Abstract
Objectives
Long-term use of anticholinergic medication in older people is associated with increased risk of cognitive decline and mortality, but this relationship could be confounded by the underlying illness the drugs are treating. To investigate associations between central anticholinergic antidepressants or antipsychotics and mortality, hospitalisation and cognitive decline in people with dementia.
Method
In cohorts of patients with a dementia diagnosis receiving antidepressant and/or antipsychotic medication (N = 4,380 and N = 2,335 respectively), assembled from a large healthcare database, central anticholinergic burden scores were estimated using the Anticholinergic Effect on Cognition (AEC) scale. Data were linked to national mortality and hospitalisation data sources, and Mini-Mental State Examination (MMSE) scores were used to investigate cognitive decline.
Results
There was a reduced mortality risk in people receiving agents with high central anticholinergic burden compared to those with no or low burden which was statistically significant in the antidepressant cohort (Hazard ratio (HR): 0.88; 95% confidence interval (CI): 0.79-0.98; p = 0.023) but not the antipsychotic one (HR: 0.91; 95% CI: 0.82-1.02; p = 0.105). Patients on antidepressants with no central anticholinergic burden had accelerated cognitive decline compared with other groups, whereas no differences were found in the antipsychotic cohort. No significant associations were detected between antidepressant or antipsychotic-related central anticholinergic burden and hospitalisation.
Conclusion
These counter-intuitive findings may reflect factors underlying the choice of psychotropics rather than the agents themselves, although do not support a strong role for central anticholinergic drug actions on dementia outcomes. Further studies, including randomized switching of agents are needed to clarify this relationship.
Key points
Anticholinergic drugs are associated with increased mortality, hospitalisation and cognitive decline. This study investigates the associations between central anticholinergic burden (using the AEC scale) and mortality, hospitalisation and cognitive decline in people with dementia on antidepressant or antipsychotic drugs. In summary, no evidence for this was found, with all associations either null or in the opposite direction to that anticipated.
Introduction
There is growing evidence linking the long-term use of anticholinergic medication in community samples of older people with increased risk of cognitive decline, dementia and mortality (Fox et al., Citation2011b). Research has focused on the relationship between overall anticholinergic activity and dementia risk, with fewer studies investigating the relationship with dementia outcomes. Studies have reported consistent associations between certain classes of anticholinergic drugs and future dementia incidence (Coupland et al., Citation2019; Richardson et al., Citation2018). While this could reflect a class specific effect of anticholinergic drugs, it could also be confounded by the underlying illnesses that these drugs are treating: depression for example, which is a potential risk factor for dementia (Saczynski et al., Citation2010).
Evidence is lacking on associations between central anticholinergic activity and dementia outcomes. The Anticholinergic Effect on Cognition (AEC) scale (Bishara et al., Citation2017) is an anticholinergic burden scale which specifically allows clinicians to easily identify which medicines have a central anticholinergic effect on cognition, along with the size of the effect for different medicines individually and in combination. This helps to inform the choice of medicines and any changes required. This scale has shown that patients with dementia receiving medication with high central anticholinergic activity (as measured on the AEC scale), appear to have worse prognosis in terms of mortality and hospitalisation risk (Bishara et al., Citation2020).
The purpose of this study was to investigate the associations between AEC scores within specific drug classes (antidepressants and antipsychotics) and mortality, hospitalisation and cognitive function in people with dementia. Since data suggest that antipsychotics and antidepressants are associated with increased mortality in people with dementia (Mueller et al., Citation2017, Citation2020), our aim was to find out whether central anticholinergic burden is a potential driver for this increased mortality risk.
This was a retrospective study of patients with dementia using anonymised mental health records linked with mortality and hospitalisation data. We compared the risks associated with drugs within the same therapeutic class, so that the resulting outcomes could not be attributed to the illnesses being treated, but to the drugs themselves. We hypothesised that drugs with high central anticholinergic burden would be associated with worse outcomes compared with those with no central anticholinergic burden.
Methods
Data source
Data for this study were obtained from the South London and Maudsley NHS Foundation Trust (SLaM) Clinical Record Interactive Search (CRIS) resource. This system provides research access to more than 500,000 health records from SLaM within a robust governance framework (Perera et al., 2016; Stewart et al., Citation2009). CRIS has received ethical approval as an anonymised data resource (Oxford Research Ethics Committee C, reference 18/SC/0372), and has been linked to national mortality and hospitalisation (Hospital Episode Statistics; HES) data.
