Abstract
Objectives
Compared with younger and middle-aged adults, older adults are less likely to adopt new computer technology, potentially limiting access to healthcare and many other important resources available online. This limitation could impact cognitive abilities, well-being, and mental health outcomes of older adults. The aims of the present study were to increase access to online county and healthcare resources, while also assessing the impact of technology access on cognitive functioning and multiple well-being domains.
Methods
A pilot community collaboration provided a two-month tablet training intervention, focused on increasing digital independence via tablet navigation, resources access, and fraud and scam prevention, to 20 low-income older adult participants (75% female, Mage = 70.85). Pre- and post-test phone interviews were conducted to measure any changes in digital independence, cognitive abilities, well-being, mental health, and mindset.
Results
Linear mixed effects models revealed no significant changes in outcome measures from pre- to post-test. However, we found effects of digital independence on several well-being measures, providing important information for the impact of technology access and training for low-income older adults.
Conclusion
This pilot intervention offers limited but promising results, inspiring further investigations that may inform public health and policy services to address barriers to access and potentially improve psychological health.
Keywords:
Introduction
Despite internet usage rates for older adults rapidly increasing (Faverio, Citation2022), there remains a large divide for information technology adoption (namely for computers and tablets) between other age groups and within the older adult population. Compared with younger and middle-aged adults, older adults consistently encompass the smallest percentage of the population to utilize information technology, despite the ever-growing size of the older adult population (Charness & Boot, Citation2022; Faverio, Citation2022).
Recent reports have indicated that the majority of upper-middle aged and older adults report limited internet experience or use (Kim et al., Citation2023; Li, Citation2015; Rosell et al., Citation2022), and that, among middle-aged and older adults, younger and more educated adults were more likely to use information technology and e-health services (Irizarry et al., Citation2017; Reinwand et al., Citation2018; Shaffer et al., Citation2018). Studies have also reported that the two most prominent factors associated with information technology use among older adults are cognitive abilities (Choi et al., Citation2021; Dequanter et al., Citation2022; Kobayashi et al., Citation2015; Slegers et al., Citation2009) as well as prior experience and access to support (Czaja et al., Citation2013; Duan-Porter et al., Citation2018; Mariano et al., Citation2021; Pang et al., Citation2021; Vaportzis et al., Citation2017). However, low-income older adults experience the most barriers for accessing IT devices and support during learning (Moody et al., Citation2022; Rosell et al., Citation2022; Wang et al., Citation2021; Yu et al., Citation2016) and are therefore the most likely to not adopt technology. Disparities in income, education, and cognitive functioning affect usage and comfort-level with information technology among older adults (Choi & DiNitto, Citation2013; Estacio et al., Citation2019; Hall et al., Citation2015) and raise numerous concerns for access to online health resources, functional independence, well-being, and social connection (Cheshmehzangi et al., Citation2022; Czaja, Citation2017; McCloud et al., Citation2016), particularly as societal resources continue to become more online based.
Use of information technology, such as computers and tablets, among older adults has been positively associated with feelings of self-efficacy (Hvalič-Touzery et al., Citation2022; Woodward et al., Citation2011), social support and connectedness (Choi & DiNitto, Citation2013; Czaja et al., Citation2018; Torp et al., Citation2008), and well-being and quality of life (Heo et al., Citation2015; Zheng et al., Citation2016). Additionally, research has indicated reduced depression and loneliness among participants who more frequently used the internet or information technology (Cotten et al., Citation2013; Laganá & García, Citation2013; Shapira et al., Citation2007). With the potential benefits of technology access, it is important to address barriers to entry for low-income older adults populations, such as developing programs to connect individuals with training for devices while providing user support and an encouraging environment to foster learning (e.g. Han & Nam, Citation2021).
While a number of studies have examined the relationship of technology (tablet) training and cognitive and well-being factors, only a handful have demonstrated that technology and tablet training has been associated with an increase in cognitive abilities, such as processing speed (Chan et al., Citation2016; Elliot et al., Citation2014; Vaportzis et al., Citation2017). Most other studies have found no evidence of cognitive benefits from casual technology use (e.g. Pauly et al., Citation2019; Zhang et al., Citation2022) but rather that internet or technology usage can be a protective factor for cognitive decline (e.g. Byrne & Ghaiumy Anaraky, Citation2022; Calhoun & Lee, Citation2019). Others have demonstrated moderate improvements in perceived isolation, mental well-being, and computer self-efficacy (Czaja et al., Citation2018; Pauly et al., Citation2019; Zheng et al., Citation2016), but these findings are mixed as well (Cid et al., Citation2020; Fields et al., Citation2021; Slegers et al., Citation2009).
