 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objectives: A psychosocial intervention for spousal carers of people with dementia promoted emotional well-being through self-monitoring and personalized feedback, as demonstrated in a previous randomized controlled trial. The mechanism behind the intervention effects is thought to lie in increased awareness of, and thus, engagement in behaviours that elicit positive emotions (PA). This secondary analysis tests the assumption by investigating momentary data on activities, affect, and stress and explores the relevance of personalized feedback compared to self-monitoring only.
Methods: The intervention was based on the experience sampling method (ESM), meaning that carers self-monitored own affect and behaviours 10 times/day over 6 weeks. The experimental group received personalized feedback on behaviours that elicit PA, while the pseudo-experimental group performed self-monitoring only. A control group was also included. ESM-data of 72 carers was analysed using multilevel mixed-effects models.
Results: The experimental group reported significant increases in passive relaxation activities over the 6 weeks (B = 0.28, SE = 0.12, Z = 2.43, p < .05). Passive relaxation in this group was negatively associated with negative affect (r = –0.50, p = .01) and positively associated with activity-related stress (r = 0.52, p = .007) from baseline to post-intervention. Other activities in this or the other groups did not change significantly.
Conclusion: Carer’s daily behaviours were only affected when self-monitoring was combined with personalized feedback. Changing one’s daily behaviour while caring for a person with dementia is challenging and aligned with mixed emotions. Acknowledging simultaneously positive and negative emotions, and feelings of stress is suggested to embrace the complexity of carer’s life and provide sustainable support.
Introduction
Spousal carers of people living with dementia invest time in the care with great dedication, but combining time-consuming care tasks with common day-to-day activities can be challenging. Carers spend less time on self-care, physical activity, or social interactions than noncarers, which can negatively influence carers’ physical and mental health (Acton, Citation2002; Fredman, Bertrand, Martire, Hochberg, & Harris, Citation2006; Marquez, Bustamante, Kozey-Keadle, Kraemer, & Carrion, Citation2012; Schüz et al., Citation2015). Contrary, engagement in enjoyable activities encompassing mental, physical, and social stimulation is associated with greater positive affect (PA) (Mausbach, Coon, Patterson, & Grant, Citation2008). The term ‘PA’ refers to a wide range of positive emotions such as happiness, enthusiasm, and satisfaction and PA is important for coping with the challenge of caregiving as emphasized by the coping process model (Folkman & Moskowitz, Citation2000). Especially when individuals need to cope with a stressful situation for a longer time, positive emotions support the coping process by energizing goal-directed behaviour or gaining relief from the ongoing stress (Folkman, Citation1997). Additionally, positive emotions can broaden a person’s thought-action-repertoire, build their resources, and increase resilience and emotional well-being (Fredrickson, Citation1998, Citation2004, Citation2013). Psychosocial interventions for carers have shown to increase PA, and thus, support coping (Dowling et al., Citation2014).
The ‘partner in sight’ intervention and experience sampling method
The six-week ‘Partner in Sight’ intervention for carers of people living with dementia was designed to raise awareness for PA and related behaviours (van Knippenberg, de Vugt, Ponds, Myin-Germeys, & Verhey, Citation2016). Participants self-monitored current affect, context, and activities 10 times per day using a mobile device. Additionally, a coach provided the experimental group with a personalized feedback to stimulate carers to think about their daily activities and potentially redirect their behaviours towards activities that elicit more positive emotions. The pseudo-experimental group engaged in self-monitoring only and did not receive personalized feedback. A previous randomized controlled trial (RCT) showed that the intervention improved carer’s emotional well-being, namely sense of competence and perceived stress, in both intervention groups (van Knippenberg, de Vugt, Ponds, Myin-Germeys, & Verhey, Citation2018). However, the underlying intervention mechanism was not unravelled, as it happens in most effectiveness studies when the initial focus lies on the pre- versus post-intervention difference in outcome measures (Egan et al., Citation2018; Waller, Dilworth, Mansfield, & Sanson-Fisher, Citation2017). The mechanism behind the improved carer’s emotional well-being in the ‘Partner in Sight’ intervention is thought to lie in the increased awareness of, and engagement in activities that create positive emotions in the carers. Momentary data is ideally suited to map out this potential behavioural change (Snippe et al., Citation2016).
The term ‘behavioural change’ is defined as a significant increase/decrease of engagement in certain daily activities. Momentary data can be collected through the so called experience sampling method (ESM), which was used in the ‘Partner in Sight’ intervention to enable self-monitoring with the mobile device. This momentary information can reveal daily behavioural and emotional patterns, such as which activities are related to high positive or negative affect (Csikszentmihalyi & Larson, Citation1987; Myin‐Germeys et al., 2018; Shiffman & Stone, Citation1998), and illustrates the complexity of everyday life.
The present study
The present study aimed to determine if a behavioural change was the intervention mechanism that led to improved carer’s emotional well-being in the ‘Partner in Sight’ intervention study. This secondary approach is necessary to identify the impact the intervention had on the participant’s everyday life, and thus, test the proposed mechanism.
