Abstract
Introduction: Effective use of contraception requires women to make an informed choice about methods that match their individual needs and expectations. The European Thinking About Needs in Contraception (TANCO) study is a quantitative, online survey of healthcare provider and women’s views on aspects of counselling around contraception and contraceptive use.
Methods: Healthcare providers and women attending their practices for contraceptive counselling were invited to complete online questionnaires. The women’s survey explored knowledge and use of contraceptive methods, satisfaction with current method, and interest in receiving more information about all methods. Healthcare provider views were gathered in parallel.
Results: A total of 676 healthcare providers and 6027 women completed the online surveys in 11 countries. There was a high prevalence of contraceptive use and general satisfaction with current method across the countries. Fifty-five percent of women were using short-acting contraception (SAC) methods; 19% were using a long-acting reversible contraception (LARC) method. Sixty percent of women were interested in receiving more information about all methods; 73% of women said they would consider LARC if they received more comprehensive information. Healthcare providers tend to underestimate women’s interest in receiving information on contraception in general and, more specifically, LARC methods.
Conclusions: Despite high levels of use and satisfaction with current methods, women were interested in receiving more information about all contraceptive methods. Greater exploration of women’s views on their needs and expectations of contraception could lead to increased knowledge, more effective discussions with healthcare providers and the greater likelihood of informed contraceptive choice.
摘要
引言:有效应用避孕措施要求妇女在知情的情况下选择符合其个人需要和期望的方法。《欧洲人对避孕需求的思考》(TANCO)研究是一项定量的在线调查, 调查对象是医疗服务提供者和女性对避孕咨询和避孕使用方面的看法。
方法:卫生保健服务提供者和参加避孕咨询实践的妇女被邀请填写在线问卷。妇女调查涉及避孕方法的相关知识和使用, 对现行方法的满意度, 以及对获得更多关于所有方法的信息兴趣。医疗服务提供者的相应问题看法是同时收集的。
结果:共有676名医疗服务提供者和6027名女性在11个国家完成了在线调查。避孕药具的使用率很高, 各国对现行避孕方法普遍感到满意。55%的女性使用的是短效避孕法(SAC);19%使用长效可逆避孕(LARC)方法;60%的女性有兴趣获得更多关于所有方法的信息;73%的女性表示, 如果得到更全面的信息, 她们会考虑LARC。卫生保健提供者往往低估了妇女对常用避孕方法信息的兴趣, 更具体地说, 是LARC方法。
结论:尽管对目前的避孕方法的应用和满意程度很高, 但妇女有兴趣获得关于所有避孕方法的更多资料。更多地了解妇女对避孕的需求和期望的看法, 可以增加知识, 更有效地与卫生保健提供者进行讨论, 进而做出知情避孕选择的可能性也更大。
Introduction
Today, there is a broad range of effective contraceptive methods available. Women need access to accurate information about these different methods to choose an option that matches their individual needs regarding lifestyle, family planning, risk factors and non-contraceptive benefits [Citation1,Citation2]. However, to be most effective, delivery of counselling needs to be within a patient-centred framework that encourages discussion and shared-decision making between a woman and her healthcare provider (HCP) [Citation3,Citation4]. The US Contraceptive CHOICE study in the United States demonstrated a clear difference in uptake of long-acting reversible contraception (LARC) methods (intrauterine contraception [IUC] and hormonal implant) when lack of awareness of method safety and efficacy was addressed during a structured counselling approach and all options were available at no cost [Citation5,Citation6]. Increasing knowledge and removing financial barriers also led to greater satisfaction and continuation with LARC methods at 12 months when compared with the use of oral contraceptives (OC) [Citation6].
Despite the availability of multiple, effective contraceptive methods, there remains a high rate of unintended pregnancies globally [Citation7], with significant social and economic consequences [Citation8,Citation9]. Improved access to LARC methods in the US Contraceptive CHOICE study reduced the incidence of teenage pregnancy and birth and abortion rates when compared with national rates among sexually experienced teens and led to cost savings within the US healthcare system [Citation10]. In an effort to increase the use of more effective, user-independent methods, there has been a paradigm shift in recommendations regarding the counselling of young women on the use of LARCs. Guidance on best practice from global and national organizations is focused on broadening access to LARC methods by attempting to remove barriers relating to age, parity and risk of sexually transmitted infections [Citation11–14]. Despite these recommendations, lack of knowledge of LARCs and misperceptions around efficacy and side effects continue to limit women’s choice of these highly effective methods [Citation15,Citation16]. Furthermore, discussion of LARCs may be limited by HCP assumptions about women’s interests and beliefs when choosing a method of contraception [Citation15,Citation17,Citation18]. Healthcare providers continue to be the most trusted source of sexual health information and therefore hold a key position in the delivery of reliable facts about contraception, despite a global increase in use of the internet and social media [Citation19]. In addition, limitations around reimbursement for counselling itself may represent a barrier in HCP provision of counselling on all methods. The initial Thinking About Needs in Contraception (TANCO) study, conducted in Germany, provided country-specific insights into the extent to which women’s choice of contraceptive method depends on their gynaecologist’s advice and whether broader counselling, which includes all methods, could increase interest in use of LARC methods [Citation18]. In this survey, only 9% of the 18,521 women were using LARC methods, yet 60% of the women stated they would consider LARCs as an option if they were provided with more information. Gynaecologists underestimated this high-level interest, believing that only 18% of women would be interested in LARC methods.
