Abstract
Objective
The objectives of this systematic review and meta-analysis were to identify the characteristics of internet-based psychoeducational programs for caregivers of people living with dementia and to synthesise program effectiveness.
Method
Five English databases and four Chinese databases were searched in June 2021 with no time limit applied. A narrative summary was performed to describe the characteristics of studies reviewed. Meta-analysis was applied to synthesise the pooled effects where data were available.
Results
A total of 14352 articles were identified from the database search and 19 were included in the final review. Interventions comprised educational, psychological, and behavioural training relevant to dementia care. Program duration ranged from 3 weeks to 12 months. Meta-analysis of 13 RCTs showed that internet-based psychoeducational programs had a significant effect on reducing caregivers’ depressive symptoms (SMD −0.19; 95% CI −0.03 − 0.35) and stress (SMD −0.29; 95% CI −0.03 −0.54). However, these programs did not show an effect on quality of life, anxiety, burden or self-efficacy in caregivers.
Conclusion
Internet-based psychoeducational programs can improve some aspects of caregivers’ mental health and emotional wellbeing. The effects of programs on self-efficacy, anxiety, burden and quality of life for caregivers remain inconclusive.
Introduction
Dementia currently affects 55 million people worldwide and this number is projected to reach 152 million by 2050 (World Health Organization, Citation2021). Most people with dementia (PwD) are cared for by family caregivers at home (World Health Organization, Citation2021). It is well-researched that caring for PwD at home is physically stressful for caregivers due to the nature of the disease which requires 24-hour supervision, assistance with activities of daily living and management of a treatment regime for chronic conditions (World Health Organization, Citation2021). Caring for the PwD is also a source of psychological stress for caregivers (World Health Organization, Citation2021). Inability of caregivers to cope with physical and psychological stress contributes to their poor health, wellbeing and quality of life (QoL) (Farina et al., Citation2017). Psychoeducation is a major category of non-pharmacological interventions and is widely used to reduce caregivers’ stress (Frias, Garcia-Pascual, et al., Citation2020). In this review, we describe the definition of psychoeducation as educational programs designed to improve caregivers’ capabilities in providing daily care activities for people with dementia and in coping with stress (Cheng et al., Citation2020). This definition includes psychoeducation-a, or programs without mentioning psychological theories, and psychoeducation-b, or programs with psychotherapeutic components (Cheng et al., Citation2020).
Internet-based psychoeducation has been used increasingly in the past decade due to its flexibility and low costs (Egan et al., Citation2018). The prolonged COVID-19 outbreak has interrupted most face-to-face education programs for caregivers, and internet-based psychoeducation has advantages for overcoming COVID-19 related challenges (World Health Organization, Citation2021). In this review, we considered the definition of internet-based education by Singh and Thurman (Citation2019) and the definition of psychoeducation by Cheng et al. (Citation2020). We describe the Internet-based psychoeducation for caregivers of PwD as an educational program that is (1) designed to improve caregivers’ capabilities in providing daily care activities for PwD and in coping with stress; (2) delivered in an online environment using the Internet; (3) has flexible and accessible online learning activities without physical or virtual location restrictions (or asynchronous programs); and (4) may or may not have facilitators to interact with caregivers. Previous systematic reviews on internet-based interventions for caregivers were not specifically focused on psychoeducation but considered all types of interventions or did not undertake meta-analysis (Egan et al., Citation2018; Hopwood et al., Citation2018; Leng et al., Citation2020; Zhao et al., Citation2019). This systematic review and meta-analysis address this gap in the dementia care literature.
Psychoeducation for dementia caregivers is informed by stress and coping theories (Cheng et al., Citation2020; Frias, Garcia-Pascual, et al., Citation2020). Among various stress and coping theories, we found that the ‘stress and health process’ model described by Conde-Sala et al. (Citation2010) was most relevant to this review as it explains the source of stress, negative impacts on caregivers and interventions (i.e. psychoeducation) that mitigate these negative impacts. This model was a combination of the stress process models introduced by Pearlin et al. (Citation1990) and Schulz et al. (Citation2002) which highlight the intervention effect on stressors (Conde-Sala et al., Citation2010). The ‘stress and health process’ model informed the design of program analysis and understandings about the relationships between sources of stress, effects on caregivers’ health and wellbeing, and chosen outcomes. According to Conde-Sala et al. (Citation2010), variables affecting caregiver health and wellbeing include caregiver contextual factors (i.e. ability to provide dementia care, family relationships, co-residing status, gender and time spent on care activities); care recipient factors or primary stressors (i.e. changed behaviours, dependence and multimorbidity); and other factors or secondary stressors (i.e. family conflict and financial difficulties). Interventions that can improve caregivers’ symptoms of stress, such as anxiety, depression, isolation, burden and physical health, include non-pharmacological interventions (i.e. psychoeducation, social support and social resources) and treatment (i.e. pharmacological treatment)(Conde-Sala et al., Citation2010). Previous systematic reviews on the effectiveness of psychoeducation included all types of program delivery (i.e. face-to-face, telephone and internet-based delivery) (Cheng et al., Citation2020; Frias, Garcia-Pascual, et al., Citation2020). Systematic reviews on internet-based psychoeducation specifically are scarce. The lack of synthesis of research evidence in this increasingly demanding area of caregiver support may affect the development of evidence-based policy and practices.
Previous systematic reviews showed that dementia care education can mitigate caregiver contextual factors by equipping them with capabilities to effectively handle daily care activities and to develop positive thoughts towards dementia care (Jensen et al., Citation2015; Klimova et al., Citation2019). Studies also confirmed that dementia care education improved caregivers’ self-efficacy (Easom et al., Citation2020). Dementia caregivers’ self-efficacy is described as their belief that they can control upsetting thoughts, respond to changed behaviours and obtain respite care (Crellin et al., Citation2014; Steffen et al., Citation2002). Caregivers’ self-efficacy is related to their QoL (Crellin et al., Citation2014; Farina et al., Citation2017). Based on these known relationships between dementia care education and outcomes on caregivers regarding contextual factors, a systematic review and meta-analysis needs to include self-efficacy and QoL of caregivers’ and caregivers’ responses to stressful care situations in the outcome measures.
The most commonly mentioned changed behaviours are apathy, confusion, agitation (i.e. wandering or vocal disruption) and depression (Perera et al., Citation2017; Pond et al., Citation2019). These are often associated with other factors besides physiological changes in the brain such as health and environment factors (i.e. comfort, inclusion, identity, attachment and occupation) (Cunningham et al., Citation2019; T. Kitwood, Citation1998; T. M. Kitwood & Kitwood, Citation1997). Although there is no consensus regarding the preferred terminology to describe this group of symptoms, there is general agreement that the language used needs to be dementia friendly (Wolverson et al., Citation2021). Therefore, consistent with view of the World Health Organization, we prefer to use the term ‘changed behaviours’ instead of medical terminology such as psychological and behavioural symptoms of dementia (BPSD) or neuropsychiatric symptoms in PwD (Burley et al., Citation2021; Wolverson et al., Citation2021).
In the ‘stress and health process’ model, changed behaviours are main primary stressors that contribute to caregiver stress and burden (Conde-Sala et al., Citation2010). Stress is described as the caregivers’ emotional reactions to challenging situations beyond their abilities and resources to cope (Conde-Sala et al., Citation2010), while burden is described as a subjective feeling of negative impact on caregivers’ functioning (Williams et al., Citation2019). Caregiver burden can be conceptualised into objective burden (i.e. physical task due to the dependence of the PwD and the level of changed behaviours) and subjective burden (i.e. emotional distress due to caregivers’ negative reactions to these behaviours) (Feast et al., Citation2016; Poon, Citation2019). Changed behaviours in PwD cause increased objective burden, and impact on family relationships and contributed to caregiver subjective burden (Conde-Sala et al., Citation2010; Williams et al., Citation2019). Up to 88% of PwD in community care settings showed changed behaviours (Poon, Citation2019). Yet, most caregivers showed limited knowledge about how to prevent and manage changed behaviours (Chiu et al., Citation2015). The relationship between primary stressors and caregivers’ health and wellbeing indicates that the changed behaviours in PwD and caregivers’ stress and burden need to be measured in a systematic review and meta-analysis.