First, we hypothesized that the ESM self-monitoring in the ‘Partner in Sight’ intervention, particularly in combination with personalized feedback, would promote a behavioural change in the carers towards more enjoyable activities, such as self-care or relaxation. Therefore, the ESM-based daily activity data of carers was investigated from baseline to post-intervention as well as throughout the six intervention weeks. Second, we examined associations between the changes in behaviours (e.g. doing nothing, caregiving, active and passive relaxation, and self-care; self-defined by carer) and changes in affect as well as stress.
Material and methods
Participants and design
A secondary analysis of the ESM-data of the ‘Partner in Sight’ intervention was performed in this study. In short, participants (n = 76) were informal dementia carers of all subtypes and stages, who were primarily recruited from memory clinics, via digital newsletters, and the website of the Dutch Alzheimer Association (Alzheimer Nederland). Inclusion criteria included being a spousal caregiver of a person living with dementia and sharing a household with the care recipient. Participants were excluded from the study if their cognitive abilities were clinically judged as insufficient to engage in ESM (inability to use the mobile device) or if caregivers felt overburdened or had severe health problems. All participants provided written informed consent. The Medical Ethics Committee of the Maastricht University Medical Centre Plus approved the study (#143040). A more detailed summary of the design of the ‘Partner in Sight’ RCT and the effectiveness of the intervention can be found elsewhere (van Knippenberg et al., Citation2016; van Knippenberg et al., Citation2018).
The complete original study protocol included a baseline assessment, a six-week intervention period, a post-intervention assessment, and 2- and 6-month follow-up assessments. A RCT was conducted with three treatment arms, including an experimental group, a pseudo-experimental group, and a control group. Of interest in the present study is the ESM-data from the baseline assessment, intervention period, and post-intervention assessment.
Participants in the experimental and pseudo-experimental group were asked to complete the ESM-questionnaires for three consecutive days at baseline, in each intervention week, and during the post-intervention assessment. The experimental group additionally received personalized feedback (see ‘Intervention’ section for details). The control arm provided ESM-data only at baseline and for the post-intervention assessment and continued with care as usual during the intervention period. provides a graphical overview of the intervention elements per group.
Intervention
The program ‘Partner in Sight’ ran over six consecutive weeks. Both the experimental and the pseudo-experimental group engaged in ESM self-monitoring. On self-monitoring days, the ESM-questionnaire was filled in ten times per day, for a total of 30 time-points at baseline and post-intervention (10 beeps × 3 consecutive days) and 180 time-points during the intervention period (10 beeps × 3 consecutive days × 6 weeks). A ‘beep’ is a signal (sound and vibration) given by the mobile device at random time intervals between 7:30 am and 10:30 pm, prompting the participant to answer the ESM-questionnaire. Additionally, a morning and evening ESM-questionnaire asked the participants to reflect on the previous night and day, respectively. The ‘PsyMate’ mobile device was used to collect the data, and its feasibility in dementia carers has been demonstrated (van Knippenberg et al., Citation2016). ESM included questions on current mood, behaviours, and context. The full ESM-questionnaire can be found in the Appendix ().
Table A1. Description of the ESM concepts, items, and response choices in the daily, morning, and evening questionnaire.
Additionally, the experimental group received face-to-face feedback from a coach every 2 weeks. The reason for having two intervention groups was to investigate the added benefit of personalized feedback compared to self-monitoring only. Each feedback session followed a standardized protocol. Feedback was provided both verbally and graphically by a personal coach (i.e. psychologist) on the contexts and activities and their relation to the levels of PA experienced in daily life. Also, changes in daily average PA during the intervention period were discussed, and thus, positively reinforced as part of the motivational coaching. A summary of the feedback was handed out to each participant. An example of the feedback graphs can be found in the Appendix ().
Measures
Baseline assessment
The sociodemographic information of the carer and the person living with dementia was assessed at baseline, including age, sex, profession, and level of education. Additional information and the full list of baseline questionnaires, which are not part of the present post hoc analysis, can be found elsewhere (van Knippenberg et al., Citation2018).
ESM assessments
To include different days of the week, the ‘PsyMate’ mobile device beeped alternately on Friday, Saturday, and Sunday, or Tuesday, Wednesday, and Thursday during the intervention period. Behaviours were assessed with the following question: ‘What am I doing?’ Participant could choose one or more activities from the following categories: ‘doing nothing’, ‘work’, ‘household’, self-care’, ‘caring for partner’, ‘active relaxation’, ‘passive relaxation’, and ‘something else’. These daily behaviours were chosen in the daily questionnaires based on previous ESM-based studies as the most common daily behaviours (Kramer et al., Citation2014; Verhagen, Hasmi, Drukker, Van Os, & Delespaul, Citation2016) and ‘caring for partner’ was added. The present study focuses on the occurrence (0 or 1) of doing nothing, self-care behaviour, active and passive relaxation, and caregiving behaviour. Participants defined the behaviours subjectively.
PA, NA, and activity-related stress were measured on a 7-point Likert scale ranging from 1 (not at all) to 7 (very) ten times per day. The level of momentary PA was defined by the mean score of the following four items: ‘I feel cheerful’, ‘I feel relaxed’, ‘I feel enthusiastic’, and ‘I feel satisfied’. Momentary NA resulted from the ESM items ‘I feel insecure’, ‘I feel lonely’, ‘I feel anxious’, ‘I feel irritated’, ‘I feel down’, ‘I feel desperate’, and ‘I feel tensed’.
