Abstract
Purpose
To explore the perceived need and enthusiasm for over the counter (OTC) progestogen-only pills (POP).
Materials and Methods
A web-based survey of 1000 sexually active women (16–45) and 100 pharmacists in Germany, Italy and Spain.
Results
Despite not wanting to conceive, 5–6% of women in each country were not using contraception and 8–20% were using methods less effective than condoms. At least 74% of respondents felt knowledgeable about the different contraceptives available but at least 1/3 had experienced difficulty accessing oral contraceptive (OCs) in the past two years. The cost of contraceptives, the need to see a doctor and long waits for appointments were cited as barriers for not using OCs. The majority agreed they would discuss with their doctor the decision to buy the POP, consult about side effects and other reproductive health issues. Over 2/3 of pharmacists in each country would be very, or fairly, likely to recommend the POP, agreeing that the benefits included improved access for women, and offered them more independence.
Conclusions
Asked directly, women in Germany, Spain and Italy currently using contraception are positive about a POP OTC. Pharmacists are also positive, with the overwhelming majority in favour of providing POPs.
摘要
目的:探讨人们对非处方药(OTC)单孕激素片(POP)的需求和热情。
材料和方法:对德国、意大利和西班牙的1000名性活跃女性(16-45岁)和100名药剂师进行网络调查。
结果:尽管不想怀孕, 但每个国家有5-6%的女性没有使用避孕方法, 8-20%的女性使用的避孕方法不如避孕套有效。至少74%的受访者对可用的不同避孕药感到了解, 但至少1/3的受访者在过去两年中遇到了口服避孕药(OCs)的困难。避孕药具的成本、看医生的需求和预约的长时间等待被认为是不使用口服避孕药的障碍。大多数人同意, 他们将与医生讨论购买单孕激素片的决定, 咨询副作用和其他生殖健康问题。每个国家超过2/3的药剂师都会非常或公平地推荐单孕激素片, 同意其好处包括改善妇女的获得机会, 并为她们提供更多的独立性。
结论:直接询问时, 德国、西班牙和意大利目前正在避孕的女性对单孕激素片非处方药持肯定态度。药剂师也持积极态度, 绝大多数人赞成提供单孕激素片。
Introduction
Despite widespread availability of modern methods of contraception in most European countries [Citation1], unintended pregnancy remains a public health problem [Citation2]. Access to the more effective contraceptives (hormonal and long-acting methods) involves seeing a healthcare provider (HCP), usually a doctor. Oral contraceptive pills (OCPs) are still the most widely used effective contraceptive in Europe [Citation1] and the arguments for making them available without the need for a prescription from a doctor (over the counter OTC) have been repeatedly rehearsed over the last thirty years [Citation3–5]. The recent approval in the UK of a progestogen-only pill (POP) for sale in pharmacies without the need to see a doctor [Citation6] has prompted renewed interest and enthusiasm in the subject. Aiming to determine the prevailing situation in three European countries, a survey was undertaken to explore, among both potential providers and users, the perceived need and enthusiasm for and concerns about, the proposal for a contraceptive pill over the counter. The survey explored views about OTC oral contraception in general but focussed more specifically on the progestogen-only pill. In this paper we report on current patterns of contraceptive use among consumers and the attitudes of both potential consumers and pharmacists to the idea of a POP being available OTC-only pill.
Materials and methods
The survey was commissioned by HRA Pharma (Chatillon, Paris) to explore the potential interest in a POP OTC in Europe. A series of qualitative interviews was undertaken initially in order to inform and build the content of the quantitative survey. Interviews were performed by IPSOS (3 Thomas More Square London E1W 1YW – UK). Thirty-six women in Germany (n = 12), Italy (n = 12), Spain (n = 12) aged 16–45 participated in an online community. They were sexually active with a male partner and not wanting to have children in the near future or ever. Quotas were set to include a spread of women currently using oral contraception, barrier, and fertility awareness methods and those not currently using oral contraception but open to using it in the future. Overall, the tasks lasted up to one hour and took place over 2 weeks between 5th and 19th July 2021. Web-assisted telephone depth interviews among 31 pharmacists in Germany (n = 11), Italy (n = 10) and Spain (n = 10) and six gynaecologists in Germany were undertaken between 15th and 28th July 2021. Pharmacists had to be regularly speaking to customers about oral contraceptives (at least one day/week) and dispense oral contraceptives to at least 5% of their monthly patient caseload. Gynaecologists had to see at least 15 patients regarding contraception in an average month, be based in an office practice (single or group practice) and dispense oral contraceptives to at least 5% of their monthly patient caseload. Both types of healthcare provider had to be in role for 3–30 years. Interviews for pharmacists lasted 30 minutes, gynaecologists (Germany only) were interviewed for 45 minutes. All interviews were undertaken in the interviewee’s native language.
