Abstract
Objective
Few studies have examined lockdown effects on the way of living and well-being of older adults stratified by cognitive state. Since cognitive deficits are common in this population, we investigated how cognition influenced their understanding of the pandemic, socio-behavioral responses and lifestyle adaptations during lockdown, and how these factors affected their mood or memory.
Method
Telephone-based survey involving 204 older adults ≥65 y/o (median: 82) with previous assessments of cognitive state: 164 normal-old (NOLD), 24 mild-neurocognitive disorder (mild-NCD), 18 mild-moderate dementia. A structured questionnaire was developed to assess psychological and socio-behavioral variables. Logistic regression was used to ascertain their effects on mood and memory.
Results
With increasing cognitive deficits, understanding of the pandemic and the ability to follow lockdown policies, adapt to lifestyle changes, and maintain remote interactions decreased. Participants with dementia were more depressed; NOLDs remained physically and mentally active but were more bored and anxious. Sleeping and health problems independently increased the likelihood of depression (OR: 2.29; CI: 1.06–4.93; p = 0.034 and OR: 2.45; CI: 1.16–5.16; p = 0.018, respectively); Regular exercise was protective (OR: 0.30; CI: 0.12–0.72; p = 0.007). Worsening subjective memory complaints were associated with dementia (p = 0.006) and depression (p = 0.004); New-onset sleeping problems raised their odds (OR: 10.26; CI: 1.13–93.41; p = 0.039). Finally, >40% with health problems avoided healthcare mainly due to fear of contagion.
Discussion
NOLD and mild-NCD groups showed similar mood-behavioral profiles suggesting better tolerance of lockdown. Those with dementia were unable to adapt and suffered from depression and cognitive complaints. To counteract lockdown effects, physical and mental activities and digital literacy should be encouraged.
Introduction and historical background
Our history is highly influenced by the many infectious diseases that have scourged civilizations throughout time. Among the oldest and most effective preventive measures were isolation and quarantine. ‘Isolation’ is the separation of sick subjects to prevent contagion of healthy individuals, while ‘quarantine’ refers to the restriction of movement of suspected transmitters before symptoms could appear (Gensini, Yacoub, & Conti, Citation2004; Wilder-Smith & Freedman, Citation2020).
Isolation was a commonly used measure with leprosy, a chronic progressive disease (McNeill, Citation1976). The Book of Leviticus in the Old Testament contained one of the oldest evidence of laws regarding the diagnosis, separation, and purification of lepers (McEwen, Citation1911). A more strategic isolation of lepers began in 4th century AD Europe with the construction of numerous Lazzaretti or leper houses (Cosmacini, Citation2014; McNeill, Citation1976). These lazzaretti also isolated plague victims, but since plague was an acute and frequently fatal disease, measures to limit movement of potentially-infected individuals were further taken, especially following the Black Death caused by Yersinia pestis (1347) (McNeill, Citation1976). By 1377, Ragusa (modern-day Dubrovnik) pioneered a 30-day period in which ships arriving from plague-endemic areas were forced to wait before docking (Gensini et al., Citation2004; Sehdev, Citation2002; Stuard, Citation1992). Venice later improved this strategy by transforming the island of Lazzaretto into a confinement station for incoming maritime travelers (Gensini et al., Citation2004). The initial one-month period was extended to 40 days, probably to reflect religious or biblical occurrences, thus giving rise to the present-day quarantine (from the Italian word quaranta, meaning ‘forty’) (Gensini et al., Citation2004; Sehdev, Citation2002).
The rise of modern medicine in the late 1800s resulted in innovative treatments, and isolation and quarantine were then considered obsolete measures (Tognotti, Citation2013). Nonetheless, when the Spanish flu began in 1918, war-torn countries struggled to reimplement them (Tognotti, Citation2013). With censorship limiting information to avoid creating panic, it was too late when local authorities started using containment strategies like closing schools, churches, and theaters; banning gatherings; and restricting travel (Tognotti, Citation2013). Overall, most attempts to thwart viral transmission failed and the Spanish flu spread globally, killing at least 20 million people, primarily young and healthy adults (McNeill, Citation1976).
An infectious disease outbreak on a global scale had not been witnessed for over a century until the recent emergence of the Coronavirus Disease 19 (COVID-19) pandemic. Contemporary healthcare systems were caught unprepared for the first time and governments were once more forced to resort to, and even magnify, apparently-outdated segregation methods to limit disease transmission in anticipation of a cure or vaccine. A new politically-enforced, medically-encouraged preventive measure was introduced to limit viral transmission—the ‘lockdown’. Unlike in the past when quarantine was localized and limited in time, lockdown involved mandatory home segregation of not only suspected transmitters but the entire population of a region or country for an undefined period of time, made possible through social conditioning and mass surveillance. Thus, lockdown could be considered an extreme and radical version of quarantine.
Italy was the second country to impose a total nationwide lockdown from March 9 to May 3, 2020. People were strictly prohibited from leaving their homes except for work or health reasons or necessities like grocery shopping. The country started easing restrictions on May 4, 2020 with the beginning of the so-called ‘Phase 2’.
