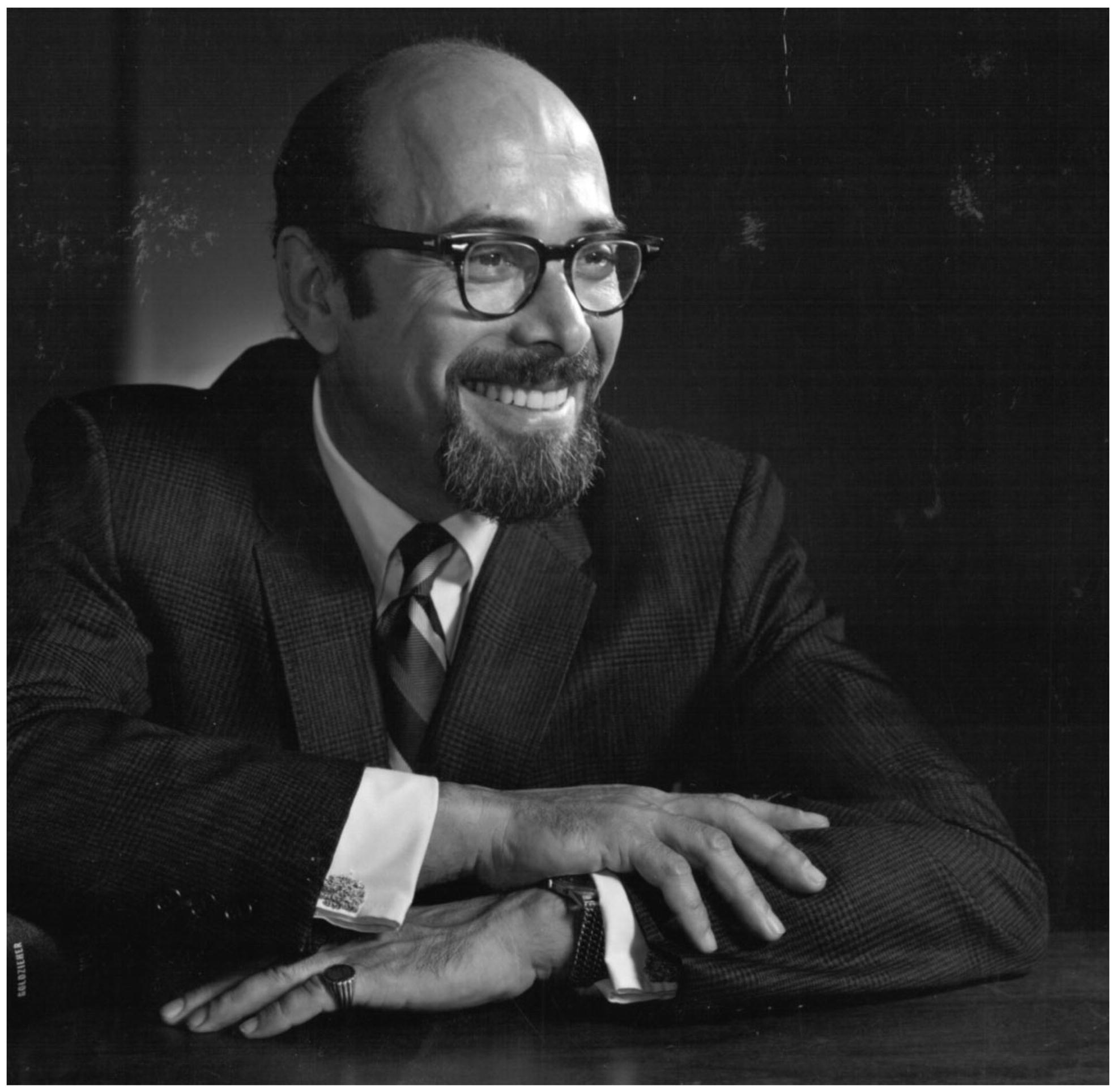
Joseph W. Goldzieher is the last survivor of the group of pioneers who, following the pivotal investigations of Gregory Pincus and his team [Citation1–3], transformed an idea into a never-ending series of orally administered hormonal contraceptives, universally known as ‘the pill’. They are utilized today by tens of millions of women.
