 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objectives
Mental health for older people has become a major social concern. Literature has shown that older people, especially when they become empty nesters—when a parent lives alone or lives with his/her spouse after the youngest child leaves home—may start to develop various mental health problems due to reduced contacts with their children.
Using fixed-effects, multivariate regression with a difference-in-differences approach and propensity score matching, this paper examines the relationship between being an empty nester and mental health among older people in China, and the moderating effects of social contact and contact with one’s children in terms of mental health. Our data come from the China Health and Retirement Longitudinal Study of 2011, 2013, 2015 and 2018.
Results
We found that, in the short term, the mental health of older people may not be affected after they became empty nesters. But in the longer term, if they did not have regular contact with their children, their mental health would deteriorate with time. Social contact, especially cognitive activities, was beneficial to the mental health of the older empty nesters. We also found that for older empty nesters with disabilities, frequent social contact and contact with their children were more important.
Conclusion
We urge the government to promote community-based social activities for older people, especially for those with functional limitations.
Introduction
Population ageing has become a global phenomenon in the past few decades. The United Nations Population Fund (UNPFA) estimates that people aged 60 and above will account for approximately 22% of the world’s population by 2050 (UNFPA and HelpAge International, Citation2012). Along with global ageing, mental health for older people has become a social concern in many countries (World Health Organization, Citation2017a). Around the world, over 20% of the older people aged 60 and above suffer from at least one mental or neurological disorder, and 6.6% of the disabilities among those older than 60 are attributed to mental and neurological disorders (World Health Organization, Citation2020). In China, mental health disorders have brought significant burdens to the society during the recent decades (Liang et al., Citation2018; Xiang et al., Citation2012). Literature has shown that older people, especially when they become empty nesters—when a parent lives alone or lives with his/her spouse after the youngest child leaves home (Lowenthal & Chiriboga, Citation1972)—may start to develop various mental health problems due to reduced contacts with their children (Guo et al., Citation2016; Zhai et al., Citation2015). Strengthening and promoting mental health of older people has been recognised as a health system priority in many countries (World Health Organization, Citation2017b).
Living arrangements play an important role for older people’s mental health. In high-income countries (HICs), the proportion of older people live independently is higher than in low- and middle-income countries (LMICs). This could be attributed to cultural factors, individual choices as well as established long-term care (LTC) and public support systems (Gaymu et al., Citation2006). Due to the traditional norm of filial piety, older people in many East Asian countries, including China, prefer to live with their children (You et al., Citation2009); however, this living arrangement has changed dramatically in the past few decades according to recent data (National Bureau of Statistics of China, Citation2020). Empty nesters accounted for over half of the older population in 2014, and this figure is expected to reach 90% by 2030 (Chang et al., Citation2016). In the rural China, many older people have become empty-nesters because of the mass rural to urban migration of younger generations since the 1990s. In the urban China, the younger generations also tend to live independently due to changing family structure and pursuing of freedom (Chen, Citation2019; Sun et al., Citation2011). The association between empty-nest and mental health has been explored for decades but no consistent findings have been established. Some found that due to the sense of loss and role change, some empty-nesters may experience temporal depression because they need to adapt themselves to the new living arrangement (Aranda, Citation2015; Lee et al., Citation2017; Oliver, Citation1977; Xu, Citation2018). Others found that empty nesters have better mental health due to a sense of relief and reduction of caring burden, but only conditional on the fact that they remain frequent contacts with nonresident children (Dennerstein et al., Citation2002; Radloff, Citation1980; White & Edwards, Citation1990).
Social contact and contact with one’s children are believed to have critical impacts on older people’s mental health. According to the stress-buffering model, the availability of social contact may eliminate or weaken the negative association between perceived stress as a result of becoming an empty nester and psychological wellbeing (Gellert et al., Citation2018). The stress-buffering hypothesis has been tested in a number of studies, which show that social contact or social support may potentially act as a source of destress as well as a source of satisfaction (Bennett et al., Citation2006; Cho et al., Citation2016; Dias et al., Citation2015). Social contact, such as participation in community events and involvement in social networks, benefits mental health by receiving positive social influence (e.g. guidance about health-related behaviours, such as regular exercises), producing positive affective states (e.g. a sense of purpose, belonging and security) and modulating neuroendocrine responses to stress (Cohen & Wills, Citation1985; Kawachi & Berkman, Citation2001; Roberts et al., Citation1994).
No consistent conclusion has been established on the influence of contact with one’s children on mental health. Studies suggest that emotional support from children will improve the mental health of older people due to increased feelings of closeness (Tosi & Grundy, Citation2019), but excessive children contact may harm the mental health of older people since more frequent contacts often lead to more disagreements due to varied opinions and life styles (Beckman, Citation1981; Litwin, Citation2004).
Although the existing literature has examined the determinants of older people’s mental health, limited empirical evidence has been demonstrated on the moderating effects of social contact and contact with one’s children for the relationship between becoming empty-nester and one’s mental health. Even less is known on how this relationship varies among empty nester with different health and LTC needs, such as people with or without functional limitations. Furthermore, existing literature mainly looks at the short-term effects on older people’ mental health after they become empty nesters (Lee et al., Citation2017; Zhai et al., Citation2015), but longer-term outcomes remain unassessed. Using China as an example, where filial piety and intergenerational support play crucial roles in the later periods of life, we aim to fill in these research gaps by examining this relationship and the moderating effect of social contact and contact with one’s children. We are particularly interested in knowing whether older people with functional limitations are more likely to experience mental health problems after becoming empty nesters, and how the impact of becoming an empty nester on one’s mental health has changes over time.
