Abstract
Objectives
To examine prospectively the association between unmet needs for daytime activities and company and behavioural and psychological symptoms of dementia.
Methods
We included 451 people with mild or moderate dementia, from eight European countries, who were assessed three times over 12 months. Unmet needs were measured with the Camberwell Assessment of Need for the Elderly. Three sub-syndromes of the Neuropsychiatric Inventory-Questionnaire were regressed, one-by-one, against unmet needs for daytime activities and company, adjusting for demographic and clinical-functional covariates.
Results
Unmet needs for daytime activities were associated with more affective symptoms at baseline, six and twelve months, mean 0.74 (p < 0.001), 0.76 (p < 0.001) and 0.78 (p = 0.001) points higher score respectively, and with more psychotic symptoms at baseline (mean 0.39 points, p = 0.007) and at six months follow-up (mean 0.31 points, p = 0.006). Unmet needs for company were associated with more affective symptoms at baseline, six and twelve months, mean 0.44 (p = 0.033), 0.67 (p < 0.001) and 0.91 (p < 0.001) points higher score respectively, and with more psychotic symptoms at baseline (mean 0.40 points, p = 0.005) and at six months (mean 0.35 points, p = 0.002) follow-up.
Conclusion
Interventions to reduce unmet needs for daytime activities and company could reduce affective and psychotic symptoms in people with dementia.
Introduction
For people with dementia, thorough assessments of individual needs are important for efficiently delivering high-quality health and social services that are individually tailored (Curnow, Rush, Maciver, Gorska, & Forsyth, Citation2021; van der Roest et al., Citation2009). These assessments should include the perspective of the person with dementia, as his or her perceptions of unmet and met needs may differ from those of informal caregivers or health care professionals. Studies have shown that people with dementia generally report fewer unmet needs than researchers and their informal caregivers report them to have (Kerpershoek et al., Citation2018; van der Roest et al., Citation2009).
Studies investigating unmet needs in home-dwelling people with dementia by use of the widely used Camberwell Assessment of Need for the Elderly (CANE), found that daytime activities and company were two of the most commonly reported areas of unmet need (Mazurek et al., Citation2019; Miranda-Castillo et al., Citation2010; van der Roest et al., Citation2009). The item daytime activities include social, work, leisure and learning activities, and the item company is described as social contact. Other unmet needs frequently reported by people with dementia, as well as their caregivers, include needs related to memory problems, information and psychological distress (Curnow et al., Citation2021; Miranda-Castillo et al., Citation2010; van der Roest et al., Citation2009). In a large European cohort study including people with dementia from eight countries, daytime activities and company were again two of the items that both people with dementia and caregivers most frequently reported as unmet needs (Kerpershoek et al., Citation2018).
Identifying and seeking to meet unmet needs of people with dementia is important because unmet needs have been found to be associated with a lower health-related quality of life (Handels et al., Citation2018; Hoe, Hancock, Livingston, & Orrell, Citation2006; Janssen et al., Citation2018; Kerpershoek et al., Citation2018; Miranda-Castillo et al., Citation2010). Miranda-Castillo et al. (Citation2010) suggest that unmet needs mediate the relationship between behavioural and psychological symptoms of dementia (BPSD) and quality of life. BPSD is a term referring to a heterogeneous range of phenomena, considered to be highly prevalent and occur in the majority of people with dementia over the course of the disease (Kales, Gitlin, & Lyketsos, Citation2015). The term BPSD has lately been raised as controversial, and there is an ongoing discussion to find a more psychosocial term that reflects the multiple causes of behaviour in dementia care (Cunningham, Macfarlane, & Brodaty, Citation2019; Wolverson et al., Citation2019). Although we acknowledge the importance of this debate, we do not aim to take a stand in it. We have chosen to use the term BPSD in this manuscript, as this is the term most widely used in our references. BPSD have been cited as major risk factors for higher caregiver burden, greater functional impairment, more rapid cognitive decline, poorer quality of life and nursing home admission (Kales et al., Citation2015; Wergeland, Selbaek, Bergh, Soederhamn, & Kirkevold, Citation2015). The grouping of BPSD into sub-syndromes has been suggested as a more effective strategy for examining interventions than to report on each of the symptoms individually (van der Linde, Dening, Matthews, & Brayne, Citation2014). Symptom groups commonly used are affective symptoms, psychosis, hyperactivity and euphoria (van der Linde et al., Citation2014).
Unmet needs are widely considered to be one of the contributory factors of BPSD (Black et al., Citation2019; Cohen-Mansfield, Dakheel-Ali, Marx, Thein, & Regier, Citation2015; Cunningham et al., Citation2019; Kales et al., Citation2015). Many stakeholders in fact claim that BPSD are better considered as responses to unmet needs and suggest that the term ‘unmet needs’ might be used instead of BPSD (Wolverson et al., Citation2019). The links between unmet needs and BPSD may indicate that unmet needs should always be assessed, preferably with a standardised measure such as the CANE, in order to understand BPSD. These links may further indicate that meeting unmet needs should be a first choice to prevent and treat BPSD. From a research perspective, few studies have included a measurement of specific unmet needs when examining possible associations with BPSD in home-dwelling people with dementia. Thus, the aim of the current study was to examine prospectively over 12 months the association between unmet needs for daytime activities and company and the severity of different BPSD sub-syndromes.
Methods
The Access to Timely Formal Care (Actifcare) study was an EU Joint Programme – Neurodegenerative Disease Research (JPND) project where access to and uptake of formal community care services were explored in the following eight European countries: Germany, Ireland, Italy, the Netherlands, Norway, Portugal, Sweden and the United Kingdom. This study included data from the Actifcare prospective cohort study, a longitudinal study following people with dementia and their informal caregivers. Details about the Actifcare project and its cohort study can be found in the protocol paper (Kerpershoek et al., Citation2016).
