Abstract
Objectives
Caring for a relative with dementia can be extremely challenging especially when someone presents with behavioural and psychological symptoms of dementia (BPSD). The training provided to informal carers is varied and inconsistent. Group-based training programmes are often prescribed but their impact on care-recipient wellbeing and symptomology is yet to be well established. This review synthesises the literature on consensus, themes and effectiveness of informal-carer, group-based educational training programmes on BPSD symptoms.
Methods
Ten papers were included of which very few considered BPSD outcomes as their primary aim of investigation.
Results
Methodological and theoretical approaches across the empirical papers varied considerably. Generally, studies of higher quality and with some positive results on BPSD outcomes tended to incorporate teaching on structured problem-solving skills. Studies measuring for longer term changes also tended to conclude more beneficial outcomes. The length and duration of groups and the group-sizes appeared inconsequential to BPSD outcomes.
Conclusion
The empirical evidence is weak for carer group interventions in the management of BPSD. Practice reasons for this are discussed. Future studies designed to measure BPSD as a primary outcome would be a welcome addition to the literature.
Introduction
Dementia and BPSD
Dementia is a progressive neurodegenerative condition that most often affects memory, language, and other cognitive functions which impact greatly on daily functioning. Behavioural and psychological symptoms of dementia (BPSD) is an umbrella term describing all other ‘neuro-psychiatric’ symptoms common in dementia (Finkel et al., Citation1997; Lawlor, Citation2002). BPSD can include agitation, irritability, inappropriate behaviours, depression, delusions and anxiety amongst others (Cerejeira et al., Citation2012; Taemeeyapradit et al., Citation2014). An estimated 80% of people living with dementia (PLWD) experience BPSD symptoms (Margallo-Lana et al., 2001; Aalten et al., Citation2003). Research suggests that BPSD contribute not only to high levels of distress amongst PLWD and their carers but are also associated with accelerated disease progression (Paulsen et al., Citation2000), and earlier institutionalisation (Luppa et al., Citation2008).
The National Institute for Health and Care Excellence (NICE) recommends non-pharmacological assessment of environmental factors as the first-line treatment for agitation, aggression, distress and psychosis in PLWD (NICE, Citation2018). However, where symptoms pose a risk to person or severe distress, antipsychotic medication is recommended, often indicated, and commonly used to treat BPSD with a prescription rate of 20–50% (Brimelow et al., Citation2019; Lee et al., Citation2004; Sturm et al., Citation2018). Such medications have widely recognised side effects and require specialist management and frequent review (Ohno et al., Citation2019).
Several theoretical frameworks have been proposed to explain the aetiology of BPSD, without universal consensus. The ‘needs-driven dementia comprised behaviour’ (NDB) model (Algase et al., Citation1996; Cohen-Mansfield, Citation2001) theorises that behaviours are a result of unmet physiological and social needs, common in dementia due in part to communication difficulties between care-recipient and care-provider. Hall and Buckwalter (Citation1987) argue that BPSD are common due to a ‘progressively lowered stress threshold’ (PLST) in PLWD. Behavioural learning theory explains BPSD through operant conditioning, in which symptoms are positively reinforced through carer-attention (Teri et al., Citation1998). These various factors likely act in combination to produce a BPSD profile and thus hypothesised mechanisms of change in non-pharmacological interventions may be underpinned by these theoretical perspectives. For example, change could occur through improving communication skills or using behavioural assessment to understand and change reinforcement contingencies.
Informal caregiver training
An informal carer is anyone who provides care outside of a ‘professional’ or paid role; this could for example be a family member, friend, or neighbour. PLWD have complex difficulties often requiring support from others with activities of daily living. Support needs are also changeable due to the progressive nature of the disease. There are an estimated 700,000 informal carers providing support to PLWD in the UK (Lewis et al., Citation2014), the majority of whom are family members with little previous experience or knowledge of dementia care. More recent reports looking at informal carers, indiscriminate across health conditions, have found that since the global Covid-19 pandemic more people than ever are providing informal care (Carers Week Report, Citation2020), as well as increased hours of care (Carers UK Report, 2020). In moving away from an overly biomedical model to the treatment of dementia, NICE guidelines currently state that all informal carers should receive psychoeducation and skills training interventions to support them in their caring roles at the point of diagnosis (NICE, Citation2018). There is however very little guidance on how this should be delivered or what constitutes ‘effective’ support. The NICE guidelines also state that interventions are most likely to be effective when offered in ‘group-settings’.
Rationale for review
The limited research that exists in this area has routinely focussed on carer-wellbeing outcomes (e.g. carer quality of life, burden and depression), underpinned by a theoretical assumption that improved carer well-being should have an associative positive effect on those for whom they provide care. Black and Almeida (Citation2004) did find a moderately strong association between BPSD, and caregiver burden and depression rates. However, their systematic review highlighted a paucity of data and methodological issues as well as a suggestion that carer outcomes are more predictive of PLWD institutionalisation than of BPSD.
There are several recent systematic reviews that have investigated the impact of psycho-educational and non-pharmaceutical interventions for family-carers’ sense of burden, wellbeing, mood and quality of life, with evidence of positive effects (Cheng & Zhang, Citation2020; Frias et al., Citation2020). Poon (Citation2019) recently conducted a review and meta-analysis of dyadic psychological interventions which concluded that psychosocial interventions in clinical practice should aim to involve both the carer and the PLWD. Dual-participation however, is regrettably not always possible or warranted in clinical practice where the PLWD may present with apathy, disengagement or distress in receiving direct input.