Lockdown decreased COVID-19 incidence and mortality rates when implemented promptly (Nussbaumer-Streit et al., Citation2020)—but this benefit came at a price: a considerable psychological impact (Brooks et al., Citation2020). The psychological effects of isolation and quarantine were oftentimes overlooked, and historical documents failed to report their existence. In the last 20 years, a number of studies recently reviewed (Brooks et al., Citation2020) reported detrimental psychological effects of quarantine, including depression and post-traumatic stress disorder triggered by smaller epidemics.
In older adults, COVID-19 has increased severity, morbidity and mortality (Lithander et al., Citation2020; L. Wang, Pan, et al., Citation2020). A shift in distribution of the world’s population toward older ages is present nowadays, (World Health Organization, Citation2018) and about 23% of Italy’s population is now constituted by older adults aged 65 and above (Onder, Rezza, & Brusaferro, Citation2020). In addition to this, the psychological effects of quarantine are more likely to occur in this older population (Qiu et al., Citation2020; C. Wang, Pan, et al., Citation2020), and since multiple comorbidities are also more common, the decreased access to healthcare facilities observed recently due to fear of contracting COVID-19 (Morelli et al., Citation2020; Poloni et al., Citation2020) poses a great threat. Many studies report the severity of COVID-19 in older adults, but only few online surveys address how this population has comprehended, endured and behaved during lockdown (Barber & Kim, Citation2020; García-Portilla et al., Citation2020; Lopez et al., Citation2020; Losada-Baltar et al., Citation2020). Studies comparing how older adults with different cognitive states reacted are scarce.
Older adults are frequently affected by cognitive problems. We hypothesize different behavioral, psychological, and lifestyle profiles during lockdown based on diverse cognitive states. Specifically, we aim to: (1) investigate how the cognitive state influenced the acquisition of information and understanding of COVID-19 pandemic and lockdown, compliance with lockdown policies and socio-behavioral responses, lifestyle, mood, memory and general health; (2) verify how socio-behavioral responses, general health and lifestyle factors affected mood or memory, and identify any risk or protective factors; and, finally, (3) report the frequency of healthcare avoidance due to fear of contracting COVID-19.
Methods
Study design and setting
This is a cross-sectional telephone-based survey conducted at the Abbiategrasso Brain Bank (ABB)(Poloni et al., Citation2020) and the Golgi-Redaelli Geriatric Hospital Memory Clinic (MC) between April 9, 2020, one month after the implementation of lockdown, and May 4, 2020, the day of transition to ‘phase 2’. Trained professionals conducted the interviews, which had a concomitant aim of ensuring the participants’ general health and of providing medical counseling whenever possible. This study was performed in accordance with the principles outlined in the Declaration of Helsinki of 1964, including all amendments and revisions. Although each ABB donor and MC patient had beforehand signed a consent form for collection and processing of sensitive personal data intended for medical purposes and research, informed verbal consent was nonetheless sought at the beginning of each interview.
Participants
Our participants belonged to a specific population, including ABB brain donors and long-term MC patients with a previously scheduled check-up during the study period that was postponed due to lockdown; all with no history of major depression or other psychiatric illnesses, or any recent (<6 months) acute exacerbation of a chronic disease or hospitalization. The inclusion criteria consisted of being ≥65 years old and having an existing assessment of cognitive functions. The only exclusion criterion was the presence of severe dementia.
Variables and data collection
Information about baseline cognitive state was available in medical records. Cognitive impairment was defined using the DSM-5 criteria (American Psychiatric Association, Citation2013). Mild- and major-neurocognitive disorder (NCD) were differentiated based on the presence or absence of independent functioning, respectively. Older adults who did not meet these criteria were considered NOLD (normal old). The severity of cognitive and functional deficits was assessed using the 5-point Clinical Dementia Rating (CDR)(Hughes, Berg, Danziger, Coben, & Martin, Citation1982) scale. An overall CDR score was assigned, where CDR 1, 2, and 3 represented mild, moderate and severe dementia (major-NCD), respectively.
We devised a structured questionnaire to determine the ability to acquire information, comprehend the COVID-19 pandemic and lockdown, and comply with lockdown policies; the socio-behavioral responses to the health crisis; and any changes in lifestyle, involving diet, exercise, sleep and digital literacy. Digital literacy was assessed through the use of internet for communication, information and/or leisure. We used the short form of Geriatric Depression Scale (GDS)-5 (Rinaldi et al., Citation2003; Yesavage, Citation1988) to assess the possibility of depression, assigning 1 point each for (1) dissatisfaction with life, (2) boredom, (3) feeling helpless, (4) preference to stay indoors rather than going out and trying new activities and (5) feeling worthless. A GDS-5 score of ≥2 suggested significant depressive symptoms. Each participant was also asked about subjective memory complaints (SMC) and possible worsening during lockdown. Finally, we inquired about any health problems experienced during lockdown and asked if medical assistance was requested or avoided. Specific interview questions are found in and .