Sample and exposure
CRIS was used to extract data on patients aged 50 years or older who received a first diagnosis of dementia from SLaM outpatient services between 1st January 2008 and 31st December 2017. Dementia diagnosis date and other data of interest were extracted either from structured fields in the source record or from free-text clinical documents through natural language processing (NLP) algorithms using General Architecture for Text Engineering (GATE) software (Cunningham, Citation2002; Perera et al., 2016).
A GATE-supported NLP algorithm (Cunningham, Citation2002; Perera et al., 2016) was used to extract data on medications recorded in text fields (e.g. case notes, clinical correspondence) in a 6-month window before and after the dementia diagnosis as a measure of prevalent prescribing, supplemented by mentions in relevant structured fields from the record. Through this we identified subsamples of patients prescribed antidepressants and patients prescribed antipsychotics, who formed the two studied cohorts. Central anticholinergic burden in the antidepressant and antipsychotic cohort was quantified using the AEC scale (Bishara et al., Citation2017, Citation2020). Antidepressants and antipsychotics classified by AEC score are presented in Supplementary Table 1. According to the recommendations of this scale (Bishara et al., Citation2017) we created the following control and exposure groups based on the antidepressants/antipsychotics received: ‘No Central Anticholinergic’ (NCA), ‘Caution Required’ (CR), ‘Review Needed’ (RN).
Outcomes
From linked HES data we ascertained any unplanned or emergency hospitalisations to acute hospitals in the follow up time available. Mortality and hospitalisation data were available for all admission episodes in England until a censoring point on 31st March 2018.
Cognitive trajectory was measured from recorded Mini-Mental State Examination scores (Folstein et al., Citation1975), extracted from structured fields and a bespoke natural language processing algorithm (Mueller et al., Citation2021; Perera et al., Citation2014). Rate of cognitive decline was obtained using Generalised Estimated Equations (GEE) models (Liang & Zeger, Citation1986), whereby the dependent variable was the MMSE score modelled as longitudinal data. MMSE scores were included if these were measured from 6 months before dementia diagnosis (index date) to 18 months after dementia diagnosis and categorised into 3-month time periods. Patients were included if they had at least one MMSE score point in this two-year time-window. If a patient had more than one MMSE score point during a given 3-month period, average of MMSE was obtained. GEE models provide population-average effects of cognitive deterioration in terms of MMSE score decline per year. MMSE distribution for the GEE model was assumed to have Gaussian distribution and rate of MMSE decline was obtained in unadjusted and adjusted for confounding variables in models described below.
Covariates
Covariates ascertained at the time of dementia diagnosis included socio-demographic variables (age, sex, ethnicity (dichotomised to White and Non-White), marital status (dichotomised to cohabiting and non-cohabiting), and a neighbourhood-level index of multiple deprivation (IMD) (Noble et al., Citation2007). The IMD combines area-level indicators of deprivation across the domains of income, employment, health, disability, education, housing deprivation, living environment, and crime (Tsamakis et al., Citation2021). In addition, the Mini-Mental State Examination (MMSE) score was applied as a measure of cognition and approximated dementia severity closest to dementia diagnosis.
Mental health symptoms and functioning measures were extracted from the Health of the Nation Outcome Scales (HoNOS) instrument, routinely used in UK dementia assessment services, and we dichotomised subscales to ‘no problem or minor’ (scores 0–1) and ‘mild to severe problems’ (scores 2–4) (Mueller et al., Citation2018b), apart from the HoNOS subscale for physical illness or disability’ which was grouped into ‘no or minor’ (score 0–1), ‘mild’ (2), and ‘moderate to severe’ (3–4) categories. Because of previously described associations with cognitive trajectories (Perera et al., Citation2014) and survival (Mueller et al., Citation2018b), we ascertained recorded acetylcholinesterase inhibitor (AChEI) use within the first 6 months after dementia diagnosis.
