Abstract
Objectives
The aim of this study was to explore the association between unintended pregnancy and related factors among congenital heart defects (CHDs) in infants.
Methods
A total of 1197 cases with isolated CHDs and 1125 controls without any abnormalities were analysed in this multicentre study at seven hospitals in China. According to the pregnancy intention, cases were divided into two groups: planned and unintended pregnancies. The adjusted odds ratio (AOR) was calculated by logistic regression analysis to assess the association between unintended pregnancy and CHD occurrence. The time to prepare for pregnancy and the influencing factors were also compared in this article.
Results
The risk for CHD occurrence was significantly associated with unintended pregnancy (AOR: 1.42; 95%CI: 1.16–1.73), which may increase the risks for each subtype of CHD occurrence. Risks such as parental smoking, housing renovation, accidental alcohol consumption, lack of health check-ups, and no folic acid supplementation before pregnancy were distributed differently among the planned and unintended pregnancy groups and were associated with CHD occurrence. However, there was no significant association between the duration of planned pregnancy and the risk of CHDs.
Conclusions
Unintended pregnancy increased the risk of CHDs in infants. This risk may be related to some known and unknown factors.
Synopsis
Some unintended pregnancy related factors may increase the risk for foetal CHDs. The duration of planning pregnancy may not be associated with the risk of CHDs.
摘要
目的:本研究的目的是探讨意外妊娠与婴儿先天性心脏病(CHDs)相关因素之间的关系。
方法:本文对中国7家医院1197例孤立性CHDs患者和1125例正常对照进行了多中心研究。根据妊娠意向将病例组分为计划妊娠和意外妊娠两组。通过Logistic回归分析计算调整后的优势比(AOR), 以评估意外妊娠与CHDs发生之间的关系。并对孕期准备时间及影响因素进行了比较。
结果:CHDs的发生风险与意外妊娠显著相关(AOR:1.42;95%CI:1.16∼1.73), 这可能增加各CHDs亚型发生的风险。父母吸烟、房屋翻新、意外饮酒、缺乏健康检查、孕前没有补充叶酸等风险在计划妊娠组和意外妊娠组中的分布不同, 与CHDs的发生有关。然而, 计划怀孕的持续时间和CHDs的风险之间没有明显的关联。
结论:意外妊娠会增加婴儿患CHDs的风险。这种风险可能与一些已知的和未知的因素有关。
概要:一些与意外妊娠相关的因素可能会增加胎儿先天性CHDs的风险。计划怀孕的持续时间可能与CHDs的风险无关。
Introduction
Congenital heart defect (CHD) is one of the most common birth defects caused by abnormal cardiovascular development of the foetal heart. According to a survey [Citation1], the prevalence of CHDs is 6–10 per 1000 births among all live births, with CHDs affecting an estimated 150,000 births per year in China. CHD is the leading cause of newborn deaths, and results in large economic and health burdens. Current studies suggest that CHDs are caused by genetic factors, environmental factors, or a combination of both [Citation2]. However, the aetiologies of most congenital heart disease cases are not clear.
The Centres for Disease Control and Prevention (CDC) defines unintended pregnancy as ‘a pregnancy that is reported to have been either unwanted (that is, the pregnancy occurred when no children, or no more children, were desired) or mistimed (that is, the pregnancy occurred earlier than desired).’ In this study, unintended pregnancy means the absence of pregnancy intention/plan before pregnancy. According to the statistics, approximately 208 million people around the world become pregnant each year, and approximately 41% of these pregnancies are unintended [Citation3]. Studies report that the prevalence of intended pregnancies ranges from one-third to one-half of all births [Citation4,Citation5].
Studies have shown that unintended pregnancy is associated with poor pregnancy behaviours [Citation6] and several adverse birth outcomes [Citation7,Citation8], including low birth weight, a shortened birth length and preterm birth [Citation9]. Many women with unintended pregnancies missing preconceptional care visits or delay their prenatal examination [Citation10]. For example, mothers with unintended pregnancies reported a greater likelihood of insufficient folic acid intake before pregnancy [Citation11], thereby placing their newborn at higher risk of developing neural tube defects [Citation12]. The study also showed that women with unintended pregnancies are at greater risk of alcohol exposure during the first trimester [Citation13], which increases the risk of abnormal foetal growth and morphogenesis [Citation14].