Activity-related stress included the items ‘I like doing this’ (reversed-scored), ‘I would rather be doing something else’, ‘This is difficult for me’, and ‘I can do this well’ (reversed-scored). The activity-related stress items were based on the appraisal theory (Lazarus & Folkman, Citation1984) declaring that for an activity to be stressful, it has to be perceived as negative and challenging, while the person experiences a lack of skills to cope with it (Vaessen et al., Citation2018). The mean PA, NA, and activity-related scores were calculated for each completed beep during the day with a higher score indicating higher levels of affect or stress. The reliability of PA, NA, and activity-related stress are presented on a between- and within-person level in the results section.
Statistical analysis
The presented analyses were performed post hoc. Multilevel (i.e. mixed-effects) models were used for the analysis, with level one corresponding to the daily ESM assessments nested within individuals on level two. The experimental and pseudo-experimental group were analysed separately, as the ‘Partner in Sight’ program had previously been shown to affect the groups unequally (van Knippenberg et al., Citation2018), and thus, group differences were expected. First, the intervention groups were compared to the control group. The models included a dummy variable for time (pre-/post-intervention), a dummy variable for treatment allocation (group), and the interaction between time and treatment allocation as fixed effects. Additionally, the behavioural change over the course of the intervention was analysed for the two ESM self-monitoring groups and seen as a ‘growth’ in behaviour (Snippe et al., Citation2016). The analyses included behaviour during the ESM intervention as the dependent variable and time in two-week blocks (weeks 1–2, 3–4, and 5–6) as a fixed effect. In this part of the analysis, time was operationalized through a dummy variable that reflected the course of the intervention (1 = weeks 1 and 2, 2 = weeks 3 and 4, 3 = weeks 5 and 6). The two-week blocks were chosen as the feedback was given every two weeks (). The control group was not included in this subanalysis, as ESM-data were only available at baseline and post-intervention.
The second main analysis focused on the associations between behavioural change and changes in PA, NA, and activity-related stress from baseline to post-intervention in the intervention groups individually. For this, first multilevel logistic regression models for the dichotomous behaviours were fitted (occurrence 0 or 1) as the dependent variable, and a time variable as a fixed effect. Time was here operationalized through a dummy variable of the baseline and post-intervention 3-day ESM assessments (0 = baseline t = 1…30; 1 = post-intervention t = 31…60). Second, linear mixed-effects models were used to analyse PA, NA, and activity-related stress as the dependent variables, with time (see above) as a fixed effect. Based on these models, the best linear unbiased predictions (BLUPs) were extracted to estimate subject-specific slopes corresponding to the changes in the various behaviours and the changes in PA, NA, and activity-related stress. Finally, the subject-specific slopes were correlated between the changes in behaviour and change in affect or stress.
In the RCT, changes in stress levels were only determined using retrospective measures. Therefore, we included a subanalysis to determine the change in activity-related stress from baseline to post-intervention in the intervention groups using the momentary data. A linear mixed-effects model was used, with activity-related stress as the dependent variable and time as a fixed effect. Time was here again operationalized through a dummy variable (0 = baseline t = 1…30; 1 = post-intervention t = 31…60).
All models included a random intercept for participants, a random slope for the time variable (dummy variable for either baseline or post-intervention or intervention weeks in two-week blocks), and an unstructured variance-covariance matrix for random effects. The alpha level was set to 0.05 throughout all analyses. For all statistical analyses, the statistical program Stata (version 13.0) was used.
Results
Participants
At baseline, approximately two-thirds of the total sample (67.1%) were female (n = 76 carers). The age of the participants ranged from 43 to 88 years (mean, 72.1 ± 8.39 years). About half (51.3%) were low-educated (primary education, including lower vocational), 19.7% medium-educated (secondary education, including intermediate vocational), and 28.9% highly educated (higher education, including higher vocational and bachelor’s, graduate, and doctoral degrees). All participants lived with their partner with dementia at home, and nearly all were retired/not working (96.1%). There were no significant differences in the sociodemographic information between the groups at baseline. A flow-chart of study participation and reasons for drop-outs have previously been reported (van Knippenberg et al., Citation2018).
General ESM assessments
Participants had to provide sufficient ESM data to be included in this secondary analysis (>10 valid beeps during baseline/post-intervention, > 60 beeps during the intervention (van Knippenberg et al., Citation2018)). Subjects not meeting this requirement were excluded from this analysis. Therefore, 72 participants were included in the present post hoc analysis (n = 72 at baseline, n = 42 during intervention, n = 60 at post-intervention). More specifically, out of these 72 participants at baseline, n = 25 were in the control, n = 25 in the experimental, and n = 22 in the pseudo-experimental group. Participants completed in total 8488 valid ESM questionnaires, 1660 at baseline, 5481 during the intervention, and 1347 at post-intervention. On average per person, 23 ESM assessments were completed during the baseline period, 134 ESM assessments during the intervention period, and 18 ESM assessment during the post-intervention period. The within- and between-person reliability measures (Cronbach’s alpha) of PA, NA, and activity-related stress at baseline/post-intervention and the six-week intervention period are presented in . The percentages and means of carers’ daily behaviours, affect, and activity-related stress at baseline and post-intervention for all three groups are presented in .