We applied the AEC scale (Bishara et al., Citation2017) to control for central anticholinergic effects, which were caused by medications other than the studied antidepressants or antipsychotics. We calculated the total AEC score generated through all medications the patient was prescribed and subtracted the AEC score attributable to antidepressant or antipsychotic prescription respectively. The resulting variable was included as ordinal co-variate in our multivariable analyses. Lastly, we determined whether patients had hospital admissions with relevant circulatory diseases (ICD-10 discharge diagnoses: I20–25, I50, I60–69) in the 2 years before dementia diagnosis.
Statistical analyses
STATA 13 software (Stata Corp LP, College Station, TX, USA) was used for all analyses. In each cohort, we used two different approaches to define exposure. First, we compared those in the RN and CR groups individually with the NCA reference. In a second step we compared the RN group to a combined reference group (NCA + CR).
Multivariable Cox regression models were used to calculate associations with mortality (to 31st March 2018) and emergency hospitalisation and the aforementioned Generalised Estimated Equations (GEE) models to examine cognitive decline. Besides a crude (unadjusted) model, we created two multivariable models. Model 1 adjusted for age, sex, ethnicity, marital status, MMSE score (except in analyses of cognitive decline), neighbourhood deprivation, additional anticholinergic burden, and whether the patient was prescribed and additional antipsychotic or antidepressant respectively (analyses of antidepressant users were adjusted for co-prescription of an antipsychotic and vice versa). Model 2 additionally adjusted for HoNOS symptom and functioning scores, AChEI use and previous circulatory disease hospitalisation. Associations in Cox regression models are reported as hazard ratios with 95% confidence intervals and in GEE models as average MMSE decline per year as well as the resulting slope differences between exposure groups.
Thirty two percent of patients included in mortality and hospitalisation analyses had missing data on at least one of the covariates. Most frequently missing were MMSE scores, whereby in 17% of the sample MMSE was the only missing co-variate. Assuming ‘missingness’ to be random, we imputed missing values using chained equations to maximise statistical power (Oudshoorn et al., Citation1999). Using the mi package in STATA we created 32 imputed datasets through replacing missing values through simulated values assembled from potential covariates and outcome values. Rubin’s rules (Rubin, Citation2004) were applied to combine coefficients in the final analyses. For cognitive decline analyses we did not impute MMSE scores, and instead excluded patients who didn’t have an MMSE score recorded between 6 months before and 18 months after dementia diagnosis. This led to a smaller sample with lower overall missingness.
Sensitivity analyses
Because it was anticipated that a significant proportion of older adults might be prescribed low dose amitriptyline (which falls into the RN category) for neuropathic pain or insomnia rather than depression, we re-analysed data after excluding patients receiving this agent. In addition, as there was a substantial subpopulation of 1,108 patients recorded as taking both an antidepressant and antipsychotic at the same time, we analysed the influence of centrally-acting anticholinergic burden in this group.
Results
In the observation period we ascertained a cohort of 15,210 patients with a first diagnosis of dementia, who were followed up for 3.0 (SD +/-2.3) years until census or death. Characteristics of the sample and subgroups are described in and further sub-cohort generation in the flow chart in . In total 11,928 patients (78.4%) had at least one MMSE score point recorded in the window between 6 months before to 18 months after dementia diagnosis.
Figure 1. Flow chart of cohort generation.
Note: The Anticholinergic Effect on Cognition (AEC) Scale- The relationship between AEC scores and Mortality, Hospitalisation and Cognitive Function for patients with dementia on Antidepressants or Antipsychotics
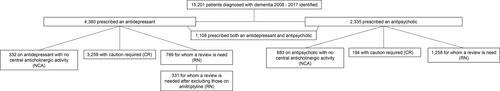
Table 1. Patient characteristics in the whole cohort and in those prescribed antidepressants and antipsychotics.
Antidepressant cohort
In total 4,380 patients (28.8% of the whole cohort) were prescribed an antidepressant around the time of dementia diagnosis. Of this cohort, 7.6% (n = 332) were prescribed an antidepressant with no centrally-acting anticholinergic activity (NCA), 74.4% (n = 3,259) were on an antidepressant that fell into the caution required (CR) category and for 18.0% (n = 789) their antidepressant use was classified as having an anticholinergic burden where a review would be recommended (RN). Differences between exposure groups according to central anticholinergic burden of the antidepressant are presented in .