There are no reviews to date, which have examined the effectiveness of informal-carer, group-based educational training programmes on, specifically, the BPSD symptoms of PLWD. This review addresses this gap, drawing inferences on the following research question; Are group-based informal carer programmes effective in reducing BPSD in PLWD? In addition, the review aims to describe common features such as content-type, dosage intensity, group size and consider whether any preliminary conclusions can be drawn as to their impact on the success of the intervention.
Materials and methods
This systematic review was conducted in a prespecified protocol, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis transport reporting systematic review recommendations (PRISMA) (Moher et al., Citation2009).
Literature search methods
The systematic literature search was conducted across PsychINFO, EMBASE, Medline, and CINALH databases using OVID and EBSCO interfaces. The population search incorporated ‘Alzheimer’s’, ‘Dementia’ and ‘Vascular’ terms. The intervention incorporated ‘Group’, ‘Training’, ‘Education’, ‘Teaching’, ‘Learning’, Psychoeducation’, ‘Carer’, ‘Caregiver’, ‘Family’ and ‘Informal’ terms. And the outcomes constituted ‘behavioural problems’, ‘psychological problems’, ‘psychiatric problems’, ‘agitation’, ‘aggression’, ‘depression’, ‘anxiety’ and ‘challenging behaviour’.
Inclusion criteria:
Randomised controlled trials (RCTs), quasi-experimental designs and patient as own comparison designs.
Group-based, face-to-face training interventions only.
Interventions for informal-carers of a person living with dementia (PLWD), only.
Peer-reviewed studies reporting quantitative results, published between 2000 and March 2020.
BPSD is evaluated, as either a primary or secondary outcome, using a measure which features in the most recent review of BPSD outcome-measures (van der Linde et al., Citation2014).
Papers written in English.
Exclusion criteria:
The intervention provided input directly to the PLWD in addition to the carer (e.g. dyadic interventions).
The intervention had a 1:1 component, as opposed to being group-based.
Interventions were delivered online or ‘virtually’.
Due to the paucity of research in this area, no studies were excluded based on sample size, hence pilot studies were also included.
Quality rating
As not all of the studies included are RCTs, quality ratings were made using the standard quality assessment criteria—’QualSyst’ (Kmet et al., Citation2004) which was specifically designed for the quality assessment of a variety of different study designs.
The QualSyst checklist assesses quality based on 14-items including randomisation, blinding, robustness of measures, sample size and subject characteristics, analytical methods, confound controlling and evidence-supported conclusions. Each item is scored a 2 for ‘yes’, 1 for ‘partial’, or 0 for ‘no’, based on whether the specific criteria are met. Item number seven was omitted for all of the literature in this review, as it relates to blinding of participants which was not possible considering the nature of intervention being offered. Summary scores are calculated based on the total obtained score, divided by the total possible score. This produces a summary decimal score where 1.0 is the maximum, of highest quality. A random sample of 33% of the papers were independently counter-quality assessed by a second reviewer. Any discrepancies were resolved through discussion and consensus, and subsequently the same principles applied to the remaining papers for any agreed changes.
Results
Included and excluded studies
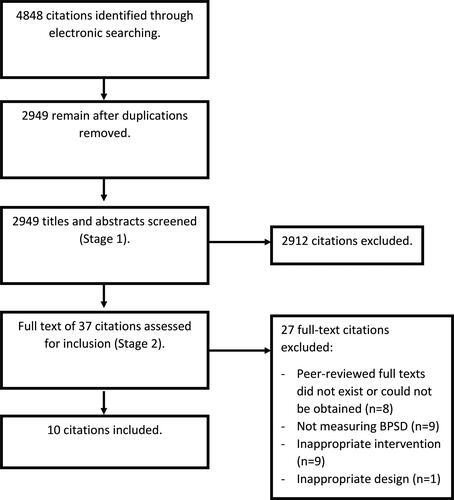
In total 4848 studies were identified initially using the established search terms (see ). Duplicates were removed and titles, abstracts, excerpts, and full papers were screened for contraventions of the inclusion criteria. The resultant total of identified papers for inclusion reached ten. outlines an overview of the included literature containing design, control type, intervention description, group facilitator and size, sessions set-up, outcomes measures, significant results related to BPSD, and quality ratings.
Table 1. Overview of included studies.
Study characteristics
Aims
All the included publications described the aim of their research as investigating the ‘effects’, ‘effectiveness’ or ‘efficacy’ of their particular group-programme. Only three studies (Chein et al., 2008; de Rotrou et al., Citation2011; Javadpour et al., Citation2009) were judged to be investigating the effects on PLWD as their primary aim. Seven out of ten were investigating the effects on carer outcomes as their primary aim, with PLWD outcomes of secondary interest (Gonzalez et al., Citation2014; Hebert et al., Citation2003; Hepburn et al., Citation2001; Kurz et al., Citation2009; Seike et al., Citation2016; Terracciano et al., Citation2020; Ulstein et al., Citation2007).
Settings
All of the included studies were conducted across a diverse geography spanning three continents. The papers were published between 2001 and 2020. Participants were selected mostly from clinical dementia services/memory clinics and third-sector organisations such as charities and societies.
