Abstract
Objectives
This study aims to investigate the impact of self and partner experiences of loneliness and social isolation on life satisfaction in people with dementia and their spousal carers.
Methods
We used data from 1042 dementia caregiving dyads in the Improving the experience of Dementia and Enhancing Active Life (IDEAL) programme cohort. Loneliness was measured using the six-item De Jong Gierveld loneliness scale and social isolation using the six-item Lubben Social Network Scale. Data were analysed using the Actor-Partner Interdependence Model framework.
Results
Self-rated loneliness was associated with poorer life satisfaction for both people with dementia and carers. The initial partner effects observed between the loneliness of the carer and the life satisfaction of the person with dementia and between social isolation reported by the person with dementia and life satisfaction of the carer were reduced to nonsignificance once the quality of the relationship between them was considered.
Discussion
Experiencing greater loneliness and social isolation is linked with reduced life satisfaction for people with dementia and carers. However, having a positive view of the quality of the relationship between them reduced the impact of loneliness and social isolation on life satisfaction. Findings suggest the need to consider the experiences of both the person with dementia and the carer when investigating the impact of loneliness and social isolation. Individual interventions to mitigate loneliness or isolation may enhance life satisfaction for both partners and not simply the intervention recipient.
Introduction
Internationally loneliness has been identified as a major public health problem by both third sector organisations and local and national governments. A range of different countries, including the UK and United States, have loneliness strategies and charities explicitly targeting loneliness, predominantly, but not exclusively, focused on older people (Prohaska et al., Citation2020). Across strategies and initiatives carers are identified as at high risk of loneliness and social isolation with attendant risks to well-being (Department for Digital, Culture, Media and Sport, Citation2018; National Academies of Sciences, Engineering, and Medicine, Citation2020). Both people with dementia and their carers have been identified as an especially vulnerable group (National Academies of Sciences, Engineering, and Medicine, Citation2020; Victor et al., Citation2021). The current study aims to investigate: (a) the impact of loneliness and social isolation on life satisfaction in a large sample of people with dementia and their spousal or partner carers living in Great Britain and (b) the extent to which each person’s loneliness or social isolation affects the other partner’s life satisfaction.
Loneliness and social isolation are distinct but related concepts (Victor et al., Citation2008). Loneliness describes the discrepancy between expectations of quantity and quality of relationships with the actuality (Perlman & Peplau, Citation1981). Whilst social isolation is characterised as having few social contacts or limited integration of an individual into the wider social environment of family, friends, neighbours and wider community (Victor et al., Citation2008). Loneliness is an evaluative concept which only individuals can assess, while social isolation is characterised as a more objective measure of social connectedness. Loneliness is independently associated with a range of physical and mental health outcomes, including depression (Courtin & Knapp, Citation2017), reduced well-being and life satisfaction (Golden et al., Citation2009; Shankar et al., Citation2015), cardiovascular disease (Courtin & Knapp, Citation2017; Valtorta et al., Citation2016) and mortality (Holt-Lunstad et al., Citation2015). Social isolation is associated with poorer mental health (Courtin & Knapp, Citation2017; Leigh-Hunt et al., Citation2017), reduced life satisfaction and well-being (Golden et al., Citation2009; Shankar et al., Citation2015), increased mortality (Holt-Lunstad et al., Citation2015), and there is mixed evidence supporting it as a potential risk factor for poorer physical health outcomes (Leigh-Hunt et al., Citation2017). Both loneliness and social isolation are potential risk factors for cognitive impairment and dementia (Kuiper et al., Citation2015; Lara et al., Citation2019; Livingston et al., Citation2020). Greater life satisfaction is linked with better health and longevity (Diener & Chan, Citation2011). Besides good social connections and relationships, socio-demographic factors, such as age and educational level, are also important for life satisfaction in older people (Huppert, Citation2009).
There is limited evidence about the experience of loneliness or social isolation from the perspective of people with dementia (Balouch et al., Citation2019; Clare, Wu, Jones, et al., Citation2019; Dyer et al., Citation2020; El Haj et al., Citation2016; Holmén et al., Citation2000; Victor et al., Citation2020) or their carers (Beeson, Citation2003; Beeson et al., Citation2000; Brodaty & Donkin, Citation2009; Clare, Wu, Quinn, et al., Citation2019; Victor et al., Citation2021; Williams, Citation2005). Available evidence suggests that people with dementia experience comparable levels of loneliness to the general population of older people (Victor et al., Citation2020) but increasing social isolation over time (Dyer et al., Citation2020). Carers experience higher levels of loneliness than the general population (Beeson, Citation2003; Victor et al., Citation2021), as well as greater isolation (Brodaty & Donkin, Citation2009). Loneliness and social isolation may have a detrimental influence on the life satisfaction of people with dementia and their family carers (Clare, Wu, Jones, et al., Citation2019; Clare, Wu, Quinn, et al., Citation2019) whilst greater social engagement is associated with higher quality of life in people with dementia (Martyr et al., Citation2018).
