Abstract
Objectives: Our purpose was to study whether there is a difference in self-rated health-related quality of life (HRQOL) and changes in HRQOL perception after 3 months of hormonal contraceptive use in adolescents. Seasonal variations in symptoms of depression were also studied.
Methods: A test group (T1) (n = 193) and a selected control group (n = 238) of women aged 14–20 years who were visiting a young person’s clinic completed the 36-item short-form health survey (SF-36) and answered additional questions on menstrual history and pattern, need for menstrual pain relief medication, and other regular medication. The test group was reassessed after 3 months of hormonal contraception (T2). Seasonal variations in reported SF-36 scores were studied for the whole group.
Results: The selected control group and test group at T1 were similar with regard to age at menarche and menstrual pattern. The duration of bleeding and use of painkillers were significantly reduced and the impact on everyday life was significantly improved after 3 months of hormonal contraception (p = .000, two-tailed). No changes in HRQOL or symptoms of possible depression were found after 3 months of hormonal contraception. The highest prevalence odds ratio for possible depression (SF-36 mental health scale score ≤48), adjusted for group, season and age, for spring vs winter, was 2.15 (95% confidence interval 0.95, 4.85).
Conclusions: After 3 months of hormonal contraception both the number of days of menstrual bleeding and the use of medication to relieve menstrual pain were reduced, but there were no significant changes in self-rated HRQOL perception. Seasonal effects on HRQOL were reported.
摘要
目的:我们的目的是研究青少年自我评定的健康相关生活质量(HRQOL)量表有无差异, 以及服用3个月激素避孕药后HRQOL量表有无变化, 还研究了抑郁症状的季节性变化。
方法:实验组(T1)(n = 193)和选定的对照组(n = 238), 在一家青年诊所就诊的年龄14-20岁的年轻女性完成36项简要格式的健康调查(SF-36), 并且回答了月经史和月经模式, 需要药物缓解痛经以及其他的规律服药情况。实验组服用3个月激素避孕药后(T2)重新评估。研究了整组SF-36评分的季节变化。
结果:选定的对照组和实验组T1关于初潮年龄和月经模式是相似的。服用3个月激素避孕药后月经出血时间和止痛药的应用明显减少, 并且明显提高每天的生活质量(p = 0.000, 双侧检验)。服用3个月激素避孕药后HRQOL和可能的抑郁症状没有改变。校正组、季节和年龄, 校正春天vs.冬天后, 可能的抑郁症(SF-36心理健康量表得分≤48)最高患病率比值比为2.15(95%可信区间0.95, 4.85)。
结论:服用3个月激素避孕药后月经出血时间和缓解痛经药物的应用减少, 但自我评定的HRQOL没有明显改变, 报告了季节对HRQOL的影响。
Introduction
The combined oral contraceptive (COC) pill is the most commonly used contraceptive method among young women in Sweden. It is an effective means of preventing pregnancy and achieving good cycle control [Citation1]. An extensive body of evidence has established that oral contraceptives protect women against somatic conditions that may affect their quality of life: dysmenorrhoea, menorrhagia, menstrual cycle irregularities, iron deficiency anaemia, ectopic pregnancy, pelvic inflammatory disease, ovarian cysts, benign breast disease, endometrial cancer and ovarian cancer. Oral contraceptives can also be an effective treatment for moderate acne vulgaris [Citation2].
However, certain side effects of hormonal contraception, such as breakthrough bleeding and changes in sexual function, which can adversely affect a woman's quality of life [Citation3,Citation4], and the occurrence of depressive symptoms, irritability and mood swings may be reasons for discontinuing or switching treatment [Citation5]. It has been suggested that the side effects on mood depend on the relationship between the estrogen and progestin, and on the type of progestin used [Citation6,Citation7]. It has also been suggested that side effects on mood are mostly confined to women with a history of mental symptoms such as those with premenstrual syndrome [Citation8].
The self-scoring 36-item short-form health survey (SF-36) [Citation9], a patient-reported health outcomes measure, is a modern health-related quality-of-life (HRQOL) instrument measuring biological, psychological and social functioning, developed to reflect the World Health Organization’s definition of health: ‘a state of a complete physical, mental and social well-being and not merely the absence of disease or infirmity’ [Citation10].
In our previous research of female adolescents attending a young person’s health centre (YHC) [Citation11], we found that the scores on the SF-36 scales of mental health and vitality significantly correlated with those of the self-rated Montgomery–Åsberg Depression Rating Scale (MADRS-S) [Citation12], indicating that the SF-36 could be used to detect possible depressive disorder in this group. Further, the group showed seasonal variations in reported health and depressive symptoms: in the dark winter months there were more symptoms and a significantly greater proportion of participants with suspected depression [Citation13].