In general, there is a growing need to address inequities in access to technological devices and learning support among low-income older adults. The technological divide creates massive disparities in perceived well-being, access to social and health-related information, and other potential benefits associated with information technology use in older adulthood (Byrne & Ghaiumy Anaraky, Citation2022; Hvalič-Touzery et al., Citation2022; Vaportzis et al., Citation2017; Zheng et al., Citation2016). By providing opportunities for low-income older adults to increase their experience and comfort level with information technology, such as tablets, we may also see increases in quality-of-life factors, such as cognitive performance, mental health, and overall well-being (e.g. Cotten et al., Citation2013; Forsman et al., Citation2018).
The present study assessed the impact of a 2-month intervention that provided technological access and training to older adults with low income. The pilot intervention was conducted entirely by community leaders from the Riverside County Office on Aging (OoA), a department whose efforts focus on developing systems to improve quality of life for vulnerable older adults, including low-income and disabled individuals. Given our prior learning intervention research with older adults (e.g. Leanos et al., Citation2020), the OoA contacted the research team to advise on their Senior Learning and Accessibility Technology Evaluation (SLATE) project during the pandemic. The role of the research team was to advise in compiling a battery of measures and developing procedures to determine if this project would improve the quality of life for their clients, thereby justifying increased efforts and funding for this program. The outcome measures for the SLATE project included digital independence (i.e. how participants rated their use and comfort level with completing various IADLs on digital devices), cognitive function, growth mindset (i.e. the belief that abilities can increase with effort), and well-being. We predicted that all outcome measures would increase from pre-test to post-test, following other skill learning interventions conducted with older adults (e.g. Chan et al. 2016; Leanos et al., Citation2020). The OoA recruited participants from their client pool, carried out the technology distribution and training with social workers, and collected the data, which was then anonymized and shared with the research team for analyses.
Method
Participants
Riverside County Office on Aging (OoA) conducted the intervention with county-level approval. The researchers were only provided with anonymized data. After conferring with the researcher’s university IRB, it was determined that, based on the advisory role the university research team was in, and that the data collected by Riverside County OoA were to be fully anonymized prior to sharing with the researchers, IRB approval for this project was not necessary. However, all participants were informed that their anonymized data from the intervention would be shared with researchers after completing the assessment timepoints, a decision made by the collaborative team to uphold transparency with the clients. More information is detailed in the procedures section below.
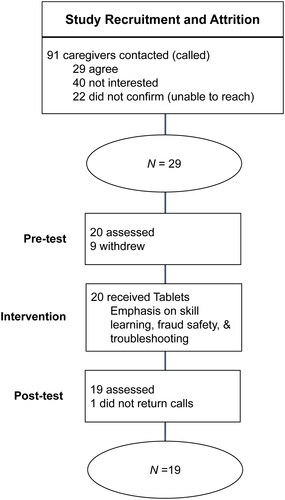
Twenty participants (75% female, Mage = 70.85, SDage = 8.95, Mdnage = 67, range = 60–87 years old at pre-test) were included in the present study (see for recruitment and attrition details and for demographic information). One participant was excluded from analyses for not completing the post-test assessment, therefore, the data were based on a 95% completion rate, with 19 of 20 participants completing post-test. Forty additional participants were contacted but ultimately denied participation because of time constraints or general disinterest.
Table 1. Participant characteristics.
The participants received no monetary compensation but were able to keep the tablets and USB WiFi dongles at the end of the intervention and were offered additional resources through the county’s network of care. Pre- and post-test assessments and questionnaires were conducted by the Office on Aging staff and social workers. Participants were also evaluated for other free support services offered through the department’s network of care.
Assessment measures
Pretest and post-test assessments measured several components of executive functioning (episodic verbal memory, working memory, cognitive control, and speed of processing), as well as general well-being, depression, loneliness, and growth mindset. An additional questionnaire relating to technological independence also was collected.
All of the measures and materials were available in English and Spanish, depending on the participants’ preferred language. When available, Spanish translations of measures provided by measure developers were used. Otherwise, a bilingual researcher, whose first language is Spanish, translated the measures/materials from English (the original language) to Spanish. The translated measures were piloted before the study to ensure that participants would understand the questions with the same meaning intended in the original English versions of the measures. Of the 19 participants included in analyses, three completed all assessments and meetings in Spanish, while the remaining 16 preferred English.
Cognitive function was assessed via the Brief Test of Adult Cognition by Telephone (BTACT; Tun & Lachman, Citation2006). This battery consists of the Rey Auditory-Verbal Learning Test (RAVLT; Schmidt, Citation1996), Backwards Digit Span (Wechsler, Citation1997), a Category Verbal Fluency task, a Number Series task, the 30-Seconds and Counting Task (30-SACT), and the Stop and Go Switch Task (SGST). Methods for testing and scoring followed Lachman and colleagues (2013) procedures. For the present study, global scores were summed from each individual task. Due to the design of some of the fluency and counting tasks, there is no established maximum global score, but within our data, the highest overall score was 148.
For all of the questionnaire measures (see Supplementary Materials), participants provided verbal number responses on a scale from 1 to 7 (specified below for each measure). Participants could provide a whole number (e.g. 3 or 7) or decimal numbers on a sliding scale (e.g. 3.2 or 6.5). Participants were always provided the option to not respond to any question.