Table 2. Characteristics of patients with dementia on antidepressants according to anticholinergic burden.
In this cohort 2,434 (55.6%) died during follow up. The median survival time was 3.8 years (interquartile range 1.5–6.9), the median time to first hospitalisation was 1.2 years (interquartile range 0.3–4.2), and 3,112 patients (71.1%) had at least one non-elective hospitalisation in the follow up period.
Associations of antidepressant-related central anticholinergic burden with mortality and hospitalisation outcomes are presented in . After full adjustment (model 2) there was a significantly reduced risk of mortality in the RN group compared to the combined NCA and CR groups (HR: 0.88; 95% CI 0.79-0.98; p = 0.023). However, when the RN group was compared to the CR and NCA groups individually, the reduced risk of mortality was not significant after adjustment of covariates No significant associations were found between antidepressant-related central anticholinergic burden and emergency hospitalisation. Excluding the 458 patients on amitriptyline from the RN group (Supplementary Table 2) yielded largely similar results: although in the fully adjusted model 2 the reduced risk of mortality in the RN compared to the combined NCA + CR groups was no longer significant, though effect sizes were similar (HR: 0.87; 95% CI 0.74-1.01; p = 0.071).
Table 3. Cox regression models of associations with central anticholinergic burden and adverse outcomes in patients on antidepressants (n = 4,380/3,415).
Comparisons between those included and excluded in analyses of cognitive trajectories are presented in Supplementary Table 3. Patients with RN, CR and NCA antidepressants declined by 0.40, 1.57, and 3.44 MMSE score points per year respectively in the fully adjusted model (Supplementary Table 4). Slope differences are presented in . Compared to patients on antidepressants in the NCA group only or in the NCA and CR groups combined, patients on an antidepressant in the RN group declined significantly slower in all three models. After excluding patients on amitriptyline, statistically significant slope differences were only detected in the fully adjusted model when comparing the RN to the NCA antidepressant group (Supplementary Table 2).
Antipsychotic cohort
Antipsychotic prescribing around the time of dementia diagnosis was present in 2,335 patients (15.4% of the whole cohort). Of this cohort, 37.8% (n = 883) were on an antipsychotic classified as having no centrally-acting anticholinergic burden (NCA), 8.3% (n = 194) on an antipsychotic in the caution required category (CR) and for 53.9% (n = 1,258) the antipsychotic related central anticholinergic burden was where a review would be recommended (RN). Differences between exposure groups according to anticholinergic burden of the antipsychotic are presented in .
Table 4. Characteristics of patients with dementia on antipsychotics according to anticholinergic burden.
In this cohort 1,408 (60.3%) people died during follow up. The median survival time was 3.5 years (interquartile range 1.3–6.7), the median time to first hospitalisation was 1.2 years, interquartile range (0.3–4.5 years) and 1,685 patients (72.2%) had at least one non-elective hospitalisation in the follow up period.
Associations of antipsychotic-related central anticholinergic burden with mortality and hospitalisation outcomes are presented in . While in unadjusted analyses and model 1 there was a reduced mortality risk in the RN compared to combined NCA and CR groups, this was no longer statistically significant after adjustment for a wider range of potential confounders in model 2 (HR: 0.91; 95% CI 0.82-1.02; p = 0.105). However, when comparing the CR and RN groups individually to the NCA reference, both had a significantly lower mortality risk in all models (for RN vs. NCA in model 2: HR: 0.88; 95% CI: 0.78-0.98; p = 0.023). No significant associations were detected between antipsychotic-related central anticholinergic burden and emergency hospitalisation.
Table 5. Cox regression models of associations with central anticholinergic burden and adverse outcomes in patients on antipsychotics (n = 2,335/1,691).
In analyses of cognitive trajectories, those in the RN, CR and NCA groups declined by 2.00, 0.68, and 2.30 MMSE score points per year respectively in fully adjusted models (Supplementary Table 4). No significant slope differences were present between groups ().