Before the initiation of the cohort study, a joint training session for the data collectors from all eight countries was carried out in order to coordinate data collection and ensure consistency and a mutual understanding of how to complete the measures.
Participants
In the Actifcare study, 451 dyads of people with dementia and their informal caregivers were included at baseline. For the present study, only data describing the people with dementia, not the informal caregivers, were included. Inclusion criteria were being home-dwelling and having a diagnosis of mild to moderate dementia indicated by a Clinical Dementia Rating scale (CDR) score of 1 or 2 or a score on the Mini Mental State Examination (MMSE) of 24 or lower. To be included, the participants should not have been receiving formal personal care related to dementia at baseline but should be believed by a health care professional to require such care within one year. A subjective risk estimate was used to estimate need for additional assistance, based on available sources such as psychologists, general practitioners, memory clinic staff members and other health care or social care professionals. These sources differed between countries and participants depending on where the participants were recruited from. Data were collected at baseline, six and twelve months.
Measures
Outcome measure: BPSD (collected at baseline, six and twelve months)
BPSD were measured using the brief version of the Neuropsychiatric Inventory-Questionnaire (NPI-Q) addressing the severity of the following twelve symptoms: delusions, hallucinations, agitation/aggression, depression/dysphoria, anxiety, elation/euphoria, apathy/indifference, disinhibition, irritability/lability, motor disturbance, night-time behaviours and appetite/eating, each on a scale from 0 to 3 with 3 indicating more severe symptoms (Kaufer et al., Citation2000). The NPI-Q was completed by the informal caregiver.
Main exposure variables: needs for daytime activities and company (collected at baseline, six and twelve months)
Needs were measured using the Camberwell Assessment of Need for the Elderly (CANE) scale (Reynolds et al., Citation2000). The CANE is an interview-based questionnaire designed to map the needs of older people (‘needs present’; if answered with ‘yes’, then ‘met’ or ‘unmet’) and amount of help (‘received’ and ‘needed’) in relation to 24 items that address psychological, physical and environmental domains (Orrell & Hancock, Citation2004). The two items ‘daytime activities’ and ‘company’ were selected for this study for which only data on whether needs were present and, if so, met or unmet, were used. In the Actifcare study, needs of the person with dementia were reported by themself, the caregiver, and the researcher; based on an overall perspective from extensive interviews with the person with dementia and the caregiver. In this study, we wanted to include the perspective of the person with dementia along with all other information. We therefore used scores for needs assessed by the researcher which are based on the reports from the person with dementia and the informal caregiver, together with all other information available to the researcher. The categories ‘no need’ and ‘met need’ were collapsed into one category and compared to ‘unmet need’. The needs variables were treated as time-dependent covariates in the analyses.
Covariates (collected at baseline, six and twelve months)
Level of dementia was measured with the Clinical Dementia Rating scale (CDR) (Hughes, Berg, Danziger, Coben, & Martin, Citation1982). Six domains of cognitive and functional performance are characterised using a scale of 0–3, where 0 indicates normal function and 3 indicates severe decline. The CDR was completed by the researchers after each interview based on all available data, and the sum of boxes scores, where the six item scores are added up (0–18 points) were used for this study (O’Bryant et al., Citation2008). Comorbidity was measured using the Charlson Comorbidity Index (Charlson, Pompei, Ales, & MacKenzie, Citation1987), where higher scores indicate more comorbidities. Quan et al. have suggested updated weights of the contribution of chronic comorbidities of this index as a result of advances in medical treatment (Quan et al., Citation2011), and these updated weights were applied for each of the Charlson Comorbidity Index item scores before a sum score was produced for use in the analyses. Instrumental activities of daily living (IADL) were measured with Lawton and Brody’s IADL scale, ranging from 0 to 8 with a lower score indicating a higher level of dependence (Lawton & Brody, Citation1969). Living situation was divided into two categories: (1) living alone and (2) living with someone.
Covariates (collected at baseline only)
The participants were from different European regions and, grouped in line with Handels et al. (Handels et al., Citation2018): North (Sweden and Norway), Middle (the Netherlands, Germany, UK and Ireland) and South (Portugal and Italy). Furthermore, all participants had a diagnosis of dementia meeting the DSM-IV criteria (American Psychiatric Association, Citation2000) following an assessment by a clinical professional. When an aetiological dementia diagnosis was available, this was recorded using the following categories: Alzheimer’s disease (AD), Vascular dementia (VaD), mixed AD and VaD, Lewy body dementia (LBD) or ‘other’ dementia. Education of person with dementia was used in the analyses as a continuous variable of years of full-time education.
Statistics
The 12 BPSD symptoms assessed with the NPI-Q are quite different and using a sum score in analyses is not a preferred solution as two different participants with the same sum score may have significantly different clinical presentation. To identify clusters and group the symptoms measured by the NPI-Q, a principal component analysis (PCA) was performed initially for the NPI-Q. We kept all items regardless of initial correlation and used varimax rotation and an eigenvalue greater than 1.0. The PCA resulted in three factors (see ) that were used in the analyses: agitation (agitation, euphoria, disinhibition, irritability and motor disturbance), affective (depression, anxiety, apathy and appetite) and psychotic (delusions, hallucinations and night-time behaviours). The three items anxiety, appetite and delusions each loaded on two factors. These items were placed in the factor on which they loaded most heavily, which was also the factor in which they are commonly found to fit (van der Linde et al., Citation2014).