General well-being was measured with the PERMA Profiler (Butler & Kern, Citation2016). This measure consists of 23 items relating to positive and negative emotion, engagements, relationships, meaning, accomplishment, and health. Participants verbally indicated the extent to which they experienced the feelings or agreed with the statements from each item on a scale of 1 (Not at all/Not often at all) to 7 (Completely/Very often). Analyses were based on the summed response scores (total possible score: 161).
Loneliness was measured with the Three Item Loneliness Scale (TILS; Hughes et al., Citation2004). Participants were read the questions and indicated how often they felt a certain way on a scale from 1 (Not at all) to 7 (Nearly everyday). Scores were the sum of the three responses provided (total possible score: 21).
For depression, the Patient Health Questionnaire (PHQ-2; Kroenke et al., Citation2003) was used with an adjusted response scale to align with the other questionnaires. Participants were asked to consider the last two weeks and how often they had been bothered by the described feelings on a scale from 1 (Not at all) to 7 (nearly every day). Responses were summed for the total score, with higher scores indicating depressive symptoms (maximum possible score: 14).
Participants were asked about their mindset about their abilities and their intelligence with the Growth Mindset Scale (modified for older adults to focus on learning and abilities by removing two questions that emphasize personality; Dweck, Citation2006). For these questions, participants indicated the amount to which they agreed or disagreed with the statements on a scale of 1 (Strongly Disagree) to 7 (Strongly Disagree). For scoring, relevant items were reverse scored and then responses were summed (total possible score: 32).
Finally, a digital independence questionnaire was administered to participants asking about their comfort level and use of technology for daily tasks. This questionnaire was adapted from the Lawton-Brody Instrumental Activities of Daily Living scale (IADL; Lawton & Brody, Citation1969), which asks about one’s abilities to complete daily functional tasks, such as grocery shopping, or managing finances. For this study, we modified the questions to relate these tasks to completing mobile or online versions of these tasks (for complete measure, see Supplementary Materials). This version consisted of four questions, focusing on online grocery shopping, booking transportation, online medical needs, and online banking. Each question was scored on a binary scale of ‘1’ for doing these tasks online fully independently or without assistance, or ‘0’ for any response noting assistance or support needed (total possible score: 4).
Procedure
The SLATE study consisted of a two-month tablet training intervention, in which participants received two monthly home visits, supplemented by six weekly one-to-one virtual meetings, that covered training topics from setting up email accounts, video calling, and basic device navigation to online resources, such as online benefits portal, health care, and grocery shopping. Additionally, every meeting and visit consisted of fraud education and alerts to ensure that participants were engaging safely with the devices. Finally, as an external resource, over-the-phone IT support was available for the participants to contact in between face-to-face visits.
Participants in this study were recruited in partnership with the Office on Aging (OoA) and the In-Home Supportive Services Public Authority (IHSS PA) through an existing caregiver support program. The inclusion criteria were: 60 years of age or older, an IHSS caregiver, and not using the IHSS web-based portal for payment (uses telephone timesheet submission, TTS). Participants were also recruited from OOA’s family caregiver support program, who were adults aged 60 or older, caring for relatives who are also 60 years or older. All caregivers in the study were individuals who were also eligible to receive state and county services, including Medi-Cal and food stamps. The participants spoke primarily English or Spanish.
Clients in the database who met the inclusion criteria were contacted over the phone, answered questions about their access to the internet and mobile and/or computer technology. Those with limited or no technology access were provided with a description of the program and research opportunity, and asked if they would be interested in participating. Clients were informed that, should they qualify for the technology distribution program, their participation in the research study would be voluntary and that they would receive the technology and training regardless of whether they participated in answering the research questions. Those who indicated interest in participating in data collection were screened and provided with a letter of agreement and procedure materials, which detailed the objectives and schedule of the project, as well as how confidentiality of information would be maintained, withdrawal processes, and rights to the technology provided to them. Participants gave verbal agreement over the phone to enroll and arrange a set-up date. They provided written consent via the letter of agreement during device delivery and set-up.
Two weeks before receiving their tablets and accessories (case and stylus; USB WiFi dongle if needed), participants completed a pre-test assessment with a social worker from the OoA consisting of an over-the-phone cognitive battery (BTACT; Tun & Lachman, Citation2006) and questionnaires on well-being (PERMA; Butler & Kern, Citation2016), loneliness (TILS; Hughes et al., Citation2004), depression (PHQ-2; Kroenke et al., Citation2003), mindset (Growth Mindset Scale; Dweck, Citation2006), and functional digital independence (adapted from Lawton & Brody, Citation1969).
Following the pre-test assessments, devices were delivered in person, and participants received one-to-one device walk-throughs and a program orientation. Participants were contacted one week later over the phone and then scheduled an in-person check-in for the following month to continue learning about the new technology and to walk through any issues they may have encountered. Supplementary one-to-one weekly Zoom meetings were held to cover fraud education and scam prevention topics. A total of two in-person meetings and six zoom meetings were held with participants.