Combined antidepressant and antipsychotic cohort
Of antidepressant users 25.3% were also on an antipsychotic and of antipsychotic users 47.5% were co-prescribed an antidepressant. Combined use of antidepressant and antipsychotic was present in 1,108 patients around the time of dementia diagnosis (7.3% of the whole cohort). Of those, 40 (3.6%) had no central anticholinergic burden related to antidepressant and antipsychotic use, 265 (23.9%) were in the CR group and 803 (72.5%) in the RN group (see ). After confounder adjustment no association between anticholinergic burden and mortality or emergency hospitalisation was detected in this group (see ). The very small group of those with no central anticholinergic burden declined by 8.62 MMSE score points per year, while the CR group declined by 0.19 and the RN group by 1.42 MMSE score points per year (see Supplementary Table 4). When combined NCA + CR group was compared to the RN group no significant difference in cognitive decline slope was seen (see ).
Table 6. Associations of central anticholinergic burden and adverse outcomes in patients on antidepressants and antipsychotics (n = 1,108/823).
Discussion
Because it is unclear whether previously reported poor outcomes associated with anticholinergic drugs were due to the drugs themselves or to the illnesses they were treating (Andrade, Citation2019; Coupland et al., Citation2019), we sought to compare outcomes solely amongst patients receiving these classes of drugs in order to reduce confounding by indication.
In this study of antidepressant and antipsychotic users with dementia, we aimed to test the hypothesis that high central anticholinergic burden associated with these agents would be related to adverse outcomes. In summary, no evidence for this was found, with all associations either null or in the opposite direction to that anticipated. Other studies have found an increased risk of mortality in people with dementia taking anticholinergic drugs (Mcmichael et al., Citation2020; Tan et al., Citation2018). However, these studies were not restricted to specific classes of drugs such as antidepressants and antipsychotics. Similarly, we looked at the effect of all anticholinergic drugs (with no restrictions) in our previous study (Bishara et al., Citation2020) and found that high anticholinergic burden was associated with poorer outcomes. Differences in the results could also be due to other studies having used primary care databases instead, having larger populations or having used different anticholinergic burden scales that do not focus on central action.
The antidepressant RN group with highest central anticholinergic burden had significantly lower rather than higher mortality risk in both comparison analyses. Reasons for this may be complex. The majority of patients in the antidepressant cohort fell into the CR category, where the central anticholinergic burden is not deemed clinically significant enough to require a change of medication, and this imbalance in group sizes may have rendered the results unstable. Excluding patients on low dose amitriptyline did not appear to influence the results substantially. It should also come as no surprise that antidepressants reduce mortality in depression (Jorge et al., Citation2003; Taylor et al., 2005). Also, it is widely known that even antidepressants with low anticholinergic burden such as SSRIs can increase mortality through other effects e.g. gastrointestinal bleeds (Paton & Ferrier, Citation2005) and mirtazapine (AEC score of 1) is often reserved for patients who are seriously ill or have contraindications to other antidepressants. It is very possible that other properties of different antidepressants may influence choice of prescribing and that there may be other confounding factors not considered. The type of illnesses being treated with anticholinergic drugs may also influence patient outcomes in dementia. Also, many of the studies on mortality risk of psychotropic drugs were done in primary care. One might argue that as the patients in our study were under secondary care, they may have received better monitoring which might mitigate risks and reduce mortality. Perhaps these drugs were more likely to be stopped after they had ceased to be useful or because the data were collected over many years, changing in prescribing habits had already occurred and high-risk drugs were avoided in vulnerable patients.
For the antipsychotic cohort, mortality risk was also lower in the RN group compared to the NCA group, as well as in the CR group. Antipsychotics with lower central anticholinergic burden include risperidone and haloperidol. The higher risks could be due to these agents being used for behavioural and psychological symptoms of dementia (or delirium for haloperidol) and therefore reserved for patients with a more severe illness. This could explain why antipsychotics with low central anticholinergic action were associated with higher mortality.
No significant associations were detected either between antidepressant-related or antipsychotic-related central anticholinergic burden and emergency hospitalisation, whereas in our previous paper examining this relationship for all classes of drugs, we found a marginally increased risk of hospitalisation (Bishara et al., Citation2020). Therefore, it does not appear that central anticholinergic burden for antidepressants or antipsychotics is a factor influencing hospitalisation in patients with dementia. As already discussed, psychotropics with low central anticholinergic burden are often used in more seriously ill patients, therefore an association with hospitalisation would be difficult to ascertain.