A limitation of research focused on loneliness and social isolation in people with dementia and carers is that studies focus on individuals rather than investigating loneliness or social isolation of the caring dyad and how they inter-relate or are linked with life satisfaction. Prior research has demonstrated how carer experiences, such as higher carer stress, perceived social restrictions, and lower caregiving competence, can affect the quality of life of the person with dementia (Quinn et al., Citation2020), and how greater caregiving satisfaction can reduce the feelings of loneliness of a care-recipient (Iecovich, Citation2016). Given that dyads may have a close interpersonal relationship it is plausible that the loneliness or social isolation experienced by one member of the dyad may influence the other partner’s life satisfaction as well as their own.
Few studies have looked directly at the dyadic association between loneliness or social isolation and life satisfaction. Relationship quality influences both loneliness and life satisfaction in dyadic studies (Carr et al., Citation2014; Stokes, Citation2017a), those focused on carers of people with Alzheimer’s disease (Beeson et al., Citation2000) and those comprising older spousal couples (De Jong Gierveld et al., Citation2009). People with dementia are often cared for by people with whom they have a close existing relationship and dementia may change previously established roles, as one of the dyad adopts the role of the ‘carer’ who increasingly has to provide care for the other person (Quinn et al., Citation2009). In this study, we focus on spousal carers. The majority of carers are the spouse or the partner of the person with dementia (Brodaty & Donkin, Citation2009). Between 60% and 70% of carers for people with dementia in the UK are female, although this sex balance changes in the oldest age groups (85 years and over) where older carers are more likely to be male than female (Alzheimer’s Research UK, Citation2015; Carers UK, Citation2019). Women are also more likely to provide care for a longer period of time than men. Some prior dyadic studies of loneliness have found sex differences (Segrin & Burke, Citation2015; Segrin et al., Citation2019) whilst others have not (Stokes, Citation2017b).
Two theoretical propositions may explain these potential inter-relationships and underpin the development of a dyadic approach to understanding loneliness and social isolation. Interdependence theory hypothesises that the behaviour or interactions of individuals in close relationships can affect the other person’s behaviour or outcomes (Rusbult & Van Lange, Citation2003) whilst the theory that loneliness is ‘contagious’ (Cacioppo et al., Citation2009) suggests that loneliness experienced by one person can spread to, or influence, loneliness in others. There is some limited evidence to support this proposition. Studies of middle-aged and older married couples have indicated that loneliness experienced by one member of the couple impacts on the other member’s experience of loneliness (Ayalon et al., Citation2013; Stokes, Citation2017b), sleep quality (Segrin & Burke, Citation2015) and relationship quality (Mund & Johnson, Citation2020; Stokes, Citation2017b). Given the close relationship between people with dementia and spousal carers it is plausible that the experiences of one partner will affect the other: if one partner is socially isolated or lonely this might make the other partner socially isolated or lonely. Understanding dyadic relationships in terms of loneliness and social isolation may be a useful approach to enhancing the life satisfaction of people with dementia and spousal carers.
Dyadic studies have predominantly used the Actor-Partner Interdependence Model (APIM) to examine the influence of a predictor as reported by both partners on their own outcome (actor effect) and that of the other member of the dyad (partner effect). Prior dyadic studies examining loneliness in caregiving dyads have found actor effects of loneliness on life satisfaction (Tough et al., Citation2018) and health-related quality of life (Segrin et al., Citation2019) but no partner effects. The samples in both these studies were small and focused on distinct health conditions and demographic groups, making direct comparison problematic. To our knowledge, there are no dyadic studies that have examined social isolation in dementia caregiving dyads.
In the present study we consider: (a) the impact of self- and partner-reported feelings of loneliness on the life satisfaction of the person with dementia and the carer; (b) the impact of self- and partner-reported experiences of social isolation on the life satisfaction of the person with dementia and the carer.
Methods
Design and methods
Design and sample
We analysed data from people with dementia and carers participating in Time 1 (2014–2016) of the Improving the experience of Dementia and Enhancing Active Life (IDEAL) cohort study (Clare et al., Citation2014). Participants with dementia and their respective carers were recruited through 29 National Health Service (NHS) Clinical Research Network sites throughout England, Scotland, and Wales. The inclusion criteria at time of enrolment were: a clinical diagnosis of dementia (any subtype) in the mild-to-moderate stages as indicated by a Mini-Mental State Examination (MMSE) (Folstein et al., Citation1975) score of 15 or over, and living in the community. Family carers of the person with dementia were approached to take part in the study if the person they cared for had agreed to take part and had nominated them. A ‘carer’ was defined as the main family member or friend providing unpaid practical or emotional support to the person with dementia (Quinn et al., Citation2020). Overall, 1537 people with dementia and 1277 carers, of whom 1042 were spouses or partners, agreed to take part in the IDEAL study. Our analytical sample comprised 1042 caregiving dyads of which there were 1034 opposite sex and eight same sex couples.
Measures
Loneliness
The revised six-item version of the De Jong Gierveld Loneliness Scale (De Jong Gierveld & Tilburg, Citation2006) was used. Total scores range from 0 to 6 with higher scores indicating more severe loneliness (Cronbach’s α = 0.63 for people with dementia and 0.77 for carers). Scores of two or more are indicative of loneliness (Victor et al., Citation2020, Citation2021).