Table 1. Principal component analysis of the Neuropsychiatric Inventory-Questionnaire (NPI-Q), Varimax rotation with Kaiser normalisation.
To describe the proportion of the participants with clinically relevant levels of BPSD at baseline, we have chosen to categorise the sum score in each NPI-Q sub-syndrome into 3 groups: no/not significant, mild/moderate and severe symptoms. There is no common agreement on cut-offs for clinically relevant symptoms using the NPI-Q, and we have used a cut-off between no/not significant and mild/moderate which is in line with similar cut-offs used for the NPI (Aalten et al., Citation2007; Lyketsos et al., Citation2002). The difference in proportion of clinically relevant symptoms between participants with no/met need and unmet need is investigated with Chi-square analyses using the following two categories: mild, moderate and severe symptoms vs no/not significant symptoms.
Linear mixed models with random intercepts and slopes were used, with the three NPI-Q sub-syndromes as the dependent variables (one-by-one) and unmet needs vs met needs/no needs for daytime activities or company as independent variables. The CDR, Charlson Comorbidity Index, IADL and a time variable (coded as 0 for baseline, 1 for six months and 2 for 12 months) were all treated as time-dependent covariates in the analyses. Because a linear time variable had equally good fit as the more complex three level dummy variable in a likelihood ratio test, the simpler continuous linear variable was preferred. The other variables were all treated as fixed time-invariant variables (dementia diagnosis, region, baseline age measured on the continuous scale). First six unadjusted linear mixed models were used, then six adjusted models where age, sex, CDR, region, Charlson Comorbidity Index, IADL, diagnosis and living together/alone were added to the model. An interaction term (needs by time) was added to test whether differences changed over time. The inclusion of both the random intercept and slope improved the fit of the models significantly as revealed by a likelihood ratio test, and thus both terms were included.
Statistical analyses were performed using IBM SPSS Statistics version 25 and Stata version 16.0.
Ethical considerations
Ethical approval was obtained separately in each of the participating countries. Written informed consent was obtained from participants or, for people with dementia with reduced ability to consent, from an informal caregiver/legal representative.
Results
Data from between 425 and 437 (depending on which CANE item and which NPI-Q sub-syndrome was being analysed) participants were sufficiently complete to be used for baseline analyses. The mean age of the participants at baseline was 78 years (SD 7.85), and 55% were female. The mean CDR sum of boxes score was 7.1 (SD 2.43), indicating mild dementia. A total of 28.9% had unmet needs for daytime activities, and 27.3% had unmet needs for company. For other characteristics of the participants, see .
Table 2. Characteristics of the participants at baseline.
shows proportions of participants with clinically significant BPSD at baseline. A larger proportion of the participants with unmet needs both for daytime activity and company had mild to moderate symptoms of affective and psychotic symptoms, compared to participants with no need or met need. Few participants had severe symptoms.
Table 3. Proportions of participants with clinically significant symptoms at baseline, per subsyndrome, classified as no/not significant symptoms – mild/moderate symptoms – severe symptoms, grouped by no/met need and unmet need for daytime activities and company.
Daytime activities
Participants with unmet needs for daytime activities had higher scores on the NPI-Q affective items with a mean of 0.74 (95% Confidence Interval [CI] 0.34, 1.14, p < 0.001), 0.76 (95% CI 0.46, 1.06, p < 0.001) and 0.78 (95% CI 0.32, 1.24, p = 0.001) points higher at baseline, six months and twelve months, respectively (, mixed model, adjusted). The SDs for NPI-Q affective scores for the reference groups (no/met need) were 2.46, 2.35 and 2.47 at baseline, six months, and twelve months, respectively. Thus, the effect sizes for the differences in scores on affective symptoms corresponded to 0.30, 0.32 and 0.32 SDs at baseline, six months and twelve months respectively. Unmet needs for daytime activities were also associated with more severe symptoms on the psychotic factor of the NPI-Q at baseline (mean of 0.39 points higher, 95% CI 0.10, 0.67, p = 0.007) and at the six-month follow-up (mean of 0.31 points higher, 95% CI 0.09, 0.52, p = 0.006). These effect sizes for psychotic symptoms corresponded to 0.23 SD at baseline and 0.19 SD at six months. The differences in the NPI-Q affective and psychotic items between the groups with no/met and unmet needs did not change over time (interaction terms unmet needs*time were not significant; p = 0.935 for affective items, p = 0.500 for psychotic items) see . Scores on the agitation factor of the NPI-Q were not associated with unmet needs for daytime activities.
Figure 1. Mean Neuropsychiatric Inventory-Questionnaire (NPI-Q) scores over time for those with no need/met needs for daytime activities versus those with unmet needs. Vertical lines are 95% confidence intervals. Estimated in mixed regression where needs was modelled as a time dependent covariate, adjusted by age, sex, living alone/with someone, region, diagnosis, education, Charlson Comorbidity Index, Clinical Dementia Rating and Instrumental Activities of Daily Living.
NPI-Q agitation sub-syndrome = agitation, euphoria, disinhibition, irritability and motor disturbance – max score = 15
NPI-Q affective sub-syndrome = depression, anxiety, apathy and appetite – max score = 12
NPI-Q psychotic sub-syndrome = delusions, hallucinations and night-time behaviours – max score = 9
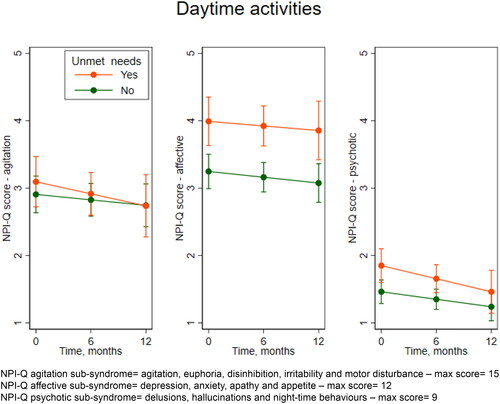
Table 4. Mean difference in NPI-Q sub-syndromes between groups: no need/met need vs unmet need, concerning daytime activities and company.