Despite the large number of adolescents worldwide who use hormonal contraception, there are to our knowledge few published studies examining the possible relationship between use of hormonal contraception in young women and perception of HRQOL and occurrence of depressive symptoms [Citation14]. This study addressed these questions as well as the possible impact of seasonality on mood in a group of adolescent women attending a YHC.
Methods
We carried out a longitudinal study on the use of hormonal contraception, including a cross-sectional cohort study to examine the seasonal effect of on mood in the whole group.
Setting
The study was conducted at a YHC at the university hospital of Uppsala, a Swedish city with over 200,000 inhabitants. The aim of the YHC is to prevent unwanted pregnancies, provide sexual and reproductive health care counselling, prevent and treat sexually transmitted infections, and provide guidance on sexual and lifestyle issues for the age group 13–20 years. The YHC complies with the policy programme of The Swedish Society for Youth Centres [Citation15]. The study was approved by the Independent Research Ethics Committee at Uppsala University.
There were 8500 registered visits to the YHC during the 1 year study period, 3100 of which were midwife visits. The total number of 13- to 20-year-old women registered in the Uppsala municipality in the 12 months between August 2014 and July 2015 was approximately 8400, which means that approximately 37% of that age group visited the YHC during the year the research material was collected.
Participants and study design
A convenience sample of 431 young women aged 14–20 years who were visiting the YHC either to request hormonal contraception or for other reasons was randomly recruited by written and oral invitation from the midwives, at their convenience. Two groups were studied: a test group (T1), followed up at 3 months (T2), and a selected control group. The T2 appointment was decided at the T1 visit. The intention of having a selected control group was to investigate whether the test group diverged in any significant way from the selected control group (i.e., a group of young women visiting the centre at the same time) in regard to the factors studied. Both groups were initially not using hormonal contraception. Those who had previously been on the pill and wanted to start again (after an interval of at least 2 months), and were not presently using hormonal contraception, could be included in the test group. Eligible participants for the test group who sought reproductive health care and obtained a prescription for hormonal contraception (e.g., pill, patch, ring, injection or levonorgestrel-releasing intrauterine system [LNG-IUS]) were randomly chosen from the appointments list by the midwife. The number of individuals who did not want to take part in the study was not registered, but common reasons given not to participate were lack of time or interest.
Data collection took place over a period of 1 year, from autumn 2014 to autumn 2015. After receiving verbal and written information and giving their consent, participants completed the Swedish version of the SF-36 [Citation16] and answered questions on the following: age, first visit to the YHC, age at menarche, regular or irregular bleeding pattern, duration of menstruation, need for painkillers during menstruation, and regular medication use. All participants met with a registered midwife who provided standard contraception counselling followed by advice or prescription of a contraceptive method. None in the test group was referred to a gynaecologist to get a prescription for hormonal contraception.
HRQOL measurement
The self-scoring SF-36 was used to investigate whether there was a difference at baseline in HRQOL perception between the test group at T1 and the selected control group. The SF-36 consists of 36 items, grouped into eight scales: (1) physical functioning (PF), (2) role limitations due to physical health (RP), (3) bodily pain (BP), (4) general health perceptions (GH), (5) vitality (VT), (6) social functioning (SF), (7) role limitations due to emotional problems (RE), and (8) mental health (MH). A high score indicates better health (0–100). The scales are sensitive to influences from both medical and psychiatric disorders and have good reliability and validity [Citation17]. The questionnaire has been standardised for use in the Swedish population of aged 15 and above, but can be used from the age of 14 years [Citation16].
In our previous report [Citation11], the coefficient of internal consistency (Cronbach’s alpha) for the eight scales of the SF-36 was between 0.80 and 0.84. There was also a strong correlation between the MADRS-S scores and all the SF-36 scale scores, especially MH and VT, indicating that the SF-36 questionnaire might be useful when screening for suspected depression in a population of young people [Citation11].
In order to study possible seasonal variations in reported SF-36 scores, especially for MH and VT, we used the results from the whole group and presented them by category of season.
Statistical analysis
Means and standard deviations (SDs) of all variables used were calculated. Associations between variables were investigated using Pearson’s correlation coefficients. Differences between categorical variables were examined using Fisher’s exact test and the Mann–Whitney U-test. A change in proportions in dependent groups was examined using McNemar’s test. The difference between groups for continuous variables was measured using the independent or paired sample t-test and Friedman’s non-parametric test for dependent groups. Logistic regression models were used to assess associations between dichotomous outcomes and group variables. Univariate models and models adjusted for the seasons and age were estimated. Models are presented as odds ratios (ORs) with 95% confidence intervals (CIs). A p ≤0.05 was considered statistically significant. The statistical analyses were performed using SAS, version 9.4 (SAS Institute, Cary, NC, USA).