Research shows that other primary stressors, such as PwD’s physical and cognitive function decline, were directly associated with increased caregiver burden and the latter was associated with caregivers’ anxiety and depressive symptoms (Armstrong et al., Citation2019; Morlett Paredes et al., Citation2017). Furthermore, other factors, such as social support, economic living standards, dyadic relationship factors and length of caring experience, also significantly correlated with carers’ anxiety and depressive symptoms (Fekete et al., Citation2019; Watson et al., Citation2019). In other words, greater caregiver burden was associated with caregivers’ psychological well-being measured as anxiety and depression.
Caregiver burden, carers’ psychological well-being and carer’s self-efficacy are all interrelated and directly linked to carers and care recipients’ QoL (Farina et al., Citation2017; Holopainen et al., Citation2019). Caregivers with high self-efficacy is related to their beliefs that they have mastered certain skills to deal with challenges (Bandura, Citation1993; Steffen et al., Citation2002). WHO defines QoL as an individual’s perception of their life expectations in the context of their culture and value systems (World Health Organization, Citation2020). Research shows caregivers of PwD reported worse health related QoL compared to non-PwD carers (Karg et al., Citation2018; Lippe et al., Citation2021). Caregivers self-perceived QoL is also linked to primary stressors such as the severity of PwD’s condition, level of changed behaviours and other factors for example, level of social support caregivers received (Frias, Cabrera, et al., Citation2020; Pessotti et al., Citation2018).
Informed by the ‘stress and health process’ model described by Conde-Sala et al. (Citation2010), the outcome measures for caregivers’ psychological wellbeing in this review focused on anxiety, depression and caregivers’ burden. In line with a previous systematic review, other outcome measures for QoL and self-efficacy were included as they directly or in-directly affect caregiver’s health and well-being (Crellin et al., Citation2014). The review questions were: (1) what are the characteristics of internet-based psychoeducational programs for caregivers of PwD living at home? and (2) What is the effectiveness of internet-based psychoeducational programs for informal caregivers of PwD living at home?
Methods
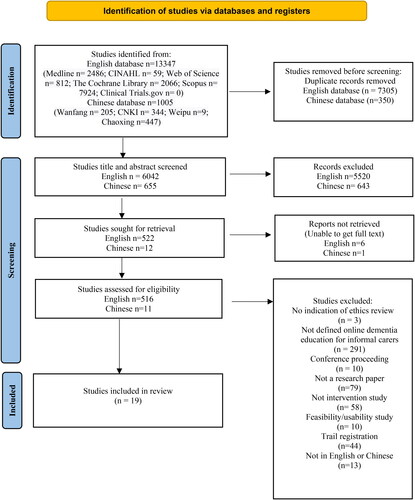
This review followed the Cochrane Handbook for systematic review of interventions (Higgins et al., Citation2021) and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al., Citation2021). The review protocol was registered with PROSPERO (registration number CRD42021257562).
Search strategies
The following English databases were searched: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, Medical Literature Analysis and Retrieval System Online (Medline), the Cochrane Library and Scopus. The following Chinese databases were also searched: China National Knowledge Infrastructure (CNKI), Wang Fang Data, Weipu Data and Chao Xing Data. The search strategies are presented in Supplementary material Appendix A. The search strategy was developed in line with the PICO framework, with no time limit applied. All key words were identified around online psychoeducation for informal caregivers of PwD and a Boolean search was conducted by combining the key words (Supplementary material Appendix B). A librarian was consulted for the database search.
Inclusion and exclusion criteria
All interventional studies reflecting our operational definition of online psychoeducational programs for informal caregivers of PwD were included. Face-to-face or telephone delivered dementia education programs using digital video discs (DVD) or booklets were excluded. Synchronised online education, which mimics the physical classroom or DVD programs delivered through the Internet, were also excluded as this type of program showed little flexibility in program delivery and were often restrained by time and space. Studies were excluded if they were not reported in English or Chinese. The inclusion and exclusion criteria are presented in Supplementary material Appendix C.
Data collection process
All searched records were imported to Endnote 20 and Covidence, with duplicates removed (The EndNote Team, Citation2013; Veritas Health Innovation, Citation2021). Four reviewers (YY, LX, CM, SU) screened English titles and abstracts to identify whether a study met the inclusion criteria. Two reviewers (JW, JH) screened Chinese language titles and abstracts. After title and abstract screening, the reference list of each selected article was manually scanned. Full text papers were uploaded to Covidence to determine further eligibility by all reviewers (YY, LX, CM, SU screened English language articles and YY, LX, JW screened Chinese language articles). All reviewers met regularly to discuss and resolve any disagreements.
Assessment of risk of bias
Risk of bias in the selected articles was assessed by two reviewers (YY, LX) according to the criteria recommended by the Cochrane Handbook (Higgins et al., Citation2021). Randomised Control Trials (RCTs) were assessed according to the Cochrane risk-of-bias tool (RoB2) (Higgins et al., Citation2021). This tool assesses bias arising from: (1) the randomisation process; (2) intervention deviation; (3) missing outcome data; (4) measurement of outcomes; and (5) selection of results. Each of these domains is ranked for risk of bias as ‘low’, ‘some concern’ or ‘high’, with an overall assessment of study quality compiled.
Non-randomised studies were assessed according to ROBINS-I tool (Sterne et al., Citation2021). This tool assesses confounding, selection, information and reporting biases. The ROBINS-I tool provides a domain-level risk-of-bias judgement of ‘low’, ‘moderate’, ‘serious’ or ‘critical’, with an additional option for ‘no information’. Two reviewers undertook an independent quality appraisal of the selected studies, with any disagreement resolved through consensus.
Data extraction
A standardised Cochrane data extraction sheet was used to extract the following data: (1) author, publication, year and country; (2) participants’ characteristics and sample size; (3) online psychoeducation or training details; 4) study setting, design and methods; (5) data collection time points, measurement tools and outcomes; and (6) main findings.
Data synthesis and analysis
Characteristics of online psychoeducation components, outcomes of RCTs not suitable for meta-analysis and outcomes of non-RCTs were presented as a descriptive summary. Where appropriate, meta-analysis of results from included RCTs was undertaken using Review Manager 5.4.1 (RevMan) to estimate the effect of the program on care outcomes (The Cochrane Collaboration, Citation2014). The meta-analysis was also run through ‘meta’ package in R program by a second reviewer to ensure the robustness of results (Balduzzi et al., Citation2019). Authors of included RCTs were contacted to request original data when reported data was not suitable for meta-analysis. Heterogeneity, including samples and settings, and methodological heterogeneity was analysed prior to performing meta-analysis. Standardised mean differences (SMD) with a 95% confidence interval (CI) were calculated for continuous data. The statistical heterogeneity between studies was examined using I2 statistics. The results of included studies were pooled, and a random-effects model applied for studies that showed heterogeneity. Sub-group analysis was planned for studies that could be grouped into the following: programs with peer support, programs with a facilitator, or program duration of three months or six months. However, these subgroup analyses were not performed due to insufficient data in the results.
Assessment of publication bias
We planned to test funnel plot asymmetry for publication bias, but this was not achievable due to the small number of RCTs identified.