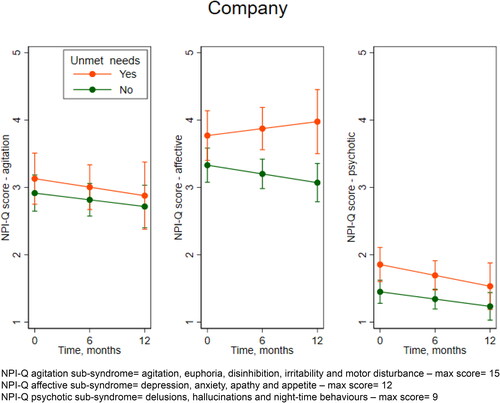
Company
Participants with unmet needs for company had higher scores on the NPI-Q affective items with a mean of 0.44 (95% CI 0.04, 0.84, p = 0.033), 0.67 (95% CI 0.35, 0.99, p < 0.001), and 0.91 (95% CI 0.41, 1.41, p < 0.001) points higher at baseline, six months and twelve months, respectively (, mixed model, adjusted). These effect sizes for the differences in scores on affective symptoms corresponded to 0.18, 0.29 and 0.36 SDs at baseline, six months and twelve months, respectively. Unmet needs for company were associated with more severe symptoms on the psychotic factor of the NPI-Q at baseline (mean of 0.40 points higher, 95% CI 0.12, 0.69, p = 0.005) and at the six-month follow-up (mean of 0.35 points higher, 95% CI 0.12, 0.58, p = 0.002). These effect sizes for difference in scores on psychotic symptoms corresponded to 0.24 SD at baseline and 0.21 SD at six months. The differences in the NPI-Q affective and psychotic items between the groups with no/met and unmet needs did not change significantly over time (interaction terms unmet needs*time were not significant; p = 0.170 for affective items, p = 0.694 for psychotic items), even though there was a tendency towards a larger difference in scores over time for affective symptoms (see ). Scores on the agitation factor of the NPI-Q were not associated with unmet needs for company.
Figure 2. Mean Neuropsychiatric Inventory-Questionnaire (NPI-Q) scores over time for those with no need/met needs for company versus those with unmet needs. Vertical lines are 95% confidence intervals. Estimated in mixed regression where needs was modelled as a time dependent covariate, adjusted by age, sex, living alone/with someone, region, diagnosis, education, Charlson Comorbidity Index, Clinical Dementia Rating and Instrumental Activities of Daily Living.
NPI-Q agitation sub-syndrome = agitation, euphoria, disinhibition, irritability and motor disturbance – max score = 15
NPI-Q affective sub-syndrome = depression, anxiety, apathy and appetite – max score = 12
NPI-Q psychotic sub-syndrome = delusions, hallucinations and night-time behaviours – max score = 9
Discussion
In this longitudinal study, we found that unmet needs for daytime activities and for company were associated with more affective and psychotic symptoms over twelve months. We also found a lack of association between agitation symptoms and unmet needs for daytime activities and company.
The differences we have found are significant, but the effect sizes are small. This is, however, on a group level. As seen in , a larger proportion of the participants with unmet needs had clinically significant BPSD at baseline compared to those with no needs or met needs. On an individual level, the presence of clinically significant symptoms may make a large impact on the life of a person with dementia, as well as on their caregivers, and even a small reduction of symptoms may improve their everyday lives.
The association between unmet needs for daytime activities and company and affective and psychotic symptoms
According to previous studies, unmet needs are, in general, associated with BPSD (Miranda-Castillo et al., Citation2010). In the Unmet Needs Model, Cohen-Mansfield et al. described BPSD (‘problem behaviours’) as a result of unmet needs stemming from a decreased ability of people with dementia to communicate those needs and to provide for themselves (Cohen-Mansfield et al., Citation2015). They focussed mainly on agitation in nursing home residents when describing the model, which is a setting that likely includes people with more severe dementia than the participants in our study. Yet the principle that behaviour is need-driven may also apply to community-dwelling people in a mild or moderate phase of dementia and to other symptoms such as affective and psychotic symptoms.
Apathy, depression, and anxiety (all included in our affective factor) are the most prevalent BPSD, and anxiety and depression are common in an early stage of dementia (Kales et al., Citation2015). The participants in our study were in a mild or moderate stage of dementia where affective symptoms are common. They could be starting to experience a decrease in their ability to meet their own needs for daytime activities and social life due to ADL impairments. Impairment in ADL has been found to be associated with a higher number of unmet needs (Eichler et al., Citation2016). Experiencing loss of function may contribute to affective symptoms because one may lose one’s sense of autonomy or feel less valued. Company and daytime activities are both considered to be social needs, and unmet social needs have been found to be associated with higher levels of depression along with unmet psychological needs (Alltag et al., Citation2018).
Depressive symptoms are described as being intensified or maintained by the absence of positive feelings resulting from participation in enjoyable and meaningful activities (Orgeta, Brede, & Livingston, Citation2017). Furthermore, having depressive symptoms, anxiety or apathy may lead to not taking the initiative to be active and to meet people even if it would be beneficial, thereby resulting in unmet needs for daytime activities and company.
