Abstract
Objectives
To identify factors that predict the risk of loneliness for people with dementia and carers during a pandemic.
Methods
People with dementia and their carers completed assessments before (July 2019–March 2020; 206 dyads) and after (July–October 2020) the first Covid-19 ‘lockdown’ in England. At follow-up, the analytic sample comprised 67 people with dementia and 108 carers. We built a longitudinal path model with loneliness as an observed outcome. Carer type and social contacts at both measurements were considered. Other social resources (quality of relationship, formal day activities), wellbeing (anxiety, psychological wellbeing) and cognitive impairment were measured with initial level and change using latent growth curves. We adjusted for socio-demographic factors and health at baseline.
Results
In carers, higher levels of loneliness were directly associated with non-spouse coresident carer type, level and increase of anxiety in carer, more formal day activities, and higher cognitive impairment in the person with dementia. In people with dementia, non-spouse coresident carer type, and higher initial levels of social resources, wellbeing, and cognitive impairment predicted the changes in these factors; this produced indirect effects on social contacts and loneliness.
Conclusion
Loneliness in the Covid-19 pandemic appears to be shaped by different mechanisms for people with dementia and their carers. The results suggest that carers of those with dementia may prioritize providing care that protects the person with dementia from loneliness at the cost of experiencing loneliness themselves. Directions for the promotion of adaptive social care during the Covid-19 pandemic and beyond are discussed.
Loneliness is a major public health concern. It is associated with poor physical and mental health, and all-cause mortality (Cohen-Mansfield et al., Citation2016; Leigh-Hunt et al., Citation2017). The coronavirus disease-2019 (COVID-19) pandemic led to government-issued social restrictions (Geirdal et al., Citation2021; World Health Organization, Citation2020). In the UK, governmental guidance advised the public to stay at home unless for essential travel or work (Iacobucci, Citation2020). Social care services (e.g. providing social interaction) were disrupted (Wheatley et al., Citation2022), and users accessed fewer out-of-home social support services (e.g. organized social activities, day care) following the onset of the pandemic (Giebel et al., Citation2021a, 2021b). This disruption to usual social engagement and social care services for people with dementia and their carers potentially rendered them particularly vulnerable to loneliness (D’Cruz & Banerjee, Citation2020b; Greenberg et al., Citation2020; Liu et al., 2021) – ‘a distressing feeling that accompanies the perception that one’s social needs are not being met by the quantity or especially the quality of one’s social relationships’ (Hawkley & Cacioppo, Citation2010, p.218). The experience of loneliness among people with dementia and caregivers during the Covid-19 pandemic is a recurring research finding (e.g. Tam et al., Citation2021). However, increases in loneliness in the pandemic seem to depend on various factors, including social resources such as living with others and wellbeing markers such as psychological distress (Bu et al., Citation2020; Frenkel-Yosef et al., Citation2020; Hansen et al., Citation2021; Macdonald & Hülür, Citation2021); people with dementia and caregivers may draw on these resources in different ways (Greenberg et al., Citation2020). In this paper, we examine the longitudinal pathways between social resources, wellbeing resources, dementia-related cognitive impairment, and loneliness to identify factors that predict the risk of loneliness for people with dementia and carers during the Covid-19 pandemic.
Evidence concerning experiences of loneliness in the Covid-19 pandemic is mixed. Whereas some studies report increases in loneliness (Killgore et al., Citation2020; Macdonald & Hülür, Citation2021; Tam et al., Citation2021; van Tilburg et al., Citation2021), others have reported no or only slight increases (Luchetti et al., Citation2020; McGinty et al., Citation2020; Peng & Roth, Citation2021) or even a decline (Sutin et al., Citation2020). One reason for such discrepancies may be that the predictors of loneliness are different in different populations. For example, loneliness has been associated with different social resources (e.g. coresidence with carer, carer type) in people with dementia and carers (Victor et al., Citation2020, Citation2021). Specifically, in the Improving the experience of Dementia and Enhancing Active Life (IDEAL) study, loneliness was associated with living alone among people with dementia (Victor et al., Citation2020), but among carers of people with dementia, who largely (97%) did not live alone, loneliness was associated with caregiver-kin relationship (Victor et al., Citation2021). Furthermore, there is evidence that individual resources (e.g. social) related differently to loneliness in different non-dementia populations during the pandemic (Bu et al., Citation2020; Frenkel-Yosef et al., Citation2020; Hansen et al., Citation2021; Macdonald & Hülür, Citation2021). Considering that loneliness is common in people with dementia (e.g. approximately 35% report moderate to severe loneliness, Victor et al., Citation2020), and dementia carers (e.g. approximately 62% report moderate to severe loneliness, Victor et al., Citation2021), it is important to understand whether loneliness predictors diverge in these populations.
Relatively consistent predictors of loneliness in older people include demographic variables (e.g. non-married status, living alone), social resources (e.g. limited social network, low social activity), wellbeing (e.g. depression/depressed mood, low life satisfaction), and poor self-reported physical health (Cohen-Mansfield et al., Citation2016; Dahlberg et al., Citation2021). However, there is limited quantitative evidence about the associations of loneliness in people with dementia (Balouch et al., Citation2019; El Haj et al., Citation2016; Holmén et al., Citation2000; Victor et al., Citation2021) and dementia carers (Beeson, Citation2003; Beeson et al., Citation2000; Clare et al., 2019; Jaremka et al., Citation2014; Victor et al., Citation2021). In this paper, we investigate, for the first time, longitudinal predictors of loneliness in people with dementia and their carers and how these converged or diverged during the first wave of the Covid-19 pandemic.
The Covid-19 pandemic presented challenges to the daily lives of people with dementia and their carers, whether shared (e.g. routine disruption), unique to people with dementia (e.g. increased reliance on carer), or unique to carers (e.g. identifying accessible carer support) (Asthana et al., Citation2021; D’Cruz & Banerjee, Citation2020b; Greenberg et al., Citation2020; Rajagopalan et al., Citation2022; Savla et al., Citation2021). Adapting to these challenges potentially shapes the experience of loneliness. For example, social restrictions during lockdown alongside decreases in dementia services (Liu et al., 2021) may increase carers’ scope for, and time spent, addressing the needs of the person with dementia, particularly when the two live together. Coresidence of carer and person with dementia during the Covid-19 pandemic is, on the one hand, potentially protective against loneliness (D’Cruz & Banerjee, Citation2020a; Moyle et al., Citation2011). On the other hand, for carers, coresidence accompanied by increases in care responsibilities is also a potential source of loneliness (D’Cruz & Banerjee, Citation2020a; Steenfeldt et al., Citation2021) and decrease in mental health (Zucca et al., 2021). Also, adverse outcomes stemming from greater caregiving burden may be shaped by the carer’s relationship (e.g. spouse, child) with the person with dementia (Chiao et al., Citation2015). In other words, during the Covid-19 pandemic, factors such as coresidence and relationship type and quality may differentially affect the experience of loneliness. Also, from the perspective of resilience in aging (MacLeod et al., Citation2016), markers of psychological wellbeing can potentially contribute to better adaptation to stressors that relate to loneliness (e.g. Covid-19-related, Kim et al., Citation2021; Kang et al., Citation2021), effects that potentially apply to people with dementia, their carers, or both. Overall, it may be, therefore, that social and psychological wellbeing resources relate in different ways to loneliness in the Covid-19 pandemic in people with dementia and their carers.