Pre-post changes of behaviour and growth over the six-week intervention period
Only the experimental group showed a significantly higher pre-to-post increase compared to the control group in one daily behaviour, namely passive relaxation (B = 0.60, SE = 0.30, Z = 1.99, p < .05). No significant differences in average change of behaviour were found in caregiving, active relaxation, self-care, or doing nothing in either of the two ESM self-monitoring groups in comparison to the control group ().
Passive relaxation showed a linear growth over the six-week course of the intervention in the experimental group. An average increase in the log-odds of passive relaxation by 0.28 every 2 weeks (B = 0.28, SE = 0.12, Z = 2.43, p < .05) was detected, while the pseudo-experimental group showed a nonsignificant trend of growth in the same activity (B = 0.18, SE = 0.11, Z = 1.67, p = .09). The other activities did not show a significant growth over the six-weeks in either of the intervention groups [Experimental group: doing nothing (B = −0.17, SE = 0.22, Z = −0.76, p = .45), self-care (B = 0.00, SE = 0.08, Z = 0.05, p = .96), active relaxation (B = 0.08, SE = 0.10, Z = 0.76, p = .45), caregiving (B = 0.03, SE = 0.17, Z = 0.15, p = .88); Pseudo-experimental group: doing nothing (B = −0.05, SE = 0.12, Z = −0.41, p = .68), self-care (B = 0.12, SE = 0.12, Z = 1.00, p = .32), active relaxation (B = −0.04, SE = 0.14, Z = −0.26, p = .8), caregiving (B = 0.08, SE = 0.15, Z = 0.54, p = .59)].
Associations between changes in behaviours and affect as well as activity-related stress
All associations between two variables reflect the change from baseline to post-intervention in behaviour, affect, or activity-related stress. In the experimental group, passive relaxation was negatively associated with NA (r = −0.50, p = .010) and positively associated with activity-related stress (r = 0.52, p = .007). The other behaviours did not show significant associations with PA, NA, or activity-related stress in the experimental group.
In the pseudo-experimental group, doing nothing (PA: r = 0.64, p = .001; NA: r = −0.46, p = .03) and self-care (PA: r = 0.55, p = .009; NA: r = −0.45, p = .034) were both positively associated with PA and at the same time negatively associated with NA. Caregiving was negatively associated with PA (r = −0.43, p = .047). All other behaviours did not show a significant association with affect and stress in the pseudo-experimental group ().
Activity-related stress showed a significant decrease from baseline to post-intervention in the experimental group (B = −0.24, SE = 0.08, Z = −2.95, p < .01), while there was no significant change in activity-related stress in the pseudo-experimental group (B = −0.11, SE = 0.13, Z= −0.83, p = .41).
Discussion
This study evaluates behavioural change as the underlying mechanism of the previously described intervention effect of Partner in Sight, namely improved emotional well-being in spousal carers of people living with dementia. The ESM data provided a detailed and complex picture of carer’s daily behaviours, affect, and stress, adding relevant information to the effectiveness study of the ‘Partner in Sight’ intervention (van Knippenberg et al., Citation2018).
First, this study showed that the ‘Partner in Sight’ intervention resulted in a behavioural change of one activity in the experimental group, namely an increase in passive relaxation throughout the intervention. Passive relaxation was self-defined by the carer and included various leisure activities, such as watching TV or reading, also in combination with other activities such as traveling or household activities. From baseline to post-intervention, spending more time in passive relaxation was strongly associated with increased activity-related stress and decreased NA. Overall, these associations indicate mixed feelings in the carers during the behavioural change towards more passive relaxation in everyday life.
Behavioural adaptation and mixed emotions during caregiving
Leisure as a ‘free or unobligated time that does not involve work or performing other life-sustaining functions’ (p. 3) (Leitner & Leitner, Citation2012) includes passive relaxation. Due to personal preferences, the form of leisure can vary, and carers might pursue a wide range of activities that provide respite (Lund, Utz, Caserta, & Wright, Citation2009). Leisure can have a therapeutic effect and be a coping mechanism for carers (Caldwell, Citation2005). Satisfaction with leisure experienced by the carer is suggested to act protectively against certain health risks (Chattillion et al., Citation2012). Therefore, interventions for carers may promote more engagement in leisure as a form of self-care to protect or improve well-being.
Following this well-meant advice to do more enjoyable activities, however, can be more challenging for carers of people living with dementia than health professionals might expect. Caregiving can be accompanied by feelings of inseparability between the carer and care recipient, which has been described as a ‘progressive compensatory symbiosis’ (Wang, Shyu, Wang, & Lu, Citation2017). In such a situation, pursuing one’s own leisure might be hindered by both external and internal barriers (Argüelles & von Simson, Citation2001).
In the present study, one external factor might have been the presence of the person living with dementia during passive relaxation, which was the case 60% of the time as background analysis revealed. It might have been difficult for the carer to relax in an adequate atmosphere when the care recipient expressed needs that interfered. Forty percent of the time, when the person living with dementia was absent, an internal dilemma could have occurred, including feelings of guilt, restriction, or dissatisfaction. The entitlement to leisure can be an intractable concept for carers, and the sense of obligation to the care recipient might make all leisure meaningless (Rogers, Citation2001). Bedim and Guinan (Citation1996) suggest that the sense of responsibility to the care recipient can outweigh the carer’s own personal and leisure needs. Furthermore, even though many carers express a desire for leisure, they may feel that leisure is not doable while embodying their helping roles. Some carers might suppress their desire for leisure or feel frustrated over the inability to access leisure satisfactorily, while others might include the care recipient into leisure activities, or find a way to pursue leisure activities by justifying it as important to fulfil the caregiving role (Bedim & Guinan, Citation1996).