The prenatal period is a critical time for foetal development. The first three months before pregnancy are important for the development of germ cells, and the first trimester is a sensitive time for foetal organ formation. However, this timeframe is exactly the most easily overlooked period by women with unintended pregnancies. Although studies have shown that unintended pregnancy is associated with adverse pregnancy outcomes, there is no evidence on the correlation between unintended pregnancy and the risk of CHDs. Therefore, we conducted a multi-site hospital-based case-control study to assess the association between unintended pregnancy and CHDs.
Materials and methods
Study design
This programme was designed to be a hospital-based case-control study conducted in seven tertiary maternal and child hospitals in seven areas (Shenzhen, Fuzhou, Nanning, Wuhan, Xi’an, Chengdu and Zhengzhou) in China from July 2010 through October 2015. The case and control foetuses were diagnosed prenatally via echocardiography. Written informed consent was also obtained from each participant. This study was approved by the Ethics Review Committee of Sichuan University (ID: 201004).
Involvement and data collection
All participants underwent prenatal systematic ultrasonography at designated hospitals. When each pregnant woman fully understood the project and signed the consent form, a face-to-face questionnaire survey was conducted. The questionnaire comprised 8 parts: parental social demographics, living environment, lifestyle habits, work environment, maternal reproductive history, maternal illness and drug use history, maternal diet and nutrition, and maternal life events and mental state. Once a pregnant woman was recruited into the case group, anoher pregnant woman of similar gestational age but no abnormal foetus was selected at the same hospital as the control. Live cases and controls were followed up for 3 months after delivery. The questionnaire, ultrasound data (including static and dynamic images) and the clinical examination results were sent to the project team for review.
The final diagnosis of live birth was determined through the routine examination, heart auscultation or neonatal echocardiography by paediatric cardiologists. Stillbirth or abortion cases were finally diagnosed by pathological autopsy under informed consent. In addition, at least 4–5 national prenatal ultrasound specialists and paediatric heart specialists examined all static and dynamic echocardiography results among the CHD cases to ensure the accuracy of the final diagnosis.
Inclusion and exclusion criteria
The inclusion criteria for cases were as follows: (1) singleton pregnancies, (2) gestational age greater than 14 weeks, (3) foetal diagnosis of CHDs, and (4) confirmation of all foetal heart defects and malformations after birth or abortion. The cases included live births, stillbirths and abortions. The inclusion criteria for controls were as follows: (1) singleton pregnancies, (2) gestational age greater than 14 week, (3) no foetal diagnosis of CHDs or other congenital malformations. The exclusion criteria were as follows: (1) unclear diagnosis or confirmation of chromosomal abnormalities or syndromes by cytogenetic analysis in the case or control foetus, (2) case and control family history of CHDs, or (3) mental disorders in the mother.
Classification of cases
In this study, we included only isolated CHD cases, which means abnormalities with only cardiac malformations but without any other form of diagnosed noncardiac malformations.
All cardiac defect cases were classified into six subtypes based on the anatomic lesion: (1) septal defects, including atrial septal defects, ventricular septal defects, and endocardial cushion defects; (2) conotruncal defects, including transposition of great arteries, tetralogy of Fallot, truncus arteriosus, and double outlet right ventricle; (3) right-sided obstructive malformations, including pulmonary valve stenosis, pulmonary atresia, tricuspid atresia, and Ebstein anomaly; (4) left-sided obstructive malformations, including aortic valve stenosis, hypoplastic left heart syndrome and variants, coarctation of the aorta, and interrupted aortic arch; (5) anomalous pulmonary venous return, including total and partial anomalous pulmonary or systematic venous return; and (6) others, including single ventricle, heterotaxias, and other cardiac structural abnormalities.
Statistical analysis
A case–control analysis was performed to assess the association between unintended pregnancy and CHDs. Several potential confounders that are correlated with CHDs and unintended pregnancy, including maternal age, residence, pre-pregnancy maternal body mass index (ppM-BMI, body weight in kilograms/meter2), and history of adverse pregnancy, induced abortion, spontaneous abortion, premature birth, stillbirth or pregnancy with defects, are presented in . The chi-square test was used to calculate the difference in confounding factors between the case group and the control group. The logistic model was used to calculate the crude odds ratio (COR), adjusted odds ratio (AOR) and 95% confidence interval (95% CI) to assess the relative risk of CHDs. In the model, the presence or absence of CHDs was the dependent variable and unplanned pregnancy was the primary independent variable. The hospital distribution was set as a random intercept effect in the generalised linear mixed model.
Table 1. The maternal and paternal characteristics of case and control participants.
The trained personnel used EpiData 3.1 software to conduct parallel entry in pairs. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS version22.0, IBM). Two-tailed values p < .05 and a 95% CI that excluded 1.000 were considered to be statistically significant.