At the end of the two-month intervention, post-test assessments were conducted over the phone. Pretest and post-test assessments took approximately 35 min to complete. Responses were transcribed on hard-copy measure forms by the social worker and transferred onto a compiled anonymous document (which included and Participant ID numbers and general demographic information) to share with the research team.
Results
Analysis plan
This study assessed whether a two-month technology training program would lead to well-being or cognitive changes in low-income older adults. Linear mixed effects models were conducted in R (version 022.12.0.353; Posit Team, 2022) using lme4 package (Bates et al., Citation2015) for each outcome measure of cognition, well-being, loneliness, depression, and growth mindset. These models considered the dependence among repeated measurements (pre- and post-test) for each participant and included fixed effects (‘average participant’) and random effects (the difference between a particular participant and the average participant). The normality assumption for each model was checked, and in cases when the normality assumption was not satisfied, transformations were employed and are indicated in each outcome section below when relevant. For each separate model, the highest level of interaction among predictor variables (gender, age, time, and functional digital independence [how participants rated their use and comfort level with completing various tasks on digital devices]) was used. Variables were then systematically removed using Bayesian Information Criteria (BIC) and performing likelihood ratio tests.
Means and standard errors of each outcome variable for both pre-test and post-test assessments are included in . Results for each outcome measure from the linear mixed-effects models are presented in . For the data reported below, we present the estimated coefficients and significant effects (ɑ = 0.05), and we also discuss any interactions in the models.
Table 2. Mean and SE of the BTACT, PERMA, TILS, PHQ-2, and growth mindset scores for pre-test and post-test.
Table 3. Results of linear mixed-effects models for all outcome measures.
Program adherence
A total of 20 participants completed the pre-test assessment prior to beginning the program, with 19 completing the post-test, a completion rate of 95%. Of the eight scheduled one-to-one meetings for this program (two in-person and six remote Zoom meetings), participants completed an average of approximately 6 meetings (M = 6.93, SD = 1.55, Mdn = 8, range = 3–8).
Cognitive performance (BTACT)
No significant changes were identified from pre-test to post-test mean scores for the cognitive measure.
Well-being (PERMA)
For well-being, no significant improvements were identified from pre-test to post-test. However, functional digital independence scores at pre-test significantly predicted well-being outcomes at post-test, such that as the level of dependency on others increased, well-being scores were estimated to decrease by 3.56 units (p = 0.003, SE = 1.02, 95% CI [-5.73, −1.40]).
Loneliness (TILS)
To satisfy the normality assumption of the linear mixed-effects model, a natural logarithmic transformation was performed on mean loneliness scores. No significant changes or interactions were identified from pre-test to post-test.
Depression (PHQ-2)
To satisfy the normality assumption of the linear mixed-effects model, a natural logarithmic transformation was performed on the mean depression scores. No significant changes in mean depression scores were identified across time (pre- to post-test). The model did reveal a significant interaction between age and digital independence (p = 0.038, SE = −0.01, 95% CI [-5.73, −1.40]), such that between two participants of the same age, the less digitally independent one was expected to have a 1.66 times higher depression score per unit difference in the digital independence score. Similarly, of two participants with the same digital independence score, the older of the two was expected to have a 1.04 times higher depression score for every year of age difference. Interestingly, functional digital independence scores at pre-test had a significant effect on mean depression scores at post-test, such that as independence increases, depression scores were also estimated to increase by 0.52 units (p = 0.034, SE = 0.22, 95% CI [0.05, 0.99]).
Growth mindset
No significant changes were found between mean growth mindset scores measured at pre-test and post-test.
Discussion
This study included a community-based two-month technology training program for low-income older adults. This pilot study assessed feasibility and potential changes in cognitive, well-being, and mindset measures. Demonstrating the feasibility of the program, the vast majority of the participants (95%) were retained from pre-test to post-test and adhered to the program schedule, attending an average of 6 out of the 8 one-to-one weekly training meeting. Results revealed no significant changes across the two-month period for all outcome measures. However, models indicated the potential importance of functional digital independence at pre-test on depression and well-being. This finding aligns with prior work showing that having technology experience and more independence with day-to-day online tasks can benefit feelings of connectedness and increase access to online health and well-being services (e.g. Cheshmehzangi et al., Citation2022). However, this finding should be interpreted with caution, as our sample size was small and there were many factors not considered in this study that could influence mental health and well-being beyond digital technology use (e.g. physical health and activity or social capital, such as support or connection; Choi & DiNitto, Citation2013; Santini et al., Citation2020). Our null results also align with prior technology intervention studies that also found null results from pre-test to post-test (e.g. Zhang et al., Citation2022).