Unfortunately, leisure activities offered for both the carer and person living with dementia together are rarely available, leading to social injustice (Fortune & McKeown, Citation2016). This lack of external offers can further complicate efforts to combine caregiving and own leisure. The dilemmas illustrated might indicate that carers experience it as difficult to act on the advice from healthcare professionals to ‘take care’, which could be generally beneficial. The need to support the dyad by offering a friendly and normalised social context remains; in this regard, Meeting Centre Support Programs, which have been proven to substantially benefit the carers and person with dementia, should be promoted (Szcześniak et al., Citation2018, Citation2019).
In summary, both external and internal barriers could explain the feelings experienced by the carers in the present study, namely a strong decrease of NA and a simultaneously strong increase in activity-related stress when spending more time in passive relaxation. PA did not change significantly in relation to passive relaxation. Generally, ESM data are known to describe complex pictures of feelings, and PA and NA can change disproportionally, as they can be seen as two separable constructs rather than two extremes of a binary continuum (Diener & Emmons, Citation1984). In the elderly, experiencing both PA and NA simultaneously could be an indicator for a typical or adaptive emotional state in a stressful situation (Scott, Sliwinski, Mogle, & Almeida, Citation2014). Future interventions need to keep individual factors, such as leisure type, age, personality, and other external and internal barriers in mind when promoting leisure to carers.
In the present study, the process of behavioural change was complex and stressful for the carers, but overall the ‘Partner in Sight’ program led to positive intervention effects, such as a retrospectively measured decrease in perceived stress and an increase in the sense of competence, as well as ESM-measured decrease of NA (van Knippenberg et al., Citation2018). Moreover, the present study showed that the ESM-measured activity-related stress generally decreased throughout the intervention. This finding suggests that, while the process of change was stressful, more leisure itself can be stress-releasing.
Personalized feedback promoting behavioural change in carers
For carers of people with dementia, the personalized feedback focusing on PA and daily activities seems crucial in their behavioural change process as only the experimental group reported a change. illustrates the intervention mechanisms as suggested in change pathways: (digital) self-monitoring of daily functioning led to increased attention to and awareness of own emotions and behaviours. This awareness directly promotes an emotional change as both the pseudo-experimental and the experimental group showed a decrease in retrospectively measured perceived stress, an increase in the sense of competence, and a decrease in ESM-measured NA as shown in the RCT (van Knippenberg et al., Citation2018).
Only when the awareness gained through the self-monitoring was combined with personalized feedback focusing concretely on daily activities that elicit PA, a change in behaviour could be promoted in the participating carers. This finding is contrary to a study with a similar setup for outpatients with depression, in which both intervention groups with and without personalized feedback reported a behavioural change (Snippe et al., Citation2016). Potentially, the personalized feedback gave a concrete impulse and increased the carer’s motivation to adapt the current situation. The behaviour change process was then challenging but resulted in increased engagement in enjoyable activities. However, carers in this study only engaged more in one activity. Eventually, more frequent personalized feedbacks could have achieved a greater behavioural change. In the mentioned intervention for patients with depression, participants received weekly personalized feedback and changes in multiple activities could be observed (Snippe et al., Citation2016). While carers of people with dementia also experience depressive symptoms (Cuijpers, Citation2005), their circumstances are likely to be different from the circumstances of patients with depression. Nevertheless, weekly personal feedback may be useful for carers and could also improve the sustainability of intervention effects (Bartels et al., Citation2020).
There are a great number of theories attempting to explain behavioural change (Davis, Campbell, Hildon, Hobbs, & Michie, Citation2015). However, none of these theories focus specifically on spousal carers of people with dementia. Raising awareness for PA and related behaviours through self-monitoring and feedback could be a key factor and mechanism to support coping in this population as illustrated in the change pathways. Future research is needed to follow-up on additional needs carers might have and explore the optimal amount of personalized feedback to achieve sustained coping during caregiving.
Methodological considerations
The uniqueness of this study is characterized by the in-depth assessment of carers’ everyday life before, during, and after an intervention. However, there are also general limitations to this study. First, the issue of reactivity should be considered when interpreting the results of ESM studies. The randomized time schedule was chosen to desensitize carers to the momentary assessments, and thus, minimize the risk for negative reactivity and preparation for completing the ESM questionnaire (Palmier-Claus et al., Citation2011). Nevertheless, it is acknowledged that repeated measures can lead to unusual attention to ones’ internal states and behaviour (Scollon, Prieto, & Diener, Citation2009). Second, the directionality of the relationship between behaviour, affect, and stress remains unclear. It is not possible to conclude from the present findings if behaviour influences feelings or vice versa. Furthermore, ESM-data collection daily over the six-week program would have allowed for an even better depiction of everyday experiences in carers. This, however, could have been too burdensome for the participants, and thus, the decision was made for only three days of sampling per week. The adherence seems to already decrease over the course of the intervention, which supports the choice for the present study design. Additionally, we acknowledge the potential selection bias during recruitment as only carers who experienced low- to medium-burden might have participated, limiting the generalisation of our results. Finally, despite the 8488 valid ESM beeps, the sample size within each group was smaller than in a comparable secondary analysis (Snippe et al., Citation2016). Thus, a replication of the study might be advisable, including a greater sample size (>30 participants per group) and carers facing a higher level of burden.