Results
From July 2010 to October 2015, 1535 women who had conceived foetuses with CHD and 1238 women who had conceived foetuses without any birth defects were enrolled in the study. Those who failed to meet the inclusion criteria were excluded, and 1197 cases and 1125 controls were ultimately analysed. The participant flow chart is shown in Supplementary Figure S1.
The parental characteristics of the case and control participants are summarised in . Most parental characteristics such as maternal age, residence, gravity, were significantly different between the mothers of cases and controls (p < .05), except for maternal pp-BMI and adverse pregnancy (p > .05).
Of the cases, 528 were planned pregnancies, and 669 were unintended pregnancies; in the control group, 655 cases were planned pregnancies and 470 were unintended pregnancies (see ). The mothers in the unintended pregnancy group had an increased risk of giving birth to offspring with CHDs (OR: 1.766; 95%CI: 1.50–2.08). After adjustment for confounders, the risks for developing CHDs was 1.42 (95% CI: 1.16–1.73).
Table 2. Association between unintended pregnancy and CHDs.
We further analysed the effects of unintended pregnancy on subtypes of CHDs (). Among the offspring with isolated cardiac defects, a significant association was observed between unintended pregnancy and offspring with septal defects (AOR: 1.50; 95%CI: 1.19–1.87), conotruncal defects (AOR: 1.47; 95%CI: 1.14–1.87), right-sided obstructive defects (AOR: 1.466; 95% CI:1.138–1.968), left-sided obstructive defects (AOR: 1.41; 95% CI:1.00–1.99), and anomalous pulmonary venous return (AOR: 1.54; 95% CI:1.06–2.23). Unintended pregnancy may increase the risk of developing each of the five types of congenital heart disease.
The results of multivariate logistic analysis of key periods of planned pregnancy and CHDs are shown in . There was no significant association between the duration of planned pregnancy and the risk of CHDs. We analysed the period when the pregnant women knew they were pregnant after last menstruation. There was no significant association between the time to awareness of the pregnancy and the risk of CHDs.
Table 3. Association between duration of planned pregnancy and CHDs.
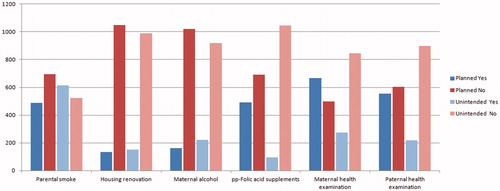
We analysed the probable influencing factors for the different risks of CHDs between the planned and unintended pregnancy groups, as shown in . It can be seen from the figure that parental smoking, housing renovation, maternal alcohol consumption, folic acid supplementation, and health examinations before pregnancy showed different distributions among the two groups. These indicators were also distributed significantly differently between the control and CHD groups ().
Table 4. Factors’ characteristics between case and control participants.
Discussion
Recent studies have shown that unintended pregnancy is associated with adverse pregnancy outcomes, including low birth weight, miscarriage, stillbirth, and neonatal death [Citation8,Citation15]. Unexpected pregnancy can significantly increase the risk of adverse pregnancy outcomes in offspring [Citation8,Citation9]. In this study, we found that unintended pregnancy was significantly associated with an increased risk of CHD in offspring. The risk may be related but not limited to factors such as parental smoking, housing renovation, accidental alcohol consumption, lack of health check-ups, and no folic acid supplementation before the unintended pregnancy.
The aetiology of most CHDs is still unknown. In this study, unintended pregnancy may increase the risk of offspring with CHDs. This risk may be related to factors such as parental smoking, housing renovation, accidental alcohol consumption, lack of health check-ups, and no folic acid supplementation before the unintended pregnancy. It was reported that several chromosomal anomalies, certain maternal illnesses, and prenatal exposure to specific environmental chemical contaminants are recognised risk factors [Citation16,Citation17]. It is believed that CHDs are the result of multifactor interactions, including the combination of environmental teratogens with genetic and chromosomal conditions [Citation18]. Existing epidemiologic studies have demonstrated that the risk of CHDs is related to the following factors: maternal age [Citation19], maternal lifestyle factors such as smoking (active smoking and passive smoking) [Citation20], intake of folic acid [Citation21], body mass index [Citation22] and psychological factors [Citation23] and environmental teratogen exposure [Citation24]. In our study, we analysed the probable related factors, such as parental smoking, housing renovation, accidental alcohol consumption, lack of health check-ups, and no folic acid supplementation before the unintended pregnancy. These factors showed different distributions among the unintended and planned pregnancy groups (p < .05). We further analysed the effect of unintended pregnancy on infant CHD occurrence after adjusting for the related factors listed above as confounding covariates (results shown in Supplementary Table S1). The AOR values were slightly lower than those after adjustments to only the demographic characteristics shown in the text. However, the AORs were still higher than 1, which means that those factors may be responsible for the increase in CHD occurrence associated with unintended pregnancy though this increase is not limited to these factors. Other factors such as work pressure, anxiety, illness and medication history, exposure to harmful substances, or nutrient supplementation [Citation17,Citation25], have also been reported to affect the occurrence of CHD. These differences may be due to differences in distribution among women planning to become pregnant. Therefore, the findings of this study may be just the tip of the iceberg.