This study demonstrated a proof-of-concept for a new collaboration between a university research team and community leaders. It is important to better understand the relationship between the use of technology and potential cognitive and mental health benefits to develop effective interventions to support and sustain technology engagement in older adults, especially those who do not engage with technology regularly (Van der Wardt et al., Citation2012). While our results did not reveal significant cognitive changes, an important outcome was our minimal attrition, indicating an interest in these types of programs from community members, as well as the feasibility of such programs. Our findings, though limited, support the need to address the digital divide, particularly in underserved, low-income, older adult communities.
There are several limitations to the presented work. Most notably, this was a pilot study working with county collaborators during the peak of the COVID-19 vaccination distributions. The sample size was justifiably small to test for feasibility for both the intervention and the overall collaboration. The null effects may be due to the heterogeneity of the participants and real-world environments and/or the true effects being small. The results also may not be widely generalizable given that the participants were a selective sample. However, this selective sample might be arguably inaccessible to typical research conducted in a lab setting, and therefore, the results may be more generalizable than a lab-based study. The measures were short and could not be comprehensive due to time limits of the social worker and participants’ willingness to participate. Perhaps more comprehensive batteries would have provided measures more sensitive to changes over time (although see Odd et al., Citation2022). Additionally, to minimize participant burden, this study did not collect information, such as educational attainment or other lifestyle factors, which also could have affected cognitive performance (e.g. Livingston et al., Citation2020). Finally, the use of quantitative methods may have been a limitation for the target population, as it was reported anecdotally that participants had a difficult time understanding the wording of the questions and the number scales used for responses. Approaching future programs with a mixed-methods (qualitative and quantitative) approach may be beneficial. The OoA team collected qualitative feedback and progress notes during one-to-one meetings with participants, and we plan to analyze this feedback to potentially gain a better understanding of how participants viewed not only the program, but their own progress and thoughts while learning how to use new technology. These qualitative data may provide a valuable perspective that is often missed with quantitative data collection.
Although the state and county were supportive of the efforts of the project (resulting in significant funding from the state to scale-up the program), county workers expressed the desire for a larger support team to collect more information from participants, as well as provide longer support sessions and additional on-call support for participants. Future research working with community collaborators in a similar fashion could consider incorporating long-term discussions of research team support, in addition to in-house county social workers and IT support. These resources would help alleviate some of the research burden on county personnel, who are extremely busy with other administrative duties. However, putting these resources in place would require more ramp-up time and funding. Another limitation to the present study was the lack of long-term follow-up data. With this particular sample, the Riverside County Office on Aging (OoA) officials discussed the difficulty of retaining participants beyond the two-month period due to caregiver or health-related responsibilities. Refining the program to create more long-term incentives, while reducing the time-burden on county employees should be explored.
As mentioned previously, the Office on Aging and other county programs received additional funding to expand technology training and support for low-income older adult members of the community. Future iterations of this intervention include plans to collect long-term follow-up assessments with larger sample sizes. The results from this study, though limited, offer some promising indications of feasibility for community-based interventions. Overall, this study and the future iterations of the technology training program may provide valuable insights for researchers, community services, and policy makers with the common goal of improving accessibility to computers and mobile devices, training, and support for low-income older adults.
Supplemental Material
Download PDF (773.8 KB)Acknowledgements
We thank the Riverside County Office on Aging for inviting the researchers to advise in the design of the study and providing us the opportunity to share this work. We thank the IT support team with OoA, the social workers who conducted over-the-phone assessments, and all members of the county team who aided in conducting this intervention. We would also like to thank the participants of this intervention. Without any of these parties, this work would not have been possible. We would like to acknowledge the research assistants and interns, namely Mehak Shahzad, who provided proof-reading and edit suggestions in prior versions of this manuscript.
Disclosure statement
The authors report there are no competing interests to declare.
Data availability statement
Data, analytic methods, and study materials will be made available upon request from the corresponding author.
Additional information
Funding
References
- Bates, D., Mächler, M., Bolker, B., Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. https://doi.org/10.18637/jss.v067.i01.