The Current Study
In the current study, we aim to identify pathways to loneliness during the Covid-19 pandemic in people with dementia and their carers. Our conceptual framework is based on the literature on predictors of loneliness in older people (Cohen-Mansfield et al., Citation2016; Dahlberg et al., Citation2021), theory about resilience in aging (Kim et al., Citation2021), and the previously unexplored potential for differential associations between social resources and loneliness in people with dementia and their carers. We conducted a multi-domain investigation of the pathways between social and wellbeing factors and loneliness, while accounting for changes in the cognitive function of the person with dementia and socio-demographic and health factors. The longitudinal modelling included two measurement occasions: one before and one after the start of the first lockdown in England. The purpose of our study is to help identify people with dementia and carers who may be at increased risk of loneliness in future lockdowns (D’Cruz & Banerjee, Citation2020b) and improve understanding about how interventions (Cohen-Mansfield & Perach, Citation2015; Williams et al., Citation2021) can be better tailored to best support these individuals within and outside pandemics.
Methods
Participants and Recruitment
Data were collected as part of the DETERMIND programme (Farina et al., 2020). Baseline face-to-face interviews of 206 dyads of carers and people recently diagnosed with dementia were completed between late July 2019 and early March 2020, prior to the first national lockdown in England. Participants were recruited from three geographically and socially diverse areas of England (Sussex/South London/Newcastle and Gateshead). Follow-up data collection (DETERMIND-C19 study; henceforth: D-C19 study) via telephone was carried out between July and October 2020; in this period, restrictions introduced during the first national lockdown (March–July, 2020) were partially lifted (e.g. two households could meet indoors; July–September, 2020) and subsequently tightened (e.g. ‘rule of six’; September–October, 2020) (Brown & Kirk-Wade, Citation2021). Capacity assessments were undertaken at both time-points. Baseline and D-C19 study questionnaire data were collected and managed using REDCap (Harris et al., Citation2009). See Appendix 1 () for more detail.
Table 1. Background variables in carers and people with dementia at baseline and among those who participated in D-C19 study.
Measures
An overview of the measures is presented below with more details outlined in Appendix 1 (). We used baseline assessments of socio-demographic variables, carer type, and self-rated health. Additional social resources, wellbeing, and cognitive impairment were assessed at baseline and D-C19 study. Loneliness was assessed in D-C19 study.
Table 2. Social resources, wellbeing, and clinical dementia rating at baseline and D-C19 study, and loneliness (D-C19 study only).
Table 3. Direct and indirect effects in the models for carers and people with dementia (the indirect paths shown in and ).
Background variables
Socio-demographic variables were coded for both the carer and person with dementia. Other covariates included the time since diagnosis of dementia in months at baseline and time between the baseline and D-C19 interviews in months, and self-rated health, which was rated by the person with dementia and the carer using the EQ5D-VAS scale (Rabin & Charro, Citation2001).
Cognitive impairment of the person with dementia was measured using Clinical Dementia Rating (CDR, Morris, Citation1993). An index score was computed using an online calculator (National Alzheimer’s Coordinating Center, Citation2021).
Wellbeing
Psychological wellbeing was evaluated using three National Statistics ONS4 (ONS, Citation2018) items. These items have shared thresholds (ONS, Citation2018) and were correlated (r for people with dementia ranged 0.50–0.72, r for carers ranged 0.53–0.65, all ps<.001); a mean of the three items was used. Anxiety was evaluated using one National Statistics ONS4 (ONS, Citation2018) item.
Social resources
Carer type was indexed as a combination of coresidence status and spouse carer variables: 1 = spouse, 2 = coresident non-spouse, 3 = non-coresident non-spouse. The quality of relationship between the person with dementia and carer was measured with four items (see Rippon et al., Citation2020), based on the Positive Affect Index (Bengtson & Schrader, Citation1982). A mean score was used; a higher score indicating better relationship quality (Cronbach’s alpha for people with dementia = 0.78, Cronbach’s alpha for carers = 0.81). Social contacts were measured with two questions at baseline: How many 1) relatives 2) friends do you see or hear from at least once a month?, based on the Lubben Social Network Scale (Lubben et al., Citation2006). In D-C19 the questions were modified: How many 1) relatives (birth, marriage, adaption) 2) friends have you seen or heard from (this could be online) during the lock-down? Because of the difference in wording and time scale used, social contacts were used as observed variables at baseline and D-C19 study (no estimation of change). Formal day activities for the person with dementia were in-person, by telephone, or online. Participation in any of the listed activities was coded as 1, otherwise 0.
Loneliness was assessed using a 3-item version of UCLA loneliness scale (Hughes et al., Citation2004; Russell et al., Citation1980) recommended by the ONS (Snape & Martin, Citation2018): A sum score was calculated, a higher score indicating more loneliness (Cronbach’s alpha for people with dementia = 0.83, Cronbach’s alpha for carers = 0.80).
Analysis
We used Structural Equation Modelling (SEM) to build a path model with loneliness as an observed outcome. Mediation was estimated using indirect effects. Social resources, wellbeing, and cognitive impairment were treated as predictors of loneliness and adjusted for the background variables at baseline. Several socio-demographic factors correlated between the carer and person with dementia (ethnicity, and the overlap between coresidence, home ownership, area deprivation and being married as most coresident carer/person with dementia dyads were couples): therefore, for these variables only, the individual’s own indicator was used in the model. For the variables with repeated measures, Latent Growth Curves were estimated for the level and change. In a Latent Growth Curve model (Meredith & Tisak, Citation1990), random effects are used to capture individual differences and fixed effects to estimate the average growth of the entire sample. Analyses were carried out with Mplus 8 (Muthén & Muthén, n.d.). With two time points, a simple linear change (slope) could be estimated with the initial level (intercept).
The fit of the model was assessed by chi-square analysis, but because this is sensitive to sample size, we also used three other recommended fit indices (Hu & Bentler, Citation1999; Kline, Citation2005): the Comparative Fit Index (CFI), Root Mean Square Error of approximation (RMSEA), and Standardized Root Mean Square Residual (SRMR). A value at or below 0.05 for the RMSEA and SRMR and at or above 0.90 for the CFI was considered to indicate an adequate fit for the model. Maximum likelihood estimation with robust standard errors (MLR) was used to take into account any sample non-normality. Missing data were handled using the full information maximum likelihood method (FIML) (Acock, Citation2005), which enables including cases with missing values for any dependent variable in path models such that information on the means and variances of all data are used.
Results
Descriptive Results
Recruitment. On average, there were 8.2 months between waves (range 5–11 months). 114 dyads in which either the carer or both the carer and person with dementia participated.Footnote1 Of these, 108 carers and 67 people with dementia completed the loneliness measure. Forty-nine (73%) of the people with dementia and 107 (94%) of the carers completed the questionnaires over the phone, the remainder posted a hardcopy back to the researchers.
Background characteristics are shown in .