Goldzieher was born on 21 September 1919, in Budapest, Hungary, into a family of famous scholars and physicians. With these admirable genes, he has today reached, in enviable condition, the longevity of one century. He is the father of a lady university professor who made good contributions in the field of international reproductive health; the grandfather of three accomplished women; and the great-grandfather of five great grandchildren already attending, or headed to, universities around the United States.
Ten years ago, when he turned 90, his life history and lifetime achievements were detailed in an Editorial in Contraception [Citation4]. For this reason, not to repeat ourselves, we decided to celebrate his 100th anniversary by highlighting his two most cited works and the lesson to be drawn from them.
Goldzieher has been a controversial figure throughout his long life and, intriguingly, in searching the Web, we found that the conclusions reached in his most widely cited report were later challenged. This article (226 citations as of the 1 January 2019) dealt with the polycystic ovary (PCO) and was published in 1962 [Citation5]. In reviewing the literature, with his co-worker JA Green, Goldzieher collected clinical, histologic and laboratory findings in 466 cases of surgically proven PCO and compared them with the findings in their own series of 39 similar patients. It is likely that the reason for the many citations was their surprising conclusion that ‘variability of the clinical features did not support the hypothesis of an associated syndrome’. They also concluded that histologic features failed to identify one, consistent entity, further illustrating a lack of homogeneity among published clinical series. It must be stressed that in those days, lack of ultrasound technology, made possible an exact diagnosis only in relatively advanced cases and therefore the treatment of choice was the so-called ‘wedge resection’ of the ovaries. In their series, this resulted in an improvement of menstrual regularity of 58% and in the studies reviewed from 6 to 93% of cases. In their series, following surgery a pregnancy rate of 33% was achieved, whereas data from the literature gave pregnancy rates between 13 and 95%, again stressing the heterogeneity of the clinical material evaluated. From the data collected (that included clinical findings and urinary steroid evaluation), they were unable to find markers capable of predicting the results of surgery. On the other hand, they found an occasional coexistence of a hyper adrenal state. This report was the first in a series in which Goldzieher and LR Axelrod evaluated specific aspects of the PCO [Citation6,Citation7].
Today, the concept of a ‘syndrome’ characterized by the presence of a PCO is an universally accepted notion and criteria have been laid down to identify variant forms [Citation8–10]. At the same time – as pointed out by Azziz [Citation11] – to be fair to Goldzieher and Green, heterogeneity of cases with PCO was evident from the very first description of seven advanced cases by Stein and Leventhal [Citation12]. In this original series, three women were obese, four hirsute (one obese), and one had acne.
The lesson to be drawn from this story is that, if scientific progress is a never-ending enterprise, such progress is also not linear at all. It is characterized by hypotheses, their testing and – more often than not – their eventual rejection for new theories. The PCO syndrome (PCOS) is a classic example of this, since today, a new theory involves genetic factors: genome-wide association studies have reproducibly identified a total of 19 shared genetic loci in subjects with PCOS [Citation13–15]. According to Day et al. [Citation16], only one locus differed significantly in its association by diagnostic criteria; otherwise, the genetic architecture was similar between PCOS diagnosed by self-report and today accepted diagnostic criteria.
Turning now the attention to Goldzieher’s second most cited work, we need to remind readers that he was the first to publish the results of a clinical trial with a long-acting injectable contraceptive progestin: depot-medroxyprogesterone acetate (DMPA) commercially known as Depo Provera [Citation17]. His Group was also the second in the world, to investigate ‘the pill’. Indeed, Pincus and his group published their first clinical experience with a combined oral contraceptive (COC) in 1958 [Citation2] and Goldzieher started his clinical work in Mexico during the following year, presenting his results for the first time at a Conference in New York in 1960 [Citation18]. This first contribution was followed by the publication of additional data in 1962, including the first ever information on return of ovulation following discontinuation [Citation19,Citation20]. What is important to remember is that he became a strong advocate of contraception, fighting all the early battles to protect womens’ reproductive rights and hormonal contraception from their many detractors [Citation21].