- Butler, J., & Kern, M. L. (2016). The PERMA-Profiler: A brief multidimensional measure of flourishing. International Journal of Wellbeing, 6(3), Article 1–48. https://doi.org/10.5502/ijw.v6i3.526
- Byrne, K. A., & Ghaiumy Anaraky, R. (2022). Identifying racial and rural disparities of cognitive functioning among older adults: The role of social isolation and social technology use. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 77(10), 1779–1790. https://doi.org/10.1093/geronb/gbac055
- Calhoun, D., & Lee, S. B. (2019). Computer usage and cognitive capability of older adults: Analysis of data from the Health and Retirement Study. Educational Gerontology, 45(1), 22–33. https://doi.org/10.1080/03601277.2019.1575026
- Chan, M. Y., Haber, S., Drew, L. M., & Park, D. C. (2016). Training older adults to use tablet computers: Does it enhance cognitive function? The Gerontologist, 56(3), 475–484. https://doi.org/10.1093/geront/gnu057
- Charness, N., & Boot, W. R. (2022). A grand challenge for psychology: Reducing the age-related digital divide. Current Directions in Psychological Science, 31(2), 187–193. https://doi.org/10.1177/09637214211068144
- Cheshmehzangi, A., Zou, T., & Su, Z. (2022). The digital divide impacts on mental health during the COVID-19 pandemic. Brain, Behavior, and Immunity, 101, 211–213. https://doi.org/10.1016/j.bbi.2022.01.009
- Choi, E. Y., Wisniewski, K. M., & Zelinski, E. M. (2021). Information and communication technology use in older adults: A unidirectional or bi-directional association with cognitive function? Computers in Human Behavior, 121, 106813. https://doi.org/10.1016/j.chb.2021.106813
- Choi, N. G., & DiNitto, D. M. (2013). Internet use among older adults: Association with health needs, psychological capital, and social capital. Journal of Medical Internet Research, 15(5), e97. https://doi.org/10.2196/jmir.2333
- Cid, A., Sotelo, R., Leguisamo, M., & Ramírez-Michelena, M. (2020). Tablets for deeply disadvantaged older adults: Challenges in long-term care facilities. International Journal of Human-Computer Studies, 144, 102504. https://doi.org/10.1016/j.ijhcs.2020.102504
- Cotten, S. R., Anderson, W. A., & McCullough, B. M. (2013). Impact of internet use on loneliness and contact with others among older adults: Cross-sectional analysis. Journal of Medical Internet Research, 15(2), e39. https://doi.org/10.2196/jmir.2306
- Czaja, S. J. (2017). The potential role of technology in supporting older adults. Public Policy & Aging Report, 27(2), 44–48. https://doi.org/10.1093/ppar/prx006
- Czaja, S. J., Boot, W. R., Charness, N., Rogers, W. A., & Sharit, J. (2018). Improving social support for older adults through technology: Findings from the PRISM randomized controlled trial. The Gerontologist, 58(3), 467–477. https://doi.org/10.1093/geront/gnw249
- Czaja, S. J., Sharit, J., Lee, C. C., Nair, S. N., Hernández, M. A., Arana, N., & Fu, S. H. (2013). Factors influencing use of an e-health website in a community sample of older adults. Journal of the American Medical Informatics Association : JAMIA, 20(2), 277–284. https://doi.org/10.1136/amiajnl-2012-000876
- Dequanter, S., Fobelets, M., Steenhout, I., Gagnon, M.-P., Bourbonnais, A., Rahimi, S., Buyl, R., & Gorus, E. (2022). Determinants of technology adoption and continued use among cognitively impaired older adults: A qualitative study. BMC Geriatrics, 22(1), 376. https://doi.org/10.1186/s12877-022-03048-w
- Duan-Porter, W., Van Houtven, C. H., Mahanna, E. P., Chapman, J. G., Stechuchak, K. M., Coffman, C. J., & Hastings, S. N. (2018). Internet use and technology-related attitudes of veterans and informal caregivers of veterans. Telemedicine Journal and e-Health : The Official Journal of the American Telemedicine Association, 24(7), 471–480. https://doi.org/10.1089/tmj.2017.0015
- Dweck, C. S. (2006). Mindset: The new psychology of success. Random House.
- Elliot, A. J., Mooney, C. J., Douthit, K. Z., & Lynch, M. F. (2014). Predictors of older adults’ technology use and its relationship to depressive symptoms and well-being. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 69(5), 667–677. https://doi.org/10.1093/geronb/gbt109
- Estacio, E. V., Whittle, R., & Protheroe, J. (2019). The digital divide: Examining socio-demographic factors associated with health literacy, access, and use of internet to seek health information. Journal of Health Psychology, 24(12), 1668–1675. https://doi.org/10.1177/1359105317695429
- Faverio, M. (2022). January 13). Share of those 65 and older who are tech users has grown in the past decade. Pew Research Center. Retrieved February 17, 2023, from https://www.pewresearch.org/fact-tank/2022/01/13/share-of-those-65-and-older-who-are-tech-users-has-grown-in-the-past-decade/#:∼:text=And%2096%25%20of%20those%2050,who%20report%20being%20internet%20users
- Fields, J., Cemballi, A. G., Michalec, C., Uchida, D., Griffiths, K., Cardes, H., Cuellar, J., Chodos, A. H., & Lyles, C. R. (2021). In-home technology training among socially isolated older adults: Findings from the Tech Allies Program. Journal of Applied Gerontology : The Official Journal of the Southern Gerontological Society, 40(5), 489–499. https://doi.org/10.1177/0733464820910028
- Forsman, A. K., Nordmyr, J., Matosevic, T., Park, A.-L., Wahlbeck, K., & McDaid, D. (2018). Promoting mental wellbeing among older people: Technology-based interventions. Health Promotion International, 33(6), 1042–1054. https://doi.org/10.1093/heapro/dax047
- Hall, A. K., Bernhardt, J. M., Dodd, V., & Vollrath, M. W. (2015). The digital health divide: Evaluating online health information access and use among older adults. Health Education & Behavior : The Official Publication of the Society for Public Health Education, 42(2), 202–209. https://doi.org/10.1177/1090198114547815