Design
The majority of publications, comprised randomised controlled trials (RCTs). One study was a pilot-RCT (Gonzalez et al., Citation2014), and two were quasi-experimental pre-post designs with no control group (Javadpour et al., Citation2009; Seike et al., Citation2016). Studies with a control group opted mostly for a treatment as usual (TAU) control (Chien & Lee, Citation2008; Gonzalez et al., Citation2014; Hebert et al., Citation2003; Kurz et al., Citation2009; Ulstein et al., Citation2007, or in the case of three studies, a ‘waitlist’ control group (de Rotrou et al., Citation2011; Hepburn et al., Citation2001; Terracciano et al., Citation2020)
Session characteristics (group sizing and duration)
The makeup of the group interventions and dosages (intensity of treatment) varied considerably. Group sizes were not documented at all in three papers (Chien & Lee, Citation2008; Seike et al., Citation2016; Ulstein et al., Citation2007) and in numerous publications only an average group size or range was provided (Kurz et al., Citation2009; Terracciano et al., Citation2020). Groups ranged from four to 16 participants. Using group-range means, and absolute group sizes values, the mean group size for the interventions was calculated as 9.5 per group.
Treatment dosage varied and was calculated for the purpose of this review by multiplying number of sessions by duration of sessions in minutes. Dosage ranged from 12 to 30 h, with an average dosage of 17.85 h. The majority implemented a weekly programme of group sessions, whereas two studies opted for fortnightly meetings.
Intervention content
The level of detail describing the treatment programmes varied amongst the included publications. Several studies provided very limited detail in the form of session titles only, brief one-sentence descriptions of the session ‘headlines’, or general overall themes (Chien & Lee, Citation2008; de Rotrou et al., Citation2011; Javadpour et al., Citation2009; Kurz et al., Citation2009; Seike et al., Citation2016; Terracciano et al., Citation2020; Ulstein et al., Citation2007). For the purpose of synthetisation in this review, the training packages can be roughly divided into content-types; ‘general dementia psychoeducation’, ‘cognitive skills-based interventions’ and ‘idiosyncratic’.
General dementia psychoeducation
Three studies predominantly described classroom-style psychoeducation lectures in which several ‘stand-alone’ sessions were offered to participants providing information about different themes in each session (Javadpour et al., Citation2009; Kurz et al. Citation2009; Seike et al. Citation2016). Content includes; general information about dementia, its diagnosis, aetiology and treatments; common symptoms and challenging behaviours; examples of typical care-challenges, with strategies to help; and social support or other available resources. Kurz et al. (Citation2009) also incorporated a session on legal and insurance-related issues, while Javadpour et al. (Citation2009) included sessions on person-centred care, and oral care. All three incorporated group discussion as part of their teaching methods.
Cognitive skills-based
Five studies were considered to be predominantly cognitive skills-based in their intervention style (Gonzalez et al., Citation2014; Hebert et al., Citation2003; Hepburn et al., Citation2001; Terracciano et al., Citation2020; Ulstein et al., Citation2007). Overall, these programmes provided some limited lecture-style general knowledge about dementia but focussed in the main on skills-based cognitive techniques and strategies; their theoretical underpinnings, implementation, and evaluation. These papers tended to provide a more thorough grounding in psychological theory such as self-regulation theory, behavioural theory, stress and coping frameworks, and cognitive theory.
Hepburn et al. (Citation2001) focused on carers’ self-appraisals and beliefs about carer-identity, role, and coping abilities. Instruction, exercises and discussion were used in a ‘workshop’ fashion to foster carer-identities separate from their familial role. Abilities, and the importance of self-care were reinforced in the sessions, thereby theoretically mediating caregivers’ responses to stressful situations. In the case of the PTC programme (Cleland et al., Citation2006; Terracciano et al., Citation2020), the focus was on carer self-care, emotional awareness and regulation, and self-efficacy. Here, carers were encouraged to develop an individualised self-care action plan and practice relaxation exercises including progressive muscle relaxation. The programme incorporated elements of assertiveness training, tools for decision making and ‘tools for optimism’ (Boise et al., Citation2005).
The remaining three publications focused more on the cognitive appraisal of caring challenges, with an additional focus on solution-based problem-solving, and decision making (Gonzalez et al., Citation2014; Hebert et al., Citation2003; Ulstein et al., Citation2007). The cognitive techniques included; shifting from a global stressor to a specific stressor; breaking down a problem into distinct elements; labelling changeable and unchangeable factors; reframing; identifying and modifying dysfunctional thoughts; and developing more realistic expectations. In all cases, problem-solving techniques involved clarifying or defining a problem in the first instance. Ulstein et al. (Citation2007) and Gonzalez et al. (Citation2014) then provided a structured framework in which carers ‘brainstormed’ multiple possible solutions, considered possible outcomes, weighed up pros and cons, and planned detailed implementation and evaluation. Participants in Hebert et al.’s (Citation2003) groups were guided to integrate behavioural assessment techniques (Zarit & Zarit, Citation2011) to assess the ‘problem’ before choosing an appropriate solution. In all cases, the group attendees were encouraged to practice and implement new skills at home independently in between sessions and collaboratively evaluate through group discussion.
Idiosyncratic
The remaining two publications were not easily classified into either a distinct psychoeducation or cognitive skills-based model (Chien & Lee, Citation2008; De Rotrou & Wenisch, Citation2009). Chien and Lee (Citation2008) provided limited detail about the sessions’ content with reference to previously developed family-programmes upon which their intervention was ‘based’ (Belle et al., Citation2006; Fung & Chien, Citation2002). However, four key phases included; orientation to dementia care; education about dementia; family role and strength rebuilding; and community support resources. This overview suggests that the programme incorporated a mixture of psychoeducational teaching and cognitive appraisal techniques. A distinctive feature of this training compared to all other studies, was that the content was ‘tailored’ to the individual group needs, as the groups consisted of family members caring for the same individual. De Rotrou et al. (Citation2011) similarly provided limited information about their group intervention, stating only that it covered education, problem-solving techniques, coping strategies, behaviour and crisis management, communication skills and resource information. A key component of this training was in teaching ecological stimulation (ES) (de Rotrou & Wenisch, Citation2009) skills, encouraging carers to stimulate care recipients with tailored activities of interest which reinforce residual abilities.