Given this background, it should not surprise that the second most cited article written by Goldzieher, definitely the one that made him known worldwide to clinicians and researchers working on hormonal contraception, dealt with COCs. Specifically, he and JP Realini put together a monumental review of the world literature on the possible association between COCs and cardiovascular diseases (As of 1 January 2019, cited 108 times) [Citation22]. They carefully reviewed all trials up to 1985, aiming at investigating the relationship of COC use with the occurrence of venous thromboembolism, stroke, myocardial infarction, and cardiovascular death. They included case-control, cohort, and mortality statistics studies in their evaluation. Of particular importance is their effort to evaluate study designs and possible shortcomings affecting conclusions.
Preliminarily, they observed that the majority of mortality statistics studies published up to 1985 offer little support for a relationship between COC use and the occurrence of cardiovascular diseases (CVD). In addition, they found major systematic problems in the epidemiologic studies, including potential for bias, in the detection of cardiovascular events and differences in the prognostic susceptibility of compared groups. This situation led to the conclusion that bias in the ascertainment of drug exposure was, at the time, an unresolved issue for most of the case-control studies. Finally, they felt that, because of possible biases arising from methodologic deficiencies, the validity of the observed associations between COC use and cardiovascular events should continue to be questioned.
We do not know how much Realini and Goldzieher critical evaluation influenced the design and conduct of all later epidemiologic studies. We know, however, that this critical overview helped contemporaries to critically assess the published data.
Venous thromboembolism (VTE)
The first possible association they investigated was that between current COC use and the incidence of VTE in women without predisposition. Such an association had been a nearly constant feature in all case-control and cohort studies after it was first presented in 1967 [Citation23]. While acknowledging this consistent finding, they pointed out to shortcomings in published studies. These included the fact that no investigation met accepted standards in addressing bias, or provided for equal medical surveillance of COC users and non-users in the target population.
Thirty-five years later, while the overall picture remains the same, a distinction is being made between COC containing different progestins, and a Danish cohort study of 2015 once more confirmed that, compared with non-users, the relative risk (RR) of confirmed VTE in users of COCs containing 30–40 µg ethinyl oestradiol plus levonorgestrel was 2.9 [95% confidence interval (CI) = 2.2–3.8]. The study also confirmed a higher RR when the progestin was desogestrel [6.6 (CI = 5.6–7.8)], gestodene [6.2 (CI = 5.6–7.0)] or drospirenone [6.4 (CI = 5.4–7.5)] [Citation24]. Therefore, a small increased risk of VTE in women using any kind of COC is considered a proven fact. Yet, the latest guidelines of the American Society for Reproductive Medicine clearly state: ‘In the patient in whom combined hormonal contraception is appropriate, it is reasonable to use any currently available preparation’ [Citation25].
Realini and Goldzieher also looked at mortality in COC users due to VTE. Here, their review found many different methods of examining trends and, while 7 studies found no relationship between COCs and death as a consequence of VTE (usually pulmonary embolism), 4 offered evidence of an increased RR.
More recently, a nation-wide case-control study in New Zealand estimated that current users of COCs had a RR of 9.6 (95% CI = 3.1–29.1) of having a fatal pulmonary embolism. The absolute risk of death from pulmonary embolism was estimated to be 10.5 per million woman-years [Citation26].
Stroke
The situation was more complex when they looked at the effect of COC use on the RR for various types of stroke. Here, several investigations found a significant association, while others did not. In addition, the diagnostic categories varied between studies, making generalisation difficult. Apparently, patients with some predisposition to cerebrovascular events were usually not investigated separately; the only study where this was done found an increase in the estimated RR for fatal cerebral VTE in non-predisposed subjects. It also found no statistically significant association for either all cases, or predisposed subjects [Citation27].
A recent Cochrane review of the risk of ischemic stroke in COC users compared to non-users found a RR of 1.7 (95% CI = 1.5–1.9) and the risk did not vary according to the type of progestin, whereas it seemed to increase with higher oestrogen dose preparations [Citation28].
