Abstract
Objectives
Constant observation is used in hospitals with people with dementia to manage their safety. However, opportunities for proactive care are not consistently recognised or utilised. A systematic review of constant observation was conducted to understand measures of effectiveness and facilitators for person-centred approaches.
Method
Electronic databases were searched between 2010 and 2022. Four reviewers completed screening, quality assessments and data extraction with 20% checked for consistency. Findings were presented through narrative synthesis (PROSPERO registration CRD42020221078).
Findings
Twenty-four studies were included. Non-registered staff without specific training were the main providers of constant observation. Assessments and processes clarifying the level of observation encouraged reviews that linked initiation and discontinuation to a patient’s changing needs. Examples of person-centred care, derived from studies of volunteers or staff employed to provide activities, demonstrated meaningful engagement could reassure a person and improve their mood. Proactive approaches that anticipated distress were thought to reduce behaviours that carried a risk of harm but supporting evidence was lacking.
Conclusion
Non-registered staff are limited by organisational efforts to reduce risk, leading to a focus on containment. Trained staff who are supported during constant observation can connect with patients, provide comfort and potentially reduce behaviours that carry a risk of harm.
Introduction
Patient safety is a major priority for hospitals and their staff. People with dementia who are admitted to hospital are at high risk of falls and delirium and may display other behaviours considered to carry risk of harm (Handley et al., Citation2019; Sinvani et al., Citation2019; White et al., Citation2017). One model of care for supporting people with dementia assessed as being at risk of harm in hospital is constant observation. Constant observation is the close monitoring of one or more patients, ranging from one-to-one supervision, also known as ‘specialling’, to monitoring a small group of patients in one area of the ward, commonly referred to as ‘cohorting’ (Coyle et al., Citation2020; Dewing, Citation2013; Wood et al., Citation2018). The evidence-base for the effectiveness or unintended consequences of constant observation for people with dementia in hospital is limited (Dewing, Citation2013). Recent studies demonstrate a wide variation in practice, with opportunities constant observation offers to get to know the person and provide person-centred care missed (Bail et al., Citation2023; Goldberg et al., Citation2014; Handley et al., Citation2019; Wood et al., Citation2018). Constant observation is resource intensive and its focus on risk management can increase distress because of an emphasis on restricting movement and containing the person with dementia.
Person-centred care requires staff to understand care from the point of view of the person and to support their fundamental psychological needs (comfort, identity, inclusion, attachment, and occupation) (Brooker & Latham, Citation2015; Kitwood, Citation1997). In hospital settings this can be compromised by competing treatment demands and system priorities (Clissett et al., Citation2013). Staff are more likely to engage in person-centred care for people with dementia if it fits with hospital and staff priorities and can be embedded in routine practice (Chenoweth et al., Citation2022; O’Brien et al., Citation2018). Developing evidence-based resources to facilitate a more person-centred approach within constant observation could support best practice and mitigate situations of stress and risk.
Previous research that has looked at the practice of constant observation has mainly focused on its use in mental health settings. Its impact on people with different needs and why they are assessed as being a risk to themselves or others are not widely discussed. Reviews of constant observation with older people in hospitals have found no evidence for how the practice could be adapted and applied with this patient population, noting a lack of agreed standards or guidelines, and detail of its impact on patient outcomes were a concern (Dewing, Citation2013; Wood et al., Citation2018). The aim of this review is to synthesise evidence on constant observation for people with dementia and/or older adults with delirium or cognitive impairment to address the following questions:
How and why is constant observation used to support people with dementia and/or delirium during their hospital admission?
How is effectiveness of constant observation understood and measured?
What is the evidence that constant observation improves outcomes for people with dementia?
What outcomes for staff are achieved/desired through improved constant observation practices?
How is person-centred care applied and supported during constant observation?
Methods
The review was reported in accordance with the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA 2020) (Page et al., Citation2021). The study protocol was registered with PROSPERO (CRD42020221078). Ethical approval was not required for the review.
Search strategy
We searched electronic databases Medline (PubMed), CINHAL, Psychinfo, and The Cochrane Library for English language articles. Building on the work of Dewing (Citation2013), who reported on studies published between 2000 and 2010, search dates were restricted to 2010 onwards. Initial searches took place in July 2021, with surveillance searches continuing to December 2022. Search terms were generated from previous studies (Dewing, Citation2013; Wood et al., Citation2018) describing the population (e.g. ‘dementia’, ‘Alzheimer*’, ‘delirium’, ‘cognitive*’) and model of care (e.g. ‘one to one nurse special*’, ‘one to one care’, ‘special observation’, ‘constant observation’, ‘bay nursing’, ‘specialling’, ‘sitters’).
In addition, we ran key word searches on Google Scholar and forward and backward citation searches of reviews and included papers.
Inclusion criteria
The review explored: measures of effectiveness of constant observation; the purpose of constant observation with people with dementia; factors that support person-centred approaches during constant observation; and outcomes for people with dementia and hospital staff. Therefore, all published research evidence and service evaluations were included. We did not include other forms of grey literature, for example conference abstracts (Scherer & Saldanha, Citation2019).
Studies reporting the use of constant observation or similar monitoring activities that involved staff, volunteers or families providing one-to-one support or support to a small group of patients within a specified area of the ward, such as a bed bay, were eligible for inclusion. Studies that reported constant observation activities with people with dementia, older people with delirium (with or without dementia), and older people with unspecified cognitive impairment were included. Studies with mixed patient populations that included people with dementia, were also included. Excluded studies were those that provided no information about who was observed, those located in care homes, mental health hospitals, high dependency and intensive care units or rehabilitation wards. We excluded studies reporting alternatives to constant observation, such as the use of technological innovations for monitoring patients.
Screening
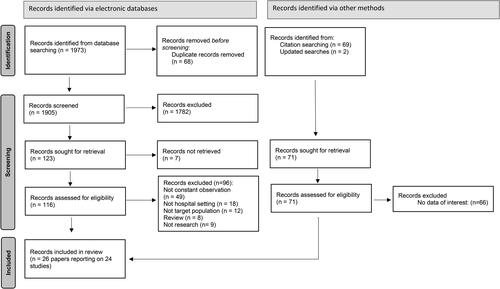
Search results were downloaded into Rayyan (Ouzzani et al., Citation2016) and two reviewers (DT, AY) independently screened all titles and abstracts, with a 20% random selection checked by a third reviewer (MH). Where decisions were unclear or conflicting, papers were taken to full-text review. Full texts were screened by three reviewers (NT, DT, AY) with 20% double screened for consistency. Decisions were recorded using Excel. Disagreements or uncertainty were resolved in discussion with a fourth reviewer (MH). Screening of lateral and surveillance searches were completed by two reviewers (ReH, MH). The selection process is shown in .