On the other hand, many studies of unintended pregnancy have shown that mothers of unplanned pregnancies typically become aware of the pregnancy later than mothers of planned pregnancies [Citation6,Citation26]. For, those who do not want to become pregnant it may be impossible for the women to change their behaviours until the pregnancy is known. Intention to become pregnant may be an important determinant of risk. Unintended pregnancy has been associated with modifiable periconceptional exposures, including smoking and binge drinking and lack of preconceptional and prenatal vitamin use, and these are risk factors for CHDs. It can be reasonably inferred that the risk of unintended pregnancy increases CHD risk through a combination of multiple intermediate factors.
Although there are increased risks for other modifiable exposures (e.g., occupational exposures, environmental tobacco exposure, alcohol exposure,) among women who have unintended pregnancies, there is still a chance to change their behaviours, even if the opportunity comes late. This study showed that there was no significant association between the duration of planning for pregnancy and the risk of CHDs. Therefore, even a brief pre-pregnancy preparation is necessary.
Because adverse exposures and experiences of unwanted pregnancies may adversely affect embryos in the first few weeks of pregnancy, before most women know they're pregnant, a comprehensive preconception health care plan for women of childbearing age is recommended to protect the health of women and infants [Citation27,Citation28]. An important aspect of comprehensive preconception health care is attention to planned pregnancy [Citation27]. This study shows that there is no significant association between duration of planned pregnancy and the risk of CHDs, and the importance of planned pregnancy is also demonstrated.
The strengths and limitations
Our study has several strengths: (1) the cases in this study included live-born infants, stillbirths and terminated pregnancies, and the reported rate of CHDs is more accurate than those of other studies using live birth data; (2) the cases and controls in this study were recruited during pregnancy, and interviews were completed after prenatal diagnosis, which was significantly different from previous studies and may reduce reporting errors. However, this study also has the following limitations: (1) as a hospital-based case-control study, selection bias cannot be excluded; (2) in this study, information was collected by interviews, so recall bias and interviewer bias are a problem; and (3) Due to the relatively small sample size for CHD subtypes, a clearer conclusion for subtypes could not be obtained by statistical analysis A larger prospective study is needed to improve the efficacy of the analysis.
Conclusions
This study indicates that there is a significant association between unintended pregnancy and CHDs. There was no significant association between the length of planned pregnancy and the risk of CHDs. The findings underscore the importance of preventing unintended pregnancy and contribute to improving maternal and child health. Our findings may benefit public health organizations’ concerns and health education for unintended pregnancy, which can be used as a basis for effective interventions to reduce the risk of unintended pregnancy.
Author contributions
Jun Zhu and Xiaohong Li developed the study design and conducted the study; Zhen Liu and Ping Yu assisted in organising and implementing the project and drafting the manuscript; Meixian Wang performed data analysis and interpretation; Yan Tian and Qin Tang contributed to recruiting participants and diagnosing cases; Ying Deng, Nana Li, and Ping Yu participated in sorting, cleaning, and summarising the data. All authors read and approved the final manuscript.
Supplemental Material
Download MS Word (69.9 KB)Acknowledgements
We thank all participating families for their cooperation and for providing personal information. We thank the obstetricians, paediatricians, pathologists, experimental technicians and other participants involved in the project for recruiting the case and control participants and collecting the data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Zhao QM, Liu F, Wu L, et al. Prevalence of congenital heart disease at live birth in China. J Pediatr. 2019;204:53–58.
- Liu Y, Chen S, Zuhlke L, et al. Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. 2019;48(2):455–463.
- Singh S, Sedgh G, Hussain R. Unintended pregnancy: worldwide levels, trends, and outcomes. Stud Fam Plann. 2010;41(4):241–250.
- Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374(9):843–852.