Assessment of evidence quality
The overall quality of evidence for each outcome was rated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE, see Supplementary material Appendix D) (McMaster University and Evidence Prime, Citation2021).The GRADE system rates evidence at four levels: high quality, moderate quality, low quality and very low quality based on study limitations, result inconsistencies, indirectness, imprecision and reporting bias (Guyatt et al., Citation2008).
Results
Search process
A total of 14352 articles were identified (English language databases n = 13347; Chinese language databases n = 1005). Covidence automatically removed duplicates (n = 7655). A total of 527 (English language n = 516, Chinese language n = 11) full text articles were retrieved after title and abstract screening (English language n = 6042, Chinese language n = 655). After assessing the eligibility of full text articles, 19 studies written in English were included in this review. The study selection process is displayed in .
Risk of bias
All selected RCTs were assessed based on intention-to-treat effect and the assessment is displayed in Supplementary material. Five out of 13 RCTs did not provide details of the randomisation process, and thus there is uncertainty about the allocation sequence and allocation concealment (Brennan et al., Citation1995; Gustafson et al., Citation2019; Hicken et al., Citation2017; Kajiyama et al., Citation2013; Torkamani et al., Citation2014). All 13 RCTs had no significant baseline differences between intervention and control groups. Of the 13 RCTs, 10 interventions were not blinded to participants (Baruah et al., Citation2021; Boots et al., Citation2018; Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Hattink et al., Citation2015; Hicken et al., Citation2017; Kajiyama et al., Citation2013; Metcalfe et al., Citation2019; Nunez-Naveira et al., Citation2016; Torkamani et al., Citation2014), while three RCTs were not blinded to researchers (Cristancho-Lacroix et al., Citation2015; Duggleby et al., Citation2018; Torkamani et al., Citation2014). All selected studies had a pre-formulated study protocol either through trial registration (Baruah et al., Citation2021; Blom et al., Citation2015; Boots et al., Citation2018; Cristancho-Lacroix et al., Citation2015; Hattink et al., Citation2015; Kajiyama et al., Citation2013; Metcalfe et al., Citation2019) or ethics approval (Brennan et al., Citation1995; Duggleby et al., Citation2018; Gustafson et al., Citation2019; Hicken et al., Citation2017; Nunez-Naveira et al., Citation2016; Torkamani et al., Citation2014). The overall risk of bias assessment showed four RCTs to have some concerns (Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Gustafson et al., Citation2019; Hicken et al., Citation2017), while all other RCTs were considered to have low risk of bias. All non-RCT studies were assessed as low risk of bias (see Supplementary Material). Of 19 studies, 18 were funded through government grants.
Characteristics of selected studies
No studies reported in the Chinese language met the selection criteria. Among the 19 selected studies, 13 were RCTs and six had a pre- and post- intervention design. Studies were conducted in the United States (n = 6), the Netherlands (n = 4), Canada (n = 2), France (n = 1), India (n = 1) and Iran (n = 1). Four studies were collaborations between European countries (Denmark, Poland and Spain n = 1; United Kingdom (UK), Spain and Greece n = 1, France and Germany n = 1 and UK and the Netherlands n = 1). Selected studies are presented in .
Table 1. Characteristics of selected studies.
All studies included participants who were informal caregivers of PwD. The average age of informal caregivers was between 50 and 70 years old. Most informal caregivers were female, with only two studies reporting a greater proportion of males to females (Baruah et al., Citation2021; Wijma et al., Citation2018). The relationship between informal caregivers and care recipients varied from spouse, parents/children, sibling to friends.
Characteristics of internet-based psychoeducational programs
Among the 19 internet-based psychoeducational programs included in the review, six fully or partially utilised a theoretical framework to develop content (Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Duggleby et al., Citation2018; Hattink et al., Citation2015; Pleasant et al., Citation2017) (see ). ComputerLink (USA), reported in 1995, was the earliest identified internet-based psychoeducation program for informal caregivers (Brennan et al., Citation1995). Of the 19 studies we reviewed, three are psychoeducation-a programs which had no psychological and behavioural training (Brennan et al., Citation1995; Hicken et al., Citation2017; Torkamani et al., Citation2014). The other 16 psychoeducational programs remain relatively similar with all setting out to cover theoretical, psychological and behavioural training relevant to dementia care with unlimited access to the website or information, and variable duration of 3 weeks to 12 months. Basic text-based internet functions such as information, discussion boards and email functions were used ubiquitously across all studies.
Table 2. Content of psychoeducational programs and relations to the ‘stress and health process’ (SHP) model.
All programs had self-directed learning components, with eight programs using only basic functions (e.g. text-based information) (Baruah et al., Citation2021; Boots et al., Citation2018; Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Duggleby et al., Citation2018; Marziali & Garcia, Citation2011; van der Roest et al., Citation2010), and ten programs adding more complex components such as videos (Blom et al., Citation2015; Gaugler et al., Citation2015; Gustafson et al., Citation2019; Hattink et al., Citation2015; Hicken et al., Citation2017; Kajiyama et al., Citation2013; Metcalfe et al., Citation2019; Nunez-Naveira et al., Citation2016; Pleasant et al., Citation2017; Torkamani et al., Citation2014). A more recent program utilised virtual reality (n = 1) in addition to a website (Wijma et al., Citation2018). One program was delivered entirely through a telegram chat group by posting text based messages (Mollaei et al., Citation2021).
Some programs (n = 9) had functionality to facilitate interactive learning between caregivers and facilitators, and caregiver to caregiver (peer support). Interactive learning was incorporated in seven programs (e.g. iSupport program incorporated the interactive function of immediate feedback) (Baruah et al., Citation2021), while others offered recommendations to assist in service-related decision making (e.g. ComputerLink, Dementia–Comprehensive Health Enhancement Support System [D-CHESS), STAR training portal and DEMentia-specific Digital Interactive Social Chart [DEM-DISC)) (Brennan et al., Citation1995; Gustafson et al., Citation2019; Hattink et al., Citation2015; van der Roest et al., Citation2010). Two programs offered an opportunity for reflection through the ‘homework’ function on the website (Kajiyama et al., Citation2013; Nunez-Naveira et al., Citation2016). An interaction function via a health questionnaire facilitated the detection and monitoring of health changes in informal caregivers and their care recipients (Torkamani et al., Citation2014).
Furthermore, seven programs offered interactions with facilitators or health professionals (Blom et al., Citation2015; Boots et al., Citation2018; Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Gustafson et al., Citation2019; Hicken et al., Citation2017; Mollaei et al., Citation2021) via the application (Blom et al., Citation2015), email (Boots et al., Citation2018), messaging (Gustafson et al., Citation2019), telephone (Hicken et al., Citation2017) or telegram group chat (Mollaei et al., Citation2021) utilising variations of two-way contact to provide information, guide discussions, provide feedback or deliver education content. Other programs were facilitated through passive techniques only, such as monitoring or moderating discussion forums (Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015), or only answering questions if asked (Gustafson et al., Citation2019).
Peer support was facilitated in eight programs. While one program did not explain the type of social network used to support peer interaction (Nunez-Naveira et al., Citation2016), all other programs facilitated peer support through videoconferencing (n = 1) (Marziali & Garcia, Citation2011) or discussion forums (n = 5) (Boots et al., Citation2018; Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Marziali & Garcia, Citation2011; Torkamani et al., Citation2014). Private email was used in two programs to enable informal caregivers to contact each other (Brennan et al., Citation1995; Marziali & Garcia, Citation2011). The arrival of social media has changed people’s communication and interactions significantly, yet only two programs utilised social networks, such as Facebook and LinkedIn, in addition to discussion forums to facilitate peer support (Hattink et al., Citation2015; Torkamani et al., Citation2014). One study reported using a telegram chat group for peer support meetings (Mollaei et al., Citation2021).