Data source and sample selection
We drew data from the CHARLS (CHARLS, Citation2020), a nationwide survey targeted at people aged 45 and older in China; it provides individual-level panel data on health, socio-economic status, as well as social and family networks (Zhao et al., Citation2013). We used data from 2011, 2013, 2015 and 2018. In addition, we merged these longitudinal data with economic data (provincial GDP per capita) from China’s National Bureau of Statistics (National Bureau of Statistics of China, Citation2020).
We selected 11,319 observations in our sample according to the following criteria: Equation(1)(1)
(1) older people aged 60 and above; Equation(2)
(2)
(2) individuals who lived with children in all the years they were enrolled in the study (the control group), and individuals who lived with their children in the first year and lived alone or with their spouse in the last year (the treatment group). For instance, 1,537 individuals were enrolled in the survey for all four years, among whom 236, 573 and 889 became empty nesters in 2013, 2015 and 2018, respectively. In addition, we do not include individuals who only lived with their parents or grandchildren, and not lived with their children based on the definition of the empty nester. Other details of the living arrangements of the study sample are shown in .
Table 1. Summary statistics of the living arrangements of individuals included in our sample in each year.
Variable specifications
Our dependent variable was the depression score, which was calculated based on the 10-item Center for Epidemiologic Studies Depression Scale Revised (CESD-R-10). Survey participants were asked to rate eight negative statements (e.g. I felt fearful) and two positive statements (e.g. I felt hopeful) which indicates their mental health status for the past week. Each statement was measured on the following scale: 0 = less than one day, 1 = one to two days, 2 = three to four days, and 3 = five to seven days. We reverse scored the two positive statements and added up the scores of the ten statements, which enabled us to create a depressive symptoms variable ranging from 0 (no symptoms) to 30 (severe symptoms).
Our independent variable of interest is the empty nester. Following the well-established definition in the literature, we defined empty nesters as those who previously lived with their children, but then lived alone or with their spouses (Lowenthal & Chiriboga, Citation1972; Oliver, Citation1977). In this study, we defined empty nesters (the treatment group) as individuals who lived with children in the first year(s) but lived alone or with their spouses in the last year(s). We defined the control group as people who lived with their children throughout the study period. Social contact has been widely acknowledged as a main factor of mental health status (Kawachi & Berkman, Citation2001; Roberts et al., Citation1994). We considered an observation to have social contact if any of the following activities happened: interacting with friends, playing mah-jong/cards/chess, providing help to others, going to a club, taking part in a community-related organisation, doing voluntary work, caring for a sick or disabled adult, attending a course, investing in stocks, and using the Internet (0 = no social contact, 1 = at least one type of social contact). In addition, we divide the above activities of social contact into two types according to the literature (Stern & Munn, Citation2010; Weaver & Jaeggi, Citation2021), 1 = social activities (interacting with friends, providing help to others, going to a club, taking part in a community-related organisation, doing voluntary work, and caring for a sick or disabled adult) and 2 = cognitive activities (playing mah-jong/cards/chess, attending a course, investing in stocks, and using the Internet).
We controlled for the following variables that could influence a person’s depressive symptoms. Firstly, we include a set of demographic and physical health-related variables: including age, gender, the number of chronic diseases, self-perceived health status (1 = excellent/very good, 2 = good, 3 = fair/poor), whether to have one or more activities of daily living (ADL) limitations or instrumental ADL (IADL) limitations (0 = no limitations, 1 = at least one ADL/IADL limitation), and whether one is currently feeling bodily pain (Ohrnberger et al., Citation2017). Secondly, we also include a set of socio-economic variables: level of education (1 = no formal education, 2 = elementary and middle school, 3 = high school or above), quartiles of equivalent income (household income divided by the square root of household size (OECD, Citation2011)), marital status (0 = married/cohabiting, 1 = single), provincial GDP per capita, and residence area (1 = rural, 2 = urban). We do additionally robustness check analyses by replacing provincial GDP per capita with city-level GDP per capita. Results show that our analyses are robust to it (see Appendix A).
Empirical strategies
We used fixed-effects multivariate regression by adopting a difference-in-differences (DID) approach with propensity score matching (PSM) to explore the in-depth relationship between depressive symptoms and being an empty nester. The settings were DID with staggered adoption since treatment timing varied by individuals, i.e. some became empty nesters in 2013, whereas others became empty nesters in 2015 or 2018 (Athey & Imbens, Citation2022; Callaway & Sant’Anna, Citation2021; Goodman-Bacon et al., Citation2019). We performed a parallel trend test between the treatment and control groups, which demonstrates that the parallel trend assumption holds (Wooldridge, Citation2012) (see detailed results in Appendix B). The analyses we performed are shown as follows. Besides, the varied effects of being empty nesters on depressive symptoms between the rural and the urban were also explored as presented in Appendix C.