Data extraction and quality appraisal
Data were extracted by four reviewers (MH, NT, DT, AY) using a bespoke data extraction form. Data extracted included study characteristics, data collection methods, characteristics of constant observation, comparator details where applicable, participant characteristics, and outcomes related to people with dementia (e.g. falls, patient experience), staff (e.g. knowledge) and processes (e.g. use of person-centred care, feasibility and acceptability). A random sample of 20% was double extracted by two reviewers (DT, AY) to check for consistency in the process. Inconsistencies were discussed with a third reviewer (MH) to reach agreement.
Quality appraisal
The quality of empirical studies was assessed using design appropriate checklists; Mixed Methods Appraisal Tool (MMAT) (Hong et al., Citation2018), Critical Appraisal Skills Programme (CASP) for qualitative (Critical Appraisal Skills Programme, Citation2022b) and cohort studies (Critical Appraisal Skills Programme, Citation2022a). Service evaluations were not assessed. Four reviewers (MH, NT, DT, AY) independently completed quality appraisal checklists, including strengths and weaknesses of studies. A random sample of 20% were double rated to check for consistency in scoring.
Data synthesis
Following data extraction and quality appraisal, findings were synthesised using a convergent segregated approach (Stern et al., Citation2020). As meta-analysis of quantitative data and meta-aggregation of qualitative data were not possible narrative syntheses for qualitative and quantitative were undertaken. Qualitative data were coded in NVivo into categories that explored: the use of constant observation with people living with dementia; characteristics of those providing and receiving constant observation; and evidence of person-centred theories and practice. Outcome data were tabulated according to outcomes measured and organised by intervention type. Data for all intervention studies relating to implementation, fidelity and sustainability were tabulated according to the TiDier framework (Hoffmann et al., Citation2014). We recorded data relating to the sustainability of the intervention beyond the study. In addition, any evidence of co-design of the intervention (broadly defined to include for example, working groups of hospital staff as part of a quality improvement project), was documented (supplementary file 1). Quantitative and qualitative syntheses were then combined in tables and descriptive accounts of the evidence.
Findings
Initial searches identified 1905 records after duplicates were removed. A total of 116 full-text records were assessed for eligibility, of which 21 met the inclusion criteria, reporting on 20 studies (). Citation and surveillance searches identified an additional six records related to four studies, leading to a total of 26 papers reporting on 24 studies (). Seven quantitative, eleven mixed methods and six qualitative studies reported use of constant observation with people with dementia, older people with delirium (with or without dementia) and older people with cognitive impairment. Fourteen studies implemented interventions aimed at improving constant observation and ten studies reported current constant observation practices and processes.
Table 1. Characteristics of included studies.
Eleven studies were undertaken in Australia, seven in USA, five in the UK, and one in Canada. The majority (n = 20) took place in a single hospital site and four in multiple sites (range 2–7).
The fourteen intervention studies reported the impact of adaptations to constant observation in terms of: how patients were assessed as needing constant observation; the experience of patients; and patient, staff and organisational outcomes. All intervention studies were multi-component, combining elements of staff training, changes to constant observation allocation processes, and/or the development of policies or guidelines. Eight studies reported training staff or volunteers to provide one-to-one or group activities. Four studies adapted the environment so constant observation could be provided by a member of staff to more than one person at a time (e.g. cohorting). Four studies focused on improving assessments and processes for allocating patients to different levels of constant observation throughout their admission.
Participants included patients with dementia, delirium or cognitive impairment allocated to constant observation (n = 13), hospital staff involved with the provision of constant observation (n = 14), carers (n = 1), and volunteers (n = 2). For studies that included participants with dementia and/or cognitive impairment, the sample size ranged from 12—458 people. Twenty studies focused only on the use of constant observation with people with dementia and/or delirium or older people with cognitive impairment, while four studies reported the use of constant observation with mixed patient populations including those with dementia and/or delirium.
Across intervention studies, adaptations to constant observation were followed-up for between three months to two years. Reporting of the organisation of constant observation varied across studies with some detailing the number of patients supported and/or the time support was available.
Use of constant observation with people with dementia admitted to hospital
Why people with dementia are allocated to constant observation
All studies found that constant observation was used to mitigate a range of safety concerns in people with dementia. These included, risk of falling, developing delirium, behaviours expressing distress that put a person at risk of harm, such as pulling at intravenous lines or physical aggression towards staff and other patients.
Constant observation processes and practices
Constant observation involved different staff to patient ratios, from one-to-one (‘specialling’) to one-to-four or more. The proximity of a member of staff to the patient ranged from being in touching distance to staying in the same bed bay or maintaining visual contact. Eleven studies focused on constant observation as one-to-one activities, four studies focused on ‘cohorting’ constant observation activities where patients were cared for in the same bed bay, and nine studies described using combinations of the two practices. From the nine studies describing use of different levels of constant observation, four associated this decision with the completion of risk assessment tools (Bartlett & Planning, Citation2014; Connors et al., Citation2017; Jones et al., Citation2019; Wray & Rajab-Ali, Citation2014).
Staff and volunteer responsibilities during constant observation were described with reference to activities that reduced distress and/or distracted people with dementia/delirium. How staff and volunteers provide support during constant observation reflected their understanding of the role and whether there was a social element built into the work. In three studies focused on delirium prevention and management, proactive approaches were expected of staff providing constant observation (Eeles et al., Citation2013; Flaherty et al., Citation2010; Sinvani et al., Citation2018). This included staff orientating patients to time and place, promoting a healthy sleep-wake cycle, encouraging independence (consisting of activities such as supporting personal hygiene, mobility, nutrition, hydration and continence), pain assessment and management, providing activities and ensuring sensory aids were used (e.g. glasses and hearing aids). Nine studies aiming to meet a person’s emotional, psychological and social needs used staff or volunteers to provide meaningful activities (Bateman et al., Citation2016; Blair et al., Citation2018; Bray et al., Citation2015; Brooke & Herring, Citation2016; Ervin & Moore, Citation2014; Jones et al., Citation2019; McDonnell et al., Citation2014; Sinvani et al., Citation2018; Waszynski et al., Citation2013). Volunteers provided companionship and activities, and talked with the patient’s family to build an understanding of the person that could inform their work and the work of the ward team (Bateman et al., Citation2016; Blair et al., Citation2018; Ervin & Moore, Citation2014; Jones et al., Citation2019; McDonnell et al., Citation2014). Staff providing activities were often healthcare assistants who could also support personal care tasks (Bray et al., Citation2015; Brooke & Herring, Citation2016; Sinvani et al., Citation2018; Waszynski et al., Citation2013). The expectations to engage actively with patients were in contrast to how constant observation was reported in studies of usual practise. These studies found staff providing constant observation regularly provided patient care to people that they had not been assigned to work with (Cook et al., Citation2020) and often did not engage with the person they were working with beyond specific care tasks (Moyle et al., Citation2011).