Results
A total of 431 young women participated in the study. Fourteen were excluded from the analysis because they had not correctly completed the questionnaires (e.g., they had only written their names and nothing else or had only answered the background questions and not the SF-36 questionnaire). It was not possible to see whether they differed in any way from the rest of the participants. At T2, 14% of the test group did not renew their prescription. The reasons for this are not known, but these participants did not differ significantly from the rest of the T1 test group with regard to any of the baseline variables.
Baseline characteristics
The baseline characteristics of the groups are shown in : whole group (N = 431), test group at T1 (n = 193) and selected control group (n = 238). The main reason for visiting the YHC for the whole group was for sexual and reproductive health care issues (80.7%).
Table 1. Characteristics of the whole group, selected control group and test group at T1.
The two groups were similar in their baseline characteristics, with a few exceptions: the mean age of the selected control group was slightly higher than that of the T1 group (p < .001). A higher proportion of the T1 group were visiting the YHC for the first time compared with the selected control group (p < .05). A significantly higher number of women in the T1 group than in the selected control group used painkillers during menstruation (p < .05). In the whole group, 19.3% had previously used hormonal contraception and 29.5% in the selected control group vs 6.7% in the T1 group (p < .05).
The selected control group had visited the YHC more often compared with the T1 group, for emergency contraception and ‘other’ reasons (p < .05). ‘Other’ reasons could be any number of things that apply to a young woman’s life; for instance, mental health issues, social or family issues.
Of those in the T1 group who had previously used hormonal contraception, nine estimated that the length of time since they had stopped using it was between 2 and 60 months; four could not remember exactly when they had stopped but stated that it was definitely more than 3 months.
Medicines used on a regular basis were reported by 15.8% in the whole group, 18.1% in the selected control group and 13.0% in the T1 test group (p = not significant). In the whole group 6% reported that they were on medication for asthma or allergic disorders, 4% for depression, anxiety or sleep disturbances, 2% for acne or other skin disorders, 1% for anaemia and 1% for thyroid disorder. The remaining 2% were for rheumatic disease, kidney disease, epilepsy, diabetes, migraine and stomach disorders.
Test group
Hormonal contraceptive prescriptions
Combined oral contraceptives were prescribed to 92.2% and the progestogen-only pill to 4.2% of the T1 test group. Three of the group were prescribed the etonogestrel contraceptive implant (1.5%), two the LNG-IUS (1.0%), one the transdermal contraceptive patch (0.5%) and one the etonogestrel/ethinylestradiol vaginal ring (0.5%).
Vaginal bleeding and its impact on everyday life
The number of days (mean ± SD) of reported bleeding was significantly reduced in the test group between T1 (5.49 ± 1.15 days, range 3–10 days) and T2 (5.03 ± 1.23 days, range 0–28 days) (p < .05). At T1, there was a significant correlation between the impact of menstrual bleeding on everyday life and the SF-36 VT scale (p < .007), and between the use of pain relief (p < .0001) and the duration of bleeding (p < .001).
The reported impact of menstrual bleeding on everyday life was significantly reduced at T2 (Z = 4.168 [186 − 93/93]; p = .000, two-tailed); the proportion of participants who reported a negative impact on menstruation was significantly reduced from 48% at T1 to 32% at T2 (Z = 4.659 [190−102/88]; p = .000, two-tailed). There was a significant reduction from T1 to T2 in the use of pain relief medication during menstruation (Z = 5.575, n1=192, n2=192; p = .001, two-tailed).
SF-36 scores
Better GH scores were reported in the selected control group compared with the test group at T1 (p < .01), whereas higher (better) scores for RE were reported in the test group at T1 compared with the selected control group (p < .03) ().
Table 2. SF-36 scale mean scores by group (selected control group and test group at T1 and T2).
The median time between T1 and T2 in the test group was 82 days (mean 89 ± 31 days). The changes between T1 and T2, for all SF-36 scale scores, were not significant.
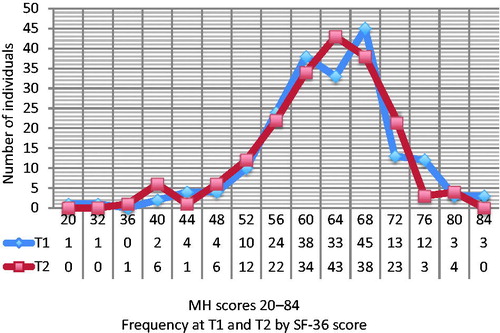
Across the whole group, 9.0% had an MH score ≤48, i.e., indicating possible depression [Citation12]. The difference between T1 and T2 for MH scores ≤48 was not significant. At T1, 6% of participants had an MH score ≤48, which rose to 7% at T2 ().
Figure 1. MH scale scores for the test group (at T1 and T2) reported by frequency (n = 193). Frequency of score ≤48 for T1 is 12 and for T2, 14 (6% vs. 7%; not significant).