The online quantitative survey was undertaken by IPSOS. Three thousand women aged 16–50 were recruited in Germany (n = 1000), Italy (n = 1000) and Spain (n = 1000). To be eligible for the study, women had to have reported having heterosexual sexual intercourse in the preceding 3 months and not wanting to conceive in the near future or ever. Post-menopausal women, women believing themselves to be infertile and those using permanent contraception were excluded from the study. Recruitment was through an online panel (Toluna, https://uk.toluna.com). Panel membership is voluntary and demographic data and lifestyle information are provided. For the survey, quotas were set by age and region in order to identify a sample representative of each country and data were weighted to bring the sample in line with the known population profile. Fieldwork took place between 11th November and 7th December 2021. The questionnaire was translated into participant’s native language and lasted 20 minutes. Three hundred community pharmacists were recruited from Germany (n = 100), Italy (n = 100) and Spain (n = 100)). Pharmacy assistants and hospital pharmacists were excluded from the survey. To be eligible for the study pharmacists had to have been qualified for 3–30 years and needed to be discussing oral contraception with clients on at least two days in a typical week and dispensing oral contraception at least once in a typical a week. Data were not weighted. Online survey lasted 15 minutes, were in the respondent’s native language and took place between 16th November and 2nd December 2021.
The survey included a range of question types, open numeric, single code, multi-code, and statement ratings and all multi-code list questions included an answer option ‘Other (please specify)’ giving respondents the option to type in their own answers. Both pharmacists and potential users were given information in the survey about POPs in general, including the fact that they contain only one hormone and no oestrogen, that they need to be taken every day without a break and that irregular bleeding is a common side effect. No type or brand of POP was specified in the survey and none were mentioned by name.
The final content of the questions was discussed with and finalised by Ipsos who administered the survey. The Consumer survey comprised a screener section (with questions on gender, age, region, sexual activity, contraceptive method, employment and education); questions on the ‘current landscape’ regarding the respondents’ usual contraceptive practice and experience; and questions about the switch of a POP to OTC availability. The survey for pharmacists comprised a screener section, questions on their perception of the current contraceptive landscape and nine questions on the possible OTC switch. The content of the survey is available as Supplementary material in Appendix 1 for consumers and Appendix 2 for the pharmacists.
The quantitative study was approved by an independent Institutional Review Board (IRB Pearl Pathways https://www.pearlirb.com). When invited to participate and in introduction to the questionnaire, respondents were advised on the length, content, and purpose of the survey and on where, how and why the data were to be stored; no personal information collected. Consent was collected at the beginning of the questionnaire through an electronic informed consent form but respondents were informed that they were free to decline to answer any question and to discontinue the survey at any time. Consumers were paid in panel points and pharmacists were paid differently per market through vouchers or prepaid Mastercard.
Results
Detailed demographic of consumers and pharmacists are shown in and , respectively. In all three countries around 10–12% of surveyed consumers were aged 16–20 years, while 49% in Germany, 52% in Italy and 47% in Spain were aged between 35 and 50 years. Forty percent or more respondents were employed full time, 13% (in Germany) to 17% (in Spain) were students and in all three countries around 55% had an annual gross household income of 20,000 to 69,999 euros. Around 70% in each country were currently living with a partner and at least one third said that their family was complete. Current method use by market and by age is shown in . Importantly, despite not wanting to get pregnant, 6% of women in Germany and Spain and 5% in Italy were currently using no method of contraception and 8% in Germany, 20% in Italy and 9% in Spain were using methods which are considered less effective than male condoms (such as withdrawal or periodic abstinence).