Staff who provide and supervise constant observation
The majority of studies (n = 18) reported that healthcare assistants (termed variously as sitters, assistants in nursing (AINs), healthcare assistants, care assistants, certified nursing assistants (CNAs), patient associates) were allocated to provide constant observation. Six studies reported the use of temporary (‘agency’ or ‘bank’) staff (Colella et al., Citation2017; Connors et al., Citation2017; Cook et al., Citation2020; de Jong et al., Citation2020; Grealish et al., Citation2019; Wray & Rajab-Ali, Citation2014). Student nurses were used in two studies (Bartlett & Planning, Citation2014; Wilkes et al., Citation2010) and registered nurses in four studies (Bray et al., Citation2015; Cook et al., Citation2020; Flaherty et al., Citation2010; Jones et al., Citation2019); the use of both student and registered nurses were in combination with healthcare assistants. In all cases, constant observation provided by healthcare assistants, temporary staff and student nurses was overseen by a named registered nurse. The level and frequency of supervision was not reported. One survey study of healthcare assistants reported variation in their experiences of supervision from registered nurses, ranging from none at all to regular and supportive contact (Graham et al., Citation2021). Staff with responsibilities for patient engagement and activities (n = 4) (Bray et al., Citation2015; Brooke & Herring, Citation2016; Jones et al., Citation2019; Sinvani et al., Citation2018) and volunteers (n = 5) (Bateman et al., Citation2016; Blair et al., Citation2018; Ervin & Moore, Citation2014; Jones et al., Citation2019; McDonnell et al., Citation2014) were supervised by a registered nurse, a senior healthcare assistant and/or a volunteer co-ordinator.
Training of staff was discussed in fifteen studies. Studies reported that the format of training was face-to-face either through workshops, classroom-based teaching or brief ward-based sessions (n = 7) (Blair et al., Citation2018; Brooke & Herring, Citation2016; Connors et al., Citation2017; Eeles et al., Citation2013; Ervin & Moore, Citation2014; Sinvani et al., Citation2018; Wray & Rajab-Ali, Citation2014). Two studies used self-directed learning methods using workbooks or an online course (Bray et al., Citation2015; Graham et al., Citation2021). Where the length and frequency of training was reported (n = 9), this varied from regular <30 min sessions (Flaherty et al., Citation2010; Sinvani et al., Citation2018; Wray & Rajab-Ali, Citation2014) to full-time training for three weeks (Sinvani et al., Citation2018). Training of one day or more was provided for volunteers (Bateman et al., Citation2016; Blair et al., Citation2018; Ervin & Moore, Citation2014) and for staff providing constant observation that focused on delirium management and prevention (Eeles et al., Citation2013; Sinvani et al., Citation2018). Only two studies reported the impact of training; volunteers’ attitude to people with dementia improved (Bateman et al., Citation2016) and staff made commitments to use person-centred approaches during constant observation (Connors et al., Citation2017). Whether these changes improved constant observation practices was unclear.
Measures of effectiveness of constant observation
Outcome measures
Twelve intervention studies reported patient outcomes, seven staff outcomes and ten process outcomes. Studies focused on current practices of constant observation reported patient outcomes (n = 1), staff outcomes (n = 7) and process outcomes (n = 6) (see ).
Table 2. Outcomes by intervention type and usual practice studies.
Patient outcomes
The majority of intervention studies measured effectiveness of constant observation in terms of patient outcomes related to safety and health status such as falls, length of stay and mortality (n = 10) (Bateman et al., Citation2016; Blair et al., Citation2018; Bray et al., Citation2015; Brooke & Herring, Citation2016; Colella et al., Citation2017; Eeles et al., Citation2013; Flaherty et al., Citation2010; Jones et al., Citation2019; Sinvani et al., Citation2018; Wray & Rajab-Ali, Citation2014). Patient experience in terms of emotional, psychological and social wellbeing was only reported in three intervention studies (Bray et al., Citation2015; McDonnell et al., Citation2014; Waszynski et al., Citation2013) and one study of usual practice (Cook et al., Citation2020).
Safety and health status related patient outcomes were mixed. Falls (measured in nine studies) were reduced in three studies (Bray et al., Citation2015; Brooke & Herring, Citation2016; Wray & Rajab-Ali, Citation2014) and were unchanged in five studies (Bateman et al., Citation2016; Blair et al., Citation2018; Colella et al., Citation2017; Eeles et al., Citation2013; Jones et al., Citation2019). Length of stay (n = 5) reduced in two studies (Bateman et al., Citation2016; Sinvani et al., Citation2018), was unchanged in two (Eeles et al., Citation2013; Flaherty et al., Citation2010) and increased in one (Blair et al., Citation2018). Two studies of multi-component constant observation interventions for delirium care found a significant reduction in mortality (Eeles et al., Citation2013; Sinvani et al., Citation2018). All four studies reporting discharge destination reported no change (Blair et al., Citation2018; Eeles et al., Citation2013; Flaherty et al., Citation2010; Sinvani et al., Citation2018). One study reported lower incidence of readmission (Blair et al., Citation2018).
Three studies recorded medication use: one study of a volunteer programme found that patients were more likely to be discharged with analgesics potentially demonstrating increased awareness and treatment of a person’s pain (Bateman et al., Citation2016); one study of cohorting that included a multidisciplinary approach to the care and treatment of patients with or at risk of delirium, found patients were less likely to be prescribed antipsychotics (Sinvani et al., Citation2018); and one study of the use of volunteers for engaging patients found no difference to medications prescribed (Blair et al., Citation2018).
Incidents of adverse events were reported in a number of studies, most reporting no change, for example due to behavioural incidents (Blair et al., Citation2018; Jones et al., Citation2019), pressure sores (Blair et al., Citation2018; Bray et al., Citation2015) and mortality (Bateman et al., Citation2016; Blair et al., Citation2018; Flaherty et al., Citation2010). Restraint use was reported in three studies, one found no change (Colella et al., Citation2017) while two reported they were less likely to be used (Sinvani et al., Citation2018; Wray & Rajab-Ali, Citation2014). One retrospective observational study of people with delirium reported improvements in activities of daily living upon discharge for those cared for on a cohorted bay for managing their delirium (Flaherty et al., Citation2010) and one study of a volunteer programme reported no change in incidence of new delirium (Bateman et al., Citation2016).
