mediators. Social Psychiatry and Psychiatric Epidemiology, 43(12), 983–998. doi:https://doi.org/10.1007/s00127-008-0388-z
- Li, S. H., & Graham, B. M. (2017). Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. The Lancet. Psychiatry, 4(1), 73–82. doi:https://doi.org/10.1016/S2215-0366(16)30358-3
- Liang, J., Xu, X., Quiñones, A. R., Bennett, J. M., & Ye, W. (2011). Multiple trajectories of depressive symptoms in middle and late life: Racial/ethnic variations. Psychology and Aging, 26(4), 761–777. doi:https://doi.org/10.1037/a0023945
- Lorant, V., Deliège, D., Eaton, W., Robert, A., Philippot, P., & Ansseau, M. (2003). Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology, 157(2), 98–112. doi:https://doi.org/10.1093/aje/kwf182
- Luppa, M., Sikorski, C., Luck, T., Ehreke, L., Konnopka, A., Wiese, B., … Riedel-Heller, S. G. (2012). Age- and gender-specific prevalence of depression in latest-life-systematic review and meta-analysis . Journal of Affective Disorders, 136(3), 212–221. doi:https://doi.org/10.1016/j.jad.2010.11.033
- Mackenzie, C. S., Gekoski, W. L., & Knox, V. J. (2006). Age, gender, and the underutilization of mental health services: The influence of help-seeking attitudes. Aging & Mental Health, 10(6), 574–582. doi:https://doi.org/10.1080/13607860600641200
- Maji, S. (2018). Society and ‘good woman’: A critical review of gender difference in depression. The International Journal of Social Psychiatry, 64(4), 396–405. doi:https://doi.org/10.1177/0020764018765023
- McCabe, C. J., Thomas, K. J., Brazier, J. E., & Coleman, P. (1996). Measuring the mental health status of a population: A comparison of the GHQ-12 and the SF-36 (MHI-5). The British Journal of Psychiatry , 169(4), 516–521. doi:https://doi.org/10.1192/bjp.169.4.516
- McLean, C. P., Asnaani, A., Litz, B. T., & Hofmann, S. G. (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035. doi:https://doi.org/10.1016/j.jpsychires.2011.03.006
- Meléndez, J. C., Mayordomo, T., Sancho, P., & Tomás, J. M. (2012). Coping strategies: Gender differences and development throughout life span. The Spanish Journal of Psychology, 15(3), 1089–1098. doi:https://doi.org/10.5209/rev_sjop.2012.v15.n3.39399
- Minicuci, N., Noale, M., Pluijm, S. M. F., Zunzunegui, M. V., Blumstein, T., Deeg, D. J. H., … Jylhä, M (2004). Disability-free life expectancy: A cross-national comparison of six longitudinal studies on aging. The CLESA project. European Journal of Ageing, 1(1), 37–44. doi:https://doi.org/10.1007/s10433-004-0002-5
- Mwinyi, J., Pisanu, C., Castelao, E., Stringhini, S., Preisig, M., & Schiöth, H. B. (2017). Anxiety disorders are associated with low socioeconomic status in women but not in men. Women’s Heal Issues, 27(3), 302–307.
- Parker, G., & Brotchie, H. (2010). Gender differences in depression. International Review of Psychiatry (Abingdon, England)), 22(5), 429–436. doi:https://doi.org/10.3109/09540261.2010.492391
- Plaisier, I., de Bruijn, J. G. M., Smit, J. H., de Graaf, R., ten Have, M., & Beekman, A. T. F. (2008). Work and family roles and the association with depressive and anxiety disorders: Differences between men and women. Journal of Affective Disorders, 105(1–3), 63–72.
- Portman, M. E., Riskind, J. H., & Rector, N. A. (2012). Generalized anxiety disorder. Encycl Hum Behav [Internet]. (criterion C):215–220. Available from: https://linkinghub.elsevier.com/retrieve/pii/B9780123750006001750.
- Ross, C. E., & Mirowsky, J. (2006). Sex differences in the effect of education on depression: Resource multiplication or resource substitution? Social Science & Medicine (1982)), 63(5), 1400–1413. doi:https://doi.org/10.1016/j.socscimed.2006.03.013
- Salk, R. H., Hyde, J. S., & Abramson, L. Y. (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143(8), 783–822.