Table 1. Demographics, clinical characteristics and lifestyle of participants stratified by cognitive state (NOLD, Mild-NCD, dementia).
Data analysis
Participants were grouped according to the baseline cognitive state (i.e. NOLD, mild-NCD, dementia), mood ( not depressed or depressed), and SMC (unchanged or worsened). Categorical variables were presented as counts and percentages and analyzed using Chi-square test or Fisher's exact test where appropriate. Continuous variables with skewed distribution were shown as median (Q1, Q3) and analyzed using Kruskal-Wallis. Logistic regression was performed to ascertain the effects of age, dementia, exercise, new hobbies, digital literacy, sleep disturbances, and general health problems on the likelihood of participants having depression or worsening SMC. A p-value of <0.05 was considered significant. Adjusted standardized residuals (z-score) was used as a post-hoc analysis for Chi-square test involving variables with 3 categories, with cells with z-scores larger than 1.96 considered statistically significant. For all statistical analyses, IBM SPSS version 26 was used.
Results
Participants and overall descriptive data
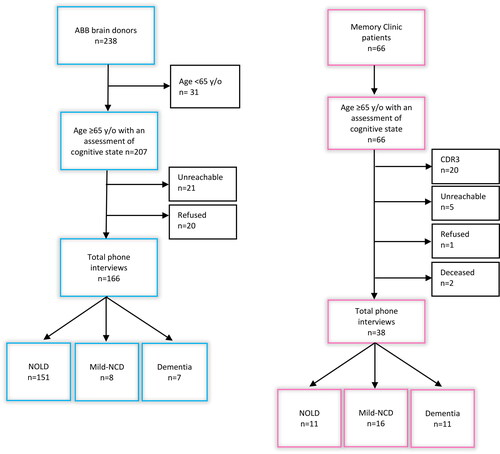
Among the 238 ABB donors, 207 were eligible for inclusion and 41 were excluded (21 unreachable, 20 refused). All 66 MC patients were eligible but 28 were excluded (20 with CDR3-dementia, 6 non-respondents, 2 deceased) (). The main reason for declining was difficulty communicating by phone. The inability to use speech reading when talking on the phone prevented participants with hearing loss from communicating effectively. Family members or caregivers acted as an intermediary in such cases. Similarly, they helped explain survey questions to some participants with moderate dementia. A total of 204 participants were interviewed: 166 (81.4%) ABB donors and 38 (18.6%) MC patients. The median age was 82 y, with the majority belonging to the 70–79 (24.0%) and 80–89 (64.2%) age groups. Females constituted 57.4% (117/204).
Main results
1. Influence of cognitive state on daily life during COVID-19 pandemic
Overall, 162/204 (79.4%) were NOLDs, 24/204 (11.7%) had mild-NCD, and 18/204 (8.8%) had mild to moderate dementia (CDR 1–2), . More than 90% of NOLDs were donors and ∼60% were females. The mild-NCD group was predominantly male (66.7%) and those with dementia were mostly females (55.6%). Based on the cognitive state, three distinct socio-behavioral profiles were observed ().
Figure 2. Socio-behavioral responses, mood and lifestyle of participants grouped based on their cognitive state.
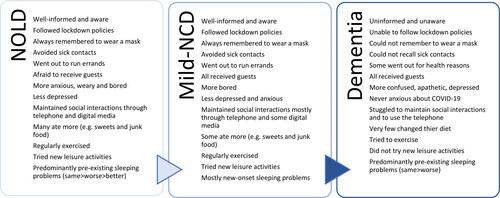
Information acquisition and COVID-19 comprehension
Understanding the unfolding health crisis greatly depended on the participants’ cognitive state. When asked if well-informed and aware of the COVID-19 pandemic and lockdown, 188/203 (92.6%) responded positively (). This decreased with increasing cognitive deficits (NOLD: 99.4%, mild-NCD: 95.8%, dementia: 27.8%; p < 0.001). The NOLD and mild-NCD groups were more able to follow the news than those with dementia (96.9% and 91.7% vs 55.6%, respectively; p < 0.001). Television was the number one source of information for >95% of all subjects. Reading online newspaper was associated almost only with normal cognition (p = 0.012). The frequency with which participants followed the news correlated with their cognitive state (p < 0.001), with NOLDs tuning in on the news constantly and those with dementia almost never. Finally, 50% (9/18) of those with dementia could not recall if they had been exposed to people with flu-like symptoms (p < 0.001); All who recounted having sick contacts were NOLDs.