Social resources, wellbeing, clinical dementia rating, and loneliness distributions are shown in . Carers were mostly spouses or long-term partners (54%; 98% were coresident). 14% of carers were non-spouse coresidents (of whom 86% were children of person with dementia) and 32% were non-spouse and not coresident (of whom 86% were children of person with dementia). 68% of the carers were coresident with the person with dementia at baseline. Formal day activities for the person with dementia declined from 43% at baseline to 11% in D-C19 study (a statistically significant negative mean slope in latent growth curve). In carers, quality of relationship was rated somewhat lower with a decline between the measurement points (a statistically significant negative slope in latent growth curve) compared to people with dementia. CDRs ranged from questionable to mild (Morris, Citation1993), increasing from baseline to D-C19 study (a statistically significant positive slope in the latent growth curve indicating increased cognitive impairment). Based on published thresholds (ONS, Citation2018), at baseline and D-C19 study, mean levels of psychological wellbeing were high, and levels of anxiety ranged low-medium. The group means of these wellbeing markers changed little between assessments in both people with dementia and their carers (). The statistically significant variances in the latent growth curves suggested differences between the individuals at the starting levels (intercepts) and rate of change (slope) between the baseline and D-C19 study both in the models for carers and people with dementia.
Social Resources, Wellbeing, and Background Variables as Predictors of Loneliness in People with Dementia and Carers
We fitted the models for people with dementia and for carers while adjusting for the background variables. With three carer type categories, the models were fitted with two alternative reference groups to show all comparisons: 1) using the non-spouse and resident carer as a reference group and 2) using non-spouse non-resident carer as a reference group.
People with dementia models
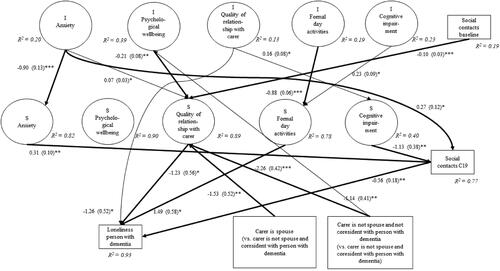
shows the significant paths for the people with dementia with non-spouse non-coresident carer as reference group. shows the significant paths for the people with dementia with non-spouse coresident carer as reference group. In both these models, direct predictors of loneliness were lower level of relationship quality and declined relationship quality with carer, larger decline in formal day activities, and fewer social contacts in D-C19 study. Indirect predictors. shows the direct effects without mediation and the indirect effects when mediation was estimated in the models shown in . Carer type was indirectly associated with loneliness through relationship with carer. Specifically, people with dementia whose carer was non-spouse and coresident with person with dementia reported less loneliness due to improved relationship with carer between assessments compared to people with dementia with spouse carers or non-spouse non-coresident carers, who reported higher levels of loneliness due to deterioration in the relationship with carer (). In addition, higher levels of anxiety at baseline were indirectly associated with higher levels of loneliness through less decline in anxiety and fewer social contacts at D-C19 study. A higher level of formal social activities at baseline predicted less decline in social formal activities between assessments and further lower levels of loneliness at D-C19 study. Increased cognitive impairment was associated with fewer contacts at D-C19 study and further higher levels of loneliness. Finally, a higher number of social contacts and higher psychological wellbeing at baseline each predicted deterioration in relationship with carer between baseline and D-C19 study and higher levels of loneliness. Supplementary Tables 4 and 5 (Appendix 2) show the associations of the background variables in the models for people with dementia in and .
Figure 1. People with dementia model: The change (S = slope) and initial level (I = Intercept) of anxiety (ONS), psychological wellbeing (ONS), quality of relationship with carer, formal day activities, and cognitive impairment (CDR) between baseline and C19 study in DETERMIND (n = 206) and further on people with dementia loneliness in D-C19 study using Latent Growth Curve and observed social contacts. Only significant paths shown for the full model. Unstandardized path estimates and standard errors in parenthesis shown. Adjusted for background variables. *p < 0.05, **p < 0.01, *** p < 0.001. Model fit: Chi-square = 99.25, degrees of freedom = 49, CFI = 0.91, RMSEA = 0.047, SRMR = 0.041. Thicker lines for the paths indicate a significant indirect effect.
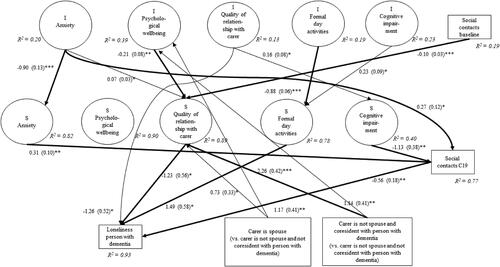
Figure 2. People with dementia model: The change (S = slope) and initial level (I = Intercept) of anxiety (ONS), psychological wellbeing (ONS), quality of relationship with carer, formal day activities and cognitive impairment (CDR) between baseline and C19 study in DETERMIND (n = 206) and further on people with dementia loneliness in D-C19 study using Latent Growth Curve and observed social contacts. Only significant paths shown for the full model. Unstandardized path estimates and standard errors in parenthesis shown. Adjusted for background variables. *p < 0.05, **p < 0.01, ***p < 0.001. Model fit: Chi-square = 99.25, degrees of freedom = 49, CFI = 0.91, RMSEA = 0.047, SRMR = 0.041. Thicker lines for the paths indicate a significant indirect effect.
Carer models
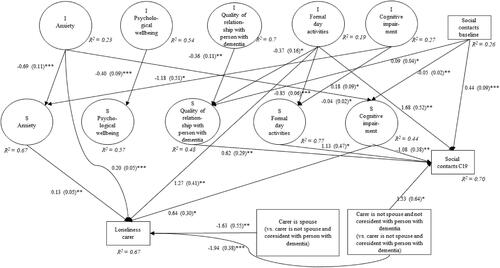
Direct predictors
Non-spouse coresident carers reported more loneliness than spouse carers or non-spouse non-coresident carers ( and ). In carers, a higher level and increase in anxiety were associated with loneliness. A higher level of formal day activities and increased cognitive impairment in the person with dementia were associated with carer loneliness. Indirect predictors. There were no significant indirect paths between the variables in the carer models. Accordingly, shows only the direct effects without mediation for carers. Supplementary Tables 6 and 7 show the associations of the background variables in the models for carers in and .
Figure 3. Carer model: The change (S = slope) and initial level (I = Intercept) of anxiety (ONS), psychological wellbeing (ONS), quality of relationship with person with dementia, formal day activities and cognitive impairment (CDR) between baseline and C19 study in DETERMIND (n = 206) and further on carer loneliness in D-C19 study using Latent Growth Curve and observed social contacts. Only significant paths shown for the full model. Unstandardized path estimates and standard errors in parenthesis shown. Adjusted for background variables. *p < 0.05, **p < 0.01, ***p < 0.001. Model fit: Chi-square = 107.54, degrees of freedom = 49, CFI = 0.91, RMSEA = 0.016, SRMR = 0.030.
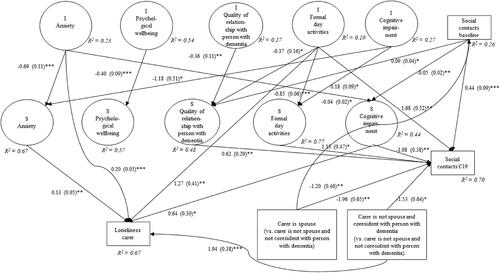
Figure 4. Carer model: The change (S = slope) and initial level (I = Intercept) of anxiety (ONS), psychological wellbeing (ONS), quality of relationship with person with dementia, formal day activities and cognitive impairment (CDR) between baseline and C19 interview in DETERMIND (n = 206) and further on carer loneliness in D-D-C19 study using Latent Growth Curve and observed social contacts. Only significant paths shown for the full model. Unstandardized path estimates and standard errors in parenthesis shown. Adjusted for background variables. *p < 0.05, **p < 0.01, ***p < 0.001. Model fit: Chi-square = 107.54, degrees of freedom = 49, CFI = 0.91, RMSEA = 0.016, SRMR = 0.030.