- Schaub, R. T., & Linden, M. (2000). Anxiety and anxiety disorders in the old and very old – Results from the Berlin aging study (BASE). Comprehensive Psychiatry [Internet], 41(2), 48–54. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0010440X00800085
- Slavich, G. M., & Sacher, J. (2019). Stress, sex hormones, inflammation, and major depressive disorder: Extending social signal transduction theory of depression to account for sex differences in mood disorders. Psychopharmacology, 236(10), 3063–3079. doi:https://doi.org/10.1007/s00213-019-05326-9
- Snaith, R. P. (2003). Hospital Anxiety and Depression scale (HADS). Health and Quality of Life Outcomes, 1(1), 29. doi:https://doi.org/10.1186/1477-7525-1-29
- Sorkin, D. H., Pham, E., & Ngo-Metzger, Q. (2009). Racial and ethnic differences in the mental health needs and access to care of older adults in California. Journal of American Geriatrics Society, 57(12), 2311–2317.
- Spiers, N., Brugha, T. S., Bebbington, P., McManus, S., Jenkins, R., & Meltzer, H. (2012). Age and birth cohort differences in depression in repeated cross-sectional surveys in England: The National Psychiatric Morbidity Surveys, 1993 to 2007. Psychological Medicine, 42(10), 2047–2055. doi:https://doi.org/10.1017/S003329171200013X
- Tampubolon, G., & Maharani, A. (2017). When did old age stop being depressing? Depression trajectories of older Americans and Britons 2002–2012. The American Journal of Geriatric Psychiatry, 25(11), 1187–1195. doi:https://doi.org/10.1016/j.jagp.2017.06.006
- Twisk, J. W. R. (2011). Applied longitudinal data analysis for epidemiology: A practical guide (2nd ed.). Cambridge, UK: Cambridge University Press
- Vable, A. M., Cohen, A. K., Leonard, S. A., Glymour, M. M., Duarte, C. D P., & Yen, I. H. (2018). Do the health benefits of education vary by sociodemographic subgroup? Differential returns to education and implications for health inequities. Annals of Epidemiology, 28(11), 759–766. doi:https://doi.org/10.1016/j.annepidem.2018.08.014
- Van De Rest, O., Van Der Zwaluw, N., Beekman, A. T. F., De Groot, L., & Geleijnse, J. M. (2009). The reliability of three depression rating scales in a general population of Dutch older persons. International Journal of Geriatric Psychiatry, 25(10), 998–1005. doi:https://doi.org/10.1002/gps.2449
- Van de Velde, S., Huijts, T., Bracke, P., & Bambra, C. (2013). Macro-level gender equality and depression in men and women in Europe. Sociology of Health & Illness, 35(5), 682–698.
- Verschuren, W. M. M., Blokstra, A., Picavet, H. S. J., & Smit, H. A. (2008). Cohort profile: The Doetinchem Cohort Study. International Journal of Epidemiology, 37(6), 1236–1241. doi:https://doi.org/10.1093/ije/dym292
- Vilagut, G., Forero, C. G., Barbaglia, G., & Alonso, J. (2016). Screening for depression in the general population with the center for epidemiologic studies depression (ces-d): A systematic review with meta-analysis. PLoS One, 11(5), e0155431. doi:https://doi.org/10.1371/journal.pone.0155431
- Vink, D., Aartsen, M. J., Comijs, H. C., Heymans, M. W., Penninx, B. W. J. H., Stek, M. L., … Beekman, A. T. F. (2009). Onset of anxiety and depression in the aging population: Comparison of risk factors in a 9-year prospective study. The American Journal of Geriatric Psychiatry, 17(8), 642–652. doi:https://doi.org/10.1097/JGP.0b013e3181a65228
- Weissman, M. M., Bland, R., Joyce, P. R., Newman, S., Wells, J. E., & Wittchen, H. U. (1993). Sex differences in rates of depression: Cross-national perspectives. Journal of Affective Disorders, 29(2–3), 77–84.
- Xu, X., Liang, J., Bennett, J. M., Quiñones, A. R., & Ye, W. (2010). Ethnic differences in the dynamics of depressive symptoms in middle-aged and older Americans. Journal of Aging and Health, 22(5), 631–652. doi:https://doi.org/10.1177/0898264310370851
- Zivin, K., Pirraglia, P. A., McCammon, R. J., Langa, K. M., & Vijan, S. (2013). Trends in depressive symptom burden among older adults in the United States from 1998 to 2008. Journal of General Internal Medicine, 28(12), 1611–1619. doi:https://doi.org/10.1007/s11606-013-2533-y
- Zunzunegui, M. V., Minicuci, N., Blumstein, T., Noale, M., Deeg, D., Jylhä, M., & Pedersen, N. L, CLESA Working Group (2007). Gender differences in depressive symptoms among older adults: A cross-national comparison: The CLESA project. Social Psychiatry and Psychiatric Epidemiology, 42(3), 198–207. doi:https://doi.org/10.1007/s00127-007-0158-3