Results of significance in reducing BPSD
The majority of studies in this review, six in total, did not find any significant beneficial effects of the intervention on BPSD (de Rotrou et al., Citation2011; Gonzalez et al., Citation2014; Hepburn et al., Citation2001; Kurz et al., Citation2009; Seike et al., Citation2016; Terracciano et al., Citation2020). Seike et al.’s (Citation2016) quasi-experimental design was limited to descriptive statistics. They reported a trend in which Dementia Behaviour Disturbance Scores (DBDS) increased from pre-post measurement. This most probably quantifies the progressive nature of dementia and hence, inferences about intervention effects were infeasible in the absence of a control group. Two studies exclusively used the Revised Memory and Behaviour Problem Checklist (RMBPC) to measure BPSD. Neither study found significant effects. Gonzalez et al. (Citation2014) documented a non-significant observable trend of fewer behavioural problems in the intervention group of negligible effect size (0.05 immediately after intervention, 0.11 six-weeks post-intervention). Three publications administered the Neuropsychiatric Inventory (NPI) as a measure of BPSD. In de Rotrou et al. (Citation2011) PLWD did not show significant functional, cognitive or behavioural changes compared to the control group at neither three (p = 0.92), nor six (p = 0.57) weeks post-intervention. Kurz et al. (2009) omitted to report on their NPI end-point data, hence it is assumed that no significant results were obtained. They reported that ‘time spent caregiving’ was lower in the intervention group post-intervention, also without significant effects (p = 0.19). The powerful tools for caregivers (PTC) programme (Terracciano et al. Citation2020) also concluded no significant effects on behavioural and psychological symptoms measured using the NPI, RMBPC and the Cohn–Mansfield Agitation Inventory (CMAI), despite encouraging results in relation to carer burden and depression outcomes. P-values were not provided.
Only four of the included studies reported some statistically significant results related to BPSD intervention (Chien & Lee, Citation2008; Hebert et al., Citation2003; Javadpour et al., Citation2009; Ulstein et al., Citation2007). Javadpour et al. (Citation2009) reported significantly reduced NPI scores (p = 0.001) from pre to post intervention, with a mean score of 32.41–28.59. Chien and Lee (Citation2008) documented a significant difference (p < 0.01) in mean between-group NPI scores at 12 months in favour of the intervention group. They also reported a positive significant difference in a number of instances of institutionalisation (p < 0.01) and duration (p < 0.001). Ulstein et al. (Citation2007) being the highest rated paper at quality assessment in this review, did not report significant results related to the intervention group on all primary outcomes analyses including overall NPI scores (p = 0.37 at 12 months). However, on sub-group analyses they found a significant between-group difference at 12 months in female PLWD only (p = 0.03), in favour of the intervention group. The final publication (Hebert et al. Citation2003) reported results that may be described as ‘borderline’ significant. This paper obtained the second highest rating in the quality appraisal. They reported that the frequency of behaviour and memory problems increased by 8% in the control group post-intervention and decreased in the intervention group by 4%; a difference which very nearly reached significance (p = 0.06). The cross-product, between frequency of behaviours and the intensity of the carer reaction, between the two groups reached statistical significance (p = 0.02) in favour of the intervention.
Discussion
Summary
This systematic literature review set out to investigate the effectiveness of group-based informal carer training interventions on BPSD in PLWD. Specifically, the aim was to consider whether such treatments have positive effects on BPSD symptoms, and whether the intervention characteristics affect outcomes. This review has highlighted the paucity of literature in this area. Research considering how interventions impact carer outcomes is much more widespread and, although intuitively assumed, there is little in the literature to evidence that improved carer-outcomes transfer to a reduction in BPSD in PLWD.
Ten papers were identified for inclusion. Whilst the content of the programmes could be roughly separated into two main ‘types’ consisting of general dementia education and cognitive-based strategies, there was much variability in the level of detail outlined with regards to the interventive approaches. This, along with the variability of outcome measures used to assess BPSD, and the variable quality of the research, made direct comparisons between the publications difficult. This inconsistency in approach, research quality and the difficulty in integrating findings between studies is similar to previous findings in reviews looking at non-pharmacological intervention on the effects of care-giver outcomes (Cheng & Zhang, Citation2020; Vandepitte et al., Citation2016).
Only three studies were found in which PLWD’s BPSD symptomology was a primary measure, indicating this this is a highly under-researched field. It is likely that researchers are deterred from measuring outcomes related to PLWD directly due to the complexities of doing so logistically, ethically and practicably. Researchers have called for consensus in this area to address the challenges such as; concerns about informed consent and capacity due to cognitive impairment; safeguarding issues; a lack of accessible, valid and reliable dementia-specific measures; as well interpreting results in the context of a progressive disease (Beuscher & Grando, Citation2009; West et al., Citation2017).
Despite many of the publications in this review reporting positive effects on carer outcomes (i.e. wellbeing, sense of burden and depression rates) they did not generally and convincingly find statistically significant positive results on BPSD outcomes. Three papers did report limited significant results on BPSD outcomes, and one paper reported results which were very close to reaching significance.