Studies reporting patient experience following changes to constant observation practices found improvements to patient and staff interactions. The introduction of ‘bay nursing’ led patients to feel safer and more involved in their care (Bray et al., Citation2015). Volunteer programmes and meaningful activities with staff improved patients’ mood, increased their engagement, relieved distress (Bray et al., Citation2015; McDonnell et al., Citation2014) and reduced agitation during and for a period after the activity (Wray & Rajab-Ali, Citation2014). One study of usual practice of patient and staff interactions during constant observation found that the majority of emotional responses to interactions with staff were often positive, measured using a structured observational tool (Emotional responses in care (ERIC (Fleming, Citation2005)) (Cook et al., Citation2020). Staff’s familiarity with the ward and with the person they were providing constant observation for were mediating factors that influenced the patient’s experience.
Staff outcomes
Intervention studies reported staff reactions to constant observation and changed practices (n = 5), impacts on staff knowledge, confidence and attitudes towards people with dementia (n = 3), and outcomes for staff (n = 4).
Changes to practices, such as use of activities during constant observation and clearer processes for allocating patients to constant observation, were linked to increased job satisfaction, reduced stress and burden and increased knowledge of their patients both for staff providing constant observation as well as other staff on the ward (Bateman et al., Citation2016; Blair et al., Citation2019; Bray et al., Citation2015; Connors et al., Citation2017; Ervin & Moore, Citation2014; Jones et al., Citation2019; McDonnell et al., Citation2014). Studies of usual practice that found constant observation was not recognised as skilled, important work by staff who were focused on risk management through restrictive practices (Moyle et al., Citation2011; Wilkes et al., Citation2010). In contrast, staff providing constant observation who recognised the model’s potential to benefit patients reported the importance of being empathic and present with the person (Schroeder, Citation2016). Despite staff recognition of the potential benefits of constant observation, one survey reported that staff felt pressured to decrease its use (Sinvani et al., Citation2019).
Knowledge, confidence and attitudes towards people with dementia improved following changes to constant observation, but it was unclear the impact this had on practice (Bateman et al., Citation2016; Connors et al., Citation2017; Jones et al., Citation2019). One study that surveyed staff on their current understanding of falls prevention (de Jong et al., Citation2020) found that while staff were knowledgeable of the risk factors associated with falls, they were limited in their capability to prevent a fall or actions to take following a fall.
Process outcomes
Process outcomes were reported in ten intervention studies focusing on the acceptability of new ways of working (Bateman et al., Citation2016; Blair et al., Citation2018; Bray et al., Citation2015; Brooke & Herring, Citation2016; McDonnell et al., Citation2014), changes in the allocation of constant observation (Blair et al., Citation2018; Brooke & Herring, Citation2016; Colella et al., Citation2017; Connors et al., Citation2017; Jones et al., Citation2019; Sinvani et al., Citation2018; Wray & Rajab-Ali, Citation2014), and numbers of patients supported through the new intervention (Blair et al., Citation2018).
The introduction of staff and volunteers to provide activities and engage people with dementia on a one-to-one or group basis was largely welcomed by ward staff (Bateman et al., Citation2016; Blair et al., Citation2018; Bray et al., Citation2015; Brooke & Herring, Citation2016; McDonnell et al., Citation2014). One mixed methods study of a non-randomised controlled trial reported initial concerns from staff about the suitability of volunteers to provide certain support, such as at meal times and for mobility (Blair et al., Citation2019). Following implementation that included clarifying the roles of volunteers, staff considered volunteers to be members of the team who contributed to the work on the ward.
Seven studies reported allocating patients to lower staff:patient ratios of constant observation, changes to decision-making processes and use of activities (Blair et al., Citation2018; Brooke & Herring, Citation2016; Colella et al., Citation2017; Connors et al., Citation2017; Jones et al., Citation2019; Sinvani et al., Citation2018; Wray & Rajab-Ali, Citation2014). Only one study reported the numbers of patients supported through the intervention (Blair et al., Citation2018).
Economic outcomes
Costs of the interventions were reported in terms of acknowledging the cost of implementing an intervention (Bateman et al., Citation2016; Bray et al., Citation2015). The details and impact on resource use, such as length of patient stay, were not, however, reported. Three studies reported reductions to staffing costs where an intervention had reduced the use of one-to-one support or provided one-to-one support differently through activities staff and volunteers (Colella et al., Citation2017; Jones et al., Citation2019; Wray & Rajab-Ali, Citation2014).
How is person-centred care applied and supported during constant observation?
Four intervention studies referenced person-centred frameworks as informing changes to constant observation practices and training of staff and volunteers (Bateman et al., Citation2016; Blair et al., Citation2019; Connors et al., Citation2017; Ervin & Moore, Citation2014). Not all studies referred to person-centred care, some referred to therapeutic approaches to constant observation and some referred to both. Therapeutic approaches was a generic term for interventions focused around practical aspects of care, such as getting a person out of bed and getting dressed, as well as providing activities (Jones et al., Citation2019), pain management, regular help to use the toilet, involvement of the family (Bartlett & Planning, Citation2014).
The components of interventions were described, however data relating to the fidelity of their use were often lacking (supplementary file 2). Five intervention studies reported use of a document to collect personal and social information from the person and their family that could be used to inform activities and care (Bateman et al., Citation2016; Blair et al., Citation2019; Bray et al., Citation2015; Ervin & Moore, Citation2014; Waszynski et al., Citation2013). However, none of the studies reported how well these documents were completed or how often they were referred to inform practice. One service evaluation of usual care using retrospective review of medical notes (Bartlett & Planning, Citation2014) reported evidence of involvement from a person’s family in care notes, although a form to gather key personal information was only completed for 13% of patients receiving constant observation.
Descriptions of person-centred care during constant observation were reported in eight intervention studies (Blair et al., Citation2019; Bray et al., Citation2015; Brooke & Herring, Citation2016; Connors et al., Citation2017; Ervin & Moore, Citation2014; Jones et al., Citation2019; McDonnell et al., Citation2014; Waszynski et al., Citation2013). This focused on examples related to volunteers or staff interacting with people with dementia in conversations and activities (Blair et al., Citation2019; Bray et al., Citation2015; Brooke & Herring, Citation2016; Connors et al., Citation2017; Ervin & Moore, Citation2014; Jones et al., Citation2019; McDonnell et al., Citation2014; Waszynski et al., Citation2013). With the exception of one case study that observed practice using Dementia Care Mapping to measure levels of wellbeing (Waszynski et al., Citation2013), all examples from the eight studies were self-reported by those providing constant observation or from interviews with other ward staff.