In both models for people with dementia and carers, most of the associations between the level and slope in the repeated measures were negative, suggesting that the higher initial level was associated with slower rate of change (e.g. higher level of anxiety at baseline was associated with slower change in anxiety between baseline and the D-C19 study, values regressing towards the mean). A sensitivity analysis of the associations with dementia type is presented in Appendix 2 (Supplementary Tables 8–10). Because of the small numbers in the dementia type categories, we could not use this variable in the full model.
Discussion
Loneliness in the Covid-19 pandemic appears to be shaped by different pathways between social resources, wellbeing, and dementia-related cognitive impairment in people with dementia and their carers. For carers, higher levels of loneliness were directly associated with carer type, level and increase of anxiety in carer, more formal day activities, and higher cognitive impairment in the person with dementia. For people with dementia, non-spouse coresident carer type, and higher initial levels of social resources, wellbeing, and cognitive impairment predicted the changes in these factors; this produced indirect effects on social contacts and loneliness. Our findings show that social and wellbeing factors have different pathways to loneliness in people with dementia and their carers. Notably, non-spouse coresident carer type directly predicted increases in loneliness in carers, and indirectly predicted decreases in loneliness in people with dementia via improved relationship. These findings suggest that, in face of Covid-19 restrictions, carers often prioritized the needs of the person with dementia at their own emotional cost. This notion is aligned with other DETERMIND evidence concerning the maintenance of quality of life in these populations (Hicks et al., Citation2022).
Being a coresident non-spouse carer positively predicted loneliness in carers, in line with reports from IDEAL (Victor et al., Citation2021). For carers, coresidency, coupled with an increase in care responsibilities and lesser availability to manage own needs during the Covid-19 pandemic, potentially leads to loneliness (D’Cruz & Banerjee, Citation2020a; Quinn et al., Citation2015; Steenfeldt et al., Citation2021). Importantly, our findings go beyond previous work by highlighting the importance of spouse status in shaping the effects of coresidency on carer loneliness. Specifically, we found increases in loneliness for coresident non-spouse, compared with spouse carers. Lower levels of loneliness among spouse carers are possibly driven by use of emotion regulation strategies in face of Covid-19-related changes in the caregiving situation (Kearns & Creaven, Citation2017; Preece et al., Citation2021). For example, use of emotion regulation strategies labelled ‘adaptive’ (e.g. positive reappraisal) has been associated with less loneliness during the Covid-19 pandemic (Gubler et al., Citation2021). It is therefore possible that spouses’ framing of changes to the caregiving situation as beneficial to the relationship may buffer against carer loneliness for coresident carers. Spouse dementia carers may perceive increased caring responsibilities as a part of couplehood (Stirling et al., Citation2010) and value having more time for rich interactions with their partners (D’Cruz & Banerjee, Citation2020a). This possibility is a direction for future research.
For people with dementia, having a non-spouse (largely adult offspring) coresident carer predicted decreases in loneliness due to increases in relationship quality with carer. Better relationship quality with carer is associated with quality of life in people with dementia (Martyr et al., 2018) and people with dementia report viewing their relationships with carers as beneficial for mitigating loneliness (Moyle et al., Citation2011). Crucially, our findings show that increases in relationship quality with carer mitigated against loneliness for people with dementia with a non-spouse coresident carer, whereas those with a spouse carer or a non-spouse (mostly adult offspring) non-coresident carer reported higher levels of loneliness due to deteriorated relationship with carer. The experience of caring for a family member with dementia can be challenging (e.g. loss of social opportunities, van Wijngaarden et al., Citation2018) in different ways for spouse and non-spouse carers (Johansson et al., Citation2021). The current findings raise the possibility that non-spouse carers who were coresiding with the person with dementia during the Covid-19 pandemic seized the opportunity to invest in the filial relationship, for example, by prioritizing the emotional needs of the person with dementia (Luichies et al., Citation2021), which ultimately mitigated against loneliness in the person with dementia. Indeed, qualitative reports show that family carers (69% adult offspring) of people with dementia deepened their caring relationship through more contact during the Covid-19 pandemic (Tulloch et al., Citation2022). A related interpretation is that people with dementia may have used the opportunity to enhance the quality of the relationship with the non-spouse carer, acting as active social agents (Bartlett & O’Connor, Citation2010) in the face of pandemic-related challenges (Dixon et al., Citation2022).
Our findings concerning formal day activities suggest another example of how the support of carers can benefit the person with dementia but carry costs for the carer. A higher level of formal day activities for the person with dementia at baseline was a direct positive predictor of loneliness in carers, and a negative indirect predictor of loneliness in person with dementia via less decline in social formal activities between assessments. Thus, whereas participation in day activities was associated with decreases in feelings of loneliness in people with dementia (Greenberg et al., Citation2020), higher levels of participation in activities potentially further limited the availability of carers to manage own emotional needs (Quinn et al., Citation2015), resulting in increases in loneliness. In other words, these findings suggest that carers’ continued support of sustaining participation in activities benefited the person with dementia at the cost of loneliness in the carer.
The current findings highlight the need for additional support for carers’ psychosocial needs (Giebel et al., Citation2021a). While restrictions imposed during the pandemic have presented challenges for delivering this support, the remote and blended approaches developed during the pandemic may enable support to be delivered in a more flexible and accessible way in the future (Wheatley et al., Citation2022). However, more evidence is needed to determine which support might best alleviate loneliness among unpaid dementia carers (Cheng & Zhang, Citation2020). A 2021 review identified potential interventions that are feasible under pandemic-related social restrictions, such as facilitating connection with peers and providing education to address barriers to social connection (Williams et al.), and testing their effectiveness among dementia carers is a direction for future research.
In addition, we have found evidence for converging wellbeing effects on loneliness in carers and people with dementia. Specifically, anxiety at baseline predicted higher levels of loneliness in both carers (direct association) and in people with dementia (via less decline in anxiety and fewer social contacts at D-C19). These findings demonstrate the importance of wellbeing indicators in understanding resilience in both people with dementia and their carers (Kim et al., Citation2021; Windle et al., Citation2021), and suggest that interventions for people with dementia that target anxiety and the sustenance of social network, for example via use of technology (Alves et al., Citation2020), may serve to alleviate loneliness in this population in the event of future pandemic restrictions and perhaps in non-pandemic situations.
Limitations
This study has important limitations. Due to the overlap of information concerning the coresident dyads, we tested separate models for people with dementia and carers. A related point is that we could not study the change in coresidence status given that this change applied to only four participants. Also, a baseline measure of loneliness was not available, and accordingly we cannot rule out the possibility that pre-existing differences in loneliness in our samples affected the findings. Nonetheless, this is the first comprehensive investigation of predictors of loneliness in people with dementia and their carers, and we will be able to include loneliness as both a predictor and outcome as additional longitudinal DETERMIND data become available.