The European TANCO study was initiated in February 2017, with the specific aim of assessing multiple aspects of contraceptive use by women in 11 countries. Healthcare provider insights were gathered in parallel to provide additional guidance on how to better address current unmet needs in contraceptive counselling. This publication describes the final results of the European TANCO study.
Objectives
The primary objectives of the TANCO European study were to:
Evaluate women’s use, awareness and self-reported knowledge of contraception;
Assess satisfaction with current methods, including compliance with OC;
Identify women’s needs and expectations of contraception and measure their interest in receiving regular or more extensive information about all methods;
Compare the insights into women’s needs and expectations with what HCPs perceive to be women’s priorities when choosing a contraceptive method.
The study also evaluated perception of HCP contraceptive counselling services from both the practitioner and patient perspective.
Materials and methods
The European TANCO study was a quantitative online survey of HCP and women’s views on aspects of counselling around contraception and contraceptive use. The study concept was designed jointly by a global market research organisation (Psyma Health and Care) and the sponsor, Bayer AG. The European Society of Contraception (ESC) supported the study by facilitating access to HCPs in target countries.
Healthcare providers with at least two years’ experience of clinical practice and providing regular contraceptive counselling services were recruited on a country by country basis from Belgium, Czech Republic, Finland, France, Ireland, Poland, Portugal, Slovenia, Spain, Sweden and Switzerland via existing local market research databases in the respective countries and included gynaecologists, general practitioners, nurses and midwives. Women were invited to participate via the individual HCP practices. Written information containing a description of the study and instructions on how to access the online questionnaire was handed to women attending for contraceptive counselling and/or women’s healthcare services. Women were then free to choose whether to participate. To be eligible, women had to be aged between 18 and 49 years.
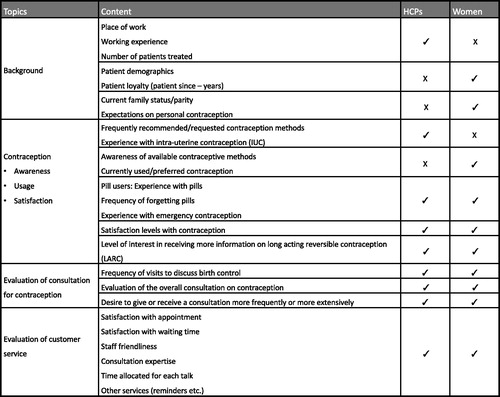
The study involved completion of online questionnaires, the starting point for which was a 45-item survey developed by contraception experts in Germany for use within the German TANCO study described by Oppelt et al. [Citation18] Questions for the European TANCO study were extracted, modified, and evaluated for scientific quality, clarity and relevance to an international population by the authors. An overview of the question topics is included in . The final questionnaires comprised 18 questions for women and 17 questions for HCPs and were designed to be completed in 10 and 15 min, respectively. Both were tested for clarity, ease of completion and accuracy regarding the time needed for completion amongst HCPs and women in one pilot country (Ireland) prior to translation and roll-out to the remaining countries. Some questions were slightly modified during the roll-out process to meet regulatory requirements and product availability in specific markets for example, exclusion of brand names was required in some countries and the hormonal implant was not available in Slovenia. Women not meeting the age criteria were automatically excluded from the study by a screening question. Initial questions for women focused on demographic data: life situation relative to job, partnership status, and family planning. They were then asked questions about their awareness, self-reported knowledge and use of different contraceptive methods. Women were asked to select one of the following four options: ‘know very well (what it is and how it works)’; ‘know some basic information’; ‘only heard of it before’; or ‘have not heard of it at all’ in response to the question ‘How well do you know… the 14 contraceptive methods’ (listed as combined pill, mini-pill [progestogen-only pill, POP], contraceptive ring, contraceptive patch, contraceptive injection, contraceptive implant, hormonal coil [IUS], copper coil [IUD], contraceptive cap, spermicide, natural methods, condom, morning after pill, and sterilisation/vasectomy). Women were asked to select their current method of contraception from an identical list.
Satisfaction with current contraceptive method and important needs and expectations around contraception were assessed using a seven-point scale (1–7, where 1 = not satisfied/not important and 7 = very satisfied/very important depending on the question). Comparison of overall satisfaction and importance was carried out using the proportion of respondents selecting the top two answers (i.e. a score of 6 or 7) to these questions plus the mean value (1–7). Women’s interest in receiving more frequent or additional information regarding all methods of contraception was assessed by asking women to choose from one of four responses: ‘yes, more frequent especially for new products’; ‘yes, more extensive’; ‘yes, more frequent and more extensive’; or ‘no, I do not need any additional information’. Additional questions regarding use of contraception focused on the frequency with which women forgot to take their OC and their use of emergency contraception. The final section of the questionnaire assessed women’s views on the contraceptive counselling services provided by their HCP, including amount of information shared, time taken to counsel, friendliness and ease of getting an appointment, using a seven-point scale (1–7, where 1 = unsatisfactory and 7 = very satisfactory). Results are reported in the manner described above.