Social isolation
The six-item Lubben Social Network Scale was used to gauge social isolation by measuring perceived social support received by family and friends (Lubben et al., Citation2006). Total scores ranged from 0 to 30. A lower score is indicative of a higher risk of social isolation (Cronbach’s α = 0.79 for people with dementia and 0.83 for carers) with a score of <12 the threshold for socially isolation.
Life satisfaction
The Satisfaction with Life Scale (Diener et al., Citation1985) was used. This comprises five positively worded statements rated on a seven-point scale from ‘strongly disagree’ to ‘strongly agree’. Scores ranged from 5 to 35, with higher scores indicating greater life satisfaction (Cronbach’s α = 0.82 for people with dementia and 0.88 for carers).
Covariates
Demographic information was collected on age, sex, and education, based on the highest qualification achieved. Number of hours spent caregiving per day (caregiving hours), the dementia subtype of the person with dementia and their MMSE score were recorded. Self-rated health for both carers and people with dementia was collected. Current relationship quality was measured using the Positive Affect Index (Bengston & Schrader, Citation1982). Scores range from 5 to 30 with higher scores indicating better relationship quality between the carer and person with dementia (Cronbach’s α = 0.81 for people with dementia and 0.84 for carers). Both the person with dementia and carer self-completed this measure.
Statistical analyses
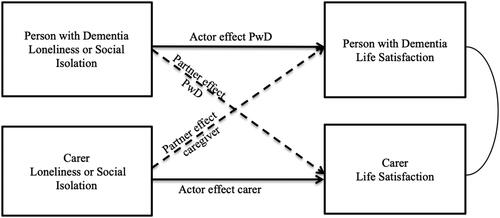
Data were analysed using structural equation modelling. Models estimated actor and partner effects of loneliness and social isolation using the APIM framework (Kenny et al., Citation2006). APIM enabled us to investigate the influence of loneliness or social isolation as reported by both partners on their own life satisfaction and that of the other member of the dyad. The influence of independent variables or predictors (in this case, loneliness or social isolation) on an individual’s own outcomes (life satisfaction) is referred to as the actor effect and the influence of these predictors on the partner’s outcome is known as the partner effect ().
Figure 1. Path diagram of the Actor-Partner Interdependence Model relating to loneliness and social isolation as predictors of life satisfaction for people with dementia and spousal carers.
The first model tested the actor (i.e. own) and partner effects of loneliness and social isolation on life satisfaction. The second model, added socio-demographic characteristics (age, sex and education); the third model added, dementia subtype, MMSE score, self-rated health and caregiving hours and our final model added actor and partner-rated current relationship quality.
To account for missing data, the maximum likelihood with missing values estimation method was applied during dyadic analyses. In over three-quarters of dyads (78%) both the person with dementia and carer completed all measures. Missing values on individual measures are shown in . People with dementia and carers who had missing loneliness and social isolation data did not have any significant differences on socio-demographic measures in comparison to participants with complete data. All data were analysed using Stata 14.2 (StataCorp LP, College Station, TX, USA) and version 7.0 of the IDEAL datasets.
Table 1. Descriptive characteristics of the participants with dementia and carers (N = 1042).
A post hoc analysis was conducted to investigate whether the results differed according to the sex composition of the dyad. The final model was repeated, stratified by sex composition (e.g. whether the dyad comprised a male person with dementia and female carer or a female person with dementia and male carer). Same sex couples were excluded from this analysis because numbers were too small for valid inference (eight same sex couples; seven female and one male).
Results
presents the characteristics of the 1042 spousal/partner dyads who participated in the study. Over half of the people with dementia had a diagnosis of Alzheimer’s disease. The mean age of the people with dementia was 75.0 (SD = 7.8), and mean age of the carers 72.3 (SD = 8.3). A higher proportion of carers were female in comparison to people with dementia (p < .001). The mean loneliness score for the people with dementia was 1.2 (SD = 1.4) points lower (less lonely) than for carers (2.5 SD = 1.9; p < .001). Almost two-thirds of carers experienced loneliness compared with a third of people with dementia (p < .001). Mean social network sizes were 15.6 (SD = 6.2) for people with dementia and 17.7 (SD = 5.5) for carers (p < .001); levels of social isolation were 26.9% for people with dementia and 12.4% for carers, respectively; 96% of dyads had known each other for more than ten years.
Females with dementia had lower MMSE scores on average (p = .004) and lower levels of education (p < .001) in comparison with males. Female carers were more likely to be lonely (p < .001), spend more hours caregiving per day (p = .026), report lower levels of education (p < .001) have poorer relationship quality (p < .001), self-rated health (p = .032), and life satisfaction (p < .001) compared with male carers but no significant differences in social isolation.
Actor and partner effects of loneliness and social isolation on life satisfaction
Results of the dyadic analyses for loneliness, social isolation, and life satisfaction are set out in . Model 1, after adjustment for both actor and partner rated loneliness and social isolation, shows both an actor and partner effect of loneliness on the life satisfaction of people with dementia. For carers, only their own loneliness affected their life satisfaction. There were no actor or partner effects of social isolation on their life satisfaction.