Again, contrary to our hypothesis, patients on an antidepressant in the NCA category had an accelerated cognitive decline compared to the RN group, and those on an antipsychotic showed no group differences in trajectory. It is important to bear in mind that both antidepressant-related and antipsychotic-related NCA groups had lowest mean MMSE scores around the time of dementia diagnosis (see and ), so the counter-intuitive findings for trajectories might reflect a later stage of presentation. On the other hand, previous studies in patients with established dementia have also failed to find any differences on cognitive decline between anticholinergic exposure groups (Bishara et al., Citation2020; Fox et al., Citation2011a). Moreover, we cannot exclude whether these patients had a concurrent delirium, which would have affected their cognitive scores.
The sensitivity analysis examining patients prescribed both antidepressant and antipsychotic drugs together found no association between anticholinergic burden and mortality, emergency hospitalisation or cognitive decline after confounder adjustment. This strengthens the argument that other receptor activities or drug actions may also be at play with regards to adverse outcomes in dementia.
Strengths of this study include the large naturalistic sample, the wide range of potential confounders considered, and linkage to what should be near-complete national data on mortality and hospitalisation. The following limitations, however, need to be acknowledged. First, anticholinergic use was evaluated based on medications used at the baseline assessment and any changes in prescribing occurring during the study period were not assessed. This is possibly the most important limitation in this study, as exclusively considering exposure to medication with a high centrally active anticholinergic burden around the time of diagnosis leads to individuals prescribed those medications in a later stage of dementia not being considered as exposed. This could potentially bias estimates towards the null and could contribute to some of the null findings in our study. Second, cognitive function was only investigated from recorded MMSE scores, which can be limited by both floor effects in those with more severe dementia and ceiling effects when used in individuals with higher educational attainment (Monroe & Carter, Citation2012). Third, comorbidity was determined with the HoNOS physical illness subscale, which is relatively brief without details on specific long-term conditions, although the subscale has been shown to a have predictive validity for unfavourable outcomes in this patient population (Mueller et al., Citation2018a, Citation2018b). Fourth, other potential risk factors for adverse outcomes and cognitive decline such as level of education were not directly captured, and socio-economic status was only estimated at neighbourhood-level (Noble et al., Citation2007). Fifth, an important limitation of the AEC scale is that it doesn’t take dose into account. Sixth, our results may also be affected by residual confounders which we were unable to adjust for, such as medication adherence or use of over-the-counter medications, although we did adjust for additional anticholinergic burden generated from other drug classes. Finally, due to the number and complexities of our analyses, we did not carry out additional subgroup analyses according to dementia type, however this will be considered in future research projects.
In conclusion, our counter-intuitive findings may reflect factors underlying the choice of psychotropic agents rather than the agents themselves. These results do not support a strong role for central anticholinergic drug actions on antidepressant- or antipsychotic-related dementia outcomes. Both antidepressants and antipsychotics act on a wide range of receptors and have broad mechanisms of action. It is possible that other mechanisms at play are producing stronger effects on mortality than anticholinergic properties in these groups of drugs such as QTc prolongation with both antidepressants and antipsychotics or increased risk of cerebrovascular accidents with antipsychotic drugs. Further studies investigating outcomes in patients with dementia taking antidepressant and antipsychotic drugs are needed in order to investigate these relationships further: for example, evaluations of a randomized switch from agents with higher to lower centrally-acting anticholinergic activity.
Supplemental Material
Download MS Word (34.5 KB)Disclosure statement
RS declares research support received in the last 36 months from Janssen, GSK and Takeda.
DT declares research support from Janssen Pharmaceuticals and Lundbeck and has received speaking honoraria from Janssen, Lundbeck, Sunovion, and Recordati.
DB has received financial remuneration for lectures from Healthcare Conferences UK; and for consultancy on guidelines from Contura.
Funding
No funding was received for this project. DB and RS are part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
References
- Andrade, C. (2019). Anticholinergic drug exposure and the risk of dementia: There is modest evidence for an association but not for causality. The Journal of Clinical Psychiatry, 80, 19f13000.