Healthcare providers completed 17 questions in total. Early questions gathered information on professional experience, place of work, number of women treated per quarter, common contraceptive methods prescribed and experience with placement of IUC devices and facilitated the filtering of those HCPs not meeting the study inclusion criteria in terms of duration of clinical practice. The remaining questions and response scales mirrored those asked of the women in order to determine HCP perceptions of women’s use of and attitudes towards contraception, their compliance and their views on the services HCPs provided.
The study took place between February and November 2017. Survey design, distribution logistics and administration were coordinated by Psyma Health and Care and funded by the sponsor, Bayer AG. International review board (IRB) approval was not sought as patient response data would be anonymized, aggregated as global data for the purposes of analysis and reporting and not retained by the market research agency. Statistical analyses of descriptive and comparative data (i.e., comparison of demographic, country, and method use) was carried out by Psyma using SPSS. Participating HCPs received monetary and non-monetary incentives equal to their dedicated time and in accordance with local market research guidelines. The latter involved the offer of individual practice data (provided at least n = 10 of their own patients completed the survey) or an analysis of the regional data. In all cases, the data included in these reports was numeric only.
Results
From February to November 2017, a total of 1049 healthcare providers and 7483 women in 11 European countries accessed the respective online surveys. Sixty-five percent (n = 676) of HCPs and 81% (n = 6027) of women accessing the survey went on to complete the respective questionnaires (see ). Of the 676 HCPs participating in the study, 87% were gynaecologists, 8% were GPs and 5% were nurses or midwives. Sixty-three percent were female. Thirty-nine percent of HCPs worked only in private practice; 13% worked only in hospitals; and 34% worked in both hospital and private practice. On average, HCPs had 20 years of working experience and saw 140 patients aged between 18 and 49 years per month for contraceptive counselling. Ninety-two percent of HCPs were currently placing IUC devices; on average, they inserted three to four IUC devices per month (range 1–8 per month).
Table 1. Number of women and HCPs who completed the respective online surveys by country.
Of the 6027 women participating in the study, the average age was 32 years; 73% were married or in a stable relationship and 67% were employed (either full- or part-time). Almost half of women (45%) were parous, with an average of two children. Seventy-two percent of women were not planning to have any children in the next three to five years.
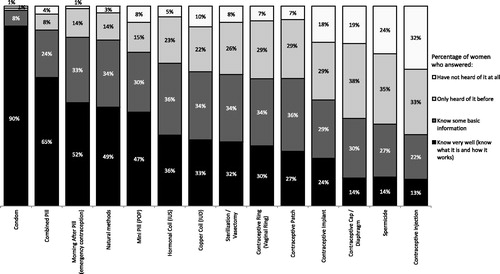
Awareness and self-reported knowledge of currently available contraceptive methods
When asked about their awareness of currently available contraceptive methods, only 17% of women reported good or basic knowledge of all 14 methods presented. On average, women knew very well or had a basic knowledge of nine methods. Women’s self-reported knowledge of combined pills, mini-pills, natural methods and emergency contraception was highest: 88%, 77%, 83%, and 84% of women respectively rated their knowledge of these methods as good or basic (see ). Women’s knowledge of the hormonal IUS, copper IUD, vaginal ring and hormonal patch was not as extensive: 71%, 67%, 64%, and 64% of women, respectively rated their knowledge of these methods as good or basic. Overall, self-reported knowledge of IUC (hormonal IUS and copper IUD) was significantly lower than for OCs (combined pill and mini-pill); 69% and 83%, respectively. Notably, significantly older women (aged 40–49 years) reported good or basic knowledge of IUC when compared with those aged 18–29 years (46% versus 27%). Levels of self-reported knowledge of different methods in individual countries were generally consistent with overall findings.
Contraceptive use by women
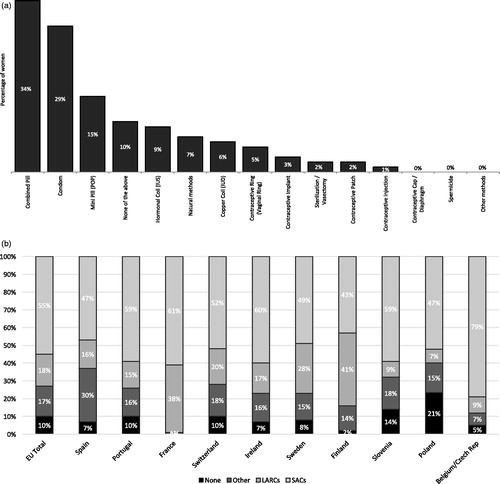
Ninety percent (n = 5448) of the women surveyed stated that they were currently using contraception (see ). More than half (55%) were using a short-acting contraception (SAC) method: 34% were using a combined pill and 15% were using a mini-pill. Eighteen percent of women were using a LARC method: 9% hormonal IUS; 6% copper IUD and 3% hormonal implant. Almost one-third (29%) of women were using the condom, of which 12% were using it as their sole method. There was greater use of SAC methods than LARC methods by women in all countries (see ). Use of SAC methods ranged from 43% (Finland) to 79% (Belgium/Czech Republic); LARC use ranged from 7% (Portugal) to 38% (France).