To our knowledge, no previous studies have found an association between psychotic symptoms and unmet needs for daytime activities and company. Psychotic symptoms in dementia may share similarities with symptoms of schizophrenia, where reduced social activity and interest, loss of motivation and reduced productive activity are often present (Cipriani, Danti, Nuti, Di Fiorino, & Cammisuli, Citation2020). It might be that people with dementia who experience psychotic symptoms are withdrawing from activities and from social interaction since their symptoms make it difficult for them to function in some kinds of activities and social settings. Delusions may make it difficult to trust others and to communicate in a relevant way. Further, psychotic symptoms may make it harder for caregivers to fulfil needs in people with dementia. It may also be that unmet needs for daytime activities and company contribute to psychotic symptoms in people with dementia, for example due to lack of interaction with other people. On the other hand, too much stimuli may add to psychotic symptoms.
The lack of association between agitation and unmet needs for daytime activities and company
In this study, no associations were found between the agitation symptom cluster and unmet needs for daytime activities or company. Agitation itself is a heterogeneous term and is often used to describe diverse symptoms such as pacing, hoarding, making disruptive sounds, asking repetitive questions and becoming upset easily (Kales et al., Citation2015). In our PCA, the items included in the agitation factor were agitation, euphoria, disinhibition, irritability, and motor disturbance. Even if these items loaded on the same factor, they may have less in common than the items in the affective or psychotic factor. Van der Linde et al. found that studies using PCA on the NPI-Q generally suggest the following symptom groups: (1) affective symptoms, (2) psychosis, (3) hyperactivity and (4) euphoria (van der Linde et al., Citation2014). Our agitation factor includes both 3 and 4, indicating that this factor may be our most heterogeneous.
The need for daytime activities and company
In research on needs among people with dementia, unmet needs for daytime activities and company are frequently found (Kerpershoek et al., Citation2018; Miranda-Castillo et al., Citation2010; van der Roest et al., Citation2009). Even if professional support was frequently provided for company and daytime activities, unmet needs were still reported in these areas (van der Roest et al., Citation2009). Involvement in meaningful activities has been found to be important for people with dementia because it gives them feelings of enjoyment and pleasure, connection and belonging as well as autonomy and identity (Phinney, Chaudhury, & O’Connor, Citation2007). Daytime activities and company are connected to the essential psychological needs for occupation, inclusion and attachment in person-centred care (Kitwood, Citation1997), and their importance may be explained by the association between occupation, health and well-being (Christiansen & Townsend, Citation2011).
Studies have shown that social isolation and reduced access to their usual activities may increase the risk of mental health problems in older adults (Armitage & Nellums, Citation2020), and it is likely that people with dementia are at particular risk. Assessing at an early stage of the disease, as well as reassessing regularly, whether needs for daytime activities and company are met and providing these if needed may prevent or reduce BPSD and enhance quality of life in people with dementia.
Implications for post-diagnostic support to reduce unmet needs
Although we have found associations between unmet needs for daytime activities and company and affective and psychotic symptoms, the direction here may be discussed. It may be that unmet needs for daytime activities and company contribute to affective and psychotic symptoms; it is also possible that these symptoms contribute to unmet needs; or it could go both ways as a downward spiral. However, this implies that if post-diagnostic support can reduce either unmet needs or affective and psychotic symptoms, this could affect the other part of the equation.
Assessing the needs of people with dementia is useful both for helping to identify interventions and services that should be tailored to each individual and planning the provision of health care on a macro level (Curnow et al., Citation2021; Reynolds et al., Citation2000). An assessment of unmet needs should be carried out as early as possible in the process of dementia and updated regularly. Sometimes it takes a while to establish a diagnosis, but interventions to target unmet needs do not have to await the diagnosis. With the assessment of symptoms and functioning and post-diagnostic support assigned to the same municipal dementia-resource team, as provided by the Norwegian model, post-diagnostic support can even include pre-diagnostic support. Moreover, it can be individually tailored and be initiated as soon as symptoms and/or needs become known (Michelet et al., Citation2020).
Enabling people with dementia to engage in meaningful activities as part of their everyday lives should be part of post-diagnostic support (Gitlin et al., Citation2009; Kales et al., Citation2015; Lobbia et al., Citation2019; Orgeta et al., Citation2017). Person-centred care includes the promotion of social participation and meaningful activities, and these are important components of several psychosocial interventions for people with dementia. Evidence of efficacy has been found for a variety of such interventions delivered to home-dwelling people with mild to moderate dementia; however, the use of such interventions remains low (Keogh, Mountain, Joddrell, & Lord, Citation2019). Informal caregivers play a crucial role in several of the interventions. In this study, we address caregivers only as partners in the provision of interventions, even though several of the interventions may also have an effect on caregivers’ health and well-being.
Adult day services such as day care for people with dementia may serve to meet the needs for daytime activities and company, given that the service is age appropriate and individually tailored (Strandenaes, Lund, & Rokstad, Citation2018, Citation2019). In a review, attending adult day care was found to increase social engagement for people with dementia through participation in activities with peers with whom they feel safe and comfortable. Further, participants who attended adult day care exhibited significantly less depression and fewer behavioural issues compared to participants who did not attend (Du Preez, Millsteed, Marquis, & Richmond, Citation2018).
Group interventions targeting activities, such as behavioural activation and Cognitive Stimulation Therapy (CST), have been found to offer several positive effects including reducing anxiety and depressive symptoms, improving quality of life and communication, reducing problematic behavioural symptoms, and increasing scores on ADL for community-dwelling people with dementia (Lobbia et al., Citation2019; Orgeta et al., Citation2017). Caregivers being taught to use activities individually tailored to the capabilities and interests of people with dementia in the Tailored Activity Program (TAP) report reduced behavioural symptoms (Gitlin et al., Citation2009).