- Bishara, D., Harwood, D., Sauer, J., & Taylor, D. M. (2017). Anticholinergic effect on cognition (AEC) of drugs commonly used in older people. International Journal of Geriatric Psychiatry, 32(6), 650–656. https://doi.org/10.1002/gps.4507
- Bishara, D., Perera, G., Harwood, D., Taylor, D., Sauer, J., Stewart, R., & Mueller, C. (2020). The anticholinergic effect on cognition (AEC) Scale: Associations with mortality, hospitalisation and cognitive decline following dementia diagnosis. International Journal of Geriatric Psychiatry, 35(9), 1069–1077. https://doi.org/10.1002/gps.5330
- Coupland, C. A. C., Hill, T., Dening, T., Morriss, R., Moore, M., & Hippisley-Cox, J. (2019). Anticholinergic drug exposure and the risk of dementia: A nested case-control study. JAMA Internal Medicine, 179(8), 1084–1093. https://doi.org/10.1001/jamainternmed.2019.0677
- Cunningham, H. (2002). GATE, a general architecture for text engineering. Computers and the Humanities, 36(2), 223–254. https://doi.org/10.1023/A:1014348124664
- Folstein, M. F., Folstein, S. E., & Mchugh, P. R. (1975). Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. https://doi.org/10.1016/0022-3956(75)90026-6
- Fox, C., Livingston, G., Maidment, I. D., Coulton, S., Smithard, D. G., Boustani, M., & Katona, C. (2011a). The impact of anticholinergic burden in Alzheimer’s Dementia: The Laser-AD Study. Age and Ageing, 40(6), 730–735. https://doi.org/10.1093/ageing/afr102
- Fox, C., Richardson, K., Maidment, I. D., Savva, G. M., Matthews, F. E., Smithard, D., Coulton, S., Katona, C., Boustani, M. A., & Brayne, C. (2011b). Anticholinergic medication use and cognitive impairment in the older population: The medical research council cognitive function and ageing study. Journal of the American Geriatrics Society, 59(8), 1477–1483. https://doi.org/10.1111/j.1532-5415.2011.03491.x
- Jorge, R. E., Robinson, R. G., Arndt, S., & Starkstein, S. (2003). Mortality and poststroke depression: A placebo-controlled trial of antidepressants. American Journal of Psychiatry, 160(10), 1823–1829. https://doi.org/10.1176/appi.ajp.160.10.1823
- Liang, K.-Y., & Zeger, S. L. (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73(1), 13–22. https://doi.org/10.1093/biomet/73.1.13
- Mcmichael, A. J., Zafeiridi, E., Ryan, M., Cunningham, E. L., Passmore, A. P., & Mcguinness, B. (2020). Anticholinergic drug use and risk of mortality for people with dementia in Northern Ireland. Aging & Mental Health, 1–8. https://doi.org/10.1080/13607863.2020.1830028
- Monroe, T., & Carter, M. (2012). Using the Folstein Mini Mental State Exam (MMSE) to explore methodological issues in cognitive aging research. European Journal of Ageing, 9(3), 265–274. https://doi.org/10.1007/s10433-012-0234-8
- Mueller, C., Huntley, J., Stubbs, B., Sommerlad, A., Carvalho, A. F., Perera, G., Stewart, R., & Veronese, N. (2017). Associations of neuropsychiatric symptoms and antidepressant prescription with survival in Alzheimer’s disease. Journal of the American Medical Directors Association, 18(12), 1076–1081. https://doi.org/10.1016/j.jamda.2017.07.001
- Mueller, C., John, C., Perera, G., Aarsland, D., Ballard, C., & Stewart, R. (2020). Antipsychotic use in dementia: The relationship between neuropsychiatric symptom profiles and adverse outcomes. European Journal of Epidemiology, 36(1), 89–101.
- Mueller, C., John, C., Perera, G., Aarsland, D., Ballard, C., & Stewart, R. (2021). Antipsychotic use in dementia: The relationship between neuropsychiatric symptom profiles and adverse outcomes. European Journal of Epidemiology, 36(1), 89–101. https://doi.org/10.1007/s10654-020-00643-2
- Mueller, C., Molokhia, M., Perera, G., Veronese, N., Stubbs, B., Shetty, H., Codling, D., Huntley, J., & Stewart, R. (2018a). Polypharmacy in people with dementia: Associations with adverse health outcomes. Experimental Gerontology, 106, 240–245. https://doi.org/10.1016/j.exger.2018.02.011
- Mueller, C., Perera, G., Hayes, R. D., Shetty, H., & Stewart, R. (2018b). Associations of acetylcholinesterase inhibitor treatment with reduced mortality in Alzheimer’s disease: A retrospective survival analysis. Age and Ageing, 47(1), 88–94. https://doi.org/10.1093/ageing/afx098
- Noble, M., Mclennan, D., Wilkinson, K., Whitworth, A., Exley, S., Barnes, H., Dibben, C., & Mclennan, D. (2007). The English Indices of Deprivation, 2007. Unknown Publisher.