Myocardial infarction (MI)
Already 35 years ago, many investigators had studied the possibility that COC use might increase the occurrence of MI. Results, however, were not uniform and national mortality statistics apparently offered no help in this regard. Of the 17 case-control studies evaluated by Realini and Goldzieher, data collection was judged unbiased in only 3 and no trial met the methodologic requirement of equal medical surveillance of COC users and no users. Only 1 study met the criterion of equal diagnostic examination for users and controls and gave a negative result. A total of 8 cohort investigations were examined and the conclusion was that their findings were mixed and performance was poor in terms of methodologic standards.
Today, there seems to be sufficient evidence of a small increase: a nationwide, population-based, case-control study published in 2001, found an odds ratio (OR) for MI among women who used any type of COC of 2.0 (95% CI = 1.5–2.8). Interestingly, OR was 2.5 (95% CI = 1.5–4.1) in users of II-generation preparations and 1.3 (95% CI = 0.7–2.5) among those who used III-generation ones [Citation29] and the above-mentioned Cochrane review found a RR for MI of 1.6 (95% CI = 1.2–2.1), also apparently increasing with higher oestrogen dose preparations [Citation28].
Mortality statistics studies attempting to correlate death by MI to the use of COCs were also analysed by Realini and Goldzieher, who concluded that they offered little support for the existence of a link.
Overall cardiovascular mortality
In the late sixties and seventies of the last century, the Royal College of General Practitioners (RCGP) initiated what remains the largest longitudinal study of COCs ever conducted; and in an early 1977 report they examined the death-rate from diseases of the circulatory system in women who had used oral contraceptives [Citation30]. They found that, overall, death-rate was five times that of never-use controls. Continuing use for 5 years or more led to a rate 10 times that of the controls.
Obviously, these observations were made in women who had used high-dose oestrogen COCs and, for this reason, Realini and Goldzieher focused on the only published case-control study addressing the global issue of cardiovascular mortality carried out by the World Health Organisation [Citation31] and concluded that its findings did not suggest an association. Their conclusion was supported already two years later by data from the USA where no deaths from CVD were reported among women who were COC users at the onset of their cardiovascular illness. For this reason, Authors concluded that the new formulation combined to greater care in prescribing COCs did substantially lower risks previously identified [Citation32].
Then, in 2010, a further analysis of the RCGP cohort provided strong additional evidence in support of the view that COC use does not increase the overall risk of a fatal complication. On the contrary, a net benefit was apparent [Citation33].
There seems to be a lesson to be learnt also from this publication by Joseph Goldzieher: Epidemiologic evidence is indirect and, as such, it must conform to strict rules to avoid bias and unsupported conclusions. At the same time, in making a judgement, each investigation must be taken into account and placed in its proper perspective. This seems especially the case when large studies combine a number of preparations containing different progestins and different dosages.
In this connection, the aphorism attributed to Claude Bernard comes to mind: “Scientific truth is an imaginary line dividing the error in two parts: the part we know is not correct and the part we still believe to be correct”!
We would like to conclude this brief presentation of Joseph W. Goldzieher as he turns the buoy of the first 100 years of his life with a simple: Happy Birthday Joe, and welcome to your second 100 years.
References
- Garcia CR, Pincus G, Rock J. Effects of three 19-nor steroids on human ovulation and menstruation. Am J Obstet Gynecol. 1958;75:82–97.
- Pincus G, Rock J, Garcia CR, et al. Fertility control with oral medication. Am J Obstet Gynecol. 1958;75:1333–1346.
- Pincus G. The hormonal control of ovulation and early development. Postgrad Med. 1958;24:654–660.
- Benagiano G. Joseph W. Goldzieher and the birth of hormonal contraception. Contraception 2010; 82:119–124.
- Goldzieher JW, Green JA. The polycystic ovary. I. clinical and histologic features. J Clin Endocrinol Metab. 1962;22:325–338.
- Goldzieher JW, Axelrod LR. The polycystic ovary. II. Urinary steroid excretion. J Clin Endocrinol Metab. 1962;22:425–430.
- Axelrod LR, Goldzieher JW. The polycystic ovary. III. Steroid biosynthesis in normal and polycystic ovarian tissue. J Clin Endocrinol Metab. 1962;22:431–440.