Analysing the impact of being an empty nester on depressive symptoms
We first assumed that the average treatment effects on the treated (ATT) would be constant across each period after treatment; in other words, we assumed that people’s depressive symptoms would be equally impacted, regardless of whether they became empty nesters for one wave, two waves or three waves (Wooldridge, Citation2012). However, this may not be the case in real life, since mental health status may be associated with how much time has passed since a person became an empty nester. Therefore, we allowed for variation in the ATT over time to determine whether the impact of being an empty nester on depressive symptoms varies with time (Laporte & Windmeijer, Citation2005). The models are presented as follows (constant ATT in Model 1; varied ATTs in Model 2):
(1)
(1)
(2)
(2)
In the two models, denotes the depression score, and
controls for the fixed effects of time.
and
indicate whether an individual
is an empty nester at time
. Specifically, assuming a constant ATT, Post 1 = 1 indicates that a person has become an empty nester, and Post 1 = 0 means that a person lives with his/her children. Assuming variation in the ATT, Post 2 = 3 denotes a person being an empty nester for three waves, Post 2 = 2 refers to a person being an empty nester for two waves, Post 2 = 1 indicates a person being an empty nester for one wave, and Post 2 = 0 denotes a person living with his/her children.
represents the following time-varying covariates: having social contact, having ADL/IADL limitations, number of chronic diseases, self-perceived health status, feeling bodily pain, quartiles of equivalent income, marital status and provincial GDP per capita. ν controls for individual fixed effects, including both observable (such as gender, birth year, level of education—which is almost constant for people aged 60 and above—and residence area) and unobservable fixed effects. ε is the idiosyncratic error term.
shows the DID estimate.
Analysing the impact of contact with one’s children on the association between depressive symptoms and being an empty nester
In the first analysis, we estimated an average treatment effect. However, varied characteristics among subgroups may modify the impact of a treatment on outcomes. Hence, we also explored the heterogeneity of the treatment effect in this second analysis (Chaisemartin & D’Haultfoeuille, Citation2020). To determine whether the frequency of contact with one’s children after becoming an empty nester was associated with depressive symptoms (i.e. whether the impact of being an empty nester differed between the subgroups by the frequency of contact with one’s children), we further divided the treatment group (the empty nesters) into two subgroups according to the literature (Stewart, Citation2003): 1) people who have contact with their children more than once a month, and 2) people who have contact with their children less than once every three months. The model is as follows:
(3)
(3)
In this model, Post 3 = 1, 2 or 3 indicates an empty nester for one wave, two waves or three waves, respectively, who has contact with his/her children more than once per month, Post 3 = 4, 5 or 6 denotes an empty nester for one wave, two waves or three waves, respectively, who has contact with his/her children less than once every three months, and Post 3 = 0 entails a person living with his/her children.
Analysing the impact of social contact on the association between depressive symptoms and being an empty nester
For our third analysis, we investigated the impact of social contact on the association between depressive symptoms and being an empty nester by further adding the interaction term between social contact and whether an individual i is an empty nester at time t in the models (Imbens & Wooldridge, Citation2007), which are displayed below:
(4)
(4)
(5)
(5)
In Model 4, denotes whether one has social contact. In model 5,
= 0 denotes a person has no social contact,
= 1 indicates one has social activities, and
= 2 entails a person has cognitive activities.
represents the following time-varying covariates:
, having ADLs/IADLs, number of chronic diseases, self-perceived health status, feeling bodily pain, quartiles of equivalent income, marital status and provincial GDP per capita.
demonstrates the effect of social contact on the association between depressive symptoms and being an empty nester.
Analysing the above impacts for the subgroup with at least one ADL/IADL limitation
We are interested in knowing for people with ADL/IADL limitations, when they become empty nesters, whether their mental health would be differently impacted and whether contact with one’s children or social contact would alleviate this impact. This additional test is important as the mental health of older people with ADL/IADL limitations may be more affected when becoming empty nesters as their live-in children are potential caregivers. When their children leave home, their care needs may not be met, and this may create stress and anxiety for them. Therefore, we repeat the above analyses for the subgroup with at least one ADL/IADL limitation to test whether social and children contacts will moderate the effect of becoming empty nesters among this group of older people.
In our study, we combined the DID approach with PSM to lower bias (Ravallion, Citation2007). To avoid selection bias, we matched them on the following variables in the pre-treatment periods (Caliendo & Kopeinig, Citation2008): birth year, gender, marital status, equivalent income, number of chronic diseases, ADL/IADL limitations, level of education, residence area and quartiles of provincial GDP per capita. We examined the matching quality according to the following three criteria: (1) the match rates for both groups were approximately 95% (Appendix D); (2) the propensity score density distributions for the matched groups were almost identical, indicating that after matching the two groups share common propensity score to be enrolled in the treatment, i.e. the two groups are comparable after matching (Appendix E); and (3) we further examined the standardised difference between the two groups after matching, which indicated that all differences were controlled around 0.1, meaning that the two groups were well balanced after matching (Austin, Citation2009; Rosenbaum & Rubin, Citation1985) (Appendix F).
Ethics considerations
This study uses publicly available secondary data; hence, no ethics approval is needed.