We used FIML to deal with missingness within and between the waves. This method makes it possible to use all available information and reduce the estimation bias related to selection. For example, it enabled us to take into account that missingness was more frequent in people with more severe dementia at baseline. FIML requires some baseline information on the participants to deal with missingness. Therefore, when the contacted person with dementia or carer did not respond at all during baseline data collection, there could be unmeasured bias due to initial selection. Bias may also have been introduced within D-C19 due to the varying methods that were used as a consequence of the pandemic despite our efforts to ensure high data quality. At follow-up, some measures that were delivered at baseline changed in wording (e.g. Lubben Social Network Scale, Lubben et al., Citation2006), were omitted as they were difficult to administer remotely (i.e. Standardized Mini Mental State Examination, Molloy & Standish, Citation1997), or were administered using a different method if the person with dementia was unable to participate in the study (e.g. CDR, Morris, Citation1993). CDR administration at follow-up involved asking the carer to score the measure, either in discussion with the researcher during telephone interviews or on their own in self-completion paper-based questionnaires, as opposed to the researchers’ scoring it based on their interviews at baseline. It is possible that this change in administration methods affected follow-up data.
Finally, our dataset did not include measures of changes in caregiving approach under lockdown, which we speculate may drive dyadic processes (e.g. investment in relationship) that shape loneliness in people with dementia and carers. Future research could develop and implement such measures to examine our interpretations, and whether carers experienced positive psychological outcomes such as self-discovery and self-affirmation (Tulloch et al., Citation2021) as a result of their caregiving decisions.
Conclusions
Through a longitudinal investigation of loneliness in the Covid-19 pandemic, we provide evidence of the differential paths predicting loneliness in people with dementia and carers. Whereas social resources predicted decreases in loneliness in people with dementia, the same resources predicted increases in loneliness in carers via processes that relate to the caregiving dyad. The current findings are in accord with additional DETERMIND evidence that highlights the vulnerability of carers of people with dementia in the Covid-19 pandemic (Hicks et al., Citation2022), and extend emerging evidence on the psychological costs of caregiving in the Covid-19 pandemic (Altieri & Santangelo, Citation2021). Together, our findings suggest that in the face of challenging circumstances, carers prioritized providing good quality care for the person with dementia that protected that person from loneliness at the cost of experiencing loneliness themselves. In this sense, the current findings are a testament to the power of adaptation and selflessness in dementia caregiving dyads to cope with adversity.
Ethical approval
Ethics approval for the DETERMIND and DETERMIND-C19 studies were obtained by the HRA Brighton and Sussex Research Ethics Committee [REC 19/LO/0528. IRAS 261263].
Supplemental Material
Download MS Word (67 KB)Acknowledgements
We thank all the people with dementia and carers that gave their time to be part of this study.
Disclosure statement
This project was supported by UK Research and Innovation (UKRI) through the Economic and Social Research Council (ESRC) by a research grant which supported travel expenses. The project used data from the DETERMIND project funded by UKRI/ESRC and the National Institute of Health and Social Research (NIHR) that supported the participation of all authors. Both grants were paid to institutions, not personally. The following are in addition to the above and are outside the submitted work. SB reports ESRC, UKRI, and NIHR institutional grant funding and personal fees and non-financial support from medicolegal reports, Lilly, personal fees from Axovant, personal fees from Lundbeck, personal fees from Nutricia, and honoraria from the Hamad Medical Service and for lectures and talks. He is a Trustee of the Alzheimer’s Society, Editor in Chief of the International Journal of Geriatric Psychiatry (personal honorarium) and a Non-Executive Director of Somerset Partnership NHS Foundation Trust. BH reports European Union (EU) ERASMAS institutional grant funding and personal lecturing fees from Bournemouth University. CB reports institutionally paid grants from: Alzheimer’s Society, Addenbrooke’s Charitable Trust, ESRC, EU, Canadian Institute of Health Research, Alzheimer’s research UK (ARUK), NIHR, National Institute on Aging/National Institutes of Health, Innovative medicines Initiative (EPAD) Innovative Medicines Initiative Joint Undertaking, UKRI GCRF, and the Gillings Family Foundation. She has received personal reimbursement for travel/accommodation/subsistence expenses to attend meetings/conferences as speaker. She is a member of: NIA HRS Data Monitoring Committee with honoraria paid to employing institution (University of Cambridge) and travel and subsistence expenses reimbursed; AXA Research Fund Scientific Board (honoraria paid to employer; DBT/Wellcome Trust India Alliance Fellowship Selection Committee (honoraria paid to self, travel & subsistence expenses reimbursed), Chair of the Canadian Longitudinal Study on Aging Scientific Advisory Board (travel/subsistence expenses reimbursed); Co-Chair of the Alzheimer’s Society Research Strategy Council (travel/subsistence expenses reimbursed); Chair of the BRAIN & HEADING International Oversight Committee (travel/subsistence expenses reimbursed); member of The Irish Longitudinal Study on Aging (TILDA) Scientific Advisory Board Travel (subsistence expenses reimbursed); CUHK Project Advisory Board; University of Sheffield Health Lifespan Institute Advisory Board; ATHLOS Advisory Board (travel/subsistence expenses reimbursed); Barcelona Brain Health Initiative Scientific Advisory Board (travel/subsistence expenses reimbursed); DZNE International Scientific Review Panel (travel/subsistence expenses reimbursed); Scientific Advisory Board for UKPRP Air pollution and cognitive health consortium, InSPIRE. She is: Chair, Faculty of Public Health Academic & Research Committee (travel/subsistence expenses reimbursed); Trustee, Faculty of Public Health Board (travel/subsistence expenses reimbursed); Chair Royal College of Physicians Advisory Group on Health Inequalities (travel/subsistence expenses reimbursed); Chair, Public Health England - University of Cambridge Academic Liaison Committee meeting; and Co-Chair, East of England Public Health England Research and Evaluation Hub. MD has the following unpaid positions: Carers UK (Charity Trustee); The Centre for Ageing Better (Charity Trustee); Crossroads Care Richmond & Kingston (Charity Trustee); The Friends of Queen Mary’s Hospital Roehampton (Charity Trustee). AT reports institutional grants from: the Alzheimer’s Society, and UKRI. RP, SR, PH, JR, JD, EM, and LR make no other disclosures.
Data availability statement
Deidentified participant data will be available with investigator support from 9 months after publication of the last DETERMIND-C19 paper via [email protected] for researchers whose proposed use of the data has been approved by the DETERMIND Programme Management Board. The study protocol will be available as a supporting document.
Additional information
Funding
Notes
1 We examined differences in background variables and cognitive impairment between 1. people with dementia and 2. carers, who participated in both waves (vs. baseline only) via chi-square and t tests. Among people with dementia, those who participated in both waves had a lower CDR score, M(SD)=0.7(0.4) vs. 0.8(0.5), t(195)=3.01, p = 0.003. Among carers, those who participated in both waves were fewer with no qualification 7% vs. 12%, and more with higher education, 35% vs. 28.5%, χ2(4)=11.28, p=.02. There were no significant differences in age, gender, marital status, education, ethnicity (White vs. non-White), occupational class, index of multiple deprivation, time since diagnosis of dementia, and physical health (among people with dementia and carers), nor in working/volunteering status and home ownership (among carers). Our use of FIML method for missingness meant that the few above differences were taken into account in the models.
References
- Acock, A. C. (2005). Working with missing values. Journal of Marriage and Family, 67(4), 1012–1028. https://doi.org/10.1111/j.1741-3737.2005.00191.x
- Altieri, M., & Santangelo, G. (2021). The psychological impact of COVID-19 pandemic and lockdown on caregivers of people with dementia. The American Journal of Geriatric Psychiatry, 29(1), 27–34.