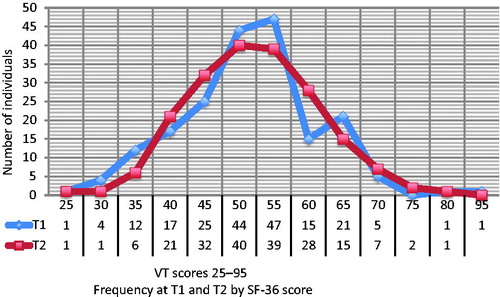
Across the whole group, 21% scored ≤40 for VT, i.e., indicating possible depression [Citation12]. No significant differences were found between T1 and T2. At T1, 17.6% of participants had a VT score ≤40, which dropped to 15.0% at T2 ().
Figure 2. VT scale scores for the test group (at T1 and T2) reported by frequency (n = 193). Frequency of score ≤40 for T1 is 34 and for T2, 29 (17.6% vs. 15.0%; not significant).
Season and SF-36 scores
The number of individuals in the selected control group and test group at T1 was not evenly distributed over the year. Therefore, three categories were created to reflect three seasons of the year: winter (November, December, January, and February), spring (March, April, May, and June), summer–autumn (July, August, September, and October).
The whole group reported significantly higher (better) mean scores in summer–autumn compared with spring in the SF-36 scales of PF, VT, RE and MH (p < .05 for all). Further, there was a significant difference in mean scores between the winter and spring categories: the scores on the RE and MH scales were lower (worse) in spring than in winter (p < .05) ().
Table 3. Mean scores on the SF-36 scales of PF, VT, RE and MH, according to three seasonal categories (n = 431 for the whole group).
The highest prevalence OR (in the whole group) for an MH score ≤48 was 2.15 (95% CI 0.95, 4.85) in spring vs winter (). The difference between the groups was not significant. There was a non-significant difference between seasons for VT scores ≤40. For VT scores ≤40 it appeared that the older the young women the higher the prevalence OR for a VT score that indicates possible depression (1.27, 95% CI 1.08, 1.49).
Table 4. Prevalence ORs for SF-36 scores of MH ≤48 and VT ≤40, adjusted for test group at T1 vs selected control group, season and age.
Discussion
Findings and interpretation
After 3 months of hormonal contraceptive (mostly COC) use among adolescents attending a YHC, the duration of bleeding and use of painkillers was reduced and the impact of menstruation on everyday life was improved. No detrimental effects on HRQOL assessment were reported.
Strengths and weaknesses of the study
To our knowledge, no study has been published using the SF-36 to assess HRQOL of hormonal contraceptive users in this population and age group. The findings of our study are important for all women prescribed hormonal contraception. Nevertheless, we cannot rule out that the lack of significant differences between T1 and T2 might have been because the study was underpowered, thus hiding subtle changes that may be of clinical interest.
Depressive symptoms, including seasonal changes in mood, become more pronounced during puberty, especially among women. There are, however, few studies that address seasonal variations in self-rated HRQOL. Since seasonal changes in mood are one possible confounding factor in the response to hormonal contraceptive use, we decided to use HRQOL scores to see if there were significant changes in mood in the gathered material. However, we encountered a problem with uneven distribution of participants over the year and we were not able to extend the time for recruiting more participants. Although a larger group would have been preferable, we nevertheless obtained results that indicated seasonal fluctuations in mood. This knowledge can be used in a clinical situation, i.e., if a woman requests hormonal contraception in February it might be wise to address her present mood before the prescription is issued.
There may be multiple reasons why 14% of women in the T1 test group did not come back for prescription renewal. It is possible that these participants might no longer have needed hormonal contraception, or they might have experienced adverse effects which caused them to discontinue use of the method.
We had intended to investigate any differences in HRQOL assessment and the hormonal contraceptive chosen, but this was not possible because of the low diversity of prescriptions. Therefore, the results relate primarily to COCs, which were prescribed to 92.2% of the whole group.
In this study, we did not adjust for possible confounding factors such as stressful life events, which are strong risk factors for depression [Citation18], nor for any prior history of mental disorder, troublesome relationships, socioeconomic difficulties or school-related stress. However, we adjusted the MH and VT scales results for group, season and age. Also, the population studied was gathered by the midwives at their convenience and in a random manner, depending on their individual interest and time as well as commitment to the study. It is difficult to speculate on whether this had an effect on the outcome.