Results
According to the descriptive statistics in , around half of the empty nesters had contact with their children more than once a month, whereas the rest had contact with their children less than once every three months. In terms of social contact, more than 50% of our observations had no social contact at all. Based on the descriptive statistics, the proportion of the disabled in the group of empty nesters was smaller than that of the control group, possibly because the disabled were more likely to live with their children.
Table 2. Descriptive statistics.
The effects of being an empty nester on depressive symptoms are listed in (see Appendix G for full sets of regression results). Column 1 displays the DID estimate when we assumed a constant ATT, while Column 2 presents the results when we allowed for varied ATTs. When we assumed that being an empty nester would have the same effect on people’s depressive symptoms, regardless of how many waves they had been empty nesters for, we found that the depression score declined, though not significantly. However, when we allowed for being an empty nester to have different influences on depressive symptoms, people’s mental health was significantly negatively impacted after being an empty nester for two and three waves. In addition, we observed a more severe deterioration in mental health for empty nesters for three waves than for two waves.
Table 3. The impact of being an empty nester on depressive symptoms for people over 60.
In , we present our results for the impact of contact with one’s children, as well as social contact, on the association between depressive symptoms and being an empty nester (see Appendix H for full sets of regression results). As outlined in Column 1, the depression score increased significantly after people became empty nesters for two and three waves, but only when they had contact with their children less than once every three months. For people who contact/are contacted by their children more than once a month, their depressive symptoms were uniquely impacted by being an empty nester. For the effect of social contact seen in Columns 2 and 3, compared to people without social contact, the impact of being an empty nester on the mental health of older people who do have social contact is different. Specifically, after becoming an empty nester, the depression score for people who have social contact declined by approximately 0.6 more than for people without social contact. When we further divide social contact into two types, we found that it is cognitive activities that contribute to the significant modification function on the effect of being an empty nester on depressive symptoms.
Table 4. The impacts of contact with one’s children and social contact on depressive symptoms for empty nesters.
We focused our study on older people with disabilities, as outlined in (see Appendix I for full sets of regression results). We found that once older people with disabilities became empty nesters, their depression scores rose significantly; the effects were greater the longer they had been empty nesters. In particular, after being an empty nester for three waves (around seven years), the depression score for older people with disabilities increased substantially by approximately 3.7. If these disabled older empty nesters had contact with their children more than once a month, it seemed that their depression status would not significantly deteriorate. However, if they had contact with each other less often, their depression score would rise significantly by approximately 2.4 on average. Finally, we found that having cognitive activities seemed to have significantly positive influence on depressive symptoms in disabled older people.
Table 5. The impact of being an empty nester on depressive symptoms in people with ADL/IADL limitations.
Discussion
Understanding how older people’s mental health changes after they become empty nesters has significant policy implications. This paper presents compelling new findings on the association between being an empty nester and depressive symptoms with the time and moderation effects of contact with one’s children and social contact in relation to this association. Our findings show that older people’s mental health does not change significantly right after they become empty nesters, but in the longer term, their mental health would deteriorate significantly with time, which is consistent with existing studies (Dennerstein et al., Citation2002; Gao et al., Citation2017). We also found that regular contact with children remain important for older people’ mental health after they become empty nester. One possible explanation is that one’s parental role and affiliated sense of accomplishment may be affected after becoming an empty nester (Bouchard, Citation2014; White & Edwards, Citation1990), however, if empty nesters maintain regular contact with their children, their parental role may remain, even without co-habiting (White & Edwards, Citation1990). Furthermore, we found that older empty nesters’ mental health is significantly improved if they have social contact, especially cognitive activities. This is consistent with existing studies (Gao et al., Citation2017; Lam et al., Citation2020).
The results from our subgroup analysis on older people with ADL/IADL limitations present a different picture. When older people with functional disabilities become empty nesters and have contact with their children less than once every three months, their mental health is affected immediately after they become empty nesters, and worsens in the longer term. In China, due to a lack of formal LTC, older people with ADL/IADL limitations primarily rely on informal LTC provided by children or other relatives (Yang et al., Citation2021). If they become empty nesters and do not have frequent contact with their children, their LTC needs are hard to meet due to reduced care, which may in turn have negative outcomes for their physical and mental health (Mahoney et al., Citation2000; Zunzunegui et al., Citation2001). This again can be supported by the stress-buffering model which has implications on caregiving and care-receiving. For older people with disabilities, their live-in children can potentially be their caregivers. Perceived support from children who have been the carers may buffer the negative stress on older people’s life, and losing such support or contact may create stress and anxiety among older people with disabilities.
This study provides fresh insight into the association between being an empty nester and mental health, as well as the moderating effects of social contact and contact with one’s children, which enabled us to draw the following policy implications. First, the local community should provide older people with social contact opportunities, especially cognitive activities (Rodda et al., Citation2011). For instance, community events, which include walking, board games, craft making, and providing older people with chances to communicate with others of the same age, have proved to be effective in improving older people’s mental health (Forsman et al., Citation2011; Jorm, Citation2012). We have also observed that these cognitive activities have greater positive impacts on the mental health of older empty nesters with functional disabilities than the other older empty nesters. This could be due to limited activities available for the older people with functional limitations as most of the older people are not able to participate in strenuous activities. However, by participating in cognitive activities, older people with disabilities may develop social ties with other people, who may offer emotional support, comfort and interpersonal interactions. Our findings are consistent with a number of studies in the field, which stress the importance of social interactions for older people (Burmeister et al., Citation2016; Gaugler & Zarit, Citation2001).