The links between applying person-centred approaches to mitigate risk and reduced instances of distressed behaviours were considered in four intervention studies (Blair et al., Citation2019; Bray et al., Citation2015; McDonnell et al., Citation2014; Waszynski et al., Citation2013). These studies suggested that by engaging with a patient’s social and emotional needs, staff could improve a person’s mood, help the person to be calmer and reduce the need to use more restrictive practices to ensure a person’s safety. In two studies on the use of volunteers, staff interviews suggested there were links between occupation and less restrictive practice (Blair et al., Citation2019) and reduced distress (McDonnell et al., Citation2014). Feedback from staff providing cohort nursing suggested that the changes had reduced incidents of aggression (Bray et al., Citation2015). However, in these three studies, with the exception of reductions in the use of one-to-one nursing support (Blair et al., Citation2018; Bray et al., Citation2015) pre-post measures related to practice and patient responses to care were not collected. One study from the USA of the use of personalised activities during constant observation (Waszynski et al., Citation2013), did measure levels of agitation before, during and after activities using the Agitated Behaviour Scale (Bogner et al., Citation1999). This study found reductions in levels of agitation during and after activities even for people rated as severely agitated. Staff reflective accounts supported these observations, suggesting that meaningful engagement with the person was beneficial. Only one study of usual practice explored the quality of interactions between staff and patients and the responses of patients to those interactions during constant observation (Cook et al., Citation2020). While the majority of interactions and responses to those interactions were rated as positive, staff attempts to reassure distressed patients received negative responses. Several studies outlined strategies staff could use to reduce distress but whether they were effective or not was not measured (Colella et al., Citation2017; Flaherty & Little, Citation2011; Wray & Rajab-Ali, Citation2014).
When person-centred approaches to constant observation extended to consider the needs of a patient’s family and the needs of staff this could reduce carer burden, provide respite and emotional support (Blair et al., Citation2019). Staff providing activities during constant observation found the work rewarding (Waszynski et al., Citation2013).
Embedding person-centred practices for constant observation was influenced by how engaged all ward staff were with the intervention. Specifically, if there was a shared understanding of constant observation responsibilities, if staff were available, and if the organisation valued this work. One study found that while there was good engagement with changes to constant observation practices in the study ward, wider engagement across the hospital was lacking (Connors et al., Citation2017). Support for cohort nursing was accepted by participating staff but they were frustrated when staff shortages meant the bay had to revert to normal ward cover practices (Bray et al., Citation2015).
In studies reporting the use of volunteers to provide engagement with people living with dementia, they were a welcome addition to the ward (Bateman et al., Citation2016; Blair et al., Citation2019; Ervin & Moore, Citation2014; McDonnell et al., Citation2014). Volunteers’ roles were understood as distinct to staff roles, with nursing staff acknowledging that when volunteers were working with patients, staff had time to work with other patients. In only one of these studies did nursing staff report that they had learnt and incorporated new strategies for working with people with dementia into their own practice (Blair et al., Citation2019). This reflected how the role of constant observers was represented as set apart from ward based work, with a division of responsibilities between staff that worked with patients receiving constant observations and those providing ward based care (Cook et al., Citation2020; Moyle et al., Citation2011; Schroeder, Citation2016).
Discussion
The review synthesised evidence from 24 studies that reported current practices and interventions to enhance constant observation for people with dementia and/or delirium during hospital admissions. Most of the studies were in single sites and reported quality improvement initiatives or descriptive accounts of practice. Constant observation was used for people with dementia who were a risk to themselves or others or who had developed delirium (Dewing, Citation2013; Wood et al., Citation2018). Non-registered staff were instrumental in delivering constant observation. The exception was where staff provided constant observation for patients with delirium or were offering social engagement as part of their role. The organisational reliance on non-registered staff with inconsistent access to professional supervision or review would infer that despite the range of issues and patient needs being addressed, this work is not seen as complex or difficult. Preparation of non-registered staff working with patients with cognitive impairment often focuses on tasks but overlooks relational aspects of care despite recognition that patient experience is enhanced when care is provided with dignity and empathy (Sarre et al., Citation2018). This, combined with a focus on prevention of falls and reduction of risk may explain the variable quality of handover information, the lack of documentation and patient specific action plans described in the studies.
Patient outcomes mainly related to safety and health status are important for both patients and hospitals. However, there was limited evidence that changes to constant observation practices and processes impacted these outcomes. This resonates with hospital studies implementing person-centred practices more generally with people with dementia that report improvements to patient and carer experience but not health status outcomes (Goldberg et al., Citation2013). Several studies theorised that patient experience could be enhanced in using therapeutic approaches to constant observation, this included efforts to maintain a person’s identity through meaningful interactions and promote independence. Interventions that focused on providing patients opportunities for conversations and activities were linked to improved engagement and reduced distress for people with dementia. Similar findings have been reported in systematic reviews of activities in hospitals and care homes for people with dementia (Lourida et al., Citation2020; Travers et al., Citation2016). Evidence associating engagement during constant observation with reductions in behaviours considered to carry risk of harm and/or decreasing a person’s actual risk of harm was lacking. Understanding if and how person-centred approaches to constant observation can meet a person’s psychosocial needs and reduce their physical risk of harm is an area for future research. While there are notable challenges to providing person-centred care in hospitals (Clissett et al., Citation2013; Grealish et al., Citation2019), it is possible and may address some of the deficiencies of the care environment. A recent pilot study of ward-wide training and on-going endorsement for person-centred care did report improvements in care quality and reductions in distressed behaviours (Chenoweth et al., Citation2022). However, reduction in distressed behaviours was not sustained over time for people with dementia with longer length of stay. Managing the complex interaction between the environment, the person and how staff are equipped to provide support is an implementation challenge.
Suggestions for strategies when working with patients in moments of severe distress and when behaviours were considered to carry risk of harm were offered as part of a few decision tools, but their effectiveness was not explored. Evidence of strategies for working with people with dementia with different needs during constant observation were limited to times when patients were able to engage with staff and volunteers in conversations, activities or when being supported with everyday tasks such as getting dressed. Examples of constant observation at times of severe patient distress were limited to a few brief reports and how staff provided constant observation at these times was not reported. There was also limited reference to staff training in de-escalation techniques. Previous studies have explored refusals of care of people with dementia in care homes and hospitals (Backhouse et al., Citation2022; Featherstone et al., Citation2019; O’Brien et al., Citation2020). In developing a training intervention to improve hospital staff communication skills with the potential to reduce refusals of care, Harwood et al. (Citation2018) acknowledged the tensions of delivering health-care tasks while employing a person-centred approach. Operationalising person-centred approaches for constant observation at times of heightened distress will require more understanding of strategies used in the moment that can support a person’s best interests without increasing their distress and associated risks of harm.
The question that was the starting point for this review remains, how can person-centred approaches be consistently applied in risk averse environments (Handley et al., Citation2019)? All interventions were multi-component and often multidisciplinary, demonstrating the complexity of embedding new ways of working. Learning from related improvement initiatives, such as End PJ Paralysis (Skrypak, Citation2018) and the TOP 5 documents in Australia (Isaac et al., Citation2018; Luxford et al., Citation2015), suggest implementation strategies that help to build a shared sense of responsibility and support staff to work closer with families or other key supporters are important factors. The level of encouragement required is likely to differ across and within hospitals depending on whether staff with different levels of responsibility and ward leadership recognise the value of any changes to practice (Aarons et al., Citation2015; Stetler et al., Citation2014). An additional challenge for constant observation will be addressing the ambiguities of developing a shared sense of responsibility when the activity is often viewed as the role of a single staff member. Building and sustaining value for new ways of working across ward teams is likely to be key for embedding change (Fossey et al., Citation2019).