Different factors are active and interactive in the complicated puzzle of health. Thus, the impact of estradiol levels, mental health or brain conditions related to depression, season, vitamin deficiency, obesity and severe stress seems to render a complicated symptomatology which is possibly triggered by genetic vulnerability. The symptoms caused by these different factors may then be interpreted by the patient to be side effects of hormonal contraception, leading to subsequent misuse, discontinuation or method switching, increasing the risk of unwanted pregnancy [Citation19]. This highlights the importance of counselling and support from qualified personnel. The results indicate that it may be fruitful to use an HRQOL instrument when prescribing hormonal contraception and again at a 3 month follow-up visit in order to early detect conditions such as, for example, sleeping disturbances, high stress levels and depression that may possibly lead to discontinuation of hormonal contraceptive use and subsequent unwanted pregnancy. Further studies on this subject are needed.
Differences and similarities in relation to other studies
The findings of this study are in line with those of previously published studies, which also found that heavy menstrual blood loss had an adverse effect on quality of life, especially general health and vitality, due to pain and loss of energy [Citation20]. Furthermore, oral contraceptive use has been found to reduce menstrual pain and duration of bleeding [Citation2]. Seasonal variations in reported health, especially mental health and vitality, have been reported in young women [Citation13, Citation21]. It is of note that seasonal sensitivity appears to be higher in women [Citation21].
Our previous study in a larger sample (n = 1250) than the present one found that young women using hormonal contraception had significantly better scores on the RP scale, compared with young women using no medication, medication (except antidepressants) plus hormonal contraception, antidepressants and other medication [Citation13]. In the present study, the difference between T1 and T2 on this scale was not significant; however, the present study is smaller than the previous one. Furthermore, the previous study showed a clear seasonal variation in reported health on the scales of psychological well-being [Citation13]. In the present study, there was also a seasonal variation in HRQOL scores. Scores were lowest in spring. This is interesting, as it may show an effect on the human system when it has been deprived of natural light for several months and also subjected to work stress (school and tests) and illnesses (the flu period usually peaks in January and February). Due to a smaller and unevenly distributed sample we had to slightly adjust the seasonal categories, but they still mainly followed the daylight pattern.
The fact that we found no detrimental effect on HRQOL after 3 months of hormonal contraceptive use could be because any detrimental effect is very low, or because the time between T1 and T2 was too short. However, if we had lengthened the time between T1 and T2, or added a T3, the effect of other confounding factors such as season, stress and vitamin D levels would have probably increased; furthermore, previous research has reported that most side effects appear early in hormonal contraceptive use [Citation22]. Study dropout would probably also have increased.
In the present study, adolescents with different chronic conditions comprised almost 17% of the whole group. Although this group was not studied it is nevertheless worth mentioning. Young women with a chronic disease have been reported to engage in risky behaviours in at least similar if not higher rates to those of their healthy peers despite having the potential for greater adverse health outcomes from these behaviours [Citation23]. Importantly, there was no significant difference between the selected control group and the T1 group with regard to HRQOL and reported chronic illness; thus it is unlikely that reported chronic illnesses had an effect on the main results of the study.
The T1 group and selected control group differed significantly with regard to age, the reason for their visit to the YHC, their use of painkillers during menstruation and whether hormonal contraception had been used prior to inclusion in the study. Some of these differences were probably caused by the study design (e.g., the reason for the visit), but others (e.g., the use of painkillers during menstruation in the T1 group) could have been a reason for wanting to try hormonal contraception. More individuals in the selected control group had previously been to the YHC and therefore might have been using its services for reasons other than obtaining a hormonal contraceptive prescription. Better GH scores were reported in the selected control group compared with the T1 group, and better RE scores were reported in the T1 group compared with the selected control group. These results are difficult to explain; however, we believe they have no effect on our results.
Bleeding and pain
After 3 months of hormonal contraception the duration of bleeding and the use of painkillers were significantly reduced and the impact on everyday life was significantly improved. This was supported by the correlation between the number of menstrual bleeding days in the T1 group and the VT and GH scores, as well as a tendency towards correlation with BP. This effect has been reported in other studies, i.e. heavy menstrual blood loss adversely affects quality of life, especially the assessment of general health and vitality, due to reduced energy and increased pain [Citation20,Citation24]. There was also a tendency to higher (better) scores on the BP scale (p < .07) after 3 months of hormonal contraception, as well as on the RE scale (p < .06), indicating less pain and reduced effects of emotional problems on daily activities.
Seasonal variations in SF-36 scores
Compared with the summer–autumn season, the scores for spring were lower (worse) on the scales of PF, VT, RE and MH (p < .05). The highest prevalence OR for possible depression (MH score ≤48) was reported for spring vs winter (2.15; 95% CI 0.95, 4.85). These findings may be related to another factor that bears a broad impact on health: recent research has shown that symptoms of depression (fatigue, changes in mood regulation and motor function) and pain might be related to vitamin D deficiency in depressed adolescents [Citation25]. Vitamin D metabolism also seems to be related to stress [Citation26]. Vitamin D deficiency is common, especially in Nordic countries, and results from inadequate endogenous skin synthesis (insufficient exposure to ultraviolet B rays) and diet [Citation13,Citation27–29]. At our latitude in Uppsala of 59°, there are normally about 50 h of sunlight during November, compared with 290 days in June, and low ultraviolet B rays from October to April [Citation30]. Furthermore, there is increasing evidence of an association between vitamin D deficiency, or insufficiency, and depression [Citation31,Citation32].