Strengths and limitations
The strength of this study is that the data were from a large cohort study with participants from eight countries across Europe and may, therefore, be representative of a larger group of people with dementia. However, this heterogeneity could also be a limitation as the recruitment of participants differed, including the sources used in estimating that need for additional assistance would likely be required within one year. The sample studied was a convenience sample. There might also have been heterogeneity among the researchers collecting data as the perceptions of different symptoms and use of the measures may differ across researchers in different countries. However, joint training was conducted, and there were meetings and regular contact within the project group to coordinate the data collection for consistency and improved inter-rater reliability.
Furthermore, in the analyses, the twelve NPI-Q items were reduced to three factors following a PCA. This may have resulted in the loss of some of the details in the data. Having three NPI-Q factors is, however, comparable to other studies that have used the NPI-Q (Truzzi et al., Citation2013). The NPI-scores are not based on direct observations or on the view of the person with dementia, but on proxy information, from an informal caregiver. This may be a limitation because proxy information could be influenced by caregiver distress or relationship quality.
From the needs assessment (CANE) data, the researchers’ assessments were used rather than those of the people with dementia. The researchers did consider the scores from the people with dementia and the informal caregiver as well as other available information, but there is always a risk that the perspective of the people with dementia was not given enough weight in these scorings.
Conclusion
In this study, we found that unmet needs for daytime activities and for company were associated with more affective and psychotic symptoms but not with more symptoms of agitation. This is in line with previous findings and may serve to elaborate the importance of structured and repeated assessment of needs and a proactive approach towards fulfilling unmet needs for daytime activities and company for people with dementia. Psychosocial interventions in post-diagnostic support creating meaningful occupations and addressing social needs may reduce unmet needs for daytime activities and company and, thereby, reduce affective and psychotic symptoms.
Acknowledgements
Data was from the Actifcare EU Joint Programme – Neurodegenerative Disease Research (JPND) project. The Actifcare Consortium partners are:
Coordinator: Maastricht University (NL): Frans Verhey, Marjolein de Vugt (scientific coordinators, WP1 leader).
Consortium members: Maastricht University (NL): Marjolein de Vugt, Claire Wolfs, Ron Handels, Liselot Kerpershoek. Martin-Luther University Halle-Wittenberg (DE): Gabriele Meyer (WP2 leader), Astrid Stephan, Anja Bieber, Anja Broda, Gabriele Bartoszek. Bangor University (UK): Bob Woods (WP3 leader), Hannah Jelley. Nottingham University (UK): Martin Orrell. Karolinska Institutet (SE): Anders Wimo (WP4 leader), Anders Sköldunger, Britt-Marie Sjölund. Oslo University Hospital (NO): Knut Engedal, Geir Selbaek (WP5 leader), Mona Michelet, Janne Rosvik, Siren Eriksen. Dublin City University (IE): Kate Irving (WP6 leader), Louise Hopper, Rachael Joyce. CEDOC, Nova Medical School/Faculdade de Ciências Médicas, Universidade Nova de Lisboa (PT): Manuel Gonçalves-Pereira, Maria J. Marques, Conceiçäo Balsinha, on behalf of the Portuguese Actifcare team (FCT-JPNDHC/0001/2012). Alzheimer’s Research Unit-Memory Clinic, IRCCS Instituto Centro San Giovanni di Dio Fatebenefratelli (IT): Orazio Zanetti, Daniel M. Portolani.
Disclosure statement
Geir Selbaek is a member of the advisory board of Biogen in Norway. The authors report no other conflict of interest.
Additional information
Funding
Funding
References
- Aalten, P., Verhey, F. R., Boziki, M., Bullock, R., Byrne, E. J., Camus, V., … Robert, P. H. (2007). Neuropsychiatric syndromes in dementia. Results from the European Alzheimer Disease Consortium: Part I. Dementia and Geriatric Cognitive Disorders, 24(6), 457–463. http://www.ncbi.nlm.nih.gov/pubmed/17986816 doi:https://doi.org/10.1159/000110738
- Alltag, S., Stein, J., Pabst, A., Weyerer, S., Werle, J., Maier, W., … Riedel-Heller, S. G. (2018). Unmet needs in the depressed primary care elderly and their relation to severity of depression: Results from the AgeMooDe study. Aging & Mental Health, 22(8), 1032–1039. doi:https://doi.org/10.1080/13607863.2017.1328480
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR (4th ed., text revision ed.). Washington, DC: American Psychiatric Association.
- Armitage, R., & Nellums, L. B. (2020). COVID-19 and the consequences of isolating the elderly. The Lancet. Public Health, 5(5), e256. doi:https://doi.org/10.1016/S2468-2667(20)30061-X
- Black, B. S., Johnston, D., Leoutsakos, J., Reuland, M., Kelly, J., Amjad, H., … Samus, Q. M. (2019). Unmet needs in community-living persons with dementia are common, often non-medical and related to patient and caregiver characteristics. International Psychogeriatrics, 31(11), 1643–1654. doi:https://doi.org/10.1017/S1041610218002296
- Charlson, M. E., Pompei, P., Ales, K. L., & MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases, 40(5), 373–383. doi:https://doi.org/10.1016/0021-9681(87)90171-8
- Christiansen, H. C., & Townsend, E. A. (2011). Introduction to occupation - The art and science of living (2nd ed.). Essex, England: Pearson Educational Limited.