Second, a formal LTC system should be created to support older empty nesters with functional disabilities. For this group of people, receiving informal LTC from families or friends is difficult since they do not live together. Hence, formal LTC becomes vital in maintaining their physical health and enabling them to live independently with respect, and in turn becomes important for their mental health (Muir, Citation2017; Yang & Tan, Citation2019). The LTC system in China is still in its early stages of development, and the family is the main provider of LTC (Peng, Citation2015). To meet the needs of older empty nesters with functional disabilities for formal LTC, day care centres could be set up in the community to provide meals and transportation services, and home-based LTC services could be provided by professional caregivers (World Health Organization, Citation2015).
This study has the following limitations. First, we were unable to identify a causal relationship between depressive symptoms and being an empty nester, as becoming an empty nester is not strictly exogenous, but rather an endogenous choice made by individuals. Second, the sample size of older people with ADL/IADL limitations was not large enough, making it difficult to perform deeper analysis based on subgroups, such as further dividing the group according to marital status. We hypothesise that single empty nesters with functional disabilities may experience more depressive symptoms than married empty nesters, as married individuals may receive care from their partners.
Acknowledgements: This paper uses data from the China Health and Retirement Longitudinal Study (CHARLS). The National School of Development of Peking University is gratefully acknowledged for providing the data (see http://charls.pku.edu.cn/en/). We thank for the support from KHYS and CSC. We also acknowledge general supports from Prof. Dr. Berthold U. Wigger and Prof. Mauricio Avendano Pabon.
Funding details: This work is funded by the Research Travel Grant provided by Karlsruhe House of Young Scientists (KHYS) and financially supported by China Scholarship Council (CSC).
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
This work is funded by the Research Travel Grant provided by Karlsruhe House of Young Scientists (KHYS) and financially supported by China Scholarship Council (CSC).
China Scholarship Council;Research Travel Grant provided by Karlsruhe House of Young Scientists;
References
- Aranda, L. (2015). Doubling up: A gift or a shame? Intergenerational households and parental depression of older Europeans. Social Science & Medicine (1982), 134, 12–22. https://doi.org/10.1016/j.socscimed.2015.03.056
- Athey, S., Imbens, G. (2022). Design-based analysis in difference-in-differences settings with staggered adoption. Journal of Econometrics, 226(1), 62–79. https://doi.org/10.1016/j.jeconom.2020.10.012
- Austin, P. C. (2009). Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Statistics in Medicine, 28(25), 3083–3107. https://doi.org/10.1002/sim
- Beckman, L. J. (1981). Effects of social interaction and children’s relative inputs on older women’s psychological well-being. Journal of Personality and Social Psychology, 41(6), 1075–1086. https://doi.org/10.1037/0022-3514.41.6.1075
- Bennett, D. A., Schneider, J. A., Tang, Y., Arnold, S. E., & Wilson, R. S. (2006). The effect of social networks on the relation between Alzheimer’s disease pathology and level of cognitive function in old people: A longitudinal cohort study. The Lancet Neurology, 5(5), 406–412. https://doi.org/10.1016/S1474-4422(06)70417-3
- Bouchard, G. (2014). How do parents react when their children leave home? An integrative review. Journal of Adult Development, 21(2), 69–79. https://doi.org/10.1007/s10804-013-9180-8
- Burmeister, O. K., Bernoth, M., Dietsch, E., & Cleary, M. (2016). Enhancing connectedness through peer training for community-dwelling older people: A person centred approach. Issues in Mental Health Nursing, 37(6), 406–411. https://doi.org/10.3109/01612840.2016.1142623
- Caliendo, M., & Kopeinig, S. (2008). Some practical guidance for the implementation of propensity score matching. Journal of Economic Surveys, 22(1), 31–72. https://doi.org/10.1111/j.1467-6419.2007.00527.x
- Callaway, B., & Sant’Anna, P. H. C. (2021). Difference-in-differences with multiple time periods. Journal of Econometrics, 225(2021), 200–230. https://doi.org/10.1016/j.jeconom.2020.12.001
- Chaisemartin, C. d., & D’Haultfoeuille, X. (2020). Two-way fixed effects estimators with heterogeneous treatment effects. American Economic Review, 110(9), 2964–2996. https://doi.org/10.1257/aer.20181169
- Chang, Y., Guo, X., Guo, L., Li, Z., Yang, H., Yu, S., Sun, G., & Sun, Y. (2016). Comprehensive comparison between empty nest and non-empty nest elderly: A cross-sectional study among rural populations in northeast China. International Journal of Environmental Research and Public Health, 13(9), 857. https://doi.org/10.3390/ijerph13090857