- Alves, G. S., Casali, M. E., Veras, A. B., Carrilho, C. G., Bruno Costa, E., Rodrigues, V. M., & Dourado, M. C. N. (2020). A systematic review of home-setting psychoeducation interventions for behavioral changes in dementia: Some lessons for the COVID-19 pandemic and post-pandemic assistance. Frontiers in Psychiatry, 11, 577871–571028. https://doi.org/10.3389/fpsyt.2020.577871
- Asthana, N. K., Mehaffey, E., & Sewell, D. D. (2021). COVID-19 associated suicidal ideation in older adults: Two case reports with a review of the literature. The American Journal of Geriatric Psychiatry, 29(11), 1101–1116. https://doi.org/10.1016/j.jagp.2021.05.026
- Balouch, S., Rifaat, E., Chen, H. L., & Tabet, N. (2019). Social networks and loneliness in people with Alzheimer’s dementia. International Journal of Geriatric Psychiatry, 34(5), 666–673. https://doi.org/10.1002/gps.5065
- Bartlett, R., & O’Connor, D. (2010). Broadening the dementia debate: Towards social citizenship. Policy Press.
- Beeson, R. A. (2003). Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17(3), 135–143. https://doi.org/10.1016/S0883-9417(03)00057-8
- Beeson, R., Horton-Deutsch, S., Farran, C., & Neundorfer, M. (2000). Loneliness and depression in caregivers of persons with Alzheimer’s disease or related disorders. Issues in Mental Health Nursing, 21(8), 779–806. https://doi.org/10.1080/016128400750044279
- Bengtson, V. L., & Schrader, S. S. (1982). Parents-child relations. In D. J. Mangen & W. A. Peterson (Eds.), Research instruments in social gerontology (pp. 115–128). University of Minnesota Press.
- Brown, J., Kirk-Wade, E. (2021). Coronavirus: A history of English lockdown laws. Retrieved from https://researchbriefings.files.parliament.uk/documents/CBP-9068/CBP-9068.pdf
- Bu, F., Steptoe, A., & Fancourt, D. (2020). Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Social Science & Medicine (1982), 265, 113521. https://doi.org/10.1016/j.socscimed.2020.113521
- Cheng, S.-T., & Zhang, F. (2020). A comprehensive meta-review of systematic reviews and meta-analyses on nonpharmacological interventions for informal dementia caregivers. BMC Geriatrics, 20(1), 137. https://doi.org/10.1186/s12877-020-01547-2
- Chiao, C. Y., Wu, H. S., & Hsiao, C. Y. (2015). Caregiver burden for informal caregivers of patients with dementia: A systematic review. International Nursing Review, 62(3), 340–350. https://doi.org/10.1111/inr.12194
- Clare, L., Wu, Y.-T., Quinn, C., Jones, I. R., Victor, C. R., Nelis, S. M., Martyr, A., Litherland, R., Pickett, J. A., Hindle, J. V., Jones, R. W., Knapp, M., Kopelman, M. D., Morris, R. G., Rusted, J. M., Thom, J. M., Lamont, R. A., Henderson, C., Rippon, I., Hillman, A., & Matthews, F. E. (2019). A comprehensive model of factors associated with capability to “live well” for family caregivers of people living with mild-to-moderate dementia: Findings from the IDEAL Study. Alzheimer Disease and Associated Disorders, 33(1), 29–35. https://doi.org/10.1097/WAD.0000000000000285
- Cohen-Mansfield, J., Hazan, H., Lerman, Y., & Shalom, V. (2016). Correlates and predictors of loneliness in older-adults: A review of quantitative results informed by qualitative insights. International Psychogeriatrics, 28(4), 557–576. https://doi.org/10.1017/S1041610215001532
- Cohen-Mansfield, J., & Perach, R. (2015). Interventions for alleviating loneliness among older persons: A critical review. American Journal of Health Promotion: AJHP, 29(3), e109–e125. https://doi.org/10.4278/ajhp.130418-LIT-182
- Dahlberg, L., McKee, K. J., Frank, A., & Naseer, M. (2022). A systematic review of longitudinal risk factors for loneliness in older adults. Aging & Mental Health, 26(2), 225-249. https://doi.org/10.1080/13607863.2021.1876638
- D’Cruz, M., & Banerjee, D. (2020a). Caring for persons living with dementia during the COVID-19 pandemic: Advocacy perspectives from India. Frontiers in Psychiatry, 11, 603231. https://doi.org/10.3389/fpsyt.2020.603231
- D’Cruz, M., & Banerjee, D. (2020b). ‘An invisible human rights crisis’: The marginalization of older adults during the COVID-19 pandemic – An advocacy review. Psychiatry Research, 292, 113369. https://doi.org/10.1016/j.psychres.2020.113369
- Dixon, J., Hicks, B., Gridley, K., Perach, R., Colclough, C., Baxter, K., … Banerjee, S. (2022). ‘Pushing back’: People newly diagnosed with dementia and their experiences of the Covid-19 pandemic in England. Manuscript submitted for publication.
- El Haj, M., Jardri, R., Larøi, F., & Antoine, P. (2016). Hallucinations, loneliness, and social isolation in Alzheimer’s disease. Cognitive Neuropsychiatry, 21(1), 1–13. https://doi.org/10.1080/13546805.2015.1121139
- Farina, N., Hicks, B., Baxter, K., Birks, Y., Brayne, C., Dangoor, M., Dixon, J., Harris, P. R., Hu, B., Knapp, M., Miles, E., Perach, R., Read, S., Robinson, L., Rusted, J., Stewart, R., Thomas, A., Wittenberg, R., & Banerjee, S. (2020). DETERMinants of quality of life, care and costs, and consequences of INequalities in people with Dementia and their carers (DETERMIND): A protocol paper. International Journal of Geriatric Psychiatry, 35(3), 290–301. https://doi.org/10.1002/gps.5246
- Frenkel-Yosef, M., Maytles, R., & Shrira, A. (2020). Loneliness and its concomitants among older adults during the COVID-19 pandemic. International Psychogeriatrics, 32(10), 1257–1259. https://doi.org/10.1017/S1041610220003476
- Geirdal, A. Ø., Ruffolo, M., Leung, J., Thygesen, H., Price, D., Bonsaksen, T., & Schoultz, M. (2021). Mental health, quality of life, wellbeing, loneliness and use of social media in a time of social distancing during the COVID-19 outbreak. A cross-country comparative study. Journal of Mental Health, 30(2), 148–148. https://doi.org/10.1080/09638237.2021.1875413
- Giebel, C., Cannon, J., Hanna, K., Butchard, S., Eley, R., Gaughan, A., Komuravelli, A., Shenton, J., Callaghan, S., Tetlow, H., Limbert, S., Whittington, R., Rogers, C., Rajagopal, M., Ward, K., Shaw, L., Corcoran, R., Bennett, K., & Gabbay, M. (2021a). Impact of COVID-19 related social support service closures on people with dementia and unpaid carers: A qualitative study. Aging & Mental Health, 25(7), 1281–1288. https://doi.org/10.1080/13607863.2020.1822292
- Giebel, C., Pulford, D., Cooper, C., Lord, K., Shenton, J., Cannon, J., Shaw, L., Tetlow, H., Limbert, S., Callaghan, S., Whittington, R., Rogers, C., Komuravelli, A., Rajagopal, M., Eley, R., Downs, M., Reilly, S., Ward, K., Gaughan, A., … Gabbay, M. (2021b). COVID-19-related social support service closures and mental well-being in older adults and those affected by dementia: A UK longitudinal survey. BMJ Open, 11(1), e045889. https://doi.org/10.1136/bmjopen-2020-045889