Figure 1. Current contraceptive method use by market and by age. SContraceptiveMethod. Which contraceptive method, if any, is your current primary method to prevent pregnancy? Base: Germany (n= 1,000), Italy (n=1,000), Spain (n=1,000). Barrier methods include: Male condoms, female condoms, contraceptive jelly/ cream/ foam/ sponge, diaphragm with/without spermicide; Long-acting methods include implant, injection, contraceptive patch, IUS/IUD (with or without hormone), vaginal ring; Natural methods include basal temperature, rhythm/ calendar, cervical mucus, fertility/ contraceptive app, withdrawal.
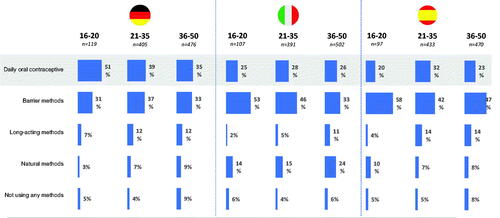
Table 1. Detailed demographic of women.
Table 2. Detailed demographic of pharmacists.
A minority of pharmacists was male (42% in Germany, 27% in Italy and 43% in Spain). Discussion/dispensing of oral contraceptives (OCs) was frequent: on average pharmacists in each country dispensed OCs to at least 25 patients in a typical week and in a typical week at least one third of them spoke about OCs to customers every day. In Germany 90% of pharmacists surveyed worked in a medium (6–10 employees) or large pharmacy (more than 11 employees) while in Italy 42% and in Spain 61% worked in small pharmacies with fewer than six employees the majority in inner city pharmacies.
Current contraceptive practice
Details of current contraceptive practice among women participating in the survey are shown in and shows the reasons for their current method choice. In all three countries the most common reason was ease of use. At least 50% of women in each country had ever used oral contraception and over 59% had used condoms. Twelve percent of women in Germany, 17% in Spain and 25% in Italy had ever used emergency contraception. The vast majority of women (69–73%) who had discussed contraception with their doctor agreed with the statement that they already knew what method they wanted to use before consulting their doctor about starting a method. Among those women who had used more than one contraceptive methods (n = 1777), over half in all three countries had first seen their doctor to discuss this, however fewer than 50% (46% in Germany, 37% in Italy, 42% in Spain) of women currently using non-hormonal methods discussed their decision with their doctor. At least 74% of respondents in each country agreed that they were knowledgeable about the different contraceptive methods available to them.
Table 3. Current contraceptive practice among women.
Table 4. Reasons for choosing current method.
Asked directly about access to oral contraception, over 90% of women in all three countries felt that easy access was important but not all agreed that access was easy in reality. Current OC users (n = 921) were asked whether they had experienced any difficulties in accessing their pill in the preceding two years. In all three countries at least one third (33%) had experienced some difficulty (). Challenges that consumers currently face regarding contraception included the cost of contraception, the cost of the consultations with a doctor, and long waiting times for doctor appointments. Some young women (aged 16–20) in Spain (n = 78), in Italy (n = 80) and Germany (n = 58) were not currently using oral contraception because it involves seeing a doctor (10–16%) or necessitates a gynecological examination (8% Spain, 8% Italy, 7% Germany). The primary benefit of a progestin-only oral contraceptive pill available to buy at the pharmacy without a prescription was ‘easier access’ in Germany and Spain and ‘no need to see a doctor’ in Italy.
Table 5. Difficulties with access to OC in the preceding two years.
A total of 300 respondents, when asked directly, admitted to having experienced an interruption in using their oral contraceptive pill because of an access issue (Germany (134), Italy (78), Spain (88). While 11% of these women (in Germany); 17% (in Spain) to 18% (in Italy) used emergency contraception, up to 19% did not use back-up contraception (19% in Germany, 16% in Spain, 9% in Italy) and a few got pregnant (12 in Germany, 2 in Spain, 4 in Italy).