Conclusion
This study describes the complex picture of carer’s everyday life and elaborates on the intervention mechanisms of the ‘Partner in Sight’ intervention. An ESM-intervention in combination with personalized feedback focusing on daily activities that elicit positive emotions can enable a behavioural change towards more passive relaxation. This behavioural change process, however, is accompanied by mixed feelings. Clinicians and researchers are advised to keep the complexity of the situation in mind when suggesting more self-care and leisure to dementia carers to improve their well-being. Personal contact is highly recommended to support carers in their daily tasks. Adapting one’s daily activities while providing care for a relative living with dementia seems to be complex and challenging, just like caregiving itself.
Authors’ Contributions
S. L. Bartels conducted the analysis, interpreted the results, and wrote the manuscript. R. J. M. van Knippenberg led the planning and execution of the ‘Partner in Sight’ intervention, supported the analysis, and provided feedback on the manuscript. W. Viechtbauer and C. J. P assisted the analysis with their statistical expertise of analysing momentary data and reviewed the manuscript. R. W. Ponds and I. Myin-Germeys were involved in the design of the intervention and provided feedback on the manuscript. F. R. J. Verhey and M. E. de Vugt were part of the design, analysis, writing, and acquisition of funding.
Acknowledgements
Thanks goes to all the participants taking part in the ‘Partner in Sight’ intervention as well as Inge Klinkenberg, Michelle Joosten, Susanne Meuwissen, and Leonie Banning for their support during the data collection.
Disclosure statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data availability statement
The data is stored at Maastricht University. Due to ethical and legal regulations, the data is only accessible for the MUMC + research team. Sharing data with another research team needs to be approved by the Medical Research Ethics Committee azM/UM or participants need to sign a new informed consent sheet.
Additional information
Funding
References
- Acton, G. J. (2002). Health-promoting self-care in family caregivers. Western Journal of Nursing Research, 24(1), 73–86. doi:https://doi.org/10.1177/01939450222045716
- Argüelles, S., & von Simson, A. (2001). Innovative family and technological interventions for encouraging leisure activities in caregivers of persons with Alzheimer's disease. Activities, Adaptation & Aging, 24, 83–97.
- Bartels, S. L., van Knippenberg, R. J., Köhler, S., Ponds, R. W., Myin-Germeys, I., Verhey, F. R., & de Vugt, M. E. (2020). The necessity for sustainable intervention effects: Lessons-learned from an experience sampling intervention for spousal carers of people with dementia. Aging & Mental Health, 24, 2082–2011. doi:https://doi.org/10.1080/13607863.2019.1647130
- Bedim, L. A., & Guinan, D. M. (1996). If I could just be selfish…: Caregivers’ perceptions of their entitlement to leisure. Leisure Sciences, 18, 227–239. doi:https://doi.org/10.1080/01490409609513284
- Caldwell, L. L. (2005). Leisure and health: Why is leisure therapeutic? British Journal of Guidance & Counselling, 33(1), 7–26.
- Chattillion, E. A., Mausbach, B. T., Roepke, S. K., von Känel, R., Mills, P. J., Dimsdale, J. E., … Grant, I. (2012). Leisure activities, caregiving demands and catecholamine levels in dementia caregivers. Psychology & Health, 27, 1134–1149. doi:https://doi.org/10.1080/08870446.2011.637559
- Csikszentmihalyi, M., & Larson, R. (1987). Validity and reliability of the experience sampling method. The Journal of Nervous and Mental Disease, 175, 526–536.