Figure 3. (a) Methods used by women at the time of the survey (multiple answers were permitted), (n = 6027). (b) Methods used by women at the time of the survey (multiple answers were permitted), in individual countries and grouped by method type (n = 6027). SAC methods include combined pill, mini-pill (POP), vaginal ring, hormone injection and hormone patch; LARC methods include IUC (both IUD and hormonal IUD) and hormone implant.
Healthcare providers also estimated combined pills to be the most frequently used method by patients (46%). When looking at the impact of age, marital status and parity on contraceptive use, women using SACs (n = 3315) were generally younger (mean age 30 years) than those using LARCs and nulliparous. The mean age of women using LARCs (n = 1057) was 36 years and they were generally married, or in a stable relationship, and parous.
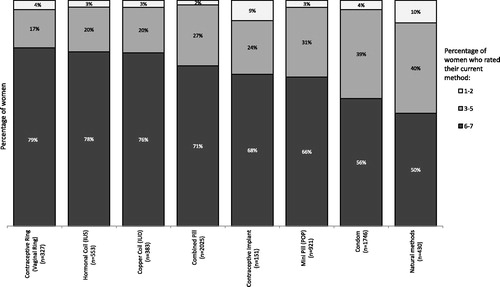
Satisfaction: the extent to which women feel happy with current method
Overall satisfaction with current contraceptive method was high; more than 50% of women indicated they were highly satisfied (i.e., rated as 6 or 7 on scale of 1–7) (see ). When looking at the three most commonly used prescription methods (combined pill, mini pill and hormonal IUS), satisfaction was significantly greater amongst users of the hormonal IUS: 78% indicated high satisfaction with this method compared to 71% for the combined pill and 66% for the mini pill (p < .05). This significant difference in satisfaction was also reflected in the comparison between SAC and LARC methods (66% and 76%; p < .05).
Figure 4. Women’s satisfaction with their current contraceptive methods rated on a scale of 1–7, where 1 = not at all satisfied, and 7 = very satisfied. Most commonly used methods (by >2.5% of women surveyed) are presented.
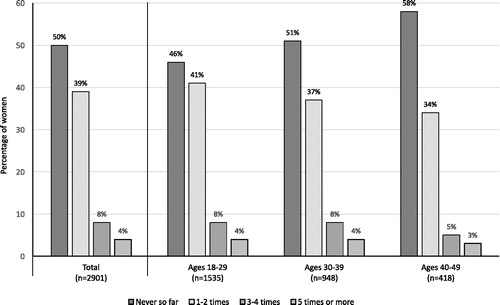
Compliance with short acting contraceptive methods
Fifty per cent of all pill users (n = 2901) stated that they had forgotten to take one or more of their pills in the last three months. Of these, the majority (78%) had forgotten to take them once or twice (see ). Women aged <30 years tended to forget the pill more often than women aged ≥30 years (54% versus 47%; p < .05). HCPs generally underestimated the extent to which women forgot to take their pill; believing that only 36% of women had forgotten at least once in the last three months.
Use of emergency contraception
Thirty seven per cent of women included in the study had used emergency contraception (EC) to prevent unintended pregnancy at some point in their life. The majority of these women (54%) had used it only once. HCPs generally underestimated the number of women who had used EC, believing on average that only 23% of women had ever used it in their lifetime.
Needs and expectations regarding contraceptive methods
When women were asked about the personal importance of different attributes of a contraceptive (17 options were presented; see ), assurance of reliability was identified as most important, rated as highly important (i.e., rated as 6 or 7 on scale of 1–7) by 90% (mean score 6.6) of those surveyed, irrespective of age or parity. A low risk of thrombosis was the second most important attribute, rated by 79% (mean score 6.2) of women as highly important. The ability to fit to their lifestyle and suitability for individual family planning were both rated as important by 72% of women (mean score 5.9). Older women had different priorities to younger or single women. For women aged ≥30 years, low risk of thrombosis, suitability for individual family planning, freedom not to think about contraception continuously and a low dose of hormones were all significantly more important than amongst younger women (aged 18–29 years). Both LARC and SAC users considered reliability, in terms of efficacy, to be the key attribute of a contraceptive method. When looking at other important attributes, low risk of thrombosis, fits to current lifestyle, suits individual family planning, low dose of hormones, suitable for nulliparous women, reduction in bleeding intensity and pain and immediate reversibility on discontinuation were all rated as highly important by 60% or more of both LARC and SAC users.
Figure 6. Actual percentage of women rating attributes of contraception 6 or 7 (on a scale of 1–7 where 1 = not important at all, and 7 = very important) versus HCP estimations of importance of those attributes to women. Only attributes rated 6 or 7 by ≥60% of women are presented.
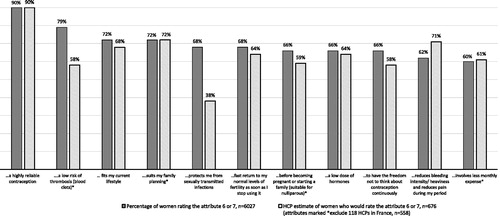
Healthcare provider perception of the importance of high reliability of a method to women matched the views of those women surveyed. However, in contrast to women’s views on the importance of safety, HCPs regarded suitability with individual family planning, reduction of bleeding intensity and pain during a period, fitting with current lifestyle, fast return to fertility with cessation of use, low dose of hormones and less monthly expense as the most important attributes for women (see ).