- Oudshoorn, C. G. M., Buuren, S., & Rijckevorsel, J. L. A. (1999). Flexible multiple imputation by chained equations of the AVO-95 survey. TNO Prevention and Health Leiden.
- Paton, C., & Ferrier, I. N. (2005). SSRIs and gastrointestinal bleeding. BMJ, 331(7516), 529–530. https://doi.org/10.1136/bmj.331.7516.529
- Perera, G., Broadbent, M., Callard, F., Chang, C. K., Downs, J., Dutta, R., Fernandes, A., Hayes, R. D., Henderson, M., Jackson, R., Jewell, A., Kadra, G., Little, R., Pritchard, M., Shetty, H., Tulloch, A., & Stewart, R. (2016). Cohort profile of the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Case Register: Current status and recent enhancement of an Electronic Mental Health Record-derived data resource. BMJ Open, 6(3), e008721. https://doi.org/10.1136/bmjopen-2015-008721
- Perera, G., Khondoker, M., Broadbent, M., Breen, G., & Stewart, R. (2014). Factors associated with response to acetylcholinesterase inhibition in dementia: A cohort study from a secondary mental health care case register in London. PLOS One, 9(11), e109484. https://doi.org/10.1371/journal.pone.0109484
- Richardson, K., Fox, C., Maidment, I., Steel, N., Loke, Y. K., Arthur, A., Myint, P. K., Grossi, C. M., Mattishent, K., Bennett, K., Campbell, N. L., Boustani, M., Robinson, L., Brayne, C., Matthews, F. E., & Savva, G. M. (2018). Anticholinergic drugs and risk of dementia: Case-control study. BMJ (Clinical Research ed.), 361, k1315. https://doi.org/10.1136/bmj.k1315
- Rubin, D. B. (2004). Multiple imputation for nonresponse in surveys. John Wiley & Sons.
- Saczynski, J. S., Beiser, A., Seshadri, S., Auerbach, S., Wolf, P. A., & Au, R. (2010). Depressive symptoms and risk of dementia: The Framingham Heart Study. Neurology, 75(1), 35–41. https://doi.org/10.1212/WNL.0b013e3181e62138
- Stewart, R., Soremekun, M., Perera, G., Broadbent, M., Callard, F., Denis, M., Hotopf, M., Thornicroft, G., & Lovestone, S. (2009). The South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLAM BRC) case register: Development and descriptive data. BMC Psychiatry, 9, 51. https://doi.org/10.1186/1471-244X-9-51
- Tan, E., Eriksdotter, M., García-Ptacek, S., Fastbom, J., & Johnell, K. (2018). Anticholinergic burden and risk of stroke and death in people with different types of dementia. Journal of Alzheimer’s Disease, 65(2), 588–589. https://doi.org/10.3233/JAD-180353
- Taylor, C. B., Youngblood, M. E., Catellier, D., Veith, R. C., Carney, R. M., Burg, M. M., Kaufmann, P. G., Shuster, J., Mellman, T., Blumenthal, J. A., Krishnan, R., Jaffe, A. S., & ENRICHD Investigators. (2005). Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Archives of General Psychiatry, 62(7), 792–798. https://doi.org/10.1001/archpsyc.62.7.792
- Tsamakis, K., Gadelrab, R., Wilson, M., Bonnici-Mallia, A. M., Hussain, L., Perera, G., Rizos, E., Das-Munshi, J., Stewart, R., & Mueller, C. (2021). Dementia in people from ethnic minority backgrounds: Disability, functioning, and pharmacotherapy at the time of diagnosis. Journal of the American Medical Directors Association, 22(2), 446–452. https://doi.org/10.1016/j.jamda.2020.06.026