- Greenberg, N. E., Wallick, A., & Brown, L. M. (2020). Impact of COVID-19 pandemic restrictions on community-dwelling caregivers and persons with dementia. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S220–S221. https://doi.org/10.1037/tra0000793
- Gubler, D. A., Makowski, L. M., Troche, S. J., & Schlegel, K. (2021). Loneliness and well-being during the Covid-19 pandemic: Associations with personality and emotion regulation. Journal of Happiness Studies, 22(5), 2323–2342. https://doi.org/10.1007/s10902-020-00326-5
- Hansen, T., Nilsen, T. S., Yu, B., Knapstad, M., Skogen, J. C., Vedaa, Ø., & Nes, R. B. (2021). Locked and lonely? A longitudinal assessment of loneliness before and during the COVID-19 pandemic in Norway. Scandinavian Journal of Public Health, 49(7), 766–773. https://doi.org/10.1177/1403494821993711
- Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J. G. (2009). Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
- Hawkley, L. C., & Cacioppo, J. T. (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. https://doi.org/10.1007/s12160-010-9210-8
- Hicks, B., Read, S., Hu, B., Wittenberg, R., Grahamslaw, A., Karim, A., … Banerjee, S. (2022). A cohort study of the impact of COVID-19 on the quality of life of people newly diagnosed with dementia and their family carers. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 8, e12236. https://doi.org/10.1002/trc2.12236.wileyonlinelibrary.com/journal/trc2
- Holmén, K., Ericsson, K., & Winblad, B. (2000). Social and emotional loneliness among non-demented and demented elderly people. Archives of Gerontology and Geriatrics, 31(3), 177–192. https://doi.org/10.1016/S0167-4943(00)00070-4
- Hu, L. t., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
- Hughes, M. E., Waite, L. J., Hawkley, L. C., & Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. https://doi.org/10.1177/0164027504268574
- Iacobucci, G. (2020). Covid-19: UK lockdown is “crucial” to saving lives, say doctors and scientists. BMJ (Clinical Research ed.), 368, m1204. https://doi.org/10.1136/bmj.m1204
- Jaremka, L. M., Andridge, R. R., Fagundes, C. P., Alfano, C. M., Povoski, S. P., Lipari, A. M., Agnese, D. M., Arnold, M. W., Farrar, W. B., Yee, L. D., Carson, W. E., Bekaii-Saab, T., Martin, E. W., Schmidt, C. R., & Kiecolt-Glaser, J. K. (2014). Pain, depression, and fatigue: Loneliness as a longitudinal risk factor. Health Psychology, 33(9), 948–957. https://doi.org/10.1037/a0034012
- Johansson, M. F., McKee, K. J., Dahlberg, L., Williams, C. L., Summer Meranius, M., Hanson, E., Magnusson, L., Ekman, B., & Marmstål Hammar, L. (2021). A comparison of spouse and non-spouse carers of people with dementia: A descriptive analysis of Swedish national survey data. BMC Geriatrics, 21(1), 338. https://doi.org/10.1186/s12877-021-02264-0
- Kang, Y., Cosme, D., Pei, R., Pandey, P., Carreras-Tartak, J., & Falk, E. B. (2021). Purpose in life, loneliness, and protective health behaviors during the COVID-19 pandemic. The Gerontologist, 61(6), 878–887. https://doi.org/10.1093/geront/gnab081
- Kearns, S. M., & Creaven, A.-M. (2017). Individual differences in positive and negative emotion regulation: Which strategies explain variability in loneliness? Personality and Mental Health, 11(1), 64–74. https://doi.org/10.1002/pmh.1363
- Killgore, W. D. S., Cloonan, S. A., Taylor, E. C., Lucas, D. A., & Dailey, N. S. (2020). Loneliness during the first half-year of COVID-19 Lockdowns. Psychiatry Research, 294, 113551. https://doi.org/10.1016/j.psychres.2020.113551
- Kim, E. S., Tkatch, R., Martin, D., MacLeod, S., Sandy, L., & Yeh, C. (2021). Resilient aging: Psychological well-being and social well-being as targets for the promotion of healthy aging. Gerontology & Geriatric Medicine, 7, 23337214211002951. https://doi.org/10.1177/23337214211002951
- Kline, R. B. (2005). Principles and practice of structural equation modelling (3rd ed.) The Guilford Press.
- Leigh-Hunt, N., Bagguley, D., Bash, K., Turner, V., Turnbull, S., Valtorta, N., & Caan, W. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health, 152, 157–171. https://doi.org/10.1016/j.puhe.2017.07.035
- Liu, K. Y., Howard, R., Banerjee, S., Comas‐Herrera, A., Goddard, J., Knapp, M., Livingston, G., Manthorpe, J., O’Brien, J. T., Paterson, R. W., Robinson, L., Rossor, M., Rowe, J. B., Sharp, D. J., Sommerlad, A., Suárez‐González, A., & Burns, A. (2021). Dementia wellbeing and COVID-19: Review and expert consensus on current research and knowledge gaps. International Journal of Geriatric Psychiatry, 36(11), 1597–1639. https://doi.org/10.1002/gps.5567
- Lubben, J., Blozik, E., Gillmann, G., Iliffe, S., von Renteln Kruse, W., Beck, J. C., & Stuck, A. E. (2006). Performance of an abbreviated version of the Lubben Social Network Scale among three european community-dwelling older adult populations. The Gerontologist, 46(4), 503–513. https://doi.org/10.1093/geront/46.4.503
- Luchetti, M., Lee, J. H., Aschwanden, D., Sesker, A., Strickhouser, J. E., Terracciano, A., & Sutin, A. R. (2020). The trajectory of loneliness in response to COVID-19. American Psychologist, 75(7), 897–908. https://doi.org/10.1037/amp0000690
- Luichies, I., Goossensen, A., & van der Meide, H. (2021). Normative tensions in filial caring for a mother with dementia: A narrative perspective. Dementia, 20(8), 2766–2778. https://doi.org/10.1177/14713012211014003
- Macdonald, B., & Hülür, G. (2021). Well-being and loneliness in Swiss older adults during the COVID-19 pandemic: The role of social relationships. The Gerontologist, 61(2), 240–250. https://doi.org/10.1093/geront/gnaa194
- MacLeod, S., Musich, S., Hawkins, K., Alsgaard, K., & Wicker, E. R. (2016). The impact of resilience among older adults. Geriatric Nursing (New York, N.Y.), 37(4), 266–272. https://doi.org/10.1016/j.gerinurse.2016.02.014
- Martyr, A., Nelis, S. M., Quinn, C., Wu, Y.-T., Lamont, R. A., Henderson, C., Clarke, R., Hindle, J. V., Thom, J. M., Jones, I. R., Morris, R. G., Rusted, J. M., Victor, C. R., & Clare, L. (2018). Living well with dementia: A systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychological Medicine, 48(13), 2130–2139. https://doi.org/10.1017/S0033291718000405
- McGinty, E. E., Presskreischer, R., Han, H., & Barry, C. L. (2020). Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA, 324(1), 93–94. https://doi.org/10.1001/jama.2020.9740
- Meredith, W., & Tisak, J. (1990). Latent curve analysis. Psychometrika, 55(1), 107–122. https://doi.org/10.1007/BF02294746
- Molloy, D. W., & Standish, T. I. M. (1997). A guide to the standardized mini-mental state examination. International Psychogeriatrics, 9(S1), 87–94. https://doi.org/10.1017/S1041610297004754