Characteristics of comparison groups
Various comparisons were used in the 13 RCTs as detailed in the following. Five studies reported usual care as the comparison group (Cristancho-Lacroix et al., Citation2015; Hattink et al., Citation2015; Metcalfe et al., Citation2019; Nunez-Naveira et al., Citation2016; Torkamani et al., Citation2014). Two studies reported usual care plus additional support (i.e. non-frequent counselling or local service training) as the comparison group (Boots et al., Citation2018; Brennan et al., Citation1995). Alternative educational information was provided to the comparison group in four studies through a booklet (Baruah et al., Citation2021; Duggleby et al., Citation2018; Gustafson et al., Citation2019; Hicken et al., Citation2017), in one study via a website (Kajiyama et al., Citation2013) and in one study via email bulletins (Blom et al., Citation2015).
Meta-analysis
Caregiver’s QoL
Six RCTs were included in the meta-analysis of the effectiveness of online psychoeducational programs on caregiver’s QoL (Baruah et al., Citation2021; Boots et al., Citation2018; Hattink et al., Citation2015; Kajiyama et al., Citation2013; Metcalfe et al., Citation2019; Torkamani et al., Citation2014). Compared to control groups, internet-based psychoeducational programs had no significant effect on caregiver’s QoL [effect size = 0.18; confidence interval (-0.22, 0.58), p = 0.38] (Supplementary material).
Caregiver’s depressive symptoms
Eight RCTs were included in the meta-analysis of the effectiveness of internet-based psychoeducational programs on caregiver’s depressive symptoms (Baruah et al., Citation2021; Blom et al., Citation2015; Boots et al., Citation2018; Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Gustafson et al., Citation2019; Kajiyama et al., Citation2013; Nunez-Naveira et al., Citation2016). Compared to control groups, internet-based psychoeducational programs had a significant effect on caregiver’s depressive symptoms [effect size =-0.19; confidence interval (- 0.35, −0.03), p = 0.02] (Supplementary material).
Two RCTs had program facilitators and these studies were included in a sub-group analysis (Blom et al., Citation2015; Boots et al., Citation2018). Compared to control groups, internet-based psychoeducational programs with a facilitator had a significant effect on caregiver’s depressive symptoms [effect size = − 0.29; confidence interval (-0.54, − 0.03), p = 0.03] (Supplementary material).
Six RCTs without a facilitator were included in a sub-group analysis (Baruah et al., Citation2021; Brennan et al., Citation1995; Cristancho-Lacroix et al., Citation2015; Gustafson et al., Citation2019; Kajiyama et al., Citation2013; Nunez-Naveira et al., Citation2016). The result revealed that internet-based psychoeducational programs without a facilitator had no effect on caregiver’s depressive symptoms [effect size = − 0.13; confidence interval (-0.33- 0.07), p = 0.21] (Supplementary material).
Caregiver’s stress
Six RCTs were included in the meta-analysis of the effectiveness of internet-based psychoeducational programs on caregiver’s stress (Boots et al., Citation2018; Cristancho-Lacroix et al., Citation2015; Hattink et al., Citation2015; Kajiyama et al., Citation2013; Metcalfe et al., Citation2019; Torkamani et al., Citation2014). Compared to control groups, internet-based psychoeducational programs showed a significant reduction in caregiver’s stress [effect size =- 0.29; confidence interval (-0.52, −0.06), p = 0.01] (Supplementary material).
Caregiver’s self-efficacy
Seven RCTs were included in the meta-analysis of the effectiveness of internet-based psychoeducational programs on caregiver’s self-efficacy (Baruah et al., Citation2021; Boots et al., Citation2018; Cristancho-Lacroix et al., Citation2015; Gustafson et al., Citation2019; Hattink et al., Citation2015; Metcalfe et al., Citation2019; Nunez-Naveira et al., Citation2016). Compared to control groups, internet-based psychoeducational programs had no significant effect on caregiver’s self-efficacy [effect size = 0.10; confidence interval (-0.12, 0.33), p = 0.37] (Supplementary material).
Caregiver’s anxiety
Three RCTs were included in the meta-analysis of the effectiveness of internet-based psychoeducational programs on caregiver’s anxiety (Blom et al., Citation2015; Boots et al., Citation2018; Gustafson et al., Citation2019). Compared to control groups, internet-based psychoeducational programs showed no significant effect on caregiver’s anxiety .effect size =-0.12; confidence interval (-0.76, 0.51), p = 0.71] (Supplementary material).
Caregiver’s burden
Six RCTs were included in meta-analysis of the effectiveness of internet-based psychoeducational programs on caregiver’s burden (Baruah et al., Citation2021; Cristancho-Lacroix et al., Citation2015; Gustafson et al., Citation2019; Hattink et al., Citation2015; Metcalfe et al., Citation2019; Torkamani et al., Citation2014). Compared to control groups, internet-based psychoeducational programs showed no significant effect on caregiver burden .effect size =-0.03; confidence interval (-0.26, 0.20), p = 0.82] (Supplementary material). A summary of meta-analysis findings is provided in Supplementary material Appendix E.
Description of studies not included in meta-analysis
Two RCTs did not have sufficient available data to be included in the meta-analysis despite us contacting authors (Duggleby et al., Citation2018; Hicken et al., Citation2017). Data from six pre-and post-test studies were not suitable for inclusion in the meta-analysis, but study results showed these programs to significantly improve participants’ mental health (Marziali & Garcia, Citation2011), well-being (Mollaei et al., Citation2021), knowledge of dementia (Gaugler et al., Citation2015; Pleasant et al., Citation2017) and competence (Pleasant et al., Citation2017; van der Roest et al., Citation2010; Wijma et al., Citation2018). Within these studies, there was no change in caregiver burden, QoL or self-efficacy (Duggleby et al., Citation2018; Hicken et al., Citation2017; van der Roest et al., Citation2010).
Discussion
Our meta-analyses showed internet-based psychoeducation programs have a significant effect on caregiver’s depressive symptoms and stress, but have no statistically significant effect on caregivers’ QoL, burden and self-efficacy. We developed a clear definition of internet-based psychoeducational programs and used it in the selection of studies which allows future studies or reviews to compare the outcomes. Furthermore, the use of the ‘stress and health process’ model informed program analysis and outcome measures of internet-based psychoeducation interventions (Conde-Sala et al., Citation2010). These measures were based on the theoretical assumption that psychoeducation programs address multifaceted factors including caregiver contextual factors (caregiver factors), primary stressors (care recipient factors) and secondary stressors (other factors) by which they have a positive effect on the health, wellbeing and QoL of caregivers (Conde-Sala et al., Citation2010). Previous systematic reviews on the impact of psychoeducation interventions rarely detailed relations between the program content and the multifaced factors the content addressed (Egan et al., Citation2018; Gonzalez-Fraile et al., Citation2021).
We carefully analysed the content of each psychoeducation program included in the review and clarified the relations between the program content and the aforementioned multifaced factors (see ). Program content that addressed caregiver factors included positive thoughts towards the relationship with PwD due to dementia (Blom et al., Citation2015; Boots et al., Citation2018); and how to be a caregiver (either as an adult-child caregiver or a spouse caregiver) (Baruah et al., Citation2021). Moreover, content that helped caregivers to cope with care recipient factors comprised how to prevent and manage changed behaviours (Hattink et al., Citation2015; Metcalfe et al., Citation2019), and how to provide activities of daily living to address the functional deficits of PwD (Cristancho-Lacroix et al., Citation2015; Nunez-Naveira et al., Citation2016). In addition, content that enabled caregivers to deal with other factors included how to seek help within and outside the family (i.e. peer support and support from facilitators (Gustafson et al., Citation2019; Kajiyama et al., Citation2013). This theory-informed analysis may enhance confidence for stakeholders to translate findings into practice.