Table 2. Actor and partner effects of loneliness and social isolation on life satisfaction using maximum likelihood to account for missing data (N = 1042 dyads).
Adjustment for socio-demographic factors (Model 2) revealed a weak partner effect between the social isolation of the person with dementia and the life satisfaction of the carer remained. Further adjustment for dementia diagnosis, MMSE score, self-rated health, and caregiving hours (actor and partner) had a more notable impact on the observed associations (Model 3). The strong actor effect of loneliness on the life satisfaction of people with dementia and carers remained as did the partner effect of loneliness on the life satisfaction of the person with dementia and the partner effect of social isolation on the carer’s life satisfaction. Following the addition of actor and partner-rated relationship quality (Model 4) the actor effects of loneliness on life satisfaction were reduced but remained significant, indicating that greater loneliness was linked with poorer life satisfaction for both people with dementia and carers. Both the partner effect of loneliness on the life satisfaction of the person with dementia and the partner effect of social isolation on the life satisfaction of the carer were no longer significant. In the final model, being older, reporting better relationship quality and self-rated health were associated with greater life satisfaction (Supporting Information Table 3). For carers, being female and spending over ten hours per day caregiving were linked with poorer life satisfaction.
Analyses examining the sex composition of dyads
The analysis by sex composition of the dyad revealed similar overall results for loneliness but a notable difference for social isolation (). For both people with dementia and carers loneliness affected their own life satisfaction whether they were male or female. There were no actor effects of social isolation on own life satisfaction for people with dementia or for carers. There was only a partner effect of social isolation on the life satisfaction of the person with dementia in dyads where the carer was male and the person with dementia was female. Supplementary analyses showed that only the interaction of carer’s social isolation and gender composition of dyad was significant (Supporting Information Table 4).
Table 3. Actor and partner effects of loneliness and social isolation on life satisfaction stratified by sex composition of dyad (n = 1034)Table Footnotea.
Discussion
To the best of our knowledge, this is the first study to use an actor-partner interdependence model to investigate the impact of loneliness or social isolation on life satisfaction in dementia caregiving dyads. This study enhances our understanding of loneliness and isolation for these specific populations, by investigating the interdependency between loneliness, social isolation, and life satisfaction. People with dementia had a higher prevalence of social isolation in comparison with carers, whilst carers reported greater feelings of loneliness in comparison to the people with dementia, confirming previous IDEAL findings (Victor et al., Citation2020, Citation2021). The higher prevalence of social isolation amongst people with dementia may reflect loss of or reduction in connection with others following a diagnosis of dementia whilst higher levels of loneliness in carers may reflect the impact of the caregiving role and change in the relationship between partners (Vasileiou et al., Citation2017). Factors relating to the caregiving role, such as caregiving stress, have previously been shown to be associated with greater loneliness (Victor et al., Citation2021).
There were strong actor effects of loneliness on life satisfaction for both people with dementia and their carers, with feeling lonely associated with reduced life satisfaction. Our hypotheses that there were partner effects of loneliness on life satisfaction was not upheld once social isolation and covariates were accounted for. This accords with previous research exploring actor and partner effects of loneliness in caregiving-care recipient dyads for people with breast cancer or spinal cord injury (Segrin et al., Citation2019; Tough et al., Citation2018). Our finding that greater loneliness was linked with poorer life satisfaction among people with dementia and spousal carers is consistent with existing evidence for older adults (Golden et al., Citation2009; Shankar et al., Citation2015). In contrast to previous studies of middle-aged and older couples (Ayalon et al., Citation2013; Segrin & Burke, Citation2015; Stokes, Citation2017b), there was no strong evidence to support the proposition that loneliness is contagious and can spread from one person to another (Cacioppo et al., Citation2009).
Our initial analysis suggested that social isolation experienced by the person with dementia had an impact on their carers’ life satisfaction. However, this finding was reduced to nonsignificance once we accounted for relationship quality. Thus, the quality of the relationship between the two individuals plays a key role in mitigating social isolation. The quality of the relationship between the person with dementia and the carer also explained some of the actor effects of loneliness on life satisfaction and the initial partner effect of the loneliness experienced by the carer on the life satisfaction of the person with dementia. Prior studies of older adults have demonstrated that closeness with a partner or family member is an important predictor of both life satisfaction and loneliness (Carr et al., Citation2014; Shiovitz-Ezra & Leitsch, Citation2010; Yang, Citation2018). The closer a person was to their spouse or partner the more this was protective against loneliness over time. Consequently, we might be able to increase the life satisfaction of people with dementia and carers by finding strategies or sources of support to enhance relationship quality and alleviate or prevent the impact of social isolation or loneliness. These finding offer limited support for interdependence theory (Rusbult & Van Lange, Citation2003) where the experience or interactions of one partner may affect their partner’s behavior. Interventions that help people with dementia to remain connected with the community or to have more social contact may help to reduce social isolation and in turn help to increase their life satisfaction and that of their carers also.