Socio-behavioral response
Comprehension of the pandemic led to compliance with the stay-at-home order and adequate socio-behavioral responses. During lockdown, 114/204 (55.9%) left their homes to run important errands—most were NOLDs or with mild-NCD (p = 0.028). More than 90% of these two groups always remembered to wear a mask, in opposition to the 40% of those with dementia (p = 0.008), who incidentally remained at home for the most part. Everyone with cognitive impairment received guests, while NOLDs were more anxious about welcoming people to their homes. The use of masks in this situation was again most common among the latter (NOLD: 70.1%, mild-NCD: 62.5%, dementia: 16.7%; p ≤ 0.001). Ten participants never left their homes nor received guests. Social interactions were maintained through the use of telephone and digital media. Keeping in touch with loved ones was most common among NOLDs and least frequent among those with dementia (p < 0.001)
Lifestyle: diet, exercise, sleep and digital literacy
Alterations in eating habits were declared by 72/204 (35.3%). Those with dementia typically maintained their normal eating habits, while the mild-NCD and NOLD groups ate more (25.0% and 21.6%, respectively), especially sweets and snacks, whenever feeling bored or stressed. Many of those who ate less, whether secondary to a poor appetite or fear of gaining weight owing to a more sedentary lifestyle, were NOLDs.
During lockdown, the majority of our older adults strived to be physically and mentally active. Regular exercise decreased with increasing cognitive deficits (NOLD: 84.6%, mild-NCD: 79.2%, dementia: 61.1%; p = 0.054). Walking exercises at home were enjoyed by all groups and were the preferred type of exercise by those with dementia (90.9%). The use of stationary bike was most prominent in the mild-NCD group (42.1%). Stretching and postural exercises were mostly associated with NOLDs. Trying new activities was associated with the cognitive state (p < 0.001); it was only found in the NOLD (66.7%) and mild-NCD (41.7%) groups. These included cooking, baking, reading, sewing or knitting, and doing household chores for the women, and playing with cards, solving crossword puzzles, gardening and home maintenance for the men.
Almost 50% (99/204) reported sleeping problems. More than 80% of the sleeping problems in the dementia and NOLD groups were pre-existing (9/11 and 70/79, respectively), which chiefly remained unchanged during lockdown. Older adults with mild-NCD were more likely to report new-onset sleeping problems (p = 0.007). Interestingly, 4/70 (5.7%) NOLDs communicated better sleep.
Unsurprisingly, advanced internet skills used for communication (e.g. use of messaging apps and video conferencing platforms), information (e.g. online newspapers and live news stream), and leisure (e.g. watching videos and playing games) were associated mostly with normal cognition (p > 0.001).
Mood and memory
The 5-item GDS was completed by 198/204 (). The median score was 1, chiefly indicating the absence of significant depressive symptoms. GDS ≥ 2 suggesting current depression was seen in 50/198 (25.3%). Boredom (31.5%), worthlessness (24.2%), and preferring to stay at home regardless of lockdown (19.5%) were most common. Depression was found to be significantly associated with the cognitive state, with 61.5% of those with dementia scoring ≥ 2 in GDS-5 as opposed to the 22.4% of NOLDs (p = 0.008).
Pre-existing SMC were reported by 121/204 (59.3%). Over 50% of NOLDs also recounted subjective decline. During lockdown, 55/121 (45.5%) experienced further worsening. This was most common in those with dementia (76.5%), followed by those with mild-NCD (56.3) and lastly by NOLDs (37.5%), (p = 0.008) ().
General health
There were no significant differences in the frequencies of health problems and of seeking medical help among the cognitive groups, although all those with mild-NCD and health issues asked for medical assistance.
2. Effects of socio-behavioral responses, lifestyle changes and general health on mood and memory
Depression
As described in , depression was significantly associated with: (a) frequency of tuning in on the news – those who checked the news once a day showed less signs of depression, while those who monitored them more frequently and those who never or rarely did so tended to be more depressed (p < 0.001); (b) social interactions with loved ones – social interactions through telephone and digital media were less common in the depressed than non-depressed group (94.0% vs 99.3%, p = 0.050); (c) regular exercise – participants who were not physically active had a greater propensity for depression than those who regularly exercised (30.0% vs 11.2%, p = 0.002); (d) finding new hobbies – new activities were found in two-thirds (95/148) of non-depressed participants and in <50% of depressed subjects (22/50) (p = 0.017); (e) sleeping problems – terrible nightmares were more common in those with depression (23.3% vs 4.5%, p = 0.009); (f) digital literacy – the ability to use the internet was more common in those without depression (32.4% vs 16.9%, p = 0.026); and (g) health problems – about 50% of those with depression also suffered from other health problems during lockdown compared to the 30.4% of those without depressive symptoms (p = 0.024). Using logistic regression and after controlling for other factors in the model, sleeping disturbances and general health problems were both found to independently increase the likelihood of depression (OR: 2.29; CI: 1.06–4.93; p = 0.034 and OR: 2.45; CI: 1.16–5.16; p = 0.018, respectively), while regular exercise was a protective factor decreasing its likelihood (OR: 0.30; CI: 0.12–0.72; p = 0.007).
Table 2. Association between participants’ clinical, socio-behavioral and lifestyle factors and depression and subjective memory complaints.