- Han, S., & Nam, S. I. (2021). Creating supportive environments and enhancing personal perception to bridge the digital divide among older adults. Educational Gerontology, 47(8), 339–352. https://doi.org/10.1080/03601277.2021.1988448
- Heo, J., Chun, S., Lee, S., Lee, K. H., & Kim, J. (2015). Internet use and well-being in older adults. Cyberpsychology, Behavior and Social Networking, 18(5), 268–272. https://doi.org/10.1089/cyber.2014.0549
- Hughes, M. E., Waite, L. J., Hawkley, L. C., & Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. https://doi.org/10.1177/0164027504268574
- Hvalič-Touzery, S., Smole-Orehek, K., & Dolničar, V. (2022). Informal caregivers’ perceptions of self-efficacy and subjective well-being when using telecare in the home environment: A qualitative study. Geriatrics, 7(5), Article 86. https://doi.org/10.3390/geriatrics7050086
- Irizarry, T., Shoemake, J., Nilsen, M. L., Czaja, S., Beach, S., & Dabbs, A. D. (2017). Patient portals as a tool for health care engagement: A mixed-method study of older adults with varying levels of health literacy and prior patient portal use. Journal of Medical Internet Research, 19(3), e7099. https://doi.org/10.2196/jmir.7099
- Kim, Y. K., Ang, S., & Fingerman, K. L. (2023). Older adults’ and family caregivers’ technological arrangements on risk of institutionalization. Work, Aging and Retirement, waad005, 1–6 https://doi.org/10.1093/workar/waad005
- Kobayashi, L. C., Wardle, J., & Wagner, C. v (2015). Internet use, social engagement and health literacy decline during ageing in a longitudinal cohort of older English adults. Journal of Epidemiology and Community Health, 69(3), 278–283. https://doi.org/10.1136/jech-2014-204733
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2003). The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. https://doi.org/10.1097/01.MLR.0000093487.78664.3C
- Laganá, L., & García, J. J. (2013). The mental health impact of computer and internet training on a multi-ethnic sample of community-dwelling older adults: Results of a pilot randomised controlled trial. International Journal of Biomedical Science : IJBS, 9(3), 135–147.
- Lawton, M. P., & Brody, E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9(3), 179–186. https://doi.org/10.1093/geront/9.3_Part_1.179
- Leanos, S., Kürüm, E., Strickland-Hughes, C. M., Ditta, A. S., Nguyen, G., Felix, M., Yum, H., Rebok, G. W., & Wu, R. (2020). The impact of learning multiple real-world skills on cognitive abilities and functional independence in healthy older adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 75(6), 1155–1169. https://doi.org/10.1093/geronb/gbz084
- Li, H. (2015). Informal caregivers’ use of the internet for caregiving information. Social Work in Health Care, 54(6), 532–546. https://doi.org/10.1080/00981389.2015.1045577
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., … Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet commission. Lancet (London, England), 396(10248), 413–446. https://doi.org/10.1016/s0140-6736(20)30367-6
- Mariano, J., Marques, S., Ramos, M. R., & de Vries, H. (2021). Internet use by middle-aged and older adults: Longitudinal relationships with functional ability, social support, and self-perceptions of aging. Psychology and Aging, 36(8), 983–995. https://doi.org/10.1037/pag0000643
- McCloud, R. F., Okechukwu, C. A., Sorensen, G., & Viswanath, K. (2016). Beyond access: Barriers to internet health information seeking among the urban poor. Journal of the American Medical Informatics Association : JAMIA, 23(6), 1053–1059. https://doi.org/10.1093/jamia/ocv204
- Moody, L., Wood, E., Needham, A., Booth, A., Jimenez-Aranda, A., & Tindale, W. (2022). Identifying individual enablers and barriers to the use of digital technology for the self-management of long-term conditions by older adults. Journal of Medical Engineering & Technology, 46(6), 448–461. https://doi.org/10.1080/03091902.2022.2089249
- Odd, K., Boron, J., Alderson, J., Lachman, M., & Turiano, N. (2022). Change in episodic memory and executive functioning predicts mortality risk. Innovation in Aging, 6(Supplement_1), 86–86. https://doi.org/10.1093/geroni/igac059.342
- Pang, C., Collin Wang, Z., McGrenere, J., Leung, R., Dai, J., & Moffatt, K. (2021 Technology adoption and learning preferences for older adults: Evolving perceptions, ongoing challenges, and emerging design opportunities [Paper presentation].Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, 1–13. https://doi.org/10.1145/3411764.3445702
- Pauly, T., Lay, J. C., Kozik, P., Graf, P., Mahmood, A., & Hoppmann, C. A. (2019). Technology, physical activity, loneliness, and cognitive functioning in old age. GeroPsych, 32(3), 111–123. https://doi.org/10.1024/1662-9647/a000208
- Reinwand, D. A., Crutzen, R., & Zank, S. (2018). Online activities among elder informal caregivers: Results from a cross-sectional study. Digital Health, 4, 2055207618779715. https://doi.org/10.1177/2055207618779715
- Rosell, J., Guerra, J., & Bustamante, F. (2022). Internet use of older caregivers and their sociodemographic characteristics. In Q. Gao & J. Zhou (Eds.), Human aspects of IT for the aged population. Design, interaction and technology acceptance (pp. 584–595). Springer International Publishing. https://doi.org/10.1007/978-3-031-05581-2_40
- Santini, Z. I., Jose, P. E., York Cornwell, E., Koyanagi, A., Nielsen, L., Hinrichsen, C., Meilstrup, C., Madsen, K. R., & Koushede, V. (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. The Lancet Public Health, 5(1), e62–e70. https://doi.org/10.1016/s2468-2667(19)30230-0
- Schmidt, M. (1996). Rey auditory verbal learning test: A handbook (p. 1996). Los Angeles, CA: Western Psychological Services.