- Zawadzki JK, Dunaif A, Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In: Dunaif A, Givens JR, Haseltine FP, et al., eds. Polycystic ovary syndrome. Boston: Blackwell Scientific; 1992. p. 377–384.
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;8:19–25.
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004;19:41–47.
- Azziz R. Controversy in clinical endocrinology: diagnosis of polycystic ovarian syndrome: the Rotterdam criteria are premature. J Clin Endocrinol Metab. 2006;91:781–785.
- Stein IF, Leventhal ML. Amenorrhea associated with bilateral polycystic ovaries. Am J Obstet Gynecol. 1935;29:181–191.
- Chen ZJ, Zhao H, He L, et al. Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nat Genet. 2011;43:55–59.
- Shi Y, Zhao H, Shi Y, et al. Genome-wide association study identifies eight new risk loci for polycystic ovary syndrome. Nat Genet. 2012;44:1020–1025.
- Hayes MG, Urbanek M, Ehrmann DA, et al. Genome-wide association of polycystic ovary syndrome implicates alterations in gonadotropin secretion in European ancestry populations. Nat Commun. 2015;6:7502.
- Day F, Karaderi T, Jones MR, et al. Large-scale genome-wide meta-analysis of polycystic ovary syndrome suggests shared genetic architecture for different diagnosis criteria. PLOS Genet. 2018;14:e1007813.
- Zañartu J, Rice-Wray E, Goldzieher JW. Fertility control with long-acting injectable steroids. A preliminary report. Obstet Gynecol. 1966;28:513–515.
- Goldzieher JW, Moses LE, Ellis LT, A field trial with a physiological method of conception control. In: Kiser CV, editor. Conference on research in family planning, New York, 1960. Princeton (NJ): Princeton University Press; 1962. p. 351–356.
- Goldzieher JW, Moses LE, Ellis LT. Study of norethindrone in contraception. JAMA. 1962;180:359–361.
- Goldzieher JW, Rice-Wray E, Schulz-Contreras M, et al. Fertility following termination of contraception with norethindrone. Endometrial morphology and conception rate. Am J Obstet Gynecol. 1962;84:1474–1477.
- Goldzieher JW. Clinical evaluation of contraceptives: a great responsibility. Yearbook Gynecol 1965–1966:371–374.
- Realini JP, Goldzieher JW. Oral contraceptives and cardiovascular disease: a critique of the epidemiologic studies. Am J Obstet Gynecol. 1985;152:729–798.
- Royal College of General Practitionrs. Oral contraception and thromboembolic disease. J Roy Coll Gen Pract. 1967;13:267–279.
- Lidegaard Ø, Nielsen LH, Skovlund CW, et al. Risk of venous thromboembolism from use of oral contraceptives containing different progestogens and oestrogen doses: Danish cohort study, 2001–2009. BMJ. 2011;343:d6423.
- Practice Committee of the American Society for Reproductive Medicine Combined hormonal contraception and the risk of venous thromboembolism: a guideline. Fertil Steril. 2017;107:43–51.
- Parkin L, Skegg DC, Wilson M, et al. Oral contraceptives and fatal pulmonary embolism. Lancet. 2000;355:2133–2134.
- Inman WHW, Vessey MP. Investigation of deaths from pulmonary, coronary and cerebral thrombosis and thromboembolism in women of childbearing age. Brit Med J. 1968;2:193–199.
- Roach RE, Helmerhorst FM, Lijfering WM, et al. Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev. 2015;CD011054.
- Tanis BC, van den Bosch MA, Kemmeren JM, et al. Oral contraceptives and the risk of myocardial infarction. N Engl J Med. 2001;345:1787–1793.
- Beral V. Mortality among oral-contraceptive users. Royal College of General Practitioners' oral contraception study. Lancet. 1977;2:727–731.
- Belsey MA, Russel Y, Kinnear K. Cardiovascular disease and oral contraceptives: a reappraisal of vital statistics. Fam Plann Perspect. 1979;2:84–89.
- Porter JB, Jick H, Walker AM. Mortality among oral contraceptive users. Obstet Gynecol. 1987;70:29–32.
- Hannaford PC, Iversen L, Macfarlane TV, et al. Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners' Oral Contraception Study. BMJ. 2010;340:c927.