- Cuijpers, P. (2005). Depressive disorders in caregivers of dementia patients: A systematic review. Aging & Mental Health, 9, 325–330. doi:https://doi.org/10.1080/13607860500090078
- Davis, R., Campbell, R., Hildon, Z., Hobbs, L., & Michie, S. (2015). Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychology Review, 9, 323–344. doi:https://doi.org/10.1080/17437199.2014.941722
- Diener, E., & Emmons, R. A. (1984). The independence of positive and negative affect. Journal of Personality and Social Psychology, 47, 1105–1117. doi:https://doi.org/10.1037//0022-3514.47.5.1105
- Dowling, G. A., Merrilees, J., Mastick, J., Chang, V. Y., Hubbard, E., & Moskowitz, J. T. (2014). Life enhancing activities for family caregivers of people with frontotemporal dementia. Alzheimer Disease and Associated Disorders, 28, 175–181. doi:https://doi.org/10.1097/WAD.0b013e3182a6b905
- Egan, K. J., Pinto-Bruno, A. C., Bighelli, I., Berg-Weger, M., Van Straten, A., Albanese, E., & Pot, A.-M. (2018). Online training and support programs designed to improve mental health and reduce burden among caregivers of people with dementia: A systematic review. Journal of the American Medical Directors Association, 19, 200–206.e1. doi:https://doi.org/10.1016/j.jamda.2017.10.023
- Folkman, S. (1997). Positive psychological state and coping with severe stress. Social Science & Medicine (1982), 45, 1207–1221. doi:https://doi.org/10.1016/S0277-9536(97)00040-3
- Folkman, S., & Moskowitz, J. T. (2000). Positive affect and the other side of coping. The American Psychologist, 55, 647–654. doi:https://doi.org/10.1037//0003-066x.55.6.647
- Fortune, D., & McKeown, J. (2016). Sharing the journey: Exploring a social leisure program for persons with dementia and their spouses. Leisure Sciences, 38, 373–387. doi:https://doi.org/10.1080/01490400.2016.1157776
- Fredman, L., Bertrand, R. M., Martire, L. M., Hochberg, M., & Harris, E. L. (2006). Leisure-time exercise and overall physical activity in older women caregivers and non-caregivers from the Caregiver-SOF study. Preventive Medicine, 43, 226–229. doi:https://doi.org/10.1016/j.ypmed.2006.04.009
- Fredrickson, B. L. (1998). What good are positive emotions? Review of General Psychology, 2, 300–319. doi:https://doi.org/10.1037/1089-2680.2.3.300
- Fredrickson, B. L. (2004). The broaden-and-build theory of positive emotions. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 359, 1367–1377. doi:https://doi.org/10.1098/rstb.2004.1512
- Fredrickson, B. L. (2013). Positive emotions broaden and build. In Advances in experimental social psychology (Vol. 47, pp. 1–53). Academic Press. https://doi.org/10.1016/B978-0-12-407236-7.00001-2
- Kramer, I., Simons, C. J. P., Hartmann, J. A., Menne-Lothmann, C., Viechtbauer, W., Peeters, F., … Wichers, M. (2014). A therapeutic application of the experience sampling method in the treatment of depression: A randomized controlled trial. World Psychiatry, 13(1), 68–77. doi:https://doi.org/10.1002/wps.20090
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping: New York, NY: Springer Publishing Company.
- Leitner, M. J., & Leitner, S. F. (2012). Leisure enhancement. Urbana, 51, 61801.
- Lund, D. A., Utz, R., Caserta, M. S., & Wright, S. D. (2009). Examining what caregivers do during respite time to make respite more effective. Journal of Applied Gerontology, 28(1), 109–131. doi:https://doi.org/10.1177/0733464808323448
- Marquez, D. X., Bustamante, E. E., Kozey-Keadle, S., Kraemer, J., & Carrion, I. (2012). Physical acitivity and psychosocial and mental health of older caregivers and non-caregivers. Geriatric Nursing, 33, 358–365. doi:https://doi.org/10.1016/j.gerinurse.2012.03.003
- Mausbach, B. T., Coon, D. W., Patterson, T. L., & Grant, I. (2008). Engagement in activities is associated with affective arousal in Alzheimer's caregivers: A preliminary examination of the temporal relations between activity and affect. Behavior Therapy, 39, 366–374. doi:https://doi.org/10.1016/j.beth.2007.10.002
- Myin‐Germeys, I., Kasanova, Z., Vaessen, T., Vachon, H., Kirtley, O., Viechtbauer, W., & Reininghaus, U. (2018). Experience sampling methodology in mental health research: New insights and technical developments. World Psychiatry, 17, 123–132.
- Palmier-Claus, J. E., Myin-Germeys, I., Barkus, E., Bentley, L., Udachina, A., Delespaul, P. A. E. G., … Dunn, G. (2011). Experience sampling research in individuals with mental illness: Reflections and guidance. Acta Psychiatrica Scandinavica, 123(1), 12–20. doi:https://doi.org/10.1111/j.1600-0447.2010.01596.x
- Rogers, N. B. (2001). Family obligation, caregiving, and loss of leisure: The experiences of three caregivers. Activities, Adaptation & Aging, 24, 35–49.
- Schüz, B., Czerniawski, A., Davie, N., Miller, L., Quinn, M. G., King, C., … Scott, J. L. (2015). Leisure time activities and mental health in informal dementia caregivers. Applied Psychology. Health and Well-Being, 7, 230–248. doi:https://doi.org/10.1111/aphw.12046
- Scollon, C. N., Prieto, C.-K., & Diener, E. (2009). Experience sampling: Promises and pitfalls, strength and weaknesses. In Assessing well-being (pp. 157–180). Dordrecht: Springer.
- Scott, S. B., Sliwinski, M. J., Mogle, J. A., & Almeida, D. M. (2014). Age, stress, and emotional complexity: Results from two studies of daily experiences. Psychology and Aging, 29, 577–587. doi:https://doi.org/10.1037/a0037282
- Shiffman, S., & Stone, A. A. (1998). Introduction to the special section: Ecological momentary assessment in health psychology. Health Psychology, 17(1), 3–5. doi:https://doi.org/10.1037/h0092706
- Snippe, E., Simons, C. J. P., Hartmann, J. A., Menne-Lothmann, C., Kramer, I., Booij, S. H., … Wichers, M. (2016). Change in daily life behaviors and depression: Within-person and between-person associations. Health Psychology , 35, 433–441. doi:https://doi.org/10.1037/hea0000312
- Szcześniak, D., Dröes, R. M., Meiland, F., Brooker, D., Farina, E., Chattat, R., … Rymaszewska, J. (2018). Does the community-based combined Meeting Center Support Programme (MCSP) make the pathway to day-care activities easier for people living with dementia? A comparison before and after implementation of MCSP in three European countries. International Psychogeriatrics, 30, 1717–1734. doi:https://doi.org/10.1017/S1041610217002885
- Szcześniak, D., Rymaszewska, J., Saibene, F. L., Lion, K. M., D’arma, A., Brooker, D., … Meiland, F. (2019). Meeting centres support programme highly appreciated by people with dementia and carers: A European cross-country evaluation. Aging & Mental Health, 1–11.