Limitations
The limitations of studies related to their transferability and potential for bias have been described as part of synthesising the evidence. The majority of included studies had small sample sizes and were conducted at single sites, some findings could be context dependent. Several studies reported service evaluations and quality improvement efforts, increasing the potential for bias. We excluded studies using interventions aimed at reducing the use of constant observation, the focus of this review was to understand how constant observation is used with people with dementia and how a person-centred approach could be achieved. It is possible that these excluded studies offered additional insights. However, their focus on the use of technology or regular rounding were unlikely to address the purpose of the review.
Conclusion
A person-centred approach to constant observation for people with dementia is likely to improve the experience for both patients and staff and could anticipate and reduce distress. When constant observation is used by staff to engage a person with dementia and their visitors in a meaningful way, the person is likely to feel comforted and connected with staff. There was a tension in the evidence for whether non-registered staff with some additional training and supervision could provide effective care when faced with organisational priorities to reduce risk through strategies that favour containment. Approaches more likely to succeed are those that are grounded in patient and staff experiences linking with wider systems of care to identify the range of skills and organisational support needed to improve the inpatient experience of people living with dementia.
Author contributions
MH, CG, RHH, RP and CS contributed to the study concept and design. MH led the conduct of the systematic review, synthesis and manuscript preparation. DT, RH, NT and AY completed data collection and extraction. All authors participated in the interpretation of results, revision of the manuscript and read and approved the final manuscript.
Supplemental Material
Download Zip (51.6 KB)Acknowledgements
The authors would like to acknowledge the contributions of the late Professor Frances Bunn who had significant involvement in the conceptualisation of the study and advised on the conduct of the systematic review.
Data sharing statement
All the data of this systematic review is available in the manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Aarons, G. A., Ehrhart, M. G., Farahnak, L. R., & Hurlburt, M. S. (2015). Leadership and organizational change for implementation (LOCI): A randomized mixed method pilot study of a leadership and organization development intervention for evidence-based practice implementation. Implementation Science, 10(1), 1–12. https://doi.org/10.1186/s13012-014-0192-y
- Backhouse, T., Jeon, Y.-H., Killett, A., & Mioshi, E. (2022). How do family carers and care-home staff manage refusals when assisting a person with advanced dementia with their personal care? Dementia (London, England), 21(8), 2458–2475. https://doi.org/10.1177/14713012221123578
- Bail, K., Barratt, M., Davidson, A., Isbel, S., Kaye, T., Kellett, J., Preston, E., Stanton, R., & Scarvell, J. (2023). A 4‐bed close-observation pod model of multidisciplinary care in hospital: A mixed methods study 4-bed close observation pod study. Collegian, 30(3), 465–474. https://doi.org/10.1016/j.colegn.2022.12.007
- Bartlett, K., & Planning, D. (2014). A cross-sectional cohort study.
- Bateman, C., Anderson, K., Bird, M., & Hungerford, C. (2016). Volunteers improving person-centred dementia and delirium care in a rural Australian hospital. Rural and Remote Health, 16(2), 1–12. https://doi.org/10.22605/RRH3667
- Blair, A., Anderson, K., & Bateman, C. (2018). The “Golden Angels”: Effects of trained volunteers on specialling and readmission rates for people with dementia and delirium in rural hospitals. International Psychogeriatrics, 30(11), 1707–1716. https://doi.org/10.1017/S1041610218000911
- Blair, A., Bateman, C., & Anderson, K. (2019). “They take a lot of pressure off us”: Volunteers reducing staff and family care burden and contributing to quality of care for older patients with cognitive impairment in rural hospitals. Australasian Journal on Ageing, 38(S2), 34–45. https://doi.org/10.1111/ajag.12612
- Bogner, J. A., Corrigan, J. D., Stange, M., & Rabold, D. (1999). Reliability of the agitated behavior scale. The Journal of Head Trauma Rehabilitation, 14(1), 91–96. https://doi.org/10.1097/00001199-199902000-00012
- Bray, J., Evans, S., Bruce, M., Carter, C., Brooker, D., Milosevic, S., Thompson, R., & Hutt, L. (2015). Improving activity and engagement for patients with dementia. Nursing Older People, 27(8), 22–26. https://doi.org/10.7748/nop.27.8.22.e700
- Brooke, J., & Herring, S. (2016). Development of an activities care crew to support patients. Nursing Older People, 28(8), 20–25. https://doi.org/10.7748/nop.2016.e835
- Brooker, D., & Latham, I. (2015). Person-centred dementia care: Making services better with the VIPS framework. Jessica Kingsley Publishers.
- Chenoweth, L., Williams, A., Fry, M., Endean, E., & Liu, Z. (2022). Outcomes of person-centered care for persons with dementia in the acute care setting: A pilot study. Clinical Gerontologist, 45(4), 983–997. https://doi.org/10.1080/07317115.2021.1946233
- Clissett, P., Davina, P., Harwood, R. H., & Gladman, J. R. (2013). The challenges of achieving person-centred care in acute hospitals: A qualitative study of people with dementia and their families. International Journal of Nursing Studies, 50(11), 1495–1503. https://doi.org/10.1016/j.ijnurstu.2013.03.001
- Colella, J., Aroh, D., Douglas, C., VanBuitenen, N., Galesi, J., Castro, A., Tank, L., Parulekar, M., & Menacker, M. (2017). Managing delirium behaviors with one-to-one sitters. Nursing, 47(8), 1–5. https://doi.org/10.1097/01.NURSE.0000521038.27830.b4
- Connors, D., Mills, B., & Dewing, J. (2017). ‘More than a sitter’: A practice development project on special observations in acute general hospital care.
- Cook, J., Palesy, D., Lapkin, S., & Chenoweth, L. (2020). An observational study of older patient specialling in acute hospital settings. International Journal of Older People Nursing, 15(4), e12323. https://doi.org/10.1111/opn.12323
- Coyle, M. A., Wilson, V., Lapkin, S., & Traynor, V. (2020). What are we asking for when requesting “specialling” for the confused hospitalised older person? A concept analysis. International Journal of Older People Nursing, 15(2), e12302. https://doi.org/10.1111/opn.12302
- Critical Appraisal Skills Programme. (2022a). CASP Cohort Study Checklist.
- Critical Appraisal Skills Programme. (2022b). CASP Qualitative Studies Checklist.