The present study indicated that the sex of the carer and person with dementia may have a potential role in the development of loneliness and social isolation. The descriptive analysis indicated that whilst female carers reported greater loneliness, poorer self-rated health and lower life satisfaction in comparison with male carers there were no significant differences in terms of social isolation. This partly accords with findings from a meta-analysis which found small differences in relation to health, depression and well-being but no sex differences in relation to social support (Pinquart & Sörensen, Citation2006). Our analysis that was stratified for sex composition of the dyad found only significant partner effects for social isolation on life satisfaction in dyads where the person with dementia was female and the carer was male. There are no comparable studies reporting life satisfaction in dementia caregiving dyads and findings for previous studies have been mixed. Further research is needed to establish the veracity of our findings and to understand the reasons for these differences. We might hypothesise that increase in isolation in male-female caregiving dyads may reflect the impact of gendered roles in maintaining social networks with family, friends and the wider community (Neri et al., Citation2012; Willis et al., Citation2020). It is plausible that better support is needed to help male carers adapt to the change in the balance of their relationship with the person with dementia.
A key strength of the present study is the use of a large sample of people with dementia and their carers. To the best of our knowledge it is the first study to examine the dyadic relationship between loneliness, social isolation and life satisfaction in people with dementia and their carers using a novel analytical method to evaluate the interdependence of loneliness and social isolation in caregiving dyads. However, our study has limitations that need to be considered. First, the current study is based on cross-sectional analyses, therefore, it is not possible to say with certainty whether or not loneliness or social isolation leads to poorer life satisfaction. However, it presents an important initial step in examining these dyadic relationships. As the IDEAL programme is longitudinal it will be possible to identify and observe any actor or partner effects of loneliness and social isolation on life satisfaction for dyads who remain in the study. Second, the sample comprises people with mild-to-moderate dementia and there may be changes to perceived quality of social relationships over time and in the number of social contacts as dementia progresses (Dyer et al., Citation2020). The study found that greater dementia severity was associated with greater decline in social network size longitudinally. Further as the sample comprised almost entirely heterosexual couples we were not able to consider any differences for same-sex couples in our analysis of the sex composition of dyads. Prior dyadic studies have suggested that there may be more concordance between gay and lesbian couples than heterosexual couples on indicators such as health and health behaviours and that this may reflect differences in relationship dynamics (Holway et al., Citation2018). Finally, we were unable to identify the amount of support the dyad received from other family members or friends. Wider support and help received from others could have implications for social contact with others and may affect the quality of the relationship between the person with dementia and carer.
The findings in the present study suggest that people with dementia have higher levels of social isolation in comparison with their carers. This could indicate that they are less socially integrated, and interventions could consider ways to keep people with mild-to-moderate dementia more socially involved. Carers, whilst reporting lower levels of isolation, have much higher levels of loneliness, and this has implications for the support received. Based on the findings of the present study, support and potential interventions should be developed in the context of dyadic caregiving relationships. Enhancing social connections may help to reduce social isolation and improve the life satisfaction of both dyadic partners. This study has indicated that further consideration of the dyadic relationship is of importance and interventions should consider the experiences of both people with dementia and their carers.
Ethical standards
The IDEAL study was approved by the Wales Research Ethics Committee 5 (reference 13/WA/0405) and the Ethics Committee of the School of Psychology, Bangor University (reference 2014-11684). The IDEAL study is registered with UKCRN, registration number 16593.
Authors’ contributions
I. Rippon is responsible for the data analysis and interpretation and for drafting the article. C.R. Victor contributed to the design of the current analysis. F.E. Matthews advised on the data analysis. C.R. Victor, A. Martyr, F.E. Matthews, C. Quinn, J.M.Rusted, R.W. Jones and L. Clare were involved in the original conception and design of the IDEAL programme. All authors contributed to the critical revision of the article and approved the final version.
Supplemental Material
Download MS Word (60.8 KB)Acknowledgements
We would like to acknowledge the support of the following research networks: NIHR Dementias and Neurodegeneration Specialty (DeNDRoN) in England, the Scottish Dementia Clinical Research Network (SDCRN), and Health and Care Research Wales. We gratefully acknowledge the local principal investigators and researchers involved in participant recruitment and assessment within these networks. We are grateful to the IDEAL study participants for their participation in the study and to members of the ALWAYs group and the Project Advisory Group for their support throughout the study. We would also like to thank Laura D. Gamble for statistical advice. L. Clare and L. Allan acknowledge support from the NIHR Applied Research Collaboration South-West Peninsula. L. Allan also acknowledges support from the Exeter NIHR Biomedical Research Centre.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
IDEAL data were deposited with the UK data archive in April 2020. Details of how to access the data can be found here: http://reshare.ukdataservice.ac.uk/854293/.