Our meta-analyses showed that internet-based psychoeducational programs had a significant effect on the reduction of depressive symptoms. The depression reduction identified in our review showed the same effect size (-0.19) to psychoeducation-a programs, but a smaller effect size compared to psychoeducation-b programs (effect size=- 0.37), as that reported by Cheng et al. (Citation2020) in their review. It should be noted that of the eight studies included in our meta-analysis of depressive symptoms, only one study was a psychoeducation-a program according to the definition by Cheng et al. (Citation2020). Therefore, our result may indicate that internet-based psychoeducation programs are less effective in depression reduction compared to psychoeducation-b programs (Cheng et al. Citation2020). It also should be mentioned that the systematic review and meta-analysis by Cheng et al. (Citation2020) included an additional 46 psychoeducation programs excluded from our review according to our definition of psychoeducation programs. Excluded programs had a broader range of program delivery methods than our focus here such as face-to-face and telephone-based programs and other information technology formats (i.e. video conferencing, web platforms or DVD based self-learning programs) and may or may not have facilitators (Cheng et al., Citation2020). Therefore, reported differences in effectiveness of psychoeducation programs between our review and the review by Cheng et al. (Citation2020) may be due to program delivery methods. Future studies need to explore the impact of program delivery on the program effectiveness.
Our sub-group analysis indicated that programs with a facilitator had a significant effect on reducing depressive symptoms (Figure 3.3), while programs without a facilitator showed no significant effect (Figure 3.4). Of the 19 programs reviewed, nine had program facilitators, and two of these studies were included in this sub-analysis. The role of facilitators in these two programs were similar and included a trained psychologist who provided feedback to caregivers (Blom et al., Citation2015; Boots et al., Citation2018). Our review supports a previous review that increased professional support in a dementia care education program were associated with a better effect on caregiver depressive symptoms (Zhao et al., Citation2019). The mechanism underlying the better effect might be due to the facilitator’s role as a mediator to address caregiver contextual factors and care recipients’ factors (Huang, Citation2022). However, as we only included two studies in the meta-analysis, the result needs to be interpreted with caution and future studies need to further explore the relationships.
Our meta-analysis also revealed that internet-based psychoeducational programs had a significant effect on improving caregivers’ emotional wellbeing as evidenced by stress reduction. The effect size of internet-based psychoeducational programs (-0.29 on stress) is similar to that reported by Cheng et al. (Citation2020) (effect size=-0.23 on stress and burden). This is evidence that internet-based psychoeducational programs show similar reduction of stress compared to psychoeducation programs delivered by various other methods as aforementioned.
Our findings suggested that internet-based psychoeducation programs did not have a significant effect on reducing anxiety symptoms. This may be due to the risk factors underlying anxiety differing from depression. Watson et al. (Citation2019) suggested that anxiety symptoms were associated with female gender, spousal caregivers, care recipients’ condition, low levels of self-efficacy and other existing underlying anxiety problems. In our systematic review, the majority of participants in the three studies that measured anxiety included in the meta-analysis were female spouse carers living with PwD in the same household. These characteristics are related to caregiver contextual factors based on the ‘stress and health process’ model (Conde-Sala et al., Citation2010). Addressing these factors may require instrumental support such as social care services (i.e. respite care and home care services for PwD) (Brodaty & Donkin, Citation2009). Our review suggested that an internet-based psychoeducation program alone may not be sufficient to achieve anxiety reduction. Future studies need to explore interventions that include multiple approaches such as emotional and instrumental support, counselling and peer support groups for reducing anxiety among caregivers.
The present review suggests that online psychoeducation programs have no statistically significant effect on caregiver burden. Research showed that caregiver burden were associated with PwD’s high level of dependence (primary stressors) and less social support for caregivers (Connors et al., Citation2020). In this review, we were unable to clarify the correlation between caregiver burden and primary stressors and between caregiver burden and social support they received due to limited data available. However, a systematic review and meta-analysis by Williams et al. (Citation2019) revealed that only multiple approaches, for example respite care, home care for PwD, peer support groups and psychoeducation, showed significant burden reduction.
Our review showed that internet-based psychoeducational programs did not have a significant effect on caregiver self-efficacy. Our finding differs from a systematic review that showed a significant effect on self-efficacy in group-based face-to-face psychoeducational programs (Frias, Garcia-Pascual, et al., Citation2020). The differences may be due to the learning environment for caregivers. In group-based face-to-face programs, caregivers had opportunities to interact with peers to share experiences in dementia care, learn from and be motivated by role models, gain emotional and social support, and gain information to cope with challenges (Frias, Garcia-Pascual, et al., Citation2020). This environment reflects Bandura’s self-efficacy development theory that emphasises a person’s ability to learn a particular task and the environmental factors which influence the learner through cognitive, motivational, affective and behavioural processes (Bandura, Citation1993).
Our review also revealed that internet-based psychoeducational programs did not have a statistically significant effect on QoL. The finding is in line with a systematic review by Frias, Garcia-Pascual, et al. (Citation2020) who reported that technology-based intervention (i.e. Website and telephone assisted interventions) had no significant effect on QoL. However, findings from Frias, Garcia-Pascual, et al. (Citation2020) were based on narrative summary, rather than a meta-analysis and our review did not include telephone assisted interventions. Moreover, Frias, Garcia-Pascual, et al. (Citation2020) stated that face-to-face group interventions showed significant improvement on QoL. This result may be due to multiple approaches to interventions being included in group-based face-to-face psychoeducational programs than internet-based programs; for example, offering additional individualised supports such as providing resources, information, follow-up phone calls and help with navigating the health and social care system (Frias, Garcia-Pascual, et al., Citation2020). However, among six studies that measured QoL in our review, five programs were self-directed learning which means no additional support to caregivers in the Internet-based psychoeducation programs (Baruah et al., Citation2021; Hattink et al., Citation2015; Kajiyama et al., Citation2013; Metcalfe et al., Citation2019; Torkamani et al., Citation2014). Moreover, the comparison groups in the six studies on QoL in our review received usual care (n = 3) (Hattink et al., Citation2015; Metcalfe et al., Citation2019; Torkamani et al., Citation2014), additional information support (n = 2) (Baruah et al., Citation2021; Kajiyama et al., Citation2013) and infrequent counselling (Boots et al., Citation2018), which were similar to the comparison groups in the review of face-to-face programs (n = 5) by Frias, Garcia-Pascual, et al. (Citation2020) which included usual care (n = 4) and additional information support (n = 1). Therefore, the differences on QoL might not be associate with the comparison groups, but the multiple approaches to interventions used in the face-to-face programs aforementioned. Future interventional programs need to consider multiple approaches to interventions in order to improve QoL for caregivers.
Crellin et al. (Citation2014) in their systematic review identified that dementia caregiving related self-efficacy was a main factor contributing to caregivers’ QoL. In addition, Farina et al. (Citation2017) in their systematic review confirmed at least 10 factors associated with caregivers’ QoL, for example care recipient factors, didactic relationship factors, caregivers’ self-efficacy, health and emotional wellbeing, and support received. These findings suggest that future internet-based psychoeducational programs should be designed to target as many QoL factors as possible to achieve a positive effect for caregivers.