- CHARLS. (2020). Data of China health and retirement longitudinal study. http://charls.pku.edu.cn/pages/data/111/en.html
- Chen, T. (2019). Living arrangement preferences and realities for elderly Chinese: Implications for subjective wellbeing. Ageing and Society, 39(8), 1557–1581. https://doi.org/10.1017/S0144686X18000041
- Cho, J., Ory, M. G., & Stevens, A. B. (2016). Socioecological factors and positive aspects of caregiving: Findings from the REACH II intervention. Aging & Mental Health, 20(11), 1190–1201. https://doi.org/10.1080/13607863.2015.1068739
- Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. https://doi.org/10.1037/0033-2909.98.2.310
- Dennerstein, L., Dudley, E., & Guthrie, J. (2002). Empty nest or revolving door? A prospective study of women’s quality of life in midlife during the phase of children leaving and re-entering the home. Psychological Medicine, 32(3), 545–550. https://doi.org/10.1017/s0033291701004810
- Dias, R., Santos, R. L., Sousa, M. F. B. d., Nogueira, M. M. L., Torres, B., Belfort, T., & Dourado, M. C. N. (2015). Resilience of caregivers of people with dementia: A systematic review of biological and psychosocial determinants. Trends in Psychiatry and Psychotherapy, 37(1), 12–19. https://doi.org/10.1590/2237-6089-2014-0032
- Forsman, A. K., Nordmyr, J., & Wahlbeck, K. (2011). Psychosocial interventions for the promotion of mental health and the prevention of depression among older adults. Health Promotion International, 26(suppl_1), i85–107. https://doi.org/10.1093/heapro/dar074
- Gao, M., Li, Y., Zhang, S., Gu, L., Zhang, J., Li, Z., Zhang, W., & Tian, D. (2017). Does an empty nest affect elders’ health? Empirical evidence from China. International Journal of Environmental Research and Public Health, 14(5), 463. https://doi.org/10.3390/ijerph14050463
- Gaugler, J. E., & Zarit, S. H. (2001). The effectiveness of adult day services for disabled older people. Journal of Aging & Social Policy, 12(2), 23–47. https://doi.org/10.1300/J031v12n02_03
- Gaymu, J., Delbès, C., Springer, S., Binet, A., Désesquelles, A., Kalogirou, S., & Ziegler, U. (2006). Determinants of the living arrangements of older people in Europe. European Journal of Population / Revue Européenne de Démographie, 22(3), 241–262. https://doi.org/10.1007/s10680-006-9004-7
- Gellert, P., Häusler, A., Suhr, R., Gholami, M., Rapp, M., Kuhlmey, A., & Nordheim, J. (2018). Testing the stress-buffering hypothesis of social support in couples coping with early-stage dementia. PLoS One, 13(1), e0189849–14. https://doi.org/10.1371/journal.pone.0189849
- Goodman-Bacon, A., Nichols, A., & Goldring, T. (2019). Bacon decomposition for understanding differences-in-differences with variation in treatment timing [Paper presentation]. Stata Conference.
- Guo, Y. Q., Zhang, C. C., Huang, H., Zheng, X., Pan, X. J., & Zheng, J. Z. (2016). Mental health and related influencing factors among the empty-nest elderly and the non-empty-nest elderly in Taiyuan, China: A cross-sectional study. Public Health, 141(December), 210–217. https://doi.org/10.1016/j.puhe.2016.09.005
- Imbens, G., & Wooldridge, J. (2007). What’s new in econometrics? (pp. 1–19). NBER Summer Institute. http://www.nber.org/WNE/lect_10_diffindiffs.pdf
- Jorm, A. F. (2012). Mental health literacy: Empowering the community to take action for better mental health. The American Psychologist, 67(3), 231–243. https://doi.org/10.1037/a0025957
- Kawachi, I., & Berkman, L. F. (2001). Social ties and mental health. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 78(3), 458–467. https://doi.org/10.1093/jurban/78.3.458
- Lam, B. C. P., Haslam, C., Steffens, N. K., Yang, J., Haslam, S. A., Cruwys, T., & Pachana, N. A. (2020). Longitudinal evidence for the effects of social group engagement on the cognitive and mental health of Chinese retirees. The Journals of Gerontology: Series B, 75(10), 2142–2151. https://doi.org/10.1093/geronb/gbz134
- Laporte, A., & Windmeijer, F. (2005). Estimation of panel data models with binary indicators when treatment effects are not constant over time. Economics Letters, 88(3), 389–396. https://doi.org/10.1016/j.econlet.2005.04.002
- Lee, J., Ham, M. J., Pyeon, J. Y., Oh, E., Jeong, S. H., Sohn, E. H., & Lee, A. Y. (2017). Factors affecting cognitive impairment and depression in the elderly who live alone: Cases in Daejeon metropolitan city. Dementia and Neurocognitive Disorders, 16(1), 12–19. https://doi.org/10.12779/dnd.2017.16.1.12
- Liang, D., Mays, V. M., & Hwang, W. C. (2018). Integrated mental health services in China: Challenges and planning for the future. Health Policy and Planning, 33(1), 107–122. https://doi.org/10.1093/heapol/czx137
- Litwin, H. (2004). Intergenerational exchange and mental health in later-life-the case of older Jewish Israelis. Aging & Mental Health, 8(3), 196–200. https://doi.org/10.1080/13607860410001669723