Additional information
Funding
References
- Alzheimer’s Research UK. (2015). Women and dementia: A marginalised majority. Alzheimer’s Research UK. https://www.alzheimersresearchuk.org/wp-content/uploads/2015/03/Women-and-Dementia-A-Marginalised-Majority1.pdf
- Ayalon, L., Shiovitz-Ezra, S., & Palgi, Y. (2013). Associations of loneliness in older married men and women. Aging & Mental Health, 17(1), 33–39. https://doi.org/10.1080/13607863.2012.702725
- Balouch, S., Rifaat, E., Chen, H. L., & Tabet, N. (2019). Social networks and loneliness in people with Alzheimer’s dementia. International Journal of Geriatric Psychiatry, 34(5), 666–673. https://doi.org/10.1002/gps.5065
- Beeson, R. (2003). Loneliness and depression in spousal caregivers of those with Alzheimer’s disease versus non-caregiving spouses. Archives of Psychiatric Nursing, 17(3), 135–143. https://doi.org/10.1016/S0883-9417(03)00057-8
- Beeson, R., Horton-Deutsch, S., Farran, C., & Neundorfer, M. (2000). Loneliness and depression in caregivers of persons with Alzheimer’s disease or related disorders. Issues in Mental Health Nursing, 21(8), 779–806. https://doi.org/10.1080/016128400750044279
- Bengston, V. L., & Schrader, S. S. (1982). Parent-child relationship. In D. J. Mangon & W. A. Peterson (Eds.), Research instruments in social gerontology: Social roles and social participation (Vol. 2, pp. 115–185). University of Minnesota Press.
- Brodaty, H., & Donkin, M. (2009). Family caregivers of people with dementia. Dialogues in Clinical Neuroscience, 11(2), 217–228. https://doi.org/10.31887/DCNS.2009.11.2/hbrodaty
- Cacioppo, J. T., Fowler, J. H., & Christakis, N. A. (2009). Alone in the crowd: The structure and spread of loneliness in a large social network. Journal of Personality and Social Psychology, 97(6), 977–991. https://doi.org/10.1037/a0016076
- Carers UK. (2019). Facts about carers. Carers UK. https://www.carersuk.org/for-professionals/policy/policy-library/facts-about-carers-2019
- Carr, D., Freedman, V. A., Cornman, J. C., & Schwarz, N. (2014). Happy marriage, happy life? Marital quality and subjective well-being in later life. Journal of Marriage and the Family, 76(5), 930–948. https://doi.org/10.1111/jomf.12133
- Clare, L., Nelis, S. M., Quinn, C., Martyr, A., Henderson, C., Hindle, J. V., Jones, I. R., Jones, R. W., Knapp, M., Kopelman, M. D., Morris, R. G., Pickett, J. A., Rusted, J. M., Savitch, N. M., Thom, J. M., & Victor, C. R. (2014). Improving the experience of dementia and enhancing active life - living well with dementia: Study protocol for the IDEAL study. Health and Quality of Life Outcomes, 12(1), 164. https://doi.org/10.1186/s12955-014-0164-6
- Clare, L., Wu, Y.-T., Jones, I. R., Victor, C. R., Nelis, S. M., Martyr, A., Quinn, C., Litherland, R., Pickett, J. A., Hindle, J. V., Jones, R. W., Knapp, M., Kopelman, M. D., Morris, R. G., Rusted, J. M., Thom, J. M., Lamont, R. A., Henderson, C., Rippon, I., . . . IDEAL Study Team. (2019). A comprehensive model of factors associated with subjective perceptions of “living well” with dementia: Findings from the IDEAL study. Alzheimer Disease and Associated Disorders, 33(1), 36–41. https://doi.org/10.1097/WAD.0000000000000286
- Clare, L., Wu, Y.-T., Quinn, C., Jones, I. R., Victor, C. R., Nelis, S. M., Martyr, A., Litherland, R., Pickett, J. A., Hindle, J. V., Jones, R. W., Knapp, M., Kopelman, M. D., Morris, R. G., Rusted, J. M., Thom, J. M., Lamont, R. A., Henderson, C., Rippon, I., . . . IDEAL Study Team. (2019). A comprehensive model of factors associated with capability to “live well” for family caregivers of people living with mild-to-moderate dementia: Findings from the IDEAL study. Alzheimer Disease and Associated Disorders, 33(1), 29–35. https://doi.org/10.1097/WAD.0000000000000285
- Courtin, E., & Knapp, M. (2017). Social isolation, loneliness and health in old age: A scoping review. Health & Social Care in the Community, 25(3), 799–812. https://doi.org/10.1111/hsc.12311
- De Jong Gierveld, J., & Tilburg, T. V. (2006). A 6-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Research on Aging, 28(5), 582–598. https://doi.org/10.1177/0164027506289723
- De Jong Gierveld, J., van Groenou, M. B., Hoogendoorn, A. W., & Smit, J. H. (2009). Quality of marriages in later life and emotional and social loneliness. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 64(4), 497–506. https://doi.org/10.1093/geronb/gbn043
- Department for Digital, Culture, Media and Sport. (2018). A connected society: A strategy for tackling loneliness – laying the foundations for change. Department for Digital, Culture, Media and Sport. https://www.gov.uk/government/publications/a-connected-society-a-strategy-for-tackling-loneliness
- Diener, E., & Chan, M. Y. (2011). Happy people live longer: Subjective well-being contributes to health and longevity. Applied Psychology: Health and Well-Being, 3(1), 1–43. https://doi.org/10.1111/j.1758-0854.2010.01045.x