- Cipriani, G., Danti, S., Nuti, A., Di Fiorino, M., & Cammisuli, D. M. (2020). Is that schizophrenia or frontotemporal dementia? Supporting clinicians in making the right diagnosis. Acta Neurologica Belgica, 120(4), 799–804. doi:https://doi.org/10.1007/s13760-020-01352-z
- Cohen-Mansfield, J., Dakheel-Ali, M., Marx, M. S., Thein, K., & Regier, N. G. (2015). Which unmet needs contribute to behavior problems in persons with advanced dementia?Psychiatry Research, 228(1), 59–64. doi:https://doi.org/10.1016/j.psychres.2015.03.043
- Cunningham, C., Macfarlane, S., & Brodaty, H. (2019). Language paradigms when behaviour changes with dementia: #BanBPSD. International Journal of Geriatric Psychiatry, 34(8), 1109–1113. doi:https://doi.org/10.1002/gps.5122
- Curnow, E., Rush, R., Maciver, D., Gorska, S., & Forsyth, K. (2021). Exploring the needs of people with dementia living at home reported by people with dementia and informal caregivers: A systematic review and Meta-analysis. Aging and Mental Health, 25(3), 397–407. doi:https://doi.org/10.1080/13607863.2019.1695741
- Du Preez, J., Millsteed, J., Marquis, R., & Richmond, J. (2018). The role of adult day services in supporting the occupational participation of people with dementia and their carers: An integrative review. Healthcare (Basel), 6(2), 43. doi:https://doi.org/10.3390/healthcare6020043
- Eichler, T., Thyrian, J. R., Hertel, J., Richter, S., Wucherer, D., Michalowsky, B., … Hoffmann, W. (2016). Unmet needs of community-dwelling primary care patients with dementia in Germany: Prevalence and correlates. Journal of Alzheimer’s Disease, 51(3), 847–855. doi:https://doi.org/10.3233/JAD-150935
- Gitlin, L. N., Winter, L., Vause Earland, T., Adel Herge, E., Chernett, N. L., Piersol, C. V., & Burke, J. P. (2009). The Tailored Activity Program to reduce behavioral symptoms in individuals with dementia: Feasibility, acceptability, and replication potential. The Gerontologist, 49(3), 428–439. doi:https://doi.org/10.1093/geront/gnp087
- Handels, R. L. H., Skoldunger, A., Bieber, A., Edwards, R. T., Goncalves-Pereira, M., Hopper, L., … Wimo, A. (2018). Quality of life, care resource use, and costs of dementia in 8 European countries in a cross-sectional cohort of the actifcare study. Journal of Alzheimer’s Disease: JAD, 66(3), 1027–1040. doi:https://doi.org/10.3233/JAD-180275
- Hoe, J., Hancock, G., Livingston, G., & Orrell, M. (2006). Quality of life of people with dementia in residential care homes. British Journal of Psychiatry, 188(5), 460–464. doi:https://doi.org/10.1192/bjp.bp.104.007658
- Hughes, C. P., Berg, L., Danziger, W. L., Coben, L. A., & Martin, R. L. (1982). A new clinical scale for the staging of dementia. The British Journal of Psychiatry: The Journal of Mental Science, 140, 566–572. doi:https://doi.org/10.1192/bjp.140.6.566
- Janssen, N., Handels, R. L., Sköldunger, A., Woods, B., Jelley, H., Edwards, R. T., … Wimo, A. (2018). Impact of untimely access to formal care on costs and quality of life in community dwelling people with dementia. Journal of Alzheimer’s Disease: JAD, 66(3), 1165–1174. doi:https://doi.org/10.3233/JAD-180531
- Kales, H. C., Gitlin, L. N., & Lyketsos, C. G. (2015). Assessment and management of behavioral and psychological symptoms of dementia. BMJ (Clinical Research Ed.), 350, h369. doi:https://doi.org/10.1136/bmj.h369
- Kaufer, D. I., Cummings, J. L., Ketchel, P., Smith, V., MacMillan, A., Shelley, T., … DeKosky, S. T. (2000). Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory [npi npi-q]. Journal of Neuropsychiatry and Clinical Neurosciences, 12(2), 233–239. doi:https://doi.org/10.1176/jnp.12.2.233
- Keogh, F., Mountain, G., Joddrell, P., & Lord, K. (2019). Psychosocial interventions for community-dwelling people following diagnosis of mild to moderate dementia: Findings of a systematic scoping review. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 27(6), 641–651. doi:https://doi.org/10.1016/j.jagp.2018.12.027
- Kerpershoek, L., de Vugt, M., Wolfs, C., Jelley, H., Orrell, M., Woods, B., … Verhey, F. (2016). Access to timely formal dementia care in Europe: Protocol of the Actifcare (ACcess to Timely Formal Care) study. BMC Health Services Ressearch, 16(1), 423. doi:https://doi.org/10.1186/s12913-016-1672-3
- Kerpershoek, L., de Vugt, M., Wolfs, C., Woods, B., Jelley, H., Orrell, M., … Verhey, F. (2018). Needs and quality of life of people with middle-stage dementia and their family carers from the European Actifcare study. When informal care alone may not suffice. Aging & Mental Health, 22(7), 897–902. doi:https://doi.org/10.1080/13607863.2017.1390732
- Kitwood, T. (1997). Dementia reconsidered: The person comes first. Buckinham: Open University Press.