Methodological issues
Of those studies describing statistically significant results multiple methodological issues were of note including the omission of control groups and the presence of multiple possible confounds. Most studies provided very little detail about what other services were being offered or accessed, and it is likely that these would varying considerably across the different countries and clinical services in which the research took place. This was similar to previous reviews undertaken on informal-carer interventions (Vandepitte et al. Citation2016).
Due to the nature of the interventions it was not possible for participants to be blinded. This may have contributed to a bias in outcomes, especially as results were based on self-completed measures in which informal carers rated BPSD subjectively. There is, as yet no consensus on how to measure the construct of BPSD especially as there is no unified definition of the construct, or of the individual symptoms. Some symptoms may overlap and some may be more or less visible, or more or less likely to be recalled by informal carers who are dealing with the behavioural and personal consequences (van der Linde et al., Citation2014). Terracciano et al. (Citation2020) proposed that participation in group psycho-education may reduce the stigma associated with reporting BPSD and hence intervention-recipients may rate BPSD more readily than those in control groups. It may also be the case that with increased knowledge from interventions, informal carers are more attuned to notice signs of BPSD. Such hypotheses may explain instances in which results find no effect, or even adverse effects of training programmes.
A majority of publications measured outcomes only immediately post-intervention. Of those that did consider follow-up, the follow-up period was often short at six weeks, or six months post-intervention. Hence it is not possible to draw conclusions about the longer-term effects of group-interventions as disease progresses. Two papers which found significant results, one of which was of the highest quality rating (Ulstein et al., Citation2007), considered outcomes at 12-months post-intervention, and found significant results at this time point. This tentatively suggests that any active components of the group-interventions which are effective in reducing BPSD may take time to embed within a caregiver’s daily practice. This is of particular note, as it is rare to find significant positive results in high-quality dementia studies as late as at one-year follow up. Research investigating psychoeducational interventions and carer outcomes for instance, report efficacy in the short term, and then diminishing effects over time (Yarnoz et al., Citation2008; Zabalegui et al., Citation2008).
Due to the varied methodological issues, a clear evaluation of ‘intervention-efficacy’ is unsubstantiated here given the lack of quality of the research conducted in this area. More high-quality research must be conducted in this area to establish a consensus on the most likely effective ‘active ingredients’, and consequent mechanisms of change within group-based carer interventions on BPSD, if any.
Content-type and effectiveness
Given the caveats described above in relation to study quality and variability it is difficult to draw any conclusions within this review on the effectiveness of content-approach. However, it is of note that the two studies of highest quality rating, and with significant or near-to significant results had a key element in common; structured problem-solving skills. Using structured problem-solving to define a problem and work through active steps to resolution is a practical, tangible skill. As problem-solving is ‘task-oriented’ it is likely to have more of a direct impact on PLWD and not solely on carer-outcomes. As a result of the intervention carers may be better placed to notice triggers for some of the more noticeable BPSD symptoms such as behavioural distress and agitation, and proactively intervene before an escalation occurs. Generally, those studies which exclusively offered general psycho-education about dementia in a classroom-style format, appeared to have been of lower quality or have minimal effects on BPSD outcomes.
Dosage/group size and effectiveness
Regarding dosage, it is equally challenging to draw conclusions from the varied approaches taken in which sessions offered totalled between 12 and 30 h of intervention. It appears therefore, that time exposed to treatment may not be an important factor related to effectiveness and that instead, the approach and content may be more salient. The same can be said of group sizing, as no discernible trends can be drawn from the studies which ranged in group size considerably from five and up to 16 participants. Two of the studies which concluded significant findings did not report their group-sizings, suggesting that the researchers did not note this to be of key importance. Where it may be of importance, is in relation to clinical practice where resources are so often scarce. It would be of interest for future research in this area to consider whether dosage or group size truly are an irrelevance, in which case, shorter dosages can be offered to a higher number of service users at once; thereby providing the most efficient use of resources at lowest cost to providers.
Clinical implications
None of the programmes provided a detailed implementation protocol or session-by-session delivery guidelines, save for one paper which referred readers to a purchasable manual (Terracciano et al. Citation2020). One paper outlined that manuals would be available ‘shortly’, however these were not obtainable at the time of this review (Hebert et al. Citation2003). In order for research into this area to be replicable and consistently applicable within clinical practice, authors must provide accessible and detailed guidance. This would also generate greater scope for the development of practice-based evidence within the clinical domain.
None of the studies in this review compared results with comparable individualised approaches. There is evidence to suggest for example that individualised interventions are more effective than group-based treatments on informal carers’ outcomes such as depression (Selwood et al., Citation2007). If the same applies to PLWD outcomes and BPSD, then resources may be far better funnelled into tailor-made individualised approaches and hence research into this area should be prioritised.
Future research needs also to incorporate more diverse groups of recipients and consider how diverse participant demographics impact the efficacy of treatment. In this review, Ulstein et al. (Citation2007) found a significant positive effect on BPSD symptoms in female PLWD, only in post-hoc analysis. Due to the retrospective nature of this analysis it must be interpreted with caution, but none-the-less it raises questions about the potential differential effects of treatments on different groups of individuals who may seek support from clinical services.