Information needs: level of interest in receiving more information about contraceptive methods
Sixty per cent of all women stated they would be interested in receiving more information (‘more frequent, especially for new products’, or ‘more extensive’, or ‘more frequent and more extensive’) about all contraceptive methods from their HCP. There was a significant difference in interest in receiving more information between SAC and LARC users: almost two thirds (64%) of women currently using a SAC method were interested in more information compared to 51% of those using a LARC. Almost one-third (29%) of all women were interested in hearing specifically about new products. HCPs tended to underestimate women’s interest in receiving more regular or extensive information (60%), declaring that only 46% of their patients would be interested. There was also a mismatch regarding specific interest in contraception with either no hormones or a low dose of hormones: 62% of women were highly interested in such contraceptives while HCPs believed that only 45% of women would be highly interested (data not shown).
Information needs: interest in LARC
Seventy-three per cent of all women (n = 5564) stated that LARCs could be a potential option if they were to receive more information on the methods from their HCP. Women who were aged 30–39 years or parous were significantly more interested in LARCs as an option than women aged 18–29 and 40–49 years or nulliparous. However, only 28% of women aged 18–29 years stated that a LARC method would not be an option. As with interest in receiving more information on all contraceptive methods, HCPs underestimated women’s interest in LARCs as an option; on average, believing only 38% of all women to be interested.
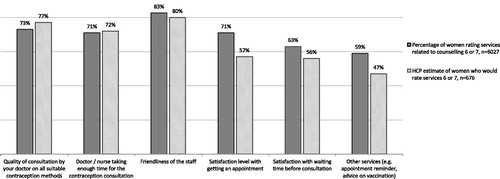
Evaluation of counselling
Women surveyed were generally more satisfied with staff friendliness than other services relating to counselling quality (see ). Staff friendliness and quality of HCP consultation on all contraceptive methods were rated as highly satisfying (i.e., rated as 6 or 7 on scale of 1–7) by 83% (mean score 6.3) and 73% (mean score 6.0) of women, respectively. Although rating of consultation quality by women was slightly lower than HCPs’ own rating (73% vs. 77%), views on the time available for a consultation were more closely aligned.
Discussion
Findings and interpretation
The European TANCO study provides insights into contraceptive use and satisfaction as well as knowledge of methods from 676 HCPs and 6027 women situated in 11 European countries. There was good awareness and self-reported knowledge of SAC, natural and emergency methods amongst the women surveyed; however, LARC methods were less well-known. There was a high prevalence of contraceptive use across the 11 European countries and women of all ages were generally satisfied with their current method. Almost half of all women were using an OC and, even though the hormonal IUS was the second most prevalent prescription method, it was used by only one in ten women. LARC methods tended to be used by older women (≥30 years) with children, a likely consequence of previous recommendations for contraceptive counselling. Approximately three quarters of the women surveyed said they would consider LARCs as an option if they received more comprehensive information.
Despite the paradigm shift around the use of LARCs, many HCPs still believe that IUC is unsuitable for young or nulliparous women and may limit counselling to only SAC methods [Citation15]. A move towards recommendations against the use of COCs for women aged over 40 years and in those with cardiovascular risk factors will focus HCP attention on recommending IUC for this age group [Citation11,Citation14]. In addition, these women would not typically be planning to have more children and so would be more interested in using a LARC method.
Findings were generally consistent across the countries and, where disparities existed, are likely to be explained by differences in product availability and reimbursement status. Use of LARC methods remains low despite recommendations for broader use from global and national organizations in countries with unreliable SAC users and high abortion rates. This might reflect that many women continue to choose OCs due to lack of knowledge of other options or problems associated with reimbursement [Citation6,Citation20]. Factors such as the desire for good cycle control, a predictable bleeding pattern and improvement of menstrual symptoms [Citation21] may also continue to drive use of this method, despite it being demonstrated in this and other studies that correct daily pill intake is a challenge for some women [Citation18,Citation20].
Satisfaction with current contraceptive method was generally high. Apart from users of combined pills, women were generally more satisfied with their current methods than expected by HCPs. High satisfaction rates are not surprising given that dissatisfied women are likely to have switched method earlier. The study findings show current contraceptive use and related satisfaction; however, they do not provide any insights regarding previous method use and reasons for change. The greatest disparities between women’s satisfaction and HCP perception was seen with hormonal methods such as the patch, injection and implant. For example, although 68% of women stated they were highly satisfied with the hormonal implant, on average, HCPs estimated that only 22% would be satisfied.