- Diener, E., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. https://doi.org/10.1207/s15327752jpa4901_13
- Dyer, A. H., Murphy, C., Lawlor, B., Kennelly, S. P., & For The NILVAD Study Group. (2020). Social networks in mild-to-moderate Alzheimer disease: Longitudinal relationships with dementia severity, cognitive function, and adverse events. Aging & Mental Health, 25(10), 1923–1929. https://doi.org/10.1080/13607863.2020.1745146
- El Haj, M., Jardri, R., Larøi, F., & Antoine, P. (2016). Hallucinations, loneliness, and social isolation in Alzheimer’s disease. Cognitive Neuropsychiatry, 21(1), 1–13. https://doi.org/10.1080/13546805.2015.1121139
- Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. https://doi.org/10.1016/0022-3956(75)90026-6
- Golden, J., Conroy, R. M., Bruce, I., Denihan, A., Greene, E., Kirby, M., & Lawlor, B. A. (2009). Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. International Journal of Geriatric Psychiatry, 24(7), 694–700. https://doi.org/10.1002/gps.2181
- Holmén, K., Ericsson, K., & Winblad, B. (2000). Social and emotional loneliness among non-demented and demented elderly people. Archives of Gerontology and Geriatrics, 31(3), 177–192. https://doi.org/10.1016/S0167-4943(00)00070-4
- Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science: A Journal of the Association for Psychological Science, 10(2), 227–237. https://doi.org/10.1177/1745691614568352
- Holway, G. V., Umberson, D., & Donnelly, R. (2018). Health and health behavior concordance between spouses in same-sex and different-sex marriages. Social Currents, 5(4), 319–327. https://doi.org/10.1177/2329496517734570
- Huppert, F. A. (2009). Psychological well-being: Evidence regarding its causes and consequences. Applied Psychology: Health and Well-Being, 1(2), 137–164. https://doi.org/10.1111/j.1758-0854.2009.01008.x
- Iecovich, E. (2016). Do caregiving burden and satisfaction predict loneliness in older care recipients? Aging & Mental Health, 20(4), 441–449. https://doi.org/10.1080/13607863.2015.1020413
- Kenny, D. A., Kashy, D. A., & Cook, W. L. (2006). Dyadic data analysis. Guildford Publications.
- Kuiper, J. S., Zuidersma, M., Oude Voshaar, R. C., Zuidema, S. U., van den Heuvel, E. R., Stolk, R. P., & Smidt, N. (2015). Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Research Reviews, 22, 39–57. https://doi.org/10.1016/j.arr.2015.04.006
- Lara, E., Martín-María, N., De la Torre-Luque, A., Koyanagi, A., Vancampfort, D., Izquierdo, A., & Miret, M. (2019). Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Research Reviews, 52, 7–16. https://doi.org/10.1016/j.arr.2019.03.002
- Leigh-Hunt, N., Bagguley, D., Bash, K., Turner, V., Turnbull, S., Valtorta, N., & Caan, W. (2017). An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health, 152, 157–171. https://doi.org/10.1016/j.puhe.2017.07.035
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., … Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet (London, England), 396(10248), 413–446. https://doi.org/10.1016/S0140-6736(20)30367-6
- Lubben, J., Blozik, E., Gillmann, G., Iliffe, S., Kruse, W., von, R., Beck, J. C., & Stuck, A. E. (2006). Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. The Gerontologist, 46(4), 503–513. https://doi.org/10.1093/geront/46.4.503
- Martyr, A., Nelis, S. M., Quinn, C., Wu, Y.-T., Lamont, R. A., Henderson, C., Clarke, R., Hindle, J. V., Thom, J. M., Jones, I. R., Morris, R. G., Rusted, J. M., Victor, C. R., & Clare, L. (2018). Living well with dementia: A systematic review and correlational meta-analysis of factors associated with quality of life, well-being and life satisfaction in people with dementia. Psychological Medicine, 48(13), 2130–2139. https://doi.org/10.1017/S0033291718000405
- Mund, M., & Johnson, M. D. (2020). Lonely me, lonely you: Loneliness and the longitudinal course of relationship satisfaction. Journal of Happiness Studies, 22(2), 575–597. https://doi.org/10.1007/s10902-020-00241-9
- National Academies of Sciences, Engineering, and Medicine. (2020). Social isolation and loneliness in older adults: Opportunities for the health care system. The National Academies Press. https://doi.org/10.17226/25663
- Neri, A. L., Yassuda, M. S., Fortes-Burgos, A. C. G., Mantovani, E. P., Arbex, F. S., de Souza Torres, S. V., Perracini, M. R., & Guariento, M. E. (2012). Relationships between gender, age, family conditions, physical and mental health, and social isolation of elderly caregivers. International Psychogeriatrics, 24(3), 472–483. https://doi.org/10.1017/S1041610211001700
- Perlman, D., & Peplau, L. A. (1981). Toward a social psychology of loneliness. In S. Duck & R. Gilmour (Eds.), Personal relationships. 3: Personal relationships in disorder (pp. 31–56). Academic Press.