- Shaffer, K. M., Chow, P. I., Cohn, W. F., Ingersoll, K. S., & Ritterband, L. M. (2018). Informal caregivers’ use of internet-based health resources: An analysis of the Health Information National Trends survey. JMIR Aging, 1(2), e11051. https://doi.org/10.2196/11051
- Shapira, N., Barak, A., & Gal, I. (2007). Promoting older adults’ well-being through Internet training and use. Aging & Mental Health, 11(5), 477–484. https://doi.org/10.1080/13607860601086546
- Slegers, K., Boxtel, M. P. J. V., & Jolles, J. (2009). The efficiency of using everyday technological devices by older adults: The role of cognitive functions. Ageing and Society, 29(2), 309–325. https://doi.org/10.1017/S0144686X08007629
- Torp, S., Hanson, E., Hauge, S., Ulstein, I., & Magnusson, L. (2008). A pilot study of how information and communication technology may contribute to health promotion among elderly spousal carers in Norway. Health & Social Care in the Community, 16(1), 75–85. https://doi.org/10.1111/j.1365-2524.2007.00725.x
- Tun, P. A., & Lachman, M. E. (2006). Telephone assessment of cognitive function in adulthood: The Brief Test of Adult Cognition by Telephone. Age and Ageing, 35(6), 629–632. https://doi.org/10.1093/ageing/afl095
- Van der Wardt, V., Bandelow, S., & Hogervorst, E. (2012). The relationship between cognitive abilities, well-being and use of new technologies in older people. Gerontechnology Journal, 10(4), 333–334. https://doi.org/10.1145/1962300.1962372
- Vaportzis, E., Giatsi Clausen, M., & Gow, A. J. (2017). Older adults perceptions of technology and barriers to interacting with tablet computers: A focus group study. Frontiers in Psychology, 8, 1687. https://doi.org/10.3389/fpsyg.2017.01687
- Vaportzis, E., Martin, M., & Gow, A. J. (2017). A Tablet for Healthy Ageing: The effect of a tablet computer training intervention on cognitive abilities in older adults. The American Journal of Geriatric Psychiatry : official Journal of the American Association for Geriatric Psychiatry, 25(8), 841–851. https://doi.org/10.1016/j.jagp.2016.11.015
- Wang, J., Fu, Y., Lou, V., Tan, S. Y., & Chui, E. (2021). A systematic review of factors influencing attitudes towards and intention to use the long-distance caregiving technologies for older adults. International Journal of Medical Informatics, 153, 104536. https://doi.org/10.1016/j.ijmedinf.2021.104536
- Wechsler, D. (1997). Wechsler Adult Intelligence Scale- Third edition (WAIS-III) [Database record]. APA PsycTests. https://doi.org/10.1037/t49755-000
- Woodward, A. T., Freddolino, P. P., Blaschke-Thompson, C. M., Wishart, D. J., Bakk, L., Kobayashi, R., & Tupper, C. (2011). Technology and Aging Project: Training outcomes and efficacy from a randomized field trial. Ageing International, 36(1), 46–65. https://doi.org/10.1007/s12126-010-9074-z
- Yu, R. P., Ellison, N. B., McCammon, R. J., & Langa, K. M. (2016). Mapping the two levels of digital divide: Internet access and social network site adoption among older adults in the USA. Information, Communication, & Society, 19(10), 1445–1464. https://doi.org/10.1080/1369118X.2015.1109695
- Zhang, S., Boot, W. R., & Charness, N. (2022). Does computer use improve older adults’ cognitive functioning? Evidence from the Personal Reminder Information and Social Management trial. The Gerontologist, 62(7), 1063–1070. https://doi.org/10.1093/geront/gnab188
- Zheng, R., Hicken, B. L., Hill, R. D., Luptak, M., Daniel, C. M., Grant, M., & Rupper, R. (2016). Digital technology and caregiver training for older persons: Cognitive and affective perspectives. Educational Gerontology, 42(8), 540–550. https://doi.org/10.1080/03601277.2016.1161989