Subjective memory complaints
Depressive symptoms were more common in those with worsening SMC (45.1% vs 20.0%, p = 0.004) (), and dementia increased the odds of worsening memory (OR: 24.9; CI: 1.79–347.00; p = 0.017). Regular exercise was associated with unchanged perception of memory; About 90% of those with stable SMC was physically active (p = 0.058). Lastly, the sole presence of sleeping problems did not correlate with changes in memory. However, new-onset sleeping problems were more numerous in those with worsened SMC (25.7% vs 6.1%; p = 0.028, ) and was discovered to independently and strongly increase its likelihood (OR: 10.26; CI: 1.13–93.41; p = 0.039).
3. General health and healthcare avoidance
During the 10-week lockdown, 72/204 (35.3%) suffered from health problems (). About 60% (43/72) chose to seek medical care, while the remaining ∼40% (29/72) did not, because of either fear of contracting COVID-19 in 17/29 (58.6%) or chronic illnesses that could be managed independently in 12/29 (41.4%). Many of those who avoided medical help suffered from musculoskeletal problems or anxiety, but some with more urgent problems such as accidental falls (n = 1), constant severe headache lasting days (n = 1), visual loss (n = 2) and severe odontalgia (n = 1) also never contacted their physicians. All those with prominent anxiety were NOLDs. Twelve participants developed symptoms suggestive of COVID-19, such as fever (n = 8), acute dry cough (n = 7), pharyngitis (n = 8), myalgia (n = 6), conjunctivitis (n = 4), anosmia (n = 1) and dysgeusia (n = 2), diarrhea and nausea (n = 4). Only 1/12 had a pharyngeal swab and eventually tested positive for SARS-CoV-2.
Table 3. Health problems during lockdown and how participants reacted.
Discussion
To the best of our knowledge, this is the first study describing how older adults representing all cognitive states (NOLD, with or without SMC; mild-NCD; and mild to moderate dementia) reacted to lockdown. Three distinct patterns of levels of comprehension, adaptive socio-behavioral response and lifestyle changes were found based on the participants’ cognitive state, . While the mood and behavioral profiles of those with normal cognition and mild cognitive impairment were fairly similar, the way of living of older adults with dementia during lockdown differed considerably. Our key findings include: (1) older adults with mild-moderate dementia were neither able to understand the severity of the health crisis nor recall and apply the necessary preventive measures; (2) people with mild-moderate dementia suffered most from depressive symptoms and worsening SMC, while cognitively-normal older adults experienced more boredom and anxiety; (3) less depression was associated with physical activity, especially in NOLDs, and with pursuit of new leisure activities, particularly among those with mild-NCD; (4) overall, sleep and general health problems both increased the likelihood of depression, while regular exercise was a protective factor; (5) digital literacy, most common in NOLDs, was associated with less depression; (6) depressive symptoms were common in those with worsened SMC; (7) new-onset sleeping problems increased the odds of worsening SMC; and (8) more than 40% of those who experienced health problems did not seek medical help mainly due to fear of contracting COVID-19.
Recent online surveys have investigated the influence of psychological well-being(Lopez et al., Citation2020) and worrying(Barber & Kim, Citation2020) on the behavior of older adults during the pandemic. A study conducted as early as after one week of lockdown in Spain revealed that older adults with positive self-perception of aging were more resilient and less distressed than younger adults (Losada-Baltar et al., Citation2020). A similar study showed analogous results (García-Portilla et al., Citation2020). Our research examined how the cognitive state had affected certain psychological and emotional responses, and consequently, behavior during lockdown, which in turn has impacted mood and memory. Contrary to others’ findings, we did find that psychological distress was frequent among older adults, especially those with dementia. It is possible that the abovementioned studies reported more resilience and less emotional and psychological distress because they included older adults able to use social media and other online platforms, and indeed our study showed that digital literacy, present in 1/3 of NOLDs and absent in those with dementia, was associated with less depression and better tolerance of lockdown.
A strength of this study is the use of telephone interviews instead of online surveys, which allowed us to involve older adults, with or without cognitive deficits. This more direct interaction and a long-term relationship built on trust enabled our participants to willingly partake in a telephone interview and provide reliable and detailed information about their psychological experiences and lifestyle. Also, our study period began one month after the implementation of lockdown, which allowed us to study not only the disruptions of daily living but also the adaptations that occurred. On the other hand, this study is limited by its small number of participants, particularly with neurocognitive disorders; the specific population taken into consideration; and the inability to conduct more precise and specific tests to define and compare depression or cognitive decline given the dire situation. The majority of our participants with major-NCD have either Alzheimer’s or mixed dementia (Alzheimer’s + vascular), but whether the underlying pathology influenced the response to lockdown was unclear because of the small sample size.