Limitations of the review
Although an important contribution to the literature in this area, this review has several limitations not least the inclusion of several studies which were rated to be of low or medium research quality. Despite incorporating studies from across several continents, this review may have been limited by the exclusion of studies which were not written in English, thereby reducing the generalisability of the findings to other cultures and settings. Although all attempts were made for a comprehensive literature search, it was limited by the strategy adopted and by the exclusion of grey literature or literature which was unavailable. A considerable variation in approaches, research description detail, and data offered in the included publications meant that reviewers were limited in their ability to synthesise quantitative results. For example, very few studies provided effect sizes which would enable more informative comparison. Therefore, results were synthesised only by extracting observable themes in a descriptive and somewhat subjective manner. We were also unable to provide participant and carer relationship as this was not reported in the included papers. Future studies, and subsequently reviews, should consider providing this information as it will help us understand the findings.
One of the limitations of this study is that we only included group interventions for carers alone. Some work has focused on the formulation driven individualised interventions (Holle et al., Citation2017; Moniz-Cook et al., Citation2012) which may be more responsive to the individuals’ needs; for example, mixed group and individual interventions (Mittelman et al., Citation1996) and parallel-group interventions (Dröes et al., Citation2019). It may be that these types of interventions may be better than standalone carer interventions as it is often not possible to separate the person from the carer.
Conclusion
Generally, the publications in this review do not provide convincing evidence regarding the efficacy of group-based, informal carer training programmes on BPSD symptoms. It is also impossible to conclusively differentiate active components which are more efficacious than others. Tentative observations favour programmes with a ‘problem-solving’ focus, and longer-term outcomes, when strategies have been embedded into practice. This review highlights the lack of research investigating the impact on outcomes which directly relate to PLWD and their disease presentation. The empirical evidence for carer group interventions in BPSD management is weak. Future studies designed to measure BPSD as a primary outcome would be a welcome addition to the research literature, guiding future clinical practice and service provision.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
The author(s) reported there is no funding associated with the work featured in this article.
References
- Aalten, P., de Vugt, M. E., Lousberg, R., Korten, E., Jaspers, N., Senden, B., Jolles, J., & Verhey, F. R. J. (2003). Behavioral problems in dementia: A factor analysis of the neuropsychiatric inventory. Dementia and Geriatric Cognitive Disorders, 15(2), 99–105.
- Algase, D. L., Beck, C., Kolanowski, A., Whall, A., Berent, S., Richards, K., & Beattie, E. (1996). Need-driven dementia-compromised behavior: An alternative view of disruptive behavior. American Journal of Alzheimer’s Disease, 11(6), 10–19. https://doi.org/10.1177/153331759601100603
- Belle, S. H., Burgio, L., Burns, R., Coon, D., Czaja, S. J., Gallagher-Thompson, D., & Caregiver, E. A. S. (2006). Can providing support to dementia caregivers improve their quality of life. Annals of Internal Medicine, 145(10), I39–I39.
- Beuscher, L., & Grando, V. T. (2009). Challenges in conducting qualitative research with individuals with dementia. Research in Gerontological Nursing, 2(1), 6–11.
- Black, W., & Almeida, O. P. (2004). A systematic review of the association between the behavioral and psychological symptoms of dementia and burden of care. International Psychogeriatrics, 16(3), 295–315.
- Boise, L., Congleton, L., & Shannon, K. (2005). Empowering family caregivers: The powerful tools for caregiving program. Educational Gerontology, 31(7), 573–586. https://doi.org/10.1080/03601270590962523
- Brimelow, R. E., Wollin, J. A., Byrne, G. J., & Dissanayaka, N. N. (2019). Prescribing of psychotropic drugs and indicators for use in residential aged care and residents with dementia. International Psychogeriatrics, 31(6), 837–847. https://doi.org/10.1017/S1041610218001229
- Carers Week Report. (2020, January, 27). Carers Week 2020 Research Report: The rise in the number of unpaid carers during the coronavirus (COVID-19) outbreak. https://www.carersweek.org/images/CW%202020%20Research%20Report%20WEB.pdf?utm_source=Carers%20UK&utm_medium=email&utm_campaign=11593607_Carers%20Week%20email%20to%20profs%20and%20affs&dm_i=74C,6WHON,PF3NF,RQADF,1.
- Carers UK Report. (2020, January, 27). Caring behind closed doors: Forgotten families in the coronavirus outbreak. https://www.carersuk.org/images/News_and_campaigns/Behind_Closed_Doors_2020/Caring_behind_closed_doors_April20_pages_web_final.pdf.
- Cerejeira, J., Lagarto, L., & Mukaetova-Ladinska, E. (2012). Behavioral and psychological symptoms of dementia. Frontiers in Neurology, 3, 73.
- Cheng, S. T., & Zhang, F. (2020). A comprehensive meta-review of systematic reviews and meta-analyses on nonpharmacological interventions for informal dementia caregivers. BMC Geriatrics, 20(1), 1–24. https://doi.org/10.1186/s12877-020-01547-2
- Chien, W. T., & Lee, Y. M. (2008). A disease management program for families of persons in Hong Kong with dementia. Psychiatric Services, 59(4), 433–436. https://doi.org/10.1176/ps.2008.59.4.433
- Cleland, M., Schmall, V. L., Studervant, M., Congleton, L., Kirkbride, K., McFalls, J., & Turner, H. (2006). The caregiver helpbook: Powerful tools for caregivers. Legacy Caregiver Services.
- Cohen-Mansfield, J. (2001). Nonpharmacologic interventions for inappropriate behaviors in dementia: A review, summary, and critique. The American Journal of Geriatric Psychiatry, 9(4), 361–381. https://doi.org/10.1097/00019442-200111000-00005
- de Rotrou, J., & Wenisch, E. (2009). Stimulation cognitive et vieillissement. Gérontologie préventive. Collection abrégés de médecine. Masson.