- Rocca CH, Wilson MR, Jeon M, et al. Stability of retrospective pregnancy intention reporting among women with unwanted pregnancies in the United States. Matern Child Health J. 2019;23(11):1547–1555.
- Brown G, Parham DF, Harris L, et al. A survey of knowledge and practices regarding prevention of unintended pregnancies. J Physician Assist Educ. 2015;26(1):34–39.
- Flower A, Shawe J, Stephenson J, et al. Pregnancy planning, smoking behaviour during pregnancy, and neonatal outcome: UK Millennium Cohort Study. BMC Pregnancy Childbirth. 2013;13(1):238.
- Singh A, Singh A, Mahapatra B. The consequences of unintended pregnancy for maternal and child health in rural India: evidence from prospective data. Matern Child Health J. 2013;17(3):493–500.
- Lindberg L, Maddow-Zimet I, Kost K, et al. Pregnancy intentions and maternal and child health: an analysis of longitudinal data in Oklahoma. Matern Child Health J. 2015;19(5):1087–1096.
- Mastroiacovo P, Nilsen RM, Leoncini E, et al. Prevalence of maternal preconception risk factors: an Italian multicenter survey. Ital J Pediatr. 2014;40:91.
- Toivonen KI, Lacroix E, Flynn M, et al. Folic acid supplementation during the preconception period: a systematic review and meta-analysis. Prev Med. 2018;114:1–17.
- Dolin CD, Deierlein AL, Evans MI. Folic acid supplementation to prevent recurrent neural tube defects: 4 milligrams is too much. Fetal Diagn Ther. 2018;44(3):161–165.
- Roberts SC, Wilsnack SC, Foster DG, et al. Alcohol use before and during unwanted pregnancy. Alcohol Clin Exp Res. 2014;38(11):2844–2852.
- Zhu Y, Romitti PA, Caspers CK, et al. Maternal periconceptional alcohol consumption and congenital heart defects. Birth Defects Res A Clin Mol Teratol. 2015;103(7):617–629.
- Shah PS, Balkhair T, Ohlsson A, et al. Intention to become pregnant and low birth weight and preterm birth: a systematic review. Matern Child Health J. 2011;15(2):205–216.
- Jerves T, Beaton A, Kruszka P. The genetic workup for structural congenital heart disease. Am J Med Genet C Semin Med Genet. 2020;184(1):178–186.
- Kalisch-Smith JI, Ved N, Sparrow DB. Environmental risk factors for congenital heart disease. Cold Spring Harb Perspect Biol. 2020;12(3):a037234.
- Moreau J, Kesteven S, Martin E, et al. Gene-environment interaction impacts on heart development and embryo survival. Development. 2019;146(4):dev172957.
- Schulkey CE, Regmi SD, Magnan RA, et al. The maternal-age-associated risk of congenital heart disease is modifiable. Nature. 2015;520(7546):230–233.
- Zhao L, Chen L, Yang T, et al. Parental smoking and the risk of congenital heart defects in offspring: an updated meta-analysis of observational studies. Eur J Prev Cardiol. 2019;27(12):1284–1293.
- Li X, Li S, Mu D, et al. The association between periconceptional folic acid supplementation and congenital heart defects: a case-control study in China. Prev Med. 2013;56(6):385–389.
- Zhu Y, Chen Y, Feng Y, et al. Association between maternal body mass index and congenital heart defects in infants: a meta-analysis. Congenit Heart Dis. 2018;13(2):271–281.
- Meisgen S, Tingstrom J, Skog AA, et al. Environmental and lifestyle factors influencing risk of congenital heart block during pregnancy in anti-Ro/SSA-positive women. RMD Open. 2017;3(2):e520.
- Liu Z, He C, Chen M, et al. The effects of lead and aluminum exposure on congenital heart disease and the mechanism of oxidative stress. Reprod Toxicol. 2018;81:93–98.
- Nicoll R. Environmental contaminants and congenital heart defects: a re-evaluation of the evidence. Int J Environ Res Public Health. 2018;15(10):2096.
- Erfani A, Hosseini H, Nojomi M. Unintended pregnancies in Hamedan, Iran: levels and determinants. Women Health. 2019;59(3):318–333.
- Khoramrooz M, Rezapour A, Shirinbakhsh S, et al. Investigating changes in unintended pregnancies before and after the changes in the family planning policies in Iran: a multivariate decomposition analysis. Med J Islam Repub Iran. 2019;33:134
- Solanke BL, Kupoluyi JA, Akinyemi JO, et al. Do community characteristics influence unintended pregnancies in Kenya? Malawi Med J. 2019;31(1):56–64.