Depression and hormonal contraception
Nine percent of the whole group scored ≤48 on the MH scale, indicating possible depression (MADRS-S ≥21). The MH and VT scales have previously been reported to have the strongest correlation with MADRS-S [Citation11], particularly the MH scale. The figure of 9% may be compared to 11% in a YHC population (n = 453) studied approximately 10 years ago [Citation11].
No significant changes in HRQOL scores or symptoms of possible depression were found between T1 and T2, which corresponds to findings of a previous study of a YHC population, which found that those using hormonal contraception tended to report better physical health and fewer depressive symptoms than those using no medication at all [Citation13]. A Swedish nationwide register-based study reported that antidepressant drug use was generally higher among young women using hormonal contraception other than COCs, namely the LNG-IUS, implants, injections and transdermal patches [Citation33]. Since most participants (92.2%) in our study were prescribed COCs, we were not able to study the relationship between HRQOL assessment, depression and different categories of prescribed hormonal contraceptives. However, since most side effects and discontinuation seem to occur early or during the first months of use [Citation22], a future study with repeated measures of HRQOL during the first 6 months of hormonal contraceptive use might better and earlier capture possible side effects that may not be directly due to hormonal contraceptive use but induced by other important factors in the user’s life. This could shed more light on the correlation between hormonal contraceptive use, HRQOL, seasonality, depression, stress and other factors that have an impact on the perception of health.
Mood and hormones are interlinked. Notably, both the estrogen and progesterone receptors are located in brain regions involved in emotional and cognitive regulation [Citation28,Citation34]. Previous research has reported that most depressions begin during adolescence [Citation27] and that 10–20% of adolescents have had at least one major depressive episode by the age of 18 years [Citation35]. Further, a recently published study concluded that women with ongoing or previous mental disorder had a greater risk of COC-induced mood symptoms [Citation36].
Recently, COCs have been associated with small, but significant, mood side effects, particularly in the intermenstrual phase of the treatment cycle. The findings were driven by a subgroup of women who clearly suffered from COC-induced side effects [Citation5]. This effect was not found in our study, possibly due to the small size of the population studied.
A recent Danish nationwide prospective cohort study suggested that all types of hormonal contraceptive use are associated with an increased risk of depression and antidepressant treatment, especially in women aged 15–19 years. Our study can neither confirm nor refute these results [Citation37].
Confounding factors
There are many confounding factors to consider when discussing possible side effects of hormonal contraception, e.g., hereditary factors, vulnerability to mood deterioration, seasonality, obesity, psychosocial factors and school- or work-related stress [Citation1,Citation38]. Most side effects are generally self-limiting and improve with increasing duration of contraceptive use, while serious adverse events, including venous thromboembolism, are rare among healthy users [Citation39]. The seasonal effect on mood is well known and has been reported in other countries around the world [Citation40]. In our study the whole group had significantly higher (better) mean HRQOL scores on the scales of PF, VT, RE and MH during summer–autumn compared with spring. Poorer functioning in spring vs winter was found on the scales of MH and RE. Also, the prevalence OR for symptoms of possible depression (MADRS-S ≤20) was higher in spring compared with winter (2.15; 95% CI 0.95, 4.85). Furthermore, it appeared that the older the woman the higher the prevalence OR for a VT score indicating possible depression. It is difficult to speculate about the reason for this, but powerful confounding factors may be school stress, important exams and greater responsibilities.
It has been suggested that increased emotional processing and a physiological response to psychosocial stress during low estrogen phases of the menstrual cycle may contribute to depressed mood in women who are vulnerable to major depressive disorder [Citation8]. The SF-36 MH scale captured 9% of the whole group with symptoms of possible depression (MADRS-S ≤20). This is not an unexpected finding, but the VT scale rendered a higher percentage, i.e., 21% scored ≤40, which is a troubling result, since tiredness is an indicator that something is not right. In a recent review of patients in primary care complaining of tiredness, it was reported that about every fifth patient had a depressive disorder [Citation41]. Therefore, history taking, targeted at mental health and well-being, is of great importance, especially since young women with depression and stress symptoms have been reported to be at risk of using less effective contraceptive methods over time [Citation19]. Thus, it is very important to detect them early in a clinical setting.