HCPs clearly underestimated the interest in receiving information about contraceptive methods in general. They believed that just over a third of their patients (38%) would be interested in using a LARC method, if they were to receive more details, when almost double that number (73%) of women stated this to be the case. Women also had different views to their HCPs on what was important regarding a method of contraception. Whilst both HCPs and women were in agreement regarding the high importance of ‘assurance of high reliability’ of contraceptive method, our findings indicated that women were more concerned with safety than HCPs realised. Women ranked ‘a low risk of thrombosis’ as the second most important attribute of their contraceptive method. Given that the VTE risk for healthy young COC users is low [Citation21], greater clarification of this risk to women expressing concern may be needed during the consultation. On a broader basis, areas of disconnect around women’s interest in receiving information about different types of contraception and their needs and expectations of methods demonstrate the need for more effective communication and interaction between HCPs and their patients.
Women and HCPs consistently rated the quality of consultation on all suitable methods of contraception as highly satisfying but knowledge (assessed by self-reported knowledge of all 14 methods) was low, suggesting that women may have quickly discounted other methods as unsuitable at some point in the counselling process or might be unable to choose the most appropriate method for them due to reimbursement policies.
Compliance rates with the pill highlighted many contradictions. As with other studies comparing women’s use of contraceptive methods, compliance amongst pill users was poor. Although women reported high satisfaction with the pill and regarded contraceptive reliability as very important, the majority (77%) of women reporting they had missed a pill said they had forgotten on one or two occasions in the last three months. We know from studies such as CHOICE that imperfect use of OCs contributes to a decrease in efficacy as shown by the ‘typical use’ failure rate of 9% per year [Citation22,Citation23].Any missed pills may therefore contribute to an increased risk of unintended pregnancy and create uncertainty for the women concerned. For the 12% of women who reported they had forgotten more than three pills during the last three months the risk of unintended pregnancy is especially high [Citation24].
Strengths and limitations of the study
A strength of the European TANCO study is the sample size. We report the collected views of 6027 women across 11 countries. The study provides insights into factors that women consider to be important when choosing contraception and their interest in receiving more information about other methods, all of which can guide HCPs in addressing current unmet needs in contraceptive counselling. A further strength of the study is that the recruitment process i.e., via HCP practices in the 11 countries, allowed women’s views on many aspects of contraceptive use to be compared with those of their respective HCPs.
A limitation of the European TANCO study is that all respondents were self-selected by their willingness to access a website and answer an online questionnaire. Nineteen percent of women accessing the survey declined to complete the questionnaire. Lack of an incentive was thought to be the main reason for non-completion, however, this information was not captured formally.
Only women visiting a HCP were included. The lack of information about reason for the visit, absence of recruitment quotas and wide variation (no weighting) in the number of participants means that findings are unlikely to be wholly representative of contraceptive users or their HCPs in each country and valid cross-country comparison regarding attitudes or beliefs amongst sub-groups was difficult to achieve.
Levels of self-reported knowledge of contraceptive methods were low in the European TANCO study. As a short, online survey, it was difficult to correlate this self-reported knowledge with actual knowledge of different methods. As with the European CHOICE study [Citation25], which assessed women’s perceptions and reasons for choosing one of three particular methods (the pill, patch or ring), our survey showed that women reported greater knowledge of methods they were using or had used than those never used.
Although it was useful to evaluate the extent to which women were satisfied with their current method of contraception, a further limitation of an online survey such as the European TANCO study was the absence of questions about the features of a method women were satisfied with and also reasons for dissatisfaction with previous methods.
The study included over 6000 women, However, the minimum age excluded the participation of many adolescent women (those aged <18 years). This group of women were identified by the European CHOICE study as being greatly influenced by balanced counselling from their HCP [Citation26]. Analysis of the 15–20-year-old sub-group found that counselling on methods such as the combined OC, patch and ring greatly influenced decisions on which method to choose and led to broader use of the patch and the ring by this age group [Citation26].
We know from a survey by Gemzell-Danielsson et al. [Citation27] that age, gender, type of HCP and personal experience of contraceptive methods all influence the extent to which some methods (such as the pill and IUC) are discussed within a consultation. The majority of HCPs participating in the European TANCO study were gynaecologists (87%) and female (63%) and we have no knowledge of their personal (or partner) experience of contraceptive methods. Healthcare provider influence on the knowledge and use of contraceptive methods by women participating in the study could therefore be an additional limitation.
Comparison with other studies
The findings of the European TANCO study reflect those of other studies investigating women’s needs and expectations of contraception and their information requirements conducted on a national or global basis [Citation20,Citation28]. An international study of 12,094 women across Brazil, Europe, and the US reported a high level of combined OC use, high satisfaction (73%) with current methods, the importance of contraceptive reliability and a high rate of noncompliance amongst OC users [Citation20]. High use of combined OCs, high satisfaction levels and importance of reliability were also reported in a quantitative study of knowledge and use of contraceptive methods amongst 2544 women in the US, UK, Germany, Italy, and Spain [Citation28].