Strengths and limitations
This review had several strengths. First, the literature search covered both English and Chinese language databases which reduced bias. Second, we performed a meta-analysis to calculate the effect size of changed mean score which is crucial for comparisons between internet-based and the non-internet-based psychoeducational programs. In addition, we included pre- and post-test studies in addition to RCTs to analyse the educational designs. There were also several limitations of this review. First, while this review searched English and Chinese language literature, it could have expanded to other languages if other multilingual researchers were included in the study team. Second, variations in program design, intervention duration, dose and socio-cultural contexts prevented us from undertaking sub-group analysis to calculate precise intervention effect size.
Conclusion
Internet-based psychoeducation programs showed increased importance during the covid-19 pandemic due to restrictions on social contacts and the interruption of face-to-face education programs for caregivers. Our review indicated that internet-based psychoeducational programs show a significant effect on depressive symptoms and stress reduction. However, our findings also indicate that internet-based psychoeducational programs have no effect on reducing anxiety, burden, and improving self-efficacy or QoL for caregivers. Future studies need to explore how to improve internet-based psychoeducational programs to maximise effectiveness and the impact of program facilitators on the health and wellbeing of caregivers.
Authorship statement
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors and all authors agree with the manuscript.
Supplemental Material
Download MS Word (38.5 KB)Supplemental Material
Download MS Word (1.2 MB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Armstrong, N. M., Gitlin, L. N., Parisi, J. M., Roth, D. L., & Gross, A. L. (2019). Association of physical functioning of persons with dementia with caregiver burden and depression in dementia caregivers: An integrative data analysis. Aging & Mental Health, 23(5), 587–594. https://doi.org/10.1080/13607863.2018.1441263
- Balduzzi, S., Rücker, G., & Schwarzer, G. (2019). How to perform a meta-analysis with R: A practical tutorial. Evidence-Based Mental Health, 22(4), 153–160. https://doi.org/10.1136/ebmental-2019-300117
- Bandura, A. (1993). Perceived self-efficacy in cognitive development and functioning. Educational Psychologist, 28(2), 117–148. https://doi.org/10.1207/s15326985ep2802_3
- Baruah, U., Varghese, M., Loganathan, S., Mehta, K. M., Gallagher-Thompson, D., Zandi, D., Dua, T., & Pot, A. M. (2021). Feasibility and preliminary effectiveness of an online training and support program for caregivers of people with dementia in India: A randomized controlled trial. International Journal of Geriatric Psychiatry, 36(4), 606–617. https://doi.org/10.1002/gps.5502
- Blom, M. M., Zarit, S. H., Groot Zwaaftink, R. B., Cuijpers, P., & Pot, A. M. (2015). Effectiveness of an Internet intervention for family caregivers of people with dementia: Results of a randomized controlled trial. Plos One, 10(2), e0116622. https://doi.org/10.1371/journal.pone.0116622
- Boots, L. M., de Vugt, M. E., Kempen, G. I., & Verhey, F. R. (2018). Effectiveness of a blended care self-management program for caregivers of people with early-stage dementia (partner in balance): Randomized controlled trial. Journal of Medical Internet Research, 20(7), e10017. https://doi.org/10.2196/10017
- Brennan, P. F., Shirley, M. M., & Kathleen, A. S. (1995). The effects of a special computer network on caregivers of persons with Alzheimer’s disease. Nursing Research (New York), 44(3), 166–172.
- Brodaty, H., & Donkin, M. (2009). Family caregivers of people with dementia. Dialogues in Clinical Neuroscience, 11(2), 217–228.
- Burley, C. V., Chenoweth, L., Casey, A. N. S., & Brodaty, H. (2021). Changed behaviours associated with cognitive decline: Views of people living with dementia, families and healthcare professionals. Alzheimer’s & Dementia, 17(S8), e051963. https://doi.org/10.1002/alz.051963
- Cheng, S.-T., Li, K.-K., Losada, A., Zhang, F., Au, A., Thompson, L. W., & Gallagher-Thompson, D. (2020). The effectiveness of nonpharmacological interventions for informal dementia caregivers: An updated systematic review and meta-analysis. Psychology and Aging, 35(1), 55–77. https://doi.org/10.1037/pag0000401
- Chiu, M., Pauley, T., Wesson, V., Pushpakumar, D., & Sadavoy, J. (2015). Evaluation of a problem-solving (PS) techniques-based intervention for informal carers of patients with dementia receiving in-home care. International Psychogeriatrics, 27(6), 937–948. https://doi.org/10.1017/S1041610214002798
- Conde-Sala, J. L., Garre-Olmo, J., Turro-Garriga, O., Vilalta-Franch, J., & Lopez-Pousa, S. (2010). Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer’s disease: An exploratory comparative design. International Journal of Nursing Studies, 47(10), 1262–1273. https://doi.org/10.1016/j.ijnurstu.2010.03.001
- Connors, M. H., Seeher, K., Teixeira-Pinto, A., Woodward, M., Ames, D., & Brodaty, H. (2020). Dementia and caregiver burden: A three-year longitudinal study. International Journal of Geriatric Psychiatry, 35(2), 250–258. https://doi.org/10.1002/gps.5244
- Crellin, N. E., Orrell, M., McDermott, O., & Charlesworth, G. (2014). Self-efficacy and health-related quality of life in family carers of people with dementia: A systematic review. Aging & Mental Health, 18(8), 954–969. https://doi.org/10.1080/13607863.2014.915921
- Cristancho-Lacroix, V., Wrobel, J., Cantegreil-Kallen, I., Dub, T., Rouquette, A., & Rigaud, A. S. (2015). A web-based psychoeducational program for informal caregivers of patients with Alzheimer’s disease: A pilot randomized controlled trial. Journal of Medical Internet Research, 17(5), e117. https://doi.org/10.2196/jmir.3717
- Cunningham, C., Macfarlane, S., & Brodaty, H. (2019). Language paradigms when behaviour changes with dementia: #BanBPSD. International Journal of Geriatric Psychiatry, 34(8), 1109–1113. https://doi.org/10.1002/gps.5122
- Dröes, R.-M., van der Roest, H. G., van Mierlo, L., & Meiland, F. J. M. (2011). Memory problems in dementia: Adaptation and coping strategies and psychosocial treatments. Expert Review of Neurotherapeutics, 11(12), 1769–1782. https://doi.org/10.1586/ern.11.167
- Duggleby, W., Ploeg, J., McAiney, C., Peacock, S., Fisher, K., Ghosh, S., Markle-Reid, M., Swindle, J., Williams, A., Triscott, J. A., Forbes, D., & Jovel Ruiz, K. (2018). Web-based intervention for family carers of persons with dementia and multiple chronic conditions (My Tools 4 Care): Pragmatic randomized controlled trial. Journal of Medical Internet Research, 20(6), e10484. https://doi.org/10.2196/10484
- Dumont, C., Barvaux, V., & Cornil, C. (2016). Psycho-educational approach in Alzheimer’s disease. Journal of Alzheimer’s Disease and Parkinsonism, 6(5), 2161–0460. https://doi.org/10.4172/2161-0460.1000261
- Easom, L., Wang, K., & Alston, G. (2020). Increasing self-efficacy and knowledge in carer training: Hispanic versus Caucasian. Nursing Open, 7(1), 180–185. https://doi.org/10.1002/nop2.376