- de Rotrou, J., Cantegreil, I., Faucounau, V., Wenisch, E., Chausson, C., Jegou, D., Grabar, S., & Rigaud, A.-S. (2011). Do patients diagnosed with Alzheimer’s disease benefit from a psycho-educational programme for family caregivers? A randomised controlled study. International Journal of Geriatric Psychiatry, 26(8), 833–842. https://doi.org/10.1002/gps.2611
- Dröes, R. M., van Rijn, A., Rus, E., Dacier, S., & Meiland, F. (2019). Utilization, effect, and benefit of the individualized Meeting Centers Support Program for people with dementia and caregivers. Clinical Interventions in Aging, 14, 1527–1553. https://doi.org/10.2147/CIA.S212852
- Finkel, S. I., Costa e Silva, J., Cohen, G., Miller, S., & Sartorius, N. (1997). Behavioral and psychological signs and symptoms of dementia: A consensus statement on current knowledge and implications for research and treatment. International Psychogeriatrics, 8(S3), 497–500. https://doi.org/10.1017/S1041610297003943
- Frias, C. E., Garcia-Pascual, M., Montoro, M., Ribas, N., Risco, E., & Zabalegui, A. (2020). Effectiveness of a psychoeducational intervention for caregivers of people with dementia with regard to burden, anxiety and depression: A systematic Review. Journal of Advanced Nursing, 76(3), 787–802.
- Fung, W. Y., & Chien, W. T. (2002). The effectiveness of a mutual support group for family caregivers of a relative with dementia. Archives of Psychiatric Nursing, 16(3), 134–144.
- Gonzalez, E. W., Polansky, M., Lippa, C. F., Gitlin, L. N., & Zauszniewski, J. A. (2014). Enhancing resourcefulness to improve outcomes in family caregivers and persons with Alzheimer’s disease: A pilot randomized trial. International Journal of Alzheimer’s Disease, 2014, 323478. https://doi.org/10.1155/2014/323478
- Hall, G. R., & Buckwalter, K. C. (1987). Progressively lowered stress threshold: A conceptual model for care of adults with Alzheimer’s disease. Archives of Psychiatric Nursing, 1(6), 399–406.
- Hebert, R., Levesque, L., Vezina, J., Lavoie, J.-P., Ducharme, F., Gendron, C., Preville, M., Voyer, L., & Dubois, M.-F. (2003). Efficacy of a psychoeducative group program for caregivers of demented persons living at home: A randomized controlled trial. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(1), S58–S67. https://doi.org/10.1093/geronb/58.1.S58
- Hepburn, K. W., Tornatore, J., Center, B., & Ostwald, S. W. (2001). Dementia family caregiver training: Affecting beliefs about caregiving and caregiver outcomes. Journal of the American Geriatrics Society, 49(4), 450–457.
- Holle, D., Halek, M., Holle, B., & Pinkert, C. (2017). Individualized formulation-led interventions for analyzing and managing challenging behavior of people with dementia – An integrative review. Aging & Mental Health, 21(12), 1229–1247. https://doi.org/10.1080/13607863.2016.1247429
- Mittelman, M. S., Ferris, S. H., Shulman, E., Steinberg, G., & Levin, B. (1996). A family intervention to delay nursing home placement of patients with Alzheimer disease. A randomized controlled trial. JAMA, 276(21), 1725–1731. https://doi.org/10.1001/jama.1996.03540210033030
- Moniz-Cook, E. D., Swift, K., James, I., Malouf, R., De Vugt, M., & Verhey, F. (2012). Functional analysis-based interventions for challenging behaviour in dementia. Cochrane Database of Systematic Reviews, (2), CD006929. https://doi.org/10.1002/14651858.CD006929.pub2
- Javadpour, A., Ahmadzadeh, L., & Bahredar, M. J. (2009). An educative support group for female family caregivers: Impact on caregivers psychological distress and patient’s neuropsychiatry symptoms. International Journal of Geriatric Psychiatry, 24(5), 469–471. https://doi.org/10.1002/gps.2138
- Kmet, L. M., Cook, L. S., & Lee, R. C. (2004). Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Heritage Foundation for Medical Research (AHFMR).
- Kurz, A., Wagenpfeil, S., Hallauer, J., Schneider-Schelte, H., & Jansen, S. (2009). Evaluation of a brief educational program for dementia carers: The AENEAS Study. International Journal of Geriatric Psychiatry, 25(8), 861–869. https://doi.org/10.1002/gps.2428
- Lawlor, B. (2002). Managing behavioural and psychological symptoms in dementia. The British Journal of Psychiatry: The Journal of Mental Science, 181(6), 463–465. https://doi.org/10.1192/bjp.181.6.463
- Lee, P. E., Gill, S. S., Freedman, M., Bronskill, S. E., Hillmer, M. P., & Rochon, P. A. (2004). Atypical antipsychotic drugs in the treatment of behavioural and psychological symptoms of dementia: Systematic review. BMJ (Clinical Research ed.), 329(7457), 75. https://doi.org/10.1136/bmj.38125.465579.55
- Lewis, F., Karlsberg Schaffer, S., Sussex, J., O’Neill, P., & Cockcroft, L. (2014). The trajectory of dementia in the UK-making a difference. Office of Health Economics Consulting Reports.
- Luppa, M., Luck, T., Brähler, E., König, H. H., & Riedel-Heller, S. G. (2008). Prediction of institutionalisation in dementia. Dementia and Geriatric Cognitive Disorders, 26(1), 65–78.