When asking women about their needs and expectations of contraception, importance of predictability of bleeding were not included as potential factors in the European TANCO study. Several studies across different countries indicate the negative attitudes of women towards breakthrough bleeding and unpredictable bleeding, the most frequent reason for discontinuation of progestin-only pills and implants [Citation20,Citation29,Citation30]. On the one hand, we know from the study by Mansour et al. [Citation20] that many women (49%) regard the absence of a monthly period as unhealthy or see its presence as confirmation that they are not pregnant. However, in a global, population-based study focused specifically on attitudes towards monthly bleeding [Citation29], almost one-third said that bleeding had a negative impact on quality of life, 60% of women said they would like to be able to delay their bleeding and approximately one third said they would prefer to bleed less frequently i.e., once in every two or three months. These findings were also reflected in a survey of Swiss women’s preferred menstrual/withdrawal bleeding pattern over their reproductive life. Amongst almost 300 women aged between 15 and 49 years, 32% stated they would prefer to bleed every two to six months and a further 29% said they would prefer not to bleed at all [Citation30].
The high awareness and use of OCs demonstrated in this study reflects the findings of other studies [Citation20,Citation28]. The above quantitative study of 2544 women in Europe and the US [Citation28] found that women aged 25–44 were aware of a wide variety of contraceptive methods, but knowledge and usage of the pill and condoms dominated. Similarly, the international study assessing women’s attitudes to daily contraceptive use [Citation20] reported reasonable awareness of contraceptive methods, with a high level of pill use and a high level of satisfaction with its use. Use of LARC methods was low (8.5%); fears about pain (with IUC), fear of being able to feel an implant or concerns about efficacy cited as concerns by over a third of women [Citation20].
The high level of interest in information about LARC methods reflects the findings of the US Contraceptive CHOICE study, where 75% of study participants chose one of three LARC methods when provided with information on all contraceptive choices and methods were provided free of charge [Citation10]. Healthcare provider beliefs about lack of interest may limit the extent to which they share information about all contraceptive methods and artificially limit use of LARCs [Citation13]. The Contraceptive Use, Pregnancy Intentions and Decisions (CUPID) study of 3795 Australian women aged 18–23 years observed that women required consistent and accurate information that extended beyond OCs and often felt frustrated by the choice limitations imposed by their HCPs, particularly when they were seen to be linked to their age [Citation31].
The findings of the European TANCO study regarding satisfaction with the time and quality of contraceptive counselling contrast markedly with those of other studies which describe complaints by women about lack of time available to express their needs, lack of comprehensive information and a tendency towards provider–dominated interactions that fail to allow for women’s involvement [Citation32–35]. This discrepancy could be due to the design of the study; although anonymity was guaranteed, the women were recruited via their HCP and therefore were potentially prone to a social desirability or loyalty bias. However, this methodology was necessary to allow effective comparisons. The possibility of a loyalty bias is also supported by the apparent contradiction between satisfaction with counselling and the high levels of women’s interest in receiving further information about other contraceptive methods, including LARCs, a finding that is consistent with that reported by the US CHOICE study [Citation10].
Open questions and future research
Although valuable, the findings from this study point to larger, unanswered questions around the impact of social media and internet sources on women’s knowledge and use of contraception. Closer analysis of the larger sub-groups, such as nulliparous women, may also provide some useful data to compare with other studies on contraceptive use by this population.
Conclusions
The European TANCO study found contraceptive use to be generally high amongst women. However, awareness of a broader range of methods was lacking. The majority of women across Europe were using OCs; only 18% were using a LARC method. Despite high levels of satisfaction with current methods, women were interested in receiving more information about all contraceptive methods. This represents a good opportunity for HCPs to discuss use of LARCs, especially as our study showed only limited knowledge of these methods amongst respondents. When choosing a contraceptive method, women regarded reliability and safety as the two most important attributes. Greater exploration of women’s feelings regarding their needs and expectations of contraception could lead to expansion of knowledge, more effective discussions and greater likelihood of informed contraceptive choice for women. This will translate into higher satisfaction and continuation rates and, ultimately, may contribute to a decrease in the rate of unintended pregnancies.
Acknowledgements
This publication and its content are solely the responsibility of the authors. Medical writing assistance was provided by Lynn Hamilton of Clark Health Communications under the direction of the authors and paid for by Bayer AG.
Disclosure statement
Johannes Bitzer has worked as an Advisor for and received honoraria from Bayer AG, Merck, Teva, Exeltis, Lilly, Boehringer-Ingelheim, Vifor and Gedeon Richter. He has also given invited lectures and received honoraria from Bayer AG, Merck, Johnson and Johnson, Teva, Mylan, Allergan, Abbott, Lilly, Pfizer and Gedeon Richter.
Cecilia Caetano and Tobias Christian Porz are employees of Bayer.
Gabriele S. Merki-Feld has served as an adviser, given invited lectures or received research grants from Bayer AG, Merck/MSD, Teva, Gedeon Richter and Exeltis.
Additional information
Funding
References
- Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57:659–673.
- Dehlendorf C, Kimport K, Levy K, et al. A qualitative analysis of approaches to contraceptive counseling. Perspect Sex Reprod Health. 2014;46:233–240.
- Wyatt KD, Anderson RT, Creedon D, et al. Women’s values in contraceptive choice: a systematic review of relevant attributes included in decision aids. BMC Women’s Health. 2014;14:28.
- Donnelly KZ, Foster TC, Thompson R. What matters most? The content and concordance of patients’ and providers’ information priorities for contraceptive decision making. Contraception. 2014;90:280–287.
- Secura GM, Allsworth JE, Madden T, et al. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203:115.e1–117.
- Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117:1105–1113.
- Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45:301–314.
- Trussell J, Henry N, Hassan F, et al. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87:154–161.
- Monea E, Thomas A. Unintended pregnancy and taxpayer spending. Perspect Sex Reprod Health. 2011;43:88–93.
- Birgisson NE, Zhao Q, Secura GM, et al. Preventing unintended pregnancy: The Contraceptive CHOICE Project in review. J Womens Health (Larchmt). 2015;24:349–353.
- World Health Organization. Medical eligibility criteria for contraceptive use. 5th ed. Geneva: WHO; 2015.
- American College of Obstetricians and Gynecologists Committee on Gynecologic Practice; Long-Acting Reversible Contraception Working Group. ACOG Committee Opinion no 450: increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2009;114:1424–1428.
- Black A, Guilbert E, Costescu D, et al. Canadian contraception consensus (Part 3 of 4): chapter 7 – intrauterine contraception. JOGC. 2016;38:182–222.
- Faculty of Sexual & Reproductive Healthcare. Clinical Effectiveness Unit. Intrauterine Contraception. FSRH, [2007, updated 2015 Oct; cited 2017 Nov 23]. Available at: www.fsrh.org/pdfs/CEUGuidanceIntrauterineContraception.pdf.
- Black KI, Lotke P, Lira J, et al. Global survey of healthcare practitioners’ beliefs and practices around intrauterine contraceptive method use in nulliparous women. Contraception. 2013;88:650–656.
- Goldstuck ND. Reducing barriers to the use of intrauterine contraceptive device as a long acting reversible contraceptive. Afr J Reprod Health. 2014;4:15–25.
- Ihongbe TO, Mashow SW. Changes in the use of long-acting reversible contraceptive methods among U.S. nulliparous women: results from the 2006–2010, 2011–2013, and 2013–2015 National Survey of Family Growth. J Womens Health (Larchmt). 2017;27:245–252.
- Oppelt PG, Baier F, Fahlbusch C, et al. What do patients want to know about contraception and which method would they prefer?. Arch Gynecol Obstet. 2017;295:1483–1491.
- Spiedel J, Harper CC, Shiedls WC. Editorial. The potential of long-acting reversible contraception to decrease unintended pregnancy. Contraception. 2008;78:197–200.
- Mansour D. International survey to assess women’s attitudes regarding choice of daily versus nondaily female hormonal contraception. Int J Womens Health. 2014;6:367–375.
- Practice Committee of the American Society for Reproductive Medicine. Combined hormonal contraception and the risk of venous thromboembolism: a guideline. Fertil Steril. 2017;107:43–51.
- Piepert J, Madden T, Allsworth JE, et al. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120:1291–1297.
- Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404.
- Zapata LB, Steenlands MW, Brahmi D, et al. Effect of missed combined hormonal contraceptives on contraceptive effectiveness: a systematic review. Contraception. 2013;87:685–700.
- Egarter C, Frey Tirri B, Bitzer J, et al. Women’s perceptions and reasons for choosing the pill, patch, or ring in the CHOICE study: a cross-sectional survey of contraceptive method selection after counseling. BMC Women’s Health. 2013;13:9.
- Merki-Feld GS, Gruber IML. Broad counseling for adolescents about combined hormonal contraceptive methods: The CHOICE study. J Adolesc Health. 2014;54:404–409.
- Gemzell-Danielsson K, Cho S, Inki P, et al. Use of contraceptive methods and contraceptive recommendations among health care providers actively involved in contraceptive counseling – results of an international survey in 10 countries. Contraception. 2012;86:631–638.
- Johnson S, Pion C, Jennings V. Current methods and attitudes of women towards contraception in Europe and America. Reprod Health. 2013;10:7.
- Szarewski A, von Stenglin A, Rybowski S. Women's attitudes towards monthly bleeding: results of a global population-based survey. Eur J Contraception Reprod Health Care. 2012;17:270–283.
- Merki-Feld GS, Breitschmid N, Seifert B, et al. A survey on Swiss women's preferred menstrual/withdrawal bleeding pattern over different phases of reproductive life and with use of hormonal contraception. Eur J Contraception Reprod Health Care. 2014;19:266–275.
- Goldhammer DL, Fraser C, Wigginton B, et al. What do young Australian women want (when talking to doctors about contraception)? BMC Fam Pract. 2017;18:35.
- Buhling KJ, Klovekorn L, Daniels B, et al. Contraceptive counselling and self-prescription of contraceptives of German gynaecologists: results of a nationwide survey. Eur J Contraception Reprod Health Care. 2014;19:448–456.
- International Planned Parenthood Federation. Barometer of women’s access to modern contraceptive choice in 10 European Countries [June 2013; cited 2017 Nov 23]. Available from: http://www.ippfen.org/resource/barometer-womens-access-modern-contraceptive-choice-16-eu-countries-call-action.
- Isaacs JN, Creinin MD. Miscommunication between healthcare providers and patients may result in unplanned pregnancies. Contraception. 2003;68:373–376.
- Moos MK, Bartholomew NE, Lohr KN. Counseling in the clinical setting to prevent unintended pregnancy: an evidence-based research agenda. Contraception. 2003;67:115–132.