Participants with normal cognition and mild-NCD responded satisfactorily in general to both pandemic and lockdown. Contrarily, those with mild-moderate dementia suffered more from the restrictions as they endured feelings of helplessness and worthlessness, and depression, and were less able to cope with new and unfavorable circumstances. As dementia progresses, patients normally engage only in very basic and habitual daily activities. When these customary activities were partially disrupted, they were unable to adapt to the new circumstances and some degree of cognitive regression even occurred leading to confusion and apathy. The resulting perception of functional disability, whether conscious or not, could have triggered the depressive symptoms; depression was indeed found to herald functional disability in late life (Ormel, Rijsdijk, Sullivan, Van Sonderen, & Kempen, Citation2002). Concordant with previous reports (Asmer et al., Citation2018; Leyhe et al., Citation2017), we found that depression (GDS-5 ≥ 2) was strongly associated with dementia. According to literature, understanding the duration and meaning of restrictions, access to information, and the ability to communicate and do new activities were some of the factors which could potentially ease the negative consequences of quarantine (Brooks et al., Citation2020). As we know, these conditions hardly apply to patients with dementia making them more vulnerable. Since lockdown is the extremization of quarantine, escalation of the unwanted psychological effects could be expected.
Although NOLDs better tolerated lockdown, they also showed depressive symptoms and SMC. Perceived social isolation was previously named a risk factor for poorer global cognitive performance, faster cognitive decline, inferior executive functioning, and potentiation of mood, anxiety, and depressive symptomatology (Cacioppo & Hawkley, Citation2009). To counteract this feeling of social isolation, NOLDs and those with mild-NCD kept their body and mind active as they engaged in regular exercise and new hobbies. Indeed, NOLDs who exercised were significantly less depressed. The NOLD and mild-NCD groups also frequently left their homes to do groceries or run errands. Overall, physical activity decreased the likelihood of depressive symptoms by 70%, thereby acting as a protective factor. A previous study already recommended physical activity for protection from the mental and physical consequences of lockdown (Jiménez-Pavón, Carbonell-Baeza, & Lavie, Citation2020). This ability to adapt to new adverse situations probably had a beneficial role, as they were able to evade depression and even learned new skills.
The lack of knowledge about preventive measures caused massive confusion and contagion during past epidemics. Today, widespread dissemination of information regarding disease characteristics and health policies are easily provided to the general public through mass media to the point of sowing fear and panic. The resulting social conditioning together with concerns about criminal penalties increased compliance with COVID-19 containment measures. The majority of our elder participants were in fact well-informed and reacted appropriately except for those with dementia. Aside their use for information gathering, digital skills also probably decreased the sense of social isolation. We found that digital literacy, more common in NOLDs, was significantly associated with less depression. Video calls were considered a more decent substitute of face-to-face interactions than simple telephone calls, and online videos, movies and games were suitable for entertainment. Thus, internet use, online cognitive workshops, and digital games should be encouraged and advertised for older adults.
Participants from all groups reported eating more (21.1%), particularly sweets and snacks in response to boredom and stress and consequently gaining weight. A recent study revealed similar results (Zachary et al., Citation2020). Contrarily, others described eating less (14.2%), either because of concerns about gaining weight due to a more sedentary lifestyle or less appetite. Recent online surveys(Casagrande, Favieri, Tambelli, & Forte, Citation2020; Cellini, Canale, Mioni, & Costa, Citation2020) also reported sleeping problems caused by lockdown, but their cohort was made predominantly of young adults and they did not consider long-standing problems. Since disruptions in sleeping patterns are common in the elderly (Neubauer, Citation1999), we divided them into pre-existing and new-onset. Only recent-onset sleeping problems (16.2%) were associated with worsening SMC and nightmares were more common with depressive symptoms. Possible explanations for these new-onset sleeping disturbances could be anxiety and disruption of daily routines as many took daytime naps to fill the days.
Although lockdown protected those who strictly followed the stay-at-home order from COVID-19, it exposed them to other problems related to general physical health. Seventy-two participants experienced exacerbation of long-term musculoskeletal problems and other chronic illnesses, and even accidental falls. Because of fear of contracting the virus, many chose to endure pain instead of going to the general practitioner (GP)’s office. In contrast, those who developed fever or flu-like symptoms eagerly contacted their GPs, although to no avail given only 1/12 of these patients underwent a pharyngeal swab to confirm the infection. Participants revealed that GPs refrained from visiting patients with flu-like symptoms and merely prescribed antipyretics or analgesics by phone or advised to call the appropriate COVID-19 hotline.
The COVID-19 pandemic exposed deficiencies in Healthcare Systems which focus mainly on hospitals, neglecting Primary Care Medicine. The National Health System in Italy is responsible for providing equal access to welfare and uniform regional healthcare services (Remuzzi & Remuzzi, Citation2020). Primary care physicians (PCP), including GPs and Territory Medicine Physicians (out-of-hours GPs), are the gatekeeper to many medical resources and represent a fundamental defense against epidemics. During the peak of the outbreak, the lack of coordination among regional healthcare authorities, hospitals, rehabilitation centers and nursing homes enormously increased the workload expected from PCPs, who were coincidentally left without the appropriate means to protect themselves from exposure and to properly diagnose patients owing to the shortage of personal protective equipment and pharyngeal swabs, respectively. This resulted in both PCPs and patients feeling neglected and abandoned, and ultimately led to an increase in mortality in both parties, thereby forcing the government to heavily depend on lockdown. In case of another outbreak, a better coordination is necessary and PCPs should be able to rely on a team of paramedical personnel and possess adequate medical equipment (Ordine Ordine dei Medici di Brescia, Citation2020).