- Margallo-Lana, M., Swann, A., O’Brien, J., Fairbairn, A., Reichelt, K., Potkins, D., Mynt, P., & Ballard, C. (2001). Prevalence and pharmacological management of behavioural and psychological symptoms amongst dementia sufferers living in care environments. International Journal of Geriatric Psychiatry, 16(1), 39–44. https://doi.org/10.1002/1099-1166(200101)16:1<39::AID-GPS269>3.0.CO;2-F
- Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
- National Institute for Clinical Excellence (NICE). (2018). Dementia: assessment, management and support for people living with dementia and their carers. Methods, evidence and recommendations.
- Ohno, Y., Kunisawa, N., & Shimizu, S. (2019). Antipsychotic treatment of behavioral and psychological symptoms of dementia (BPSD): management of extrapyramidal side effects. Frontiers in Pharmacology, 10, 1045.
- Paulsen, J. S., Salmon, D. P., Thal, L. J., Romero, R., Weisstein-Jenkins, C., Galasko, D., Hofstetter, C. R., Thomas, R., Grant, I., & Jeste, D. V. (2000). Incidence of and risk factors for hallucinations and delusions in patients with probable AD. Neurology, 54(10), 1965–1971. https://doi.org/10.1212/wnl.54.10.1965
- Poon, E. (2019). A systematic review and meta-analysis of dyadic psychological interventions for BPSD, quality of life and/or caregiver burden in dementia or MCI. Clinical Gerontologist, 1–21.
- Seike, A., T. Sakurai, C. Sumigaki, A. Takeda, H. Endo, & K. Toba. (2016). Verification of Educational Support Intervention for Family Caregivers of Persons with Dementia. Wiley-Blackwell. 64: 661–663.
- Selwood, A., Johnston, K., Katona, C., Lyketsos, C., & Livingston, G. (2007). Systematic review of the effect of psychological interventions on family caregivers of people with dementia. Journal of Affective Disorders, 101(1-3), 75–89.
- Spector, A., Orrell, M., & Goyder, J. (2003). A systematic review of staff training interventions to reduce the behavioural and psychological symptoms of dementia. Ageing Research Reviews, 12(1), 354–364.
- Sturm, A. S., Trinkley, K. E., Porter, K., & Nahata, M. C. (2018). Efficacy and safety of atypical antipsychotics for behavioral symptoms of dementia among patients residing in long-term care. International Journal of Clinical Pharmacy, 40(1), 135–142. https://doi.org/10.1007/s11096-017-0555-y
- Taemeeyapradit, U., Udomittipong, D., & Tepparak, N. (2014). Characteristics of behavioral and psychological symptoms of dementia, severity and levels of distress on caregivers. Journal of the Medical Association of Thailand = Chotmaihet Thangphaet, 97(4), 423–430.
- Teri, L., Logsdon, R. G., Whall, A. L., Weiner, M. F., Trimmer, C., Peskind, E., & Thal, L. (1998). Treatment for agitation in dementia patients: A behavior management approach. Psychotherapy: Theory, Research, Practice, Training, 35(4), 436–443. https://doi.org/10.1037/h0087766
- Terracciano, A., Artese, A., Yeh, J., Edgerton, L., Granville, L., Aschwanden, D., Luchetti, M., Glueckauf, R. L., Stephan, Y., Sutin, A. R., & Katz, P. (2020). Effectiveness of powerful tools for caregivers on caregiver burden and on care recipient behavioral and psychological symptoms of dementia: A randomized controlled trial. Journal of the American Medical Directors Association, 21(8), 1121–1127.e1.
- Ulstein, I. D., Sandvik, L., Wyller, T. B., & Engedal, K. (2007). A one-year randomized controlled psychosocial intervention study among family carers of dementia patients–effects on patients and carers. Dementia and Geriatric Cognitive Disorders, 24(6), 469–475.
- van der Linde, R. M., Stephan, B. C., Dening, T., & Brayne, C. (2014). Instruments to measure behavioural and psychological symptoms of dementia. International Journal of Methods in Psychiatric Research, 23(1), 69–98.
- Vandepitte, S., Van den Noortgate, N., Putman, K., Verhaeghe, S., Faes, K., & Annemans, L. (2016). Effectiveness of supporting informal caregivers of people with dementia: A systematic review of randomized and non-randomized controlled trials. Journal of Alzheimer’s Disease: JAD, 52(3), 929–965.
- West, E., Stuckelberger, A., Pautex, S., Staaks, J., & Gysels, M. (2017). Operationalising ethical challenges in dementia research—a systematic review of current evidence. Age and Ageing, 46(4), 678–687.
- Yarnoz, A. Z., Diez, M. N., Torres, E. C., Fernández-Puebla, A. G., Porras, D. B., Higueras, E. R., & Remon, J. A. (2008). Efficacy of interventions aimed at the main carers of dependent individuals aged more than 65 years old. A systematic review. Revista Espanola de Geriatria y Gerontologia, 43(3), 157–166.
- Zabalegui, A., Bover, A., Rodriquez, E., Cabrera, E., Diaz, M., Gallart, A., González, A., Gual, P., Izquierdo, M. D., López, L., Pulpón, A. M., & Ramírez, A. (2008). Informal caregiving: Perceived needs. Nursing Science Quarterly, 21(2), 166–172.
- Zarit, S. H., & Zarit, J. M. (2011). Mental disorders in older adults: Fundamentals of assessment and treatment. Guilford Press.