Reactions to the concept of over-the-counter progestogen-only pill
Asked about their initial reaction to the proposal of a progestin-only pill at a pharmacy or online without a prescription, 49% of women in Germany, 55% in Spain and 65% in Italy were very positive or fairly positive (). At least one third (36% Germany, 42% Italy, 44% Spain) of the women felt that they would be very likely or fairly likely to switch their current contraceptive method should a POP become available OTC and over 40% would be likely to buy a POP from a pharmacy as back-up if they ran out of their usual contraceptive supplies. More than half of women in all three countries would have confidence in discussing the progestin-only oral contraceptive pill with their pharmacist. The main perceived benefits and the main concerns relating to a POP-OTC among consumers are shown in . Asked to imagine a scenario in which they were considering buying a POP over the counter, at least 75% of respondents in each country agreed that they would discuss this pill with their doctor before buying it and that they would go see their doctor if they were concerned about particular side effects. The vast majority of women agreed that they would go see their doctor for other women’s health issues not related to contraception (e.g., cervical and breast cancer screening) if they were using progestin-only oral contraceptive pill without prescription as their primary method of contraception.
Table 6. Reactions of women to switch.
Table 7. Benefits and concerns according to women.
Most of pharmacists (98% Germany, 98% Italy, 96% Spain) think that gaining easy access to hormonal contraception is important for women but some 10% in each country agree that gaining access is not currently easy (). More than half of pharmacists in Germany (59%) and Spain (57%), and 27% in Italy felt that restrictions for pharmacists to dispense oral contraceptives without a prescription was a main barrier to the optimal access of daily oral contraceptives. The cost of oral contraceptives was regarded as a main barrier to access by 47% of pharmacists in Italy and by 48% in Germany. Long waiting times for doctor appointments were highlighted by 48% of pharmacists in both Germany and Spain, and women not wanting to speak to a doctor about contraception (27% in Italy) or to have a gynecological examination (50% in Germany) were also considered to be barriers. In Germany 93% and Spain 90% and in Italy 80% of pharmacists feel that over-the-counter availability of POP would overcome existing barriers in the access of oral contraceptives at least to some extent. There were some differences between the views of male and female pharmacists. In Germany male and female pharmacists were equally likely to recommend the OTC POP, however female pharmacists felt the benefit was in terms of being able to offer women more contraception options, whereas men felt the benefit was a reduced cost burden for the healthcare system. In Italy male pharmacists were accepting of the OTC POP, feeling it would save women time. However, they were less likely to recommend the POP to all customer groups. Italian female pharmacists feel the OTC POP would reduce the use of emergency contraception and allow more women to get access to the contraceptive pill.
Table 8. The views of pharmacists.
Given a list of possible reactions to choose from, only 19% of pharmacists in Germany, 19% in Italy, and 11% in Spain reported feeling worried about the concept of a POP becoming available OTC (). Over two thirds of pharmacists in all three countries (69% in Germany, 66% in Italy and 79% in Spain) would be very likely or fairly likely to recommend it given that training will be available for this new method of supply at pharmacies. There was general agreement that the benefits of an OTC-POP included improved access for women, saving them time and giving them more independence. Over 60% of pharmacists in Italy and Spain felt that a reduction in the use of emergency contraception would be an important benefit. Around three quarters of pharmacists in each country felt that the availability to provide a POP without prescription would have a positive impact on their role.
When asked what the key challenges of an OTC progestin only pill would be, most pharmacists (76–82%) in each country felt that they would need additional training before they could provide the POP without a prescription. Pharmacists in Germany were most likely to worry about the lack of involvement of a doctor and 76% agreed with the statement that women who bought their contraceptive pill from a pharmacy may be less likely to attend their doctor for other women’s health issues (e.g., screening). In both Italy (56%) and Spain (48%) concern was expressed about possible misuse of the POP and in Italy (41%) about the ability of women to manage side effects. When asked about challenges pharmacists experience when discussing contraception, fewer than one in five pharmacists felt that there is no privacy in in their pharmacy to have these conversations and fewer than 15% of women in any country would be concerned about a lack of privacy in pharmacy if buying POP OTC. Overall, more than 87% of pharmacists responding to the survey already felt confident advising women on the different contraceptive methods available to them from their pharmacy and indeed at least 71% already did so. When asked specifically about their knowledge of the POP, slightly fewer (77–86%) felt knowledgeable about that particular method of contraception, particularly about suitability for women. However, at least 92% in each country would be encouraged to recommend the POP if they were to receive training on one of the following areas: the POP and different methods of contraception, how to assess customer suitability for the POP or side effects of POP.