- Egan, K. J., Pinto-Bruno, A. C., Bighelli, I., Berg-Weger, M., van Straten, A., Albanese, E., & Pot, A. M. (2018). Online training and support programs designed to improve mental health and reduce burden among caregivers of people with dementia: A systematic review. Journal of the American Medical Directors Association, 19(3), 200–206. https://doi.org/10.1016/j.jamda.2017.10.023
- Farina, N., Page, T. E., Daley, S., Brown, A., Bowling, A., Basset, T., Livingston, G., Knapp, M., Murray, J., & Banerjee, S. (2017). Factors associated with the quality of life of family carers of people with dementia: A systematic review. Alzheimer’s & Dementia, 13(5), 572–581. https://doi.org/10.1016/j.jalz.2016.12.010
- Feast, A., Moniz-Cook, E., Stoner, C., Charlesworth, G., & Orrell, M. (2016). A systematic review of the relationship between behavioral and psychological symptoms (BPSD) and caregiver well-being. International Psychogeriatrics, 28(11), 1761–1774. https://doi.org/10.1017/S1041610216000922
- Fekete, M., Szabo, A., Stephens, C., & Alpass, F. (2019). Older New Zealanders in caregiving roles: Psychological functioning of caregivers of people living with dementia. Dementia, 18(5), 1663–1678. https://doi.org/10.1177/1471301217725897
- Frias, C. E., Cabrera, E., & Zabalegui, A. (2020). Informal caregivers’ roles in dementia: The impact on their quality of life. Life, 10(11), 251. https://doi.org/10.3390/life10110251
- Frias, C. E., Garcia-Pascual, M., Montoro, M., Ribas, N., Risco, E., & Zabalegui, A. (2020). Effectiveness of a psychoeducational intervention for caregivers of people with dementia with regard to burden, anxiety and depression: A systematic review. Journal of Advanced Nursing, 76(3), 787–802. https://doi.org/10.1111/jan.14286
- Gaugler, J. E., Hobday, J. V., Robbins, J. C., & Barclay, M. P. (2015). CARES((R)) dementia care for families: Effects of online, psychoeducational training on knowledge of person-centered care and satisfaction. Journal of Gerontological Nursing, 41(10), 18–24. https://doi.org/10.3928/00989134-20150804-61
- Gonzalez-Fraile, E., Ballesteros, J., Rueda, J. R., Santos-Zorrozua, B., Sola, I., & McCleery, J. (2021). Remotely delivered information, training and support for informal caregivers of people with dementia. Cochrane Database of Systematic Reviews, 1, CD006440. https://doi.org/10.1002/14651858.CD006440.pub3
- Gustafson, D. H., Cody, O. J., Chih, M.-Y., Johnston, D. C., & Asthana, S. (2019). Pilot test of a computer-based system to help family caregivers of dementia patients. Journal of Alzheimer’s Disease, 70(2), 541–552. https://doi.org/10.3233/JAD-190052
- Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., & Schünemann, H. J. (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ, 336(7650), 924–926. https://doi.org/10.1136/bmj.39489.470347.AD
- Hattink, B. J. J., Meiland, F. J. M., van der Roest, H. G., Kevern, P., Abiuso, F., Bengtsson, J., Giuliano, A., Duca, A., Sanders, J., Basnett, F., & Nugent, C. (2015). Web-based STAR E-learning course increases empathy and understanding in dementia caregivers: Results from a randomized controlled trial in the Netherlands and the United Kingdom. Journal of Medical Internet Research, 17(10), e241. https://doi.org/10.2196/jmir.4025
- Hicken, B. L., Daniel, C., Luptak, M., Grant, M., Kilian, S., & Rupper, R. W. (2017). Supporting caregivers of rural veterans electronically (SCORE). The Journal of Rural Health, 33(3), 305–313. https://doi.org/10.1111/jrh.12195
- Higgins, J., Savović, J., Page, M. J., Elbers, R. G., & Sterne, J. A. (2021). Chapter 8: Assessing risk of bias in a randomized trial. In J. Higgins, J. Thomas, Jacqueline Chandler, Miranda Cumpston, Tianjing Li, Matthew Page, & Vivian Welch (Eds.), Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021) (pp. 205–228). Cochrane. Retrieved May 27, from www.training.cochrane.org/handbook.
- Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., & Welch, V. (Eds.). (2021). Cochrane handbook for systematic reviews of interventions version 6.2. Cochrane. www.training.cochrane.org/handbook.
- Holopainen, A., Siltanen, H., Pohjanvuori, A., Mäkisalo-Ropponen, M., & Okkonen, E. (2019). Factors associated with the quality of life of people with dementia and with quality of life-improving interventions: Scoping review. Dementia (London), 18(4), 1507–1537. https://doi.org/10.1177/1471301217716725
- Hopwood, J., Walker, N., McDonagh, L., Rait, G., Walters, K., Iliffe, S., Ross, J., & Davies, N. (2018). Internet-based interventions aimed at supporting family caregivers of people with dementia: Systematic review. Journal of Medical Internet Research, .20(6), e216. https://doi.org/10.2196/jmir.9548
- Huang, S.-S. (2022). Depression among caregivers of patients with dementia: Associative factors and management approaches. World Journal of Psychiatry, 12(1), 59–76. https://doi.org/10.5498/wjp.v12.i1.59
- Jensen, M., Agbata, I. N., Canavan, M., & McCarthy, G. (2015). Effectiveness of educational interventions for informal caregivers of individuals with dementia residing in the community: Systematic review and meta-analysis of randomised controlled trials. International Journal of Geriatric Psychiatry, 30(2), 130–143. https://doi.org/10.1002/gps.4208
- Kajiyama, B., Thompson, L. W., Eto-Iwase, T., Yamashita, M., Di Mario, J., Marian Tzuang, Y., & Gallagher-Thompson, D. (2013). Exploring the effectiveness of an internet-based program for reducing caregiver distress using the iCare Stress Management e-Training Program. Aging & Mental Health, 17(5), 544–554. https://doi.org/10.1080/13607863.2013.775641
- Karg, N., Graessel, E., Randzio, O., & Pendergrass, A. (2018). Dementia as a predictor of care-related quality of life in informal caregivers: A cross-sectional study to investigate differences in health-related outcomes between dementia and non-dementia caregivers. BMC Geriatrics, 18(1), 189–189. https://doi.org/10.1186/s12877-018-0885-1
- Kitwood, T. (1998). Toward a theory of dementia care: Ethics and interaction. The Journal of Clinical Ethics, 9(1), 23–34.
- Kitwood, T. M., & Kitwood, T. (1997). Dementia reconsidered: The person comes first (Vol. 20). Open University Press.
- Klimova, B., Valis, M., Kuca, K., & Masopust, J. (2019). E-learning as valuable caregivers’ support for people with dementia - A systematic review. BMC Health Services Research, 19(1), 781. https://doi.org/10.1186/s12913-019-4641-9
- Leng, M., Zhao, Y., Xiao, H., Li, C., & Wang, Z. (2020). Internet-based supportive interventions for family caregivers of people with dementia: Systematic review and meta-analysis. Journal of Medical Internet Research. 22(9), e19468. https://doi.org/10.2196/19468
- Lippe, M., Crowder, A., Carter, P., & Threadgill, A. H. (2021). Variables impacting the quality of life of dementia caregivers: A data visualization analysis. Journal of Nursing Scholarship, 53(6), 772–780. https://doi.org/10.1111/jnu.12718
- Marziali, E., & Garcia, L. J. (2011). Dementia caregivers’ responses to 2 Internet-based intervention programs. American Journal of Alzheimer’s Disease & Other Dementias®, 26(1), 36–43. https://doi.org/10.1177/1533317510387586
- McMaster University and Evidence Prime. (2021). GRADEpro guideline development tool [Software] gradepro.org.