- de Jong, L. D., Weselman, T., Kitchen, S., & Hill, A. M. (2020). Exploring hospital patient sitters’ fall prevention task readiness: A cross‐sectional survey. Journal of Evaluation in Clinical Practice, 26(1), 42–49. https://doi.org/10.1111/jep.13114
- Dewing, J. (2013). Special observation and older persons with dementia/delirium: A disappointing literature review. International Journal of Older People Nursing, 8(1), 19–28. https://doi.org/10.1111/j.1748-3743.2011.00304.x
- Dean, R., Proudfoot, R., & Lindesay, J. (1993). The quality of interactions schedule (QUIS): Development, reliability and use in the evaluation of two domus units. International Journal of Geriatric Psychiatry, 8(10), 819–826.
- Eeles, E., Thompson, L., McCrow, J., & Pandy, S. (2013). Management of delirium in medicine: Experience of a close observation unit. Australasian Journal on Ageing, 32(1), 60–63. https://doi.org/10.1111/ajag.12007
- Ervin, K., & Moore, S. (2014). Rural nurses’ perceptions of a volunteer program in an acute setting: Volunteers delivering person-centred care for patients with dementia and delirium. Open Journal of Nursing, 4(1), 27–33. https://doi.org/10.4236/ojn.2014.41005
- Featherstone, K., Northcott, A., & Bridges, J. (2019). Routines of resistance: An ethnography of the care of people living with dementia in acute hospital wards and its consequences. International Journal of Nursing Studies, 96, 53–60. https://doi.org/10.1016/j.ijnurstu.2018.12.009
- Flaherty, J. H., & Little, M. O. (2011). Matching the environment to patients with delirium: Lessons learned from the delirium room, a restraint‐free environment for older hospitalized adults with delirium. Journal of the American Geriatrics Society, 59, S295–S300. https://doi.org/10.1111/j.1532-5415.2011.03678.x
- Flaherty, J. H., Steele, D. K., Chibnall, J. T., Vasudevan, V. N., Bassil, N., & Vegi, S. (2010). An ACE unit with a delirium room may improve function and equalize length of stay among older delirious medical inpatients. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 65(12), 1387–1392. https://doi.org/10.1093/gerona/glq136
- Fleming, R. (2005). Emotional responses in care assessment (ERiC). The Hammond Care Group.
- Fossey, J., Garrod, L., Tolbol Froiland, C., Ballard, C., Lawrence, V., & Testad, I. (2019). What influences the sustainability of an effective psychosocial intervention for people with dementia living in care homes? A 9 to 12‐month follow‐up of the perceptions of staff in care homes involved in the WHELD randomised controlled trail. International Journal of Geriatric Psychiatry, 34(5), 674–682. https://doi.org/10.1002/gps.5066
- Goldberg, S. E., Bradshaw, L. E., Kearney, F. C., Russell, C., Whittamore, K. H., Foster, P. E. R., Mamza, J., Gladman, J. R. F., Jones, R. G., Lewis, S. A., Porock, D., & Harwood, R. H. (2013). Care in specialist medical and mental health unit compared with standard care for older people with cognitive impairment admitted to general hospital: Randomised controlled trial (NIHR TEAM trial). BMJ (Clinical Research ed.), 347, f4132. https://doi.org/10.1136/bmj.f4132
- Goldberg, S. E., Whittamore, K. H., Pollock, K., Harwood, R. H., & Gladman, J. R. (2014). Caring for cognitively impaired older patients in the general hospital: A qualitative analysis of similarities and differences between a specialist Medical and Mental Health Unit and standard care wards. International Journal of Nursing Studies, 51(10), 1332–1343. https://doi.org/10.1016/j.ijnurstu.2014.02.002
- Graham, F., Eaton, E., Jeffrey, C., Secher-Jorgensen, H., & Henderson, A. (2021). “Specialling” and “Sitters”: What does communication between registered nurses and unregulated workers reveal about care? Collegian, 28(5), 482–488. https://doi.org/10.1016/j.colegn.2020.12.004
- Grealish, L., Chaboyer, W., Darch, J., Real, B., Phelan, M., Soltau, D., Lunn, M., Brandis, S., Todd, J. A., & Cooke, M. (2019). Caring for the older person with cognitive impairment in hospital: Qualitative analysis of nursing personnel reflections on fall events. Journal of Clinical Nursing, 28(7–8), 1346–1353. https://doi.org/10.1111/jocn.14724
- Grealish, L., Simpson, T., Soltau, D., & Edvardsson, D. (2019). Assessing and providing person-centred care of older people with cognitive impairment in acute settings: Threats, variability, and challenges. Collegian, 26(1), 75–79. https://doi.org/10.1016/j.colegn.2018.03.009
- Handley, M., Bunn, F., & Goodman, C. (2019). Supporting general hospital staff to provide dementia sensitive care. A realist evaluation. International Journal of Nursing Studies, 96, 61–71. https://doi.org/10.1016/j.ijnurstu.2018.10.004
- Harwood, R. H., O’Brien, R., Goldberg, S. E., Allwood, R., Pilnick, A., Beeke, S., Thomson, L., Murray, M., Parry, R., Kearney, F., Baxendale, B., Sartain, K., & Schneider, J. (2018). A staff training intervention to improve communication between people living with dementia and health-care professionals in hospital: The VOICE mixed-methods development and evaluation study. Health Services and Delivery Research, 6(41), 1–134. https://doi.org/10.3310/hsdr06410
- Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D., Altman, D. G., Barbour, V., Macdonald, H., Johnston, M., Lamb, S. E., Dixon-Woods, M., McCulloch, P., Wyatt, J. C., Chan, A.-W., & Michie, S. (2014). Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ (Clinical Research ed.), 348, g1687. https://doi.org/10.1136/bmj.g1687
- Hong, Q. N., Gonzalez‐Reyes, A., & Pluye, P. (2018). Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). Journal of Evaluation in Clinical Practice, 24(3), 459–467. https://doi.org/10.1111/jep.12884
- Isaac, L. M., Buggy, E., Sharma, A., Karberis, A., Maddock, K. M., & Weston, K. M. (2018). Enhancing hospital care of patients with cognitive impairment. International Journal of Health Care Quality Assurance, 31(2), 173–186. https://doi.org/10.1108/IJHCQA-11-2016-0173
- Jones, A., Aylward, R., & Jones, A. (2019). Enhanced supervision: New ways to promote safety and well-being in patients requiring one-to-one or cohort nursing. Nursing Management, 26(2), 22–29. https://doi.org/10.7748/nm.2019.e1827
- Kitwood, T. M. (1997). Dementia reconsidered: The person comes first (Vol. 20) Open University Press Buckingham.