- Vaessen, T., Kasanova, Z., Hernaus, D., Lataster, J., Collip, D., van Nierop, M., & Myin-Germeys, I. (2018). Overall cortisol, diurnal slope, and stress reactivity in psychosis: An experience sampling approach. Psychoneuroendocrinology, 96, 61–68. doi:https://doi.org/10.1016/j.psyneuen.2018.06.007
- van Knippenberg, R. J. M., de Vugt, M. E., Ponds, R. W., Myin-Germeys, I., Van Twillert, B., & Verhey, F. R. J. (2017). Dealing with daily challenges in dementia (deal-id study): An experience sampling study to assess caregiver functioning in the flow of daily life. International Journal of Geriatric Psychiarty, 32(9), 949–958.
- van Knippenberg, R. J. M., de Vugt, M. E., Ponds, R. W., Myin-Germeys, I., & Verhey, F. R. J. (2016). Dealing with daily challenges in dementia (deal-id study): Effectiveness of the experience sampling method intervention 'Partner in Sight' for spousal caregivers of people with dementia: Design of a randomized controlled trial. BMC Psychiatry, 16, 136. doi:https://doi.org/10.1186/s12888-016-0834-5
- van Knippenberg, R. J. M., de Vugt, M. E., Ponds, R. W., Myin-Germeys, I., & Verhey, F. R. J. (2018). An experience sampling method intervention for dementia caregivers: Results of a randomized controlled trial. The American Journal of Geriatric Psychiatry, 26, 1231–1243.
- Verhagen, S. J. W., Hasmi, L., Drukker, M., Van Os, J., & Delespaul, P. E. G. (2016). Use of the experience sampling method in the context of clinical trials. Evidence Based Mental Health, 19, 86–89. doi:https://doi.org/10.1136/ebmental-2016-102418
- Waller, A., Dilworth, S., Mansfield, E., & Sanson-Fisher, R. (2017). Computer and telephone delivered interventions to support caregivers of people with dementia: A systematic review of research output and quality. BMC Geriatrics, 17(1), 265. doi:https://doi.org/10.1186/s12877-017-0654-6
- Wang, C.-L., Shyu, Y.-I. L., Wang, J.-Y., & Lu, C.-H. (2017). Progressive compensatory symbiosis: Spouse caregiver experiences of caring for persons with dementia in Taiwan. Aging Ment Health, 21, 241–252. doi:https://doi.org/10.1080/13607863.2015.1081148
Appendix
Figure A1. Examples of ESM-based feedback graphs. (a) Amount of time spend doing different types of activities; (b) Amount of positive affect experienced per type of activity; (c) Mean level of positive affect over the six-week intervention period. Note: (a) and (b) were provide every two weeks. Note: This graph has previously been published in Bartels et al. (Citation2020). The necessity for sustainable intervention effects: lessons-learned from an experience sampling intervention for spousal carers of people with dementia. Aging & mental health, pp. 1–11.
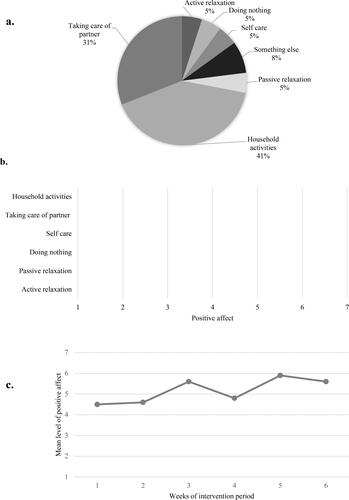
Figure 1. ‘Partner in Sight’ intervention elements per group focusing on the experience sampling method assessments.
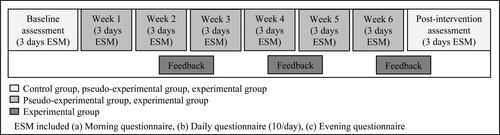
Figure 2. Intervention mechanisms explained through change pathways (based on the ‘Partner in Sight’ intervention elements for spousal carers of people with dementia). 1Findings from RCT; 2Findings from present study.
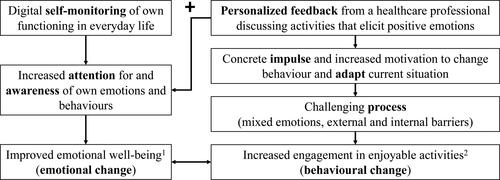
Table 1. Reliability of the repeated measures across all groups.
Table 2. Carers’ daily behaviours, PA, NA, and activity-related stress at baseline and post-intervention.
Table 3. The effect of time (dummy variable for baseline/post-intervention) on behaviours (frequency per day) for the ESM intervention groups compared with the control group (reference group).
Table 4. Associations between behaviours and affect as well as activity-related stress.