- Pinquart, M., & Sörensen, S. (2006). Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 61(1), P33–45. https://doi.org/10.1093/geronb/61.1.p33
- Prohaska, T., Burholt, V., Burns, A., Golden, J., Hawkley, L., Lawlor, B., Leavey, G., Lubben, J., O’Sullivan, R., Perissinotto, C., van Tilburg, T., Tully, M., Victor, C., & Fried, L. (2020). Consensus statement: Loneliness in older adults, the 21st century social determinant of health? BMJ Open, 10(8), e034967. https://doi.org/10.1136/bmjopen-2019-034967
- Quinn, C., Clare, L., & Woods, B. (2009). The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: A systematic review. Aging & Mental Health, 13(2), 143–154. https://doi.org/10.1080/13607860802459799
- Quinn, C., Nelis, S. M., Martyr, A., Morris, R. G., Victor, C., & Clare, L. (2020). Caregiver influences on ‘living well’ for people with dementia: Findings from the IDEAL study. Aging & Mental Health, 24(9), 1505–1513. https://doi.org/10.1080/13607863.2019.1602590
- Rusbult, C. E., & Van Lange, P. A. M. (2003). Interdependence, interaction, and relationships. Annual Review of Psychology, 54(1), 351–375. https://doi.org/10.1146/annurev.psych.54.101601.145059
- Segrin, C., Badger, T. A., & Sikorskii, A. (2019). A dyadic analysis of loneliness and health-related quality of life in Latinas with breast cancer and their informal caregivers. Journal of Psychosocial Oncology, 37(2), 213–227. https://doi.org/10.1080/07347332.2018.1520778
- Segrin, C., & Burke, T. J. (2015). Loneliness and sleep quality: Dyadic effects and stress effects. Behavioral Sleep Medicine, 13(3), 241–254. https://doi.org/10.1080/15402002.2013.860897
- Shankar, A., Rafnsson, S. B., & Steptoe, A. (2015). Longitudinal associations between social connections and subjective wellbeing in the English Longitudinal Study of Ageing. Psychology & Health, 30(6), 686–698. https://doi.org/10.1080/08870446.2014.979823
- Shiovitz-Ezra, S., & Leitsch, S. A. (2010). The role of social relationships in predicting loneliness: The National Social Life, Health, and Aging Project. Social Work Research, 34(3), 157–167. https://doi.org/10.1093/swr/34.3.157
- Stokes, J. E. (2017a). Marital quality and loneliness in later life: A dyadic analysis of older married couples in Ireland. Journal of Social and Personal Relationships, 34(1), 114–135. https://doi.org/10.1177/0265407515626309
- Stokes, J. E. (2017b). Two-wave dyadic analysis of marital quality and loneliness in later life: Results from the Irish Longitudinal Study on Ageing. Research on Aging, 39(5), 635–656. https://doi.org/10.1177/0164027515624224
- Tough, H., Brinkhof, M. W. G., Siegrist, J., & Fekete, C. (2018). The impact of loneliness and relationship quality on life satisfaction: A longitudinal dyadic analysis in persons with physical disabilities and their partners. Journal of Psychosomatic Research, 110, 61–67. https://doi.org/10.1016/j.jpsychores.2018.04.009
- Valtorta, N. K., Kanaan, M., Gilbody, S., Ronzi, S., & Hanratty, B. (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart (British Cardiac Society), 102(13), 1009–1016. https://doi.org/10.1136/heartjnl-2015-308790
- Vasileiou, K., Barnett, J., Barreto, M., Vines, J., Atkinson, M., Lawson, S., & Wilson, M. (2017). Experiences of loneliness associated with being an informal caregiver: A qualitative investigation. Frontiers in Psychology, 8, 585. https://doi.org/10.3389/fpsyg.2017.00585
- Victor, C. R., Bond, J., & Scambler, S. (2008). The social world of older people: Understanding loneliness and social isolation in later life. Open University Press.
- Victor, C. R., Rippon, I., Nelis, S. M., Martyr, A., Litherland, R., Pickett, J., Hart, N., Henley, J., Matthews, F., Clare, L., & IDEAL Programme Team. (2020). Prevalence and determinants of loneliness in people living with dementia: Findings from the IDEAL programme. International Journal of Geriatric Psychiatry, 35(8), 851–858. https://doi.org/10.1002/gps.5305
- Victor, C. R., Rippon, I., Quinn, C., Nelis, S. M., Martyr, A., Hart, N., Lamont, R., & Clare, L. (2021). The prevalence and predictors of loneliness in caregivers of people with dementia: Findings from the IDEAL programme. Aging & Mental Health, 25(7), 1232–1238. https://doi.org/10.1080/13607863.2020.1753014
- Williams, I. C. (2005). Emotional health of black and white dementia caregivers: A contextual examination. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 60(6), P287–P295. https://doi.org/10.1093/geronb/60.6.P287
- Willis, P., Vickery, A., & Symonds, J. (2020). “You have got to get off your backside; otherwise, you’ll never get out”: Older male carers’ experiences of loneliness and social isolation. International Journal of Care and Caring, 4(3), 311–330. https://doi.org/10.1332/239788220X15912928956778
- Yang, K. (2018). Longitudinal loneliness and its risk factors among older people in England. Canadian Journal on Aging = La Revue Canadienne du Vieillissement, 37(1), 12–21. https://doi.org/10.1017/S0714980817000526