- Lourida, I., Gwernan-Jones, R., Abbott, R., Rogers, M., Green, C., Ball, S., Hemsley, A., Cheeseman, D., Clare, L., Moore, D., Hussey, C., Coxon, G., Llewellyn, D. J., Naldrett, T., & Thompson Coon, J. (2020). Activity interventions to improve the experience of care in hospital for people living with dementia: A systematic review. BMC Geriatrics, 20(1), 1–14. https://doi.org/10.1186/s12877-020-01534-7
- Luxford, K., Axam, A., Hasnip, F., Dobrohotoff, J., Strudwick, M., Reeve, R., Hou, C., & Viney, R. (2015). Improving clinician–carer communication for safer hospital care: A study of the ‘TOP 5’strategy in patients with dementia. International Journal for Quality in Health Care, 27(3), 175–182. https://doi.org/10.1093/intqhc/mzv026
- McDonnell, A., McKeown, J., Keen, C., Palfreyman, J., & Bennett, N. (2014). Introducing on-ward volunteers to work with patients with dementia. Nursing Older People, 26(4), 28–33. https://doi.org/10.7748/nop2014.04.26.4.28.e572
- Moyle, W., Borbasi, S., Wallis, M., Olorenshaw, R., & Gracia, N. (2011). Acute care management of older people with dementia: A qualitative perspective. Journal of Clinical Nursing, 20(3–4), 420–428. https://doi.org/10.1111/j.1365-2702.2010.03521.x
- O’Brien, R., Beeke, S., Pilnick, A., Goldberg, S. E., & Harwood, R. H. (2020). When people living with dementia say ‘no’: Negotiating refusal in the acute hospital setting. Social Science & Medicine (1982), 263, 113188. https://doi.org/10.1016/j.socscimed.2020.113188
- O’Brien, R., Goldberg, S. E., Pilnick, A., Beeke, S., Schneider, J., Sartain, K., Thomson, L., Murray, M., Baxendale, B., & Harwood, R. H. (2018). The VOICE study–A before and after study of a dementia communication skills training course. PLoS One, 13(6), e0198567. https://doi.org/10.1371/journal.pone.0198567
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5(1), 1–10. https://doi.org/10.1186/s13643-016-0384-4
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews, 10(1), 1–11. https://doi.org/10.1186/s13643-021-01626-4
- Rochefort, C. M., Ward, L., Ritchie, J. A., Girard, N., & Tamblyn, R. M. (2012). Patient and nurse staffing characteristics associated with high sitter use costs. Journal of Advanced Nursing, 68(8), 1758–1767.
- Sarre, S., Maben, J., Aldus, C., Schneider, J., Wharrad, H., Nicholson, C., & Arthur, A. (2018). The challenges of training, support and assessment of healthcare support workers: A qualitative study of experiences in three English acute hospitals. International Journal of Nursing Studies, 79, 145–153. https://doi.org/10.1016/j.ijnurstu.2017.11.010
- Scherer, R. W., & Saldanha, I. J. (2019). How should systematic reviewers handle conference abstracts? A view from the trenches. Systematic Reviews, 8(1), 1–6. https://doi.org/10.1186/s13643-019-1188-0
- Schroeder, R. (2016). Bearing witness: The lived experience of sitting with patients. Archives of Psychiatric Nursing, 30(6), 678–684. https://doi.org/10.1016/j.apnu.2016.03.005
- Sinvani, L., Strunk, A., Patel, V., Shah, S., Mulvany, C., Kozikowski, A., Boltz, M., Pekmezaris, R., & Wolf-Klein, G. (2019). Constant observation practices for hospitalized persons with dementia: A survey study. American Journal of Alzheimer’s Disease and Other Dementias, ®, 34(4), 223–230. https://doi.org/10.1177/1533317519826272
- Sinvani, L., Warner-Cohen, J., Strunk, A., Halbert, T., Harisingani, R., Mulvany, C., Qiu, M., Kozikowski, A., Patel, V., Liberman, T., Carney, M., Pekmezaris, R., Wolf-Klein, G., & Karlin-Zysman, C. (2018). A multicomponent model to improve hospital care of older adults with cognitive impairment: A propensity score–matched analysis. Journal of the American Geriatrics Society, 66(9), 1700–1707. https://doi.org/10.1111/jgs.15452
- Skrypak, R. (2018). End PJ Paralysis Challenge takes NHS by storm. https://www.england.nhs.uk/blog/end-pj-paralysis-challenge-takes-nhs-by-storm/
- Stern, C., Lizarondo, L., Carrier, J., Godfrey, C., Rieger, K., Salmond, S., Apostolo, J., Kirkpatrick, P., & Loveday, H. (2020). Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evidence Synthesis, 18(10), 2108–2118. https://doi.org/10.11124/JBISRIR-D-19-00169
- Stetler, C. B., Ritchie, J. A., Rycroft‐Malone, J., & Charns, M. P. (2014). Leadership for evidence‐based practice: Strategic and functional behaviors for institutionalizing EBP. Worldviews on Evidence-Based Nursing, 11(4), 219–226. https://doi.org/10.1111/wvn.12044
- Travers, C., Brooks, D., Hines, S., O’Reilly, M., McMaster, M., He, W., MacAndrew, M., Fielding, E., Karlsson, L., & Beattie, E. (2016). Effectiveness of meaningful occupation interventions for people living with dementia in residential aged care: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14(12), 163–225. https://doi.org/10.11124/JBISRIR-2016-003230
- Waszynski, C., Veronneau, P., Therrien, K., Brousseau, M., Massa, A., & Levick, S. (2013). Decreasing patient agitation using individualized therapeutic activities. The American Journal of Nursing, 113(10), 32–39; quiz 40. https://doi.org/10.1097/01.NAJ.0000435345.23040.42
- White, N., Leurent, B., Lord, K., Scott, S., Jones, L., & Sampson, E. L. (2017). The management of behavioural and psychological symptoms of dementia in the acute general medical hospital: A longitudinal cohort study. International Journal of Geriatric Psychiatry, 32(3), 297–305. https://doi.org/10.1002/gps.4463
- Wilkes, L., Jackson, D., Mohan, S., & Wallis, M. (2010). Close observation by ‘specials’ to promote the safety of the older person with behavioural disturbances in the acute care setting. Contemporary Nurse, 36(1–2), 131–142. https://doi.org/10.5172/conu.2010.36.1-2.131
- Wood, V. J., Vindrola-Padros, C., Swart, N., McIntosh, M., Crowe, S., Morris, S., & Fulop, N. J. (2018). One to one specialling and sitters in acute care hospitals: A scoping review. International Journal of Nursing Studies, 84, 61–77. https://doi.org/10.1016/j.ijnurstu.2018.04.018
- Wray, K., & Rajab-Ali, R. (2014). Safety watch: Reducing constant observation through nurse empowerment and accountability. The Journal of Nursing Administration, 44(4), 237–243. https://doi.org/10.1097/NNA.0000000000000057