Discussion
Findings and interpretation
The results of this survey suggest that women in Germany, Spain and Italy currently using contraception are generally positive about the concept of over the counter availability of a progestogen-only pill. Pharmacists too are generally positive, with the overwhelming majority in favour of extending their role to provide the POP to women.
Use of the POP varies by country in Europe. Reports rarely distinguish POP use from oral contraceptive use in general but in Sweden use of the desogestrel-POP accounts for around 10% of contraceptive use among teenagers and over 20% in women aged 45–49 [Citation7]. In some countries, such as Estonia, there is a trend towards decreasing use of combined pills in favour of POPs largely due to concern about the risk of venous thromboembolism associated with the former but not with POPs [Citation8]. Data from sales suggests that the POP accounts for 7% of the oral contraceptive market in Italy, 12% in Spain and 19% in Germany [Citation9].
Rapid and convenient access to oral contraception presently depends on rapid and convenient access to a doctor who will prescribe it. In this survey both consumers and pharmacists in all three countries identified difficulties in getting appointments with doctors often involving long waits. Delayed access to contraception can result in unintended pregnancy and indeed, when asked directly, a not insignificant number of women participating in the survey, particularly in Germany had experienced an interruption to the supply of OCs and a risk of pregnancy which could have been avoided were the POP to be available without the need to see a doctor.
Would women buy a POP OTC if one were available? Although most survey participants did not regard the need for a prescription as a barrier to access, certainly over 40% of respondents said they would be likely to use it as a back-up method if they ran out of supplies of their usual contraceptive. Some women too may consider switching to the POP from their current method because of the convenience that pharmacy access would provide. Anecdotally concern has been voiced that OTC availability of oral contraception might encourage switching from more effective methods of contraception, and/or might undermine efforts to encourage increased uptake of LARC. Desogestrel POP is likely as effective as a COC as it inhibits ovulation in almost every cycle and is thought to be more forgiving of incorrect use than POPs containing second generation progestogens [Citation10, Citation11], and for this reason has become the predominant POP in Europe [Citation7, Citation9]. Few women in the survey who were using a LARC would consider switching to a POP and, in any case, removal of their device would require intervention from a skilled health provider well placed to discuss alternative methods. Indeed the majority of respondents to the survey stated that they would discuss use of an OTC-POP with their usual healthcare provider before buying it. So the fear of a wholesale switch to ‘less effective methods’ seems unfounded. However, OTC-POP would offer women who found it difficult to get to see their doctor or who for some reason were reluctant to do so, to have access to a much more effective method of contraception than those currently available from pharmacies. Some women in the survey, particularly younger women, expressed reluctance to discuss contraception with a doctor, especially if the consultation involves a routine gynaecological examination, a procedure deemed in numerous guidelines as unnecessary and unhelpful. Health checks prior to prescribing, or as part of routine follow-up for hormonal contraception, often include breast and pelvic examination. A review of the evidence for the necessity of these examinations prior to starting hormonal contraception, concluded that both examinations have low detection rates for abnormality and may yield clinically irrelevant results, causing anxiety and inconvenience to the patient for no obvious gain [Citation12]. A more recent review concluded that pelvic examination findings do not affect the decision to prescribe or withhold systemic hormonal contraception [Citation13]. The World Health Organisation (WHO) (2008) distinguishes examinations and investigations that are essential for safe prescribing of contraception from those that ‘do not contribute substantially to safe and effective use of the contraceptive method’ but which are commonly done [Citation14]. US guidelines indicate that no examinations or tests are necessary before prescribing POPs; further recommend that no routine follow-up is necessary for safe and effective continued use of POP contraception for healthy women [Citation15].
Women do not need help from a doctor to ‘diagnose’ their need for a