- Lowenthal, M. F., & Chiriboga, D. (1972). Transition to the empty nest. Crisis, challenge, or relief? Archives of General Psychiatry, 26(1), 8–14. https://doi.org/10.1001/archpsyc.1972.01750190010003
- Mahoney, J. E., Eisner, J., Havighurst, T., Gray, S., & Palta, M. (2000). Problems of older adults living alone after hospitalization. Journal of General Internal Medicine, 15(9), 611–619. https://doi.org/10.1046/j.1525-1497.2000.06139.x
- Muir, T. ((2017). Measuring social protection for long-term care. OECD Health Working Papers (No. 93; Issue 93). https://doi.org/10.1787/a411500a-en OECD
- National Bureau of Statistics of China. (2020). Tabulation on the 2010 population census of the People’s Republic of China (in Chinese). http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm
- OECD. (2011). What are equivalence scales? http://www.oecd.org/els/soc/OECD-Note-EquivalenceScales.pdf
- Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The relationship between physical and mental health: A mediation analysis. Social Science & Medicine (1982), 195 (November), 42–49. https://doi.org/10.1016/j.socscimed.2017.11.008
- Oliver, R. (1977). The “empty nest syndrome” as a focus of depression: A cognitive treatment model, based on rational emotive therapy. Psychotherapy, 14(1), 87–94. https://doi.org/10.1037/h0087497
- Peng, D. (2015). Long-term care for older persons in China, 1–22. United Nations ESCAP. http://www.unescap.org/sites/default/files/Long Term Care for older persons in China.pdf
- Radloff, L. S. (1980). Depression and the empty nest. Sex Roles, 6(6), 775–781. https://doi.org/10.1007/BF00287233
- Ravallion, M. (2007). Chapter 59: Evaluating anti-poverty programs. Handbook of development economics, 4, 3787–3846. https://doi.org/10.1016/S1573-4471(07)04059-4
- Roberts, B. L., Dunkle, R., & Haug, M. (1994). Physical, psychological, and social resources as moderators of the relationship of stress to mental health of the very old. Journal of Gerontology, 49(1), S35–S43. https://doi.org/10.1093/geronj/49.1.s35
- Rodda, J., Walker, Z., & Carter, J. (2011). Depression in older adults. BMJ (Clinical Research ed.), 343(7825), d5219–687. https://doi.org/10.1136/bmj.d5219
- Rosenbaum, P. R., & Rubin, D. B. (1985). Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. The American Statistician, 39(1), 33–38. https://www.jstor.org/stable/pdf/2683903.pdf?refreqid=excelsior%3Aff55844d4c3dc06015871bf62e859675 https://doi.org/10.2307/2683903
- Stern, C., & Munn, Z. (2010). Cognitive leisure activities and their role in preventing dementia: A systematic review. International Journal of Evidence-Based Healthcare, 8(1), 2–17. https://doi.org/10.1111/j.1744-1609.2010.00150.x
- Stewart, S. D. (2003). Nonresident parenting and adolescent adjustment: The quality of nonresident father-child interaction. Journal of Family Issues, 24(2), 217–244. https://doi.org/10.1177/0192513X02250096
- Sun, X., Lucas, H., Meng, Q., & Zhang, Y. (2011). Associations between living arrangements and health-related quality of life of urban elderly people: A study from China. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 20(3), 359–369. https://doi.org/10.1007/s11136-010-9752-z
- Tosi, M., & Grundy, E. (2019). Intergenerational contacts and depressive symptoms among older parents in Eastern Europe. Aging & Mental Health, 23(6), 686–692. https://doi.org/10.1080/13607863.2018.1442412
- UNFPA and HelpAge International. (2012). Ageing in the twenty-first century: A celebration and a challenge. https://www.unfpa.org/sites/default/files/pub-pdf/Ageing%20report.pdf
- Weaver, A. N., & Jaeggi, S. M. (2021). Activity engagement and cognitive performance amongst older adults. Frontiers in Psychology, 12(March), 620867–620812. https://doi.org/10.3389/fpsyg.2021.620867
- White, L., & Edwards, J. N. (1990). Emptying the nest and parental well-being: An analysis of national panel data. American Sociological Review, 55(2), 235–242. https://doi.org/10.2307/2095629
- Wooldridge, J. (2012). Difference-in-differences estimation programme evaluation for policy analysis. https://www.ifs.org.uk/docs/wooldridge session 5.pdf
- World Health Organization. (2017a). Depression and other common mental disorders: Global health estimates.
- World Health Organization. (2015). World report on ageing and health.
- World Health Organization. (2017b). WHO clinical consortium on healthy ageing. Topic focus: Frailty and intrinsic capacity. December, vol. 36.
- World Health Organization. (2020). Mental health of older adults. https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults
- Xiang, Y.-T., Yu, X., Sartorius, N., Ungvari, G. S., & Chiu, H. F. K. (2012). Mental health in China: Challenges and progress. The Lancet, 380(9855), 1715–1716. https://doi.org/10.1016/S0140-6736(11)60893-3
- Xu, Q. (2018). Living arrangement and depression among the Chinese elderly people: An empirical study based on CHARLS (in Chinese). Sociological Review of China, 6(4), 47–63.