In conclusion, although lockdown helped contain the spread of COVID-19, it exposed older adults (especially those with dementia) to psychological disturbances, detrimental changes in sleeping-eating habits and lifestyle, and other health predicaments which usually went unreported and ignored. The resulting depressive symptoms and memory complaints can potentially persist over time and lead to major depression or worsening cognitive functions. Verification of these long-term effects would require further longitudinal studies. Moreover, older adults with dementia represent the most vulnerable population as they are unaware of the hazard and are unable to follow precautionary measures. Efforts should be made to prevent contagion especially in this population, and Primary Care Medicine should be reinforced for their protection. Regular physical activity, pursuit of new hobbies, and the use of digital gadgets (specially for social interactions) should also be encouraged. This initial experience of lockdown should be considered an eye-opener and a guide for future pandemics. Our mission should not merely focus on shielding our older adults from COVID-19, but also safeguarding them from the effects of lockdown including depression, cognitive decline and future consequences.
Acknowledgment
We would like to thank Valeria Marzagalli for her contribution, and our ABB donors and MC patients for their participation.
Disclosure statement
No potential competing interest was reported by the authors.
Data availability statement
The data supporting the findings of this study are available from the corresponding author, [A.F.C.], upon reasonable request.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC: American Psychiatric Publishing.
- Asmer, M. S., Kirkham, J., Newton, H., Ismail, Z., Elbayoumi, H., Leung, R. H., & Seitz, D. P. (2018). Meta-analysis of the prevalence of major depressive disorder among older adults with dementia. Journal of Clinical Psychiatry, 79(5),17r11772. doi:https://doi.org/10.4088/JCP.17r11772
- Barber, S. J., & Kim, H. (2020). COVID-19 worries and behavior changes in older and younger men and women. The Journals of Gerontology: Series B, 2020 May 19; gbaa068. doi:https://doi.org/10.1093/geronb/gbaa068
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). Rapid review: The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet, 395(10227), 912–920. doi:https://doi.org/10.1016/S0140-6736(20)30460-8
- Cacioppo, J. T., & Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13(10), 447–454. doi:https://doi.org/10.1016/j.tics.2009.06.005
- Casagrande, M., Favieri, F., Tambelli, R., & Forte, G. (2020). The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Medicine, 75, 12–20. doi:https://doi.org/10.1016/j.sleep.2020.05.011
- Cellini, N., Canale, N., Mioni, G., & Costa, S. (2020). Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. Journal of Sleep Research, 29(4), e13074. doi:https://doi.org/10.1111/jsr.13074
- Cosmacini, G. (2014). L’arte lunga: Storia della medicina dall’antichità a oggi (The long art: History of medicine from ancient times to today). Bari, Italy: Editori Laterza.
- García-Portilla, P., de la Fuente Tomás, L., Bobes-Bascarán, T., Jiménez Treviño, L., Zurrón Madera, P., Suárez Álvarez, M., … Bobes, J. (2020). Are older adults also at higher psychological risk from COVID-19? Aging and Mental Health, 2020 Sep 1:1-8. doi:https://doi.org/10.1080/13607863.2020.1805723 Epub ahead of print
- Gensini, G. F., Yacoub, M. H., & Conti, A. A. (2004). The concept of quarantine in history: From plague to SARS. The Journal of Infection, 49(4), 257–261. doi:https://doi.org/10.1016/j.jinf.2004.03.002
- Hughes, C. P., Berg, L., Danziger, W. L., Coben, L. A., & Martin, R. L. (1982). A new clinical scale for the staging of dementia. The British Journal of Psychiatry: The Journal of Mental Science, 140, 566–572. doi:https://doi.org/10.1192/bjp.140.6.566
- Jiménez-Pavón, D., Carbonell-Baeza, A., & Lavie, C. J. (2020). Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Progress in Cardiovascular Diseases, 63(3), 386–388. doi:https://doi.org/10.1016/j.pcad.2020.03.009
- Leyhe, T., Reynolds, C. F., Melcher, T., Linnemann, C., Klöppel, S., Blennow, K., … Hampel, H. (2017). A common challenge in older adults: Classification, overlap, and therapy of depression and dementia. In Alzheimer’s and Dementia, 13(1), 59-71. doi:https://doi.org/10.1016/j.jalz.2016.08.007
- Lithander, F. E., Neumann, S., Tenison, E., Lloyd, K., Welsh, T. J., Rodrigues, J. C. L., … Henderson, E. J. (2020). COVID-19 in older people: A rapid clinical review. Age and Ageing, 49(4), 501–515. doi:https://doi.org/10.1093/ageing/afaa093
- Lopez, J., Perez-Rojo, G., Noriega, C., Carretero, I., Velasco, C., Martinez-Huertas, J. A., … Galarraga, L. (2020). Psychological well-being among older adults during the Covid-19 outbreak: A comparative study of the young-old and the old-old adults. International Psychogeriatrics, 32(11), 1365–1370. doi:https://doi.org/10.1017/S1041610220000964
- Losada-Baltar, A., Jiménez-Gonzalo, L., Gallego-Alberto, L., Pedroso-Chaparro, M. D. S., Fernandes-Pires, J., & Márquez-González, M. (2020). We’re staying at home. Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lock-down period of COVID-19. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, gbaa048. doi:https://doi.org/10.1093/geronb/gbaa048
- McEwen, E. L. (1911). The leprosy of the bible in its medical aspect. In The Biblical world (Vol. 38, Issue 3, pp. 194–202). The University of Chicago Press. doi:https://doi.org/10.1086/474489
- McNeill, W. H. (1976). Plagues and peoples. Garden City, New York: Anchor Press/Doubleday.