- Metcalfe, A., Jones, B., Mayer, J., Gage, H., Oyebode, J., Boucault, S., Aloui, S., Schwertel, U., Bohm, M., Tezenas Du Montcel, S., Lebbah, S., De Mendonca, A., De Vugt, M., Graff, C., Jansen, S., Hergueta, T., Dubois, B., & Kurz, A. (2019). Online information and support for carers of people with young-onset dementia: A multi-site randomised controlled pilot study. International Journal of Geriatric Psychiatry, 34(10), 1455–1464. https://doi.org/10.1002/gps.5154
- Mollaei, P., Momtaz, Y. A., & Taheri-Tanjani, P. (2021). The effect of cyberspace-based education on the well-being of caregivers of elderly people with dementia. Current Aging Science, 14(2), 105–111. https://doi.org/10.2174/1874609814666210208180051
- Morlett Paredes, A., Perrin, P. B., Peralta, S. V., Stolfi, M. E., Morelli, E., & Arango-Lasprilla, J. C. (2017). Structural equation model linking dementia cognitive functioning, caregiver mental health, burden, and quality of informal care in Argentina. Dementia, 16(6), 766–779. https://doi.org/10.1177/1471301215617080
- Nunez-Naveira, L., Alonso-Bua, B., de Labra, C., Gregersen, R., Maibom, K., Mojs, E., Krawczyk-Wasielewska, A., & Millan-Calenti, J. C. (2016). UnderstAID, an ICT platform to help informal caregivers of people with dementia: A pilot randomized controlled study. BioMed Research International, 2016, 5726465. https://doi.org/10.1155/2016/5726465
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J., M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hrobjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, … V. A., Whiting, Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (Clinical Research ed.), 372, n71. https://doi.org/10.1136/bmj.n71
- Pearlin, L. I., Mullan, J. T., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the stress process: an overview of concepts and their measures. The Gerontologist, 30(5), 583–594. https://doi.org/10.1093/geront/30.5.583
- Perera, N., Javeed, M., Lyketsos, C. G., & Leroi, I. (2017). Neuropsychiatric aspects of dementia. In D. Ames, J. T. O’Brien, & A. Burns (Eds.), Dementia (5th ed. ed., p. 59). Taylor & Francis Group.
- Pessotti, C. F. C., Fonseca, L. C., Tedrus, G. M. d A. S., & Laloni, D. T. (2018). Family caregivers of elderly with dementia: Relationship between religiosity, resilience, quality of life and burden. Dementia & Neuropsychologia, 12(4), 408–414. https://doi.org/10.1590/1980-57642018dn12-040011
- Pleasant, M. L., Molinari, V., Hobday, J. V., Fazio, S., Cullen, N., & Hyer, K. (2017). An evaluation of the CARES(R) Dementia Basics Program among caregivers. International Psychogeriatrics, 29(1), 45–56. https://doi.org/10.1017/S1041610216001526
- Pond, D., Phillips, J., Day, J., & McNeil, K. (2019). Caring for people with dementia experiencing behavioural & psychological symptoms. NHMRC Partnership Centre for Dealing with Cognitive and Related Functional Decline in Older People. https://cdpc.sydney.edu.au/wp-content/uploads/2019/09/BPSD_GPCareGuide_FINAL_24092019.pdf
- Poon, E. (2019). A systematic review and meta-analysis of dyadic psychological interventions for BPSD, quality of life and/or caregiver burden in dementia or MCI. Clinical Gerontologist, 45(4), 777–797. https://doi.org/10.1080/07317115.2019.1694117
- Schulz, R., O’Brien, A., Czaja, S., Ory, M., Norris, R., Martire, L. M., Belle, S. H., Burgio, L., Gitlin, L., Coon, D., Burns, R., Gallagher-Thompson, D., & Stevens, A. (2002). Dementia caregiver intervention research: in search of clinical significance. The Gerontologist, 42(5), 589–602. https://doi.org/10.1093/geront/42.5.589
- Singh, V., & Thurman, A. (2019). How many ways can we define online learning? A systematic literature review of definitions of online learning (1988–2018). American Journal of Distance Education, 33(4), 289–306. https://doi.org/10.1080/08923647.2019.1663082
- Steffen, A. M., McKibbin, C., Zeiss, A. M., Gallagher-Thompson, D., & Bandura, A. (2002). The revised scale for caregiving self-efficacy: Reliability and validity studies. The Journals of Gerontology, 57(1), 74–86. https://doi.org/10.1093/geronb/57.1.P74
- Sterne, J. A., Hernán, M. A., McAleenan, A., Reeves, B. C., & Higgins, J. P. (2021). Chapter 25: Assessing risk of bias in a non-randomized study. In J. Higgins, J. Thomas, Jacqueline Chandler, Miranda Cumpston, Tianjing Li, Matthew Page, & Vivian Welch (Eds.), Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021) (vol. 2021; pp. 621–641). Cochrane. Retrieved May 27, from www.training.cochrane.org/handbook.
- The Cochrane Collaboration. (2014). Review Manager (RevMan) (Version 5.1.4). The Nordic Cochrane Centre, The Cochrane Collaboration.
- The EndNote Team. (2013). EndNote (Version EndNote 20). [64 bit]. Clarivate.
- Torkamani, M., McDonald, L., Saez Aguayo, I., Kanios, C., Katsanou, M. N., Madeley, L., Limousin, P. D., Lees, A. J., Haritou, M., Jahanshahi, M., & Group, A. C. (2014). A randomized controlled pilot study to evaluate a technology platform for the assisted living of people with dementia and their carers. Journal of Alzheimer’s Disease, 41(2), 515–523. https://doi.org/10.3233/JAD-132156
- van der Roest, H. G., Meiland, F. J., Jonker, C., & Droes, R. M. (2010). User evaluation of the DEMentia-specific Digital Interactive Social Chart (DEM-DISC). A pilot study among informal carers on its impact, user friendliness and, usefulness. Aging and Mental Health, 14(4), 461–470. https://doi.org/10.1080/13607860903311741
- Veritas Health Innovation. (2021). Covidence systematic review software. www.covidence.org
- Watson, B., Tatangelo, G., & McCabe, M. (2019). Depression and anxiety among partner and offspring carers of people with dementia: A systematic review. Gerontologist, 59(5), e597–e610. https://doi.org/10.1093/geront/gny049
- Wijma, E. M., Veerbeek, M. A., Prins, M., Pot, A. M., & Willemse, B. M. (2018). A virtual reality intervention to improve the understanding and empathy for people with dementia in informal caregivers: Results of a pilot study. Aging and Mental Health, 22(9), 1115–1123. https://doi.org/10.1080/13607863.2017.1348470
- Williams, F., Moghaddam, N., Ramsden, S., & De Boos, D. (2019). Interventions for reducing levels of burden amongst informal carers of persons with dementia in the community. A systematic review and meta-analysis of randomised controlled trials. Aging and Mental Health, 23(12), 1629–1642. https://doi.org/10.1080/13607863.2018.1515886
- Wolverson, E., Dunn, R., Moniz-Cook, E., Gove, D., & Diaz-Ponce, A. (2021). The language of behaviour changes in dementia: A mixed methods survey exploring the perspectives of people with dementia. Journal of Advanced Nursing, 77(4), 1992–2001. https://doi.org/10.1111/jan.14787
- World Health Organization. (2020). WHOQOL: Measuring quality of life. World health Organization. Retrieved July 27, from https://www.who.int/tools/whoqol/whoqol-bref/docs/default-source/publishing-policies/whoqol-bref/english-australian-whoqol-bref
- World Health Organization. (2021). Global status report on the public health response to dementia. World Health Organization. Retrieved October 27, from https://www.who.int/publications/i/item/9789240033245
- Zhao, Y., Feng, H., Hu, M., Hu, H., Li, H., Ning, H., Chen, H., Liao, L., & Peng, L. (2019). Web-based interventions to improve mental health in home caregivers of people with dementia: Meta-analysis. Journal of Medical Internet Research, 21(5), e13415. https://doi.org/10.2196/13415