- Yang, W., & Tan, S. Y. (2019). Is informal care sufficient to meet the long-term care needs of older people with disabilities in China? Evidence from the China health and retirement longitudinal survey. Ageing and Society, 41(5), 1–20. https://doi.org/10.1017/S0144686X1900148X
- Yang, W., Wu, B., Tan, S. Y., Li, B., Lou, V. W. Q., Chen, Z., Chen, X., Fletcher, J. R., Carrino, L., Hu, B., Zhang, A., Hu, M., & Wang, Y. (2021). Understanding health and social challenges for aging and long-term care in China. Research on Aging, 43(3–4), 127–135. https://doi.org/10.1177/0164027520938764
- You, K. S., Lee, H. O., Fitzpatrick, J. J., Kim, S., Marui, E., Lee, J. S., & Cook, P. (2009). Spirituality, depression, living alone, and perceived health among Korean older adults in the community. Archives of Psychiatric Nursing, 23(4), 309–322. https://doi.org/10.1016/j.apnu.2008.07.003
- Zhai, Y., Yi, H., Shen, W., Xiao, Y., Fan, H., He, F., Li, F., Wang, X., Shang, X., & Lin, J. (2015). Association of empty nest with depressive symptom in a Chinese elderly population: A cross-sectional study. Journal of Affective Disorders, 187(81703324), 218–223. https://doi.org/10.1016/j.jad.2015.08.031
- Zhao, Y., Strauss, J., Giles, J., Hu, P. P., Hu, Y., Lei, X., Liu, M., Park, A., Smith, J. P., & Wang, Y. (2013). China health and retirement longitudinal study: 2011–2012 national baseline users’ guide (Issue April).
- Zunzunegui, M. V., Béland, F., & Otero, A. (2001). Support from children, living arrangements, self-rated health and depressive symptoms of older people in Spain. International Journal of Epidemiology, 30(5), 1090–1099. https://doi.org/10.1093/ije/30.5.1090
Appendix A:
Robustness check with city-level GDP per capita
Appendix B:
Parallel trend test
Appendix C:
Heterogeneous impacts of being an empty nester on depressive symptoms for people in rural/urban areas
1. Constant ATT and Varied ATTs.
2. The interaction with social contact.
Appendix D:
The matching rate for treatment and control groups
Appendix E:
Propensity score density distributions before and after the matching
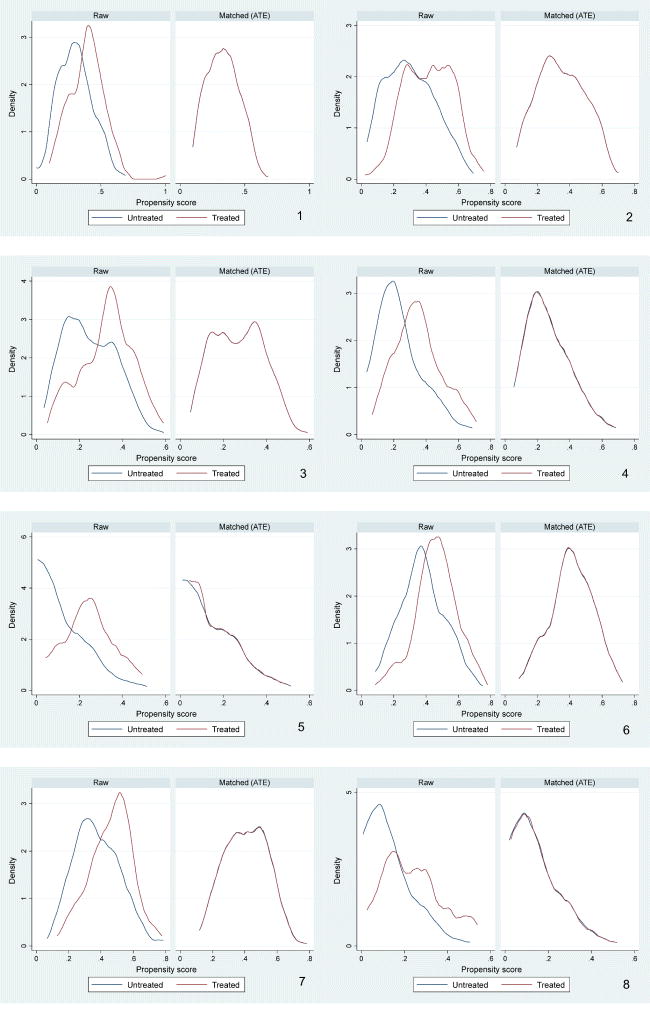
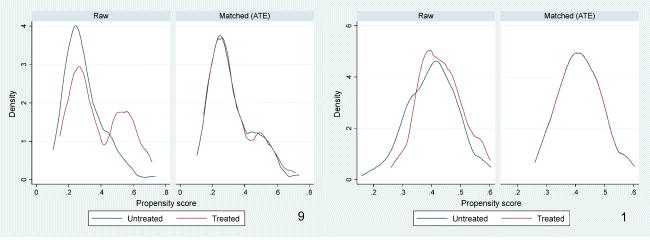
Notes. 1 = for the sample enrolled in Year 1–4 and treated in Year 4; 2 = enrolled in Year 1–4, treated in Year 3; 3 = enrolled in Year 1–4, treated in Year 2; 4 = enrolled in Year 1–3, treated in Year 3; 5 = enrolled in Year 1–3, treated in Year 2; 6 = enrolled in Year 2–4, treated in Year 4; 7 = enrolled in Year 2–4, treated in Year 3; 8 = enrolled in Year 1–2; 9 = enrolled in Year 2–3; 10 = enrolled in Year 3–4.