- Morelli, N., Rota, E., Terracciano, C., Immovilli, P., Spallazzi, M., Colombi, D., … Guidetti, D. (2020). The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. European Neurology, 83(2), 213–215. doi:https://doi.org/10.1159/000507666
- Neubauer, D. N. (1999). Sleep problems in the elderly, 59(9), 2551-2558. American Family Physician.
- Nussbaumer-Streit, B., Mayr, V., Dobrescu, A. I., Chapman, A., Persad, E., Klerings, I., … Gartlehner, G. (2020). Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database of Systematic Reviews, 4(4), CD013574. doi:https://doi.org/10.1002/14651858.CD013574
- Onder, G., Rezza, G., & Brusaferro, S. (2020). Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA – Journal of the American Medical Association,323(18), 1775-1776 . doi:https://doi.org/10.1001/jama.2020.4683
- Ordine dei Medici di Brescia. (2020). La linea d’ ombra che abbiamo attraversato Noi e il Covid-19. (THE SHADOW LINE WE HAVE CROSSED. US AND COVID-19. Retrieved from https://www.ordinemedici.brescia.it/archivio39_brescia-medica_9_9297.html
- Ormel, J., Rijsdijk, F. V., Sullivan, M., Van Sonderen, E., & Kempen, G. I. J. M. (2002). Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 57(4), P338–P347. doi:https://doi.org/10.1093/geronb/57.4.p338
- Poloni, T. E., Medici, V., Carlos, A. F., Davin, A., Ceretti, A., Mangieri, M., … Guaita, A. (2020). Abbiategrasso brain bank protocol for collecting, processing and characterizing aging brains. Journal of Visualized Experiments, 160(160), e60296. doi:https://doi.org/10.3791/60296
- Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), e100213. doi:https://doi.org/10.1136/gpsych-2020-100213
- Remuzzi, A., & Remuzzi, G. (2020). COVID-19 and Italy: What next? The Lancet, 395(10231), 1225–1228. doi:https://doi.org/10.1016/S0140-6736(20)30627-9
- Rinaldi, P., Mecocci, P., Benedetti, C., Ercolani, S., Bregnocchi, M., Menculini, G., … Cherubini, A. (2003). Validation of the five-item Geriatric Depression Scale in elderly subjects in three different settings. Journal of the American Geriatrics Society, 51(5), 694–698. doi:https://doi.org/10.1034/j.1600-0579.2003.00216.x
- Sehdev, P. S. (2002). The origin of quarantine. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, 35(9), 1071–1072. doi:https://doi.org/10.1136/bmj.1.3564.790-a
- Stuard, S. M. (1992). A state of deference: Ragusa/Dubrovnik in the medieval centuries. Philadelphia, PA: University of Pennsylvania Press.
- Tognotti, E. (2013). Lessons from the history of quarantine, from plague to influenza A. Emerging Infectious Diseases, 19(2), 254–259. doi:https://doi.org/10.3201/eid1902.120312
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., … Ho, C. (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity, 87, 40–48. doi:https://doi.org/10.1016/j.bbi.2020.04.028
- Wang, L., He, W., Yu, X., Hu, D., Bao, M., Liu, H., … Jiang, H. (2020). Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. Journal of Infection, 80(6), 639–645. doi:https://doi.org/10.1016/j.jinf.2020.03.019
- Wilder-Smith, A., & Freedman, D. O. (2020). Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of Travel Medicine, 27(2), 1–4. doi:https://doi.org/10.1093/jtm/taaa020
- World Health Organization. (2018). Ageing and health. Retrieved from https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
- Yesavage, J. A. (1988). Geriatric Depression Scale. Psychopharmacology Bulletin, 24(4), 709–710. doi:https://doi.org/10.1007/978-3-319-69892-2_736-1.
- Zachary, Z., Brianna, F., Brianna, L., Garrett, P., Jade, W., Alyssa, D., & Mikayla, K. (2020). Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obesity Research and Clinical Practice, 14(3), 210-216 doi:https://doi.org/10.1016/j.orcp.2020.05.004