Open questions and future research
To our knowledge, there are no published articles concerning HRQOL and use of hormonal contraception in the age group 14–20 years. This leads us to the conclusion that in this age group there are many interesting questions still to be answered. Given that there have been recurrent reports in the media about the supposed detrimental effects of hormonal contraception on health, some young women may hesitate to use it, other than, for example, as emergency contraception. However, in 2015, the Swedish National Board of Health and Welfare reported that there were 14.4 abortions per 1000 girls aged 15–19 years, compared with 25.4 abortions per 1000 girls in 2006. The decrease in the number of abortions is thought to be due to new methods and better provision of contraception [Citation42].
Interestingly, in the county of Uppsala, where the present study was conducted, the use of short-acting hormonal contraception (pills, patches and rings) among young women aged 15–19 years in the 10-year period between 2006 and 2016 has been rather steady: the lowest prevalence was 341.4/1000 girls in 2012, rising to 364.0/1000 girls in 2016 [Citation43]. During the same period, the use of a long-acting reversible contraceptive (LARC) method (intrauterine contraception and subdermal patches) increased from 26.9/1000 girls aged 15–19 years in 2012 to 61.2/1000 in 2016 [Citation43]. Nevertheless, in our study very few participants were prescribed LARC. In the future, it would be interesting to study HRQOL in the same age group before and after starting a LARC method. Eventually, due to increased evidence of the role of vitamin D in health and well-being [Citation44], and also evident seasonal variation in HRQOL scores [Citation13], it would be interesting to study vitamin D levels and HRQOL scores over a 12-month period in young women starting hormonal contraception.
Conclusions
After 3 months of hormonal contraceptive (mostly COC) use among adolescents visiting a YHC, the duration of bleeding and use of painkillers was reduced and the impact of menstruation on everyday life was improved. No detrimental effects on HRQOL were reported. A seasonal effect on self-reported HRQOL was found: poorer mean scores on the SF-36 scales of PF, VT, RE and MH were reported in the spring compared with the summer–autumn season.
Acknowledgements
We thank PhD Lars Berglund, at Uppsala Clinical Research Center, for his skilful help.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Frye CA. An overview of oral contraceptives: mechanism of action and clinical use. Neurology. 2006;66(6 Suppl. 3):S29–S36.
- Kaunitz AM. Oral contraceptive health benefits: perception versus reality. Contraception. 1999;59(1 Suppl):29S–33S.
- Wallwiener CW, Wallwiener LM, Seeger H, et al. Sexual function, contraception, relationship, and lifestyle in female medical students. J Women’s Health (Larchmt). 2017;26:169–177.
- Hatcher RA, Trussell J, Stewart F, et al. Contraceptive technology. 20th rev. ed. New York (NY): Ardent Media; 2011.
- Lundin C, Gemzell Danielsson K, Bixo M, et al. Combined oral contraceptive use is associated with both improvement and worsening of mood in the different phases of the treatment cycle – a double-blind, placebo-controlled randomized trial. Psychoneuroendocrinology. 2016;76:135–143.
- Poromaa IS, Segebladh B. Adverse mood symptoms with oral contraceptives. Acta Obstet Gynecol Scand. 2012;91:420–427.
- Kulkarni J. Depression as a side effect of the contraceptive pill. Expert Opin Drug Saf. 2007;6:371–374.
- Rubinow DR, Schmidt PJ, Roca CA. Estrogen–serotonin interactions: implications for affective regulation. Biol Psychiatry. 1998;44:839–850.
- Ware JE Jr, Gandek B. Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol. 1998;51:903–912.
- World Health Organization [Internet]. Constitution of WHO: principles; 2018. Available from: www.who.int/about/mission/en/
- Kristjansdottir J, Olsson GI, Sundelin C, et al. Could SF-36 be used as a screening instrument for depression in a Swedish youth population? Scand J Caring Sci. 2011;25:262–268.
- Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389.
- Kristjansdottir J, Olsson GI, Sundelin C, et al. Self-reported health in adolescent girls varies according to the season and its relation to medication and hormonal contraception – a descriptive study. Eur J Contracept Reprod Health Care. 2013;18: 343–354.
- Gupta N, O’Brien R, Jacobsen LJ, et al. Mood changes in adolescents using depot-medroxyprogesterone acetate for contraception: a prospective study. J Pediatr Adolesc Gynecol. 2001; 14:71–76.
- The Swedish Society for Youth Centres [Internet]. Guidelines for Swedish youth centres; 2018. Available from: www.fsum.org/fsum/wp-content/uploads/2011/02/guidelines_2.pdf
- Sullivan M, Karlsson J, Taft C, editors. SF-36 Hälsoenkät. Svensk Manual och Tolkningsguide 2: a upplagan. Gothenburg: Sahlgrenska University Hospital; 2002.
- Ware JE Jr, SF-36 health survey update. Spine (Phila Pa 1976). 2000;25:3130–3139.
- Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. Am J Psychiatry. 2002;159:1133–1145.