- Morris, J. C. (1993). The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology, 43(11), 2412–2414. https://doi.org/10.1212/WNL.43.11.2412-a
- Moyle, W., Kellett, U., Ballantyne, A., & Gracia, N. (2011). Dementia and loneliness: An Australian perspective. Journal of Clinical Nursing, 20(9–10), 1445–1453. https://doi.org/10.1111/j.1365-2702.2010.03549.x
- Muthén, L. K., Muthén, B. O. (n.d.). Mplus user’s guide (8th ed., Vol. 8). Retrieved from www.StatModel.com
- National Alzheimer’s Coordinating Center. (2021). CDR® Dementia Staging Instrument calculator. Retrieved from https://naccdata.org/data-collection/tools-calculators/cdr
- ONS. (2018). Personal well-being user guidance – Office for National Statistics. Retrieved June 3, 2021, from https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/methodologies/personalwellbeingsurveyuserguide
- Peng, S., & Roth, A. R. (2021). Social isolation and loneliness before and during the COVID-19 pandemic: A longitudinal study of U.S. adults older than 50. The Journals of Gerontology: Series B, 1-6. https://doi.org/10.1093/geronb/gbab068
- Preece, D. A., Goldenberg, A., Becerra, R., Boyes, M., Hasking, P., & Gross, J. J. (2021). Loneliness and emotion regulation. Personality and Individual Differences, 180, 110974. https://doi.org/10.1016/j.paid.2021.110974
- Quinn, C., Clare, L., & Woods, R. T. (2015). Balancing needs: The role of motivations, meanings and relationship dynamics in the experience of informal caregivers of people with dementia. Dementia, 14(2), 220–237. https://doi.org/10.1177/1471301213495863
- Rabin, R., & Charro, F. d. (2001). EQ-SD: A measure of health status from the EuroQol Group. Annals of Medicine, 33(5), 337–343. https://doi.org/10.3109/07853890109002087
- Rajagopalan, J., Arshad, F., Hoskeri, R. M., Nair, V. S., Hurzuk, S., Annam, H., … Alladi, S. (2022). Experiences of people with dementia and their caregivers during the COVID-19 pandemic in India: A mixed-methods study. Dementia, 21(1), 214-235. https://doi.org/10.1177/14713012211035371
- Rippon, I., Quinn, C., Martyr, A., Morris, R., Nelis, S. M., Jones, I. R., Victor, C. R., & Clare, L. (2020). The impact of relationship quality on life satisfaction and well-being in dementia caregiving dyads: Findings from the IDEAL study. Aging & Mental Health, 24(9), 1411–1420. https://doi.org/10.1080/13607863.2019.1617238
- Russell, D., Peplau, L. A., & Cutrona, C. E. (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. https://doi.org/10.1037/0022-3514.39.3.472
- Savla, J., Roberto, K. A., Blieszner, R., McCann, B. R., Hoyt, E., & Knight, A. L. (2021). Dementia caregiving during the “stay-at-home” phase of COVID-19 Pandemic. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 76(4), e241–e245. https://doi.org/10.1093/geronb/gbaa129
- Snape, D., & Martin, G. (2018). Measuring loneliness: Guidance for use of the national indicators on surveys. Office for National Statistics.
- Steenfeldt, V. Ø., Aagerup, L. C., Jacobsen, A. H., & Skjødt, U. (2021). Becoming a family caregiver to a person with dementia: A literature review on the needs of family caregivers. SAGE Open Nursing, 7, 23779608211029073. https://doi.org/10.1177/23779608211029073
- Stirling, C., Andrews, S., Croft, T., Vickers, J., Turner, P., & Robinson, A. (2010). Measuring dementia carers’ unmet need for services – An exploratory mixed method study. BMC Health Services Research, 10(1), 122. 10.1186/1472-6963-10-122
- Sutin, A. R., Luchetti, M., & Terracciano, A. (2020). Has loneliness increased during COVID-19? Comment on “Loneliness: A signature mental health concern in the era of COVID-19”. Psychiatry Research, 291, 113295–113295. https://doi.org/10.1016/j.psychres.2020.113295
- Tam, M. T., Dosso, J. A., & Robillard, J. M. (2021). The impact of a global pandemic on people living with dementia and their care partners: Analysis of 417 Lived experience reports. Journal of Alzheimer’s Disease: JAD, 80(2), 865–875. https://doi.org/10.3233/JAD-201114
- Tulloch, K., McCaul, T., & Scott, T. L. (2022). Positive aspects of dementia caregiving during the COVID-19 pandemic. Clinical Gerontologist, 45(1), 86–96. https://doi.org/10.1080/07317115.2021.1929630
- van Tilburg, T. G., Steinmetz, S., Stolte, E., van der Roest, H., & de Vries, D. H. (2021). Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. The Journals of Gerontology: Series B, 76(7), e249–e255. https://doi.org/10.1093/geronb/gbaa111
- van Wijngaarden, E., van der Wedden, H., Henning, Z., Komen, R., & The, A.-M. (2018). Entangled in uncertainty: The experience of living with dementia from the perspective of family caregivers. PLoS One, 13(6), e0198034. https://doi.org/10.1371/journal.pone.0198034
- Victor, C. R., Rippon, I., Nelis, S. M., Martyr, A., Litherland, R., Pickett, J., Hart, N., Henley, J., Matthews, F., & Clare, L. (2020). Prevalence and determinants of loneliness in people living with dementia: Findings from the IDEAL programme. International Journal of Geriatric Psychiatry, 35(8), 851–858. https://doi.org/10.1002/gps.5305
- Victor, C. R., Rippon, I., Quinn, C., Nelis, S. M., Martyr, A., Hart, N., … Clare, L. (2021). The prevalence and predictors of loneliness in caregivers of people with dementia: Findings from the IDEAL programme. Aging & Mental Health, 25(7), 1232–1238. https://doi.org/10.1080/13607863.2020.1753014
- Wheatley, A., Poole, M., & Robinson, L. (2022). Changes to postdiagnostic dementia support in England and Wales during the COVID-19 pandemic: A qualitative study. BMJ Open, 12(2), e059437. https://doi.org/10.1136/bmjopen-2021-059437
- Williams, C. Y. K., Townson, A. T., Kapur, M., Ferreira, A. F., Nunn, R., Galante, J., Phillips, V., Gentry, S., & Usher-Smith, J. A. (2021). Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: A rapid systematic review. PLoS One, 16(2), e0247139–10. 1371/journal.pone.0247139
- Windle, G., Hoare, Z., Woods, B., Huisman, M., & Burholt, V. (2021). A longitudinal exploration of mental health resilience, cognitive impairment and loneliness. International Journal of Geriatric Psychiatry, 36(7), 1020–1028. https://doi.org/10.1002/gps.5504
- World Health Organization. (2020, March 11). WHO Director-General’s opening remarks at the media briefing on COVID-19–2020. Retrieved from https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020
- Zucca, M., Isella, V., Lorenzo, R. D., Marra, C., Cagnin, A., Cupidi, C., Bonanni, L., Laganà, V., Rubino, E., Vanacore, N., Agosta, F., Caffarra, P., Sambati, R., Quaranta, D., Guglielmi, V., Appollonio, I. M., Logroscino, G., Filippi, M., Tedeschi, G., … Bruni, A. C. (2021). Being the family caregiver of a patient with dementia during the coronavirus disease 2019 lockdown. Frontiers in Aging Neuroscience, 13(132), 653533. https://doi.org/10.3389/fnagi.2021.653533