- Lawton, M. P., & Brody, E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9(3), 179–186. doi:https://doi.org/10.1093/geront/9.3_Part_1.179
- Lobbia, A., Carbone, E., Faggian, S., Gardini, S., Piras, F., Spector, A., & Borella, E. (2019). The Efficacy of Cognitive Stimulation Therapy (CST) for people with mild-to-moderate dementia. European Psychologist, 24(3), 257–277. doi:https://doi.org/10.1027/1016-9040/a000342
- Lyketsos, C. G., Lopez, O., Jones, B., Fitzpatrick, A. L., Breitner, J., & DeKosky, S. (2002). Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: Results from the cardiovascular health study. JAMA, 288(12), 1475–1483. doi:https://doi.org/10.1001/jama.288.12.1475
- Mazurek, J., Szcześniak, D., Lion, K. M., Dröes, R.-M., Karczewski, M., & Rymaszewska, J. (2019). Does the Meeting Centres Support Programme reduce unmet care needs of community-dwelling older people with dementia? A controlled, 6-month follow-up Polish study. Clinical Interventions in Aging, 14, 113–122. doi:https://doi.org/10.2147/CIA.S185683
- Michelet, M., Lund, A., Strand, B. H., Engedal, K., Selbaek, G., & Bergh, S. (2020). Characteristics of patients assessed for cognitive decline in primary healthcare, compared to patients assessed in specialist healthcare. Scandinavian Journal of Primary Health Care, 38(2), 107–110. doi:https://doi.org/10.1080/02813432.2020.1753334
- Miranda-Castillo, C., Woods, B., Galboda, K., Oomman, S., Olojugba, C., & Orrell, M. (2010). Unmet needs, quality of life and support networks of people with dementia living at home. Health and Quality of Life Outcomes, 8, 132. doi:https://doi.org/10.1186/1477-7525-8-132
- O’Bryant, S. E., Waring, S. C., Cullum, C. M., Hall, J., Lacritz, L., Massman, P. J., … Doody, R. (2008). Staging dementia using Clinical Dementia Rating Scale Sum of Boxes scores: A Texas Alzheimer’s research consortium study. Archives of Neurology, 65(8), 1091–1095. doi:https://doi.org/10.1001/archneur.65.8.1091
- Orgeta, V., Brede, J., & Livingston, G. (2017). Behavioural activation for depression in older people: Systematic review and meta-analysis. The British Journal of Psychiatry: The Journal of Mental Science, 211(5), 274–279. doi:https://doi.org/10.1192/bjp.bp.117.205021
- Orrell, M., & Hancock, G. (2004). CANE-Camberwell assessment of need for the elderly: A needs assessment for older mental health service users. London: Gaskell.
- Phinney, A., Chaudhury, H., & O’Connor, D. L. (2007). Doing as much as I can do: The meaning of activity for people with dementia. Aging & Mental Health, 11(4), 384–393. doi:https://doi.org/10.1080/13607860601086470
- Quan, H., Li, B., Couris, C. M., Fushimi, K., Graham, P., Hider, P., … Sundararajan, V. (2011). Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. American Journal of Epidemiology, 173(6), 676–682. doi:https://doi.org/10.1093/aje/kwq433
- Reynolds, T., Thornicroft, G., Abas, M., Woods, B., Hoe, J., Leese, M., &Orrell, M. (2000). Camberwell Assessment of Need for the Elderly(CANE). Development, validity and reliability. The British Journal of Psychiatry: The Journal of Mental Science, 176, 444–452. doi:https://doi.org/10.1192/bjp.176.5.444
- Strandenaes, M. G., Lund, A., & Rokstad, A. M. M. (2018). Experiences of attending day care services designed for people with dementia - A qualitative study with individual interviews. Aging & Mental Health, 22(6), 764–772. doi:https://doi.org/10.1080/13607863.2017.1304892
- Strandenaes, M. G., Lund, A., & Rokstad, A. M. M. (2019). Facilitation of activities for people with dementia in day care: A qualitative study exploring the experiences of staff. Journal of Multidisciplinary Healthcare, 12, 503–513. doi:https://doi.org/10.2147/JMDH.S198024
- Truzzi, A., Ulstein, I., Valente, L., Engelhardt, E., Coutinho, E. S., Laks, J., & Engedal, K. (2013). Patterns of neuropsychiatric sub-syndromes in Brazilian and Norwegian patients with dementia. International Psychogeriatrics, 25(2), 228–235. doi:https://doi.org/10.1017/S1041610212001640
- van der Linde, R. M., Dening, T., Matthews, F. E., & Brayne, C. (2014). Grouping of behavioural and psychological symptoms of dementia. International Journal of Geriatric Psychiatry, 29(6), 562–568. doi:https://doi.org/10.1002/gps.4037
- van der Roest, H. G., Meiland, F. J., Comijs, H. C., Derksen, E., Jansen, A. P., van Hout, H. P., … Droes, R. M. (2009). What do community-dwelling people with dementia need? A survey of those who are known to care and welfare services. International Psychogeriatrics, 21(5), 949–965. doi:https://doi.org/10.1017/S1041610209990147
- Wergeland, J. N., Selbaek, G., Bergh, S., Soederhamn, U., & Kirkevold, Ø. (2015). Predictors for nursing home admission and death among community-dwelling people 70 years and older who receive domiciliary care. Dementia and Geriatric Cognitive Disorders Extra, 5(3), 320–329. doi:https://doi.org/10.1159/000437382
- Wolverson, E., Birtles, H., Moniz-Cook, E., James, I., Brooker, D., & Duffy, F. (2019). Naming and Framing the Behavioural and Psychological Symptoms of Dementia (BPSD) paradigm: Professional stakeholder perspectives. OBM Geriatrics, 3(4), 1–1. doi:https://doi.org/10.21926/obm.geriatr.1904080