- Hall KS, Moreau C, Trussell J, et al. Role of young women's depression and stress symptoms in their weekly use and nonuse of contraceptive methods. J Adolesc Health. 2013;53: 241–248.
- Weisberg E, McGeehan K, Fraser IS. Effect of perceptions of menstrual blood loss and menstrual pain on women's quality of life. Eur J Contracept Reprod Health Care. 2016;21:431–435.
- Tonetti L, Barbato G, Fabbri M, et al. Mood seasonality: a cross-sectional study of subjects aged between 10 and 25 years. J Affect Disord. 2007;97:155–160.
- Rosenberg MJ, Waugh MS. Oral contraceptive discontinuation: a prospective evaluation of frequency and reasons. Am J Obstet Gynecol. 1998;179:577–582.
- Sawyer SM, Drew S, Yeo MS, et al. Adolescents with a chronic condition: challenges living, challenges treating. Lancet. 2007; 369:1481–1489.
- Chi C, Pollard D, Tuddenham EG, et al. Menorrhagia in adolescents with inherited bleeding disorders. J Pediatr Adolesc Gynecol. 2010;23:215–222.
- Hogberg G, Gustafsson SA, Hallstrom T, et al. Depressed adolescents in a case-series were low in vitamin D and depression was ameliorated by vitamin D supplementation. Acta Paediatr. 2012;101:779–783.
- Zhang HQ, Teng JH, Li Y, et al. Vitamin D status and its association with adiposity and oxidative stress in schoolchildren. Nutrition. 2014;30:1040–1044.
- Deecher D, Andree TH, Sloan D, et al. From menarche to menopause: exploring the underlying biology of depression in women experiencing hormonal changes. Psychoneuroendocrinology. 2008;33:3–17.
- Newhouse P, Albert K. Estrogen, stress, and depression. A neurocognitive model. JAMA Psychiatry. 2015;72:727–729.
- Krzywanski J, Mikulski T, Krysztofiak H, et al. Seasonal vitamin D status in Polish elite athletes in relation to sun exposure and oral supplementation. PLoS One. 2016;11:e0164395.
- Swedish Meteorological and Hydrological Institute. Normal sunshine for one year [Internet]; 2017. Available from: www.smhi.se/klimatdata/meteorologi/stralning/normal-solskenstid-for-ett-ar-1.3052
- Parker GB, Brotchie H, Graham RK. Vitamin D and depression. J Affect Disord. 2017;208:56–61.
- Kerr DC, Zava DT, Piper WT, et al. Associations between vitamin D levels and depressive symptoms in healthy young adult women. Psychiatry Res. 2015;227:46–51.
- Lindberg M, Foldemo A, Josefsson A, et al. Differences in prescription rates and odds ratios of antidepressant drugs in relation to individual hormonal contraceptives: a nationwide population-based study with age-specific analyses. Eur J Contracept Reprod Health Care. 2012;17:106–118.
- Toffoletto S, Lanzenberger R, Gingnell M, et al. Emotional and cognitive functional imaging of estrogen and progesterone effects in the female human brain: a systematic review. Psychoneuroendocrinology. 2014;50:28–52.
- Costello EJ, Mustillo S, Erkanli A, et al. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–484.
- Bengtsdotter H, Lundin C, Gemzell Danielsson K, et al. Ongoing or previous mental disorders predispose to adverse mood reporting during combined oral contraceptive use. Eur J Contracept Reprod Health Care. 2018;23:45–51.
- Skovlund CW, Morch LS, Kessing LV, et al. Association of hormonal contraception with depression. JAMA Psychiatry. 2016;73:1154–1162.
- Nygaard Andersen M, Bech P, Csillag C. Development and remission of depressive symptoms and treatment with hormonal contraceptives. Oxf Med Case Rep. 2014;2014:63–64.
- Dragoman MV. The combined oral contraceptive pill – recent developments, risks and benefits. Best Pract Res Clin Obstet Gynaecol. 2014;28:825–834.
- Melrose S. Seasonal affective disorder: an overview of assessment and treatment approaches. Depress Res Treat. 2015;2015: 178564.
- Stadje R, Dornieden K, Baum E, et al. The differential diagnosis of tiredness: a systematic review. BMC Fam Pract. 2016;17:147.
- Swedish National Board of Health and Welfare [Internet]. Abortion statistics; 2015. Available from: www.socialstyrelsen.se/publikationer2016/2016-5-20
- Swedish National Board of Health and Welfare [Internet]. Statistics database for medicines; 2018. Available from: www.socialstyrelsen.se/statistik/statistikdatabas/lakemedel
- Husmann C, Frank M, Schmidt B, et al. Low 25(OH)-vitamin D concentrations are associated with emotional and behavioral problems in German children and adolescents. PLoS One. 2017; 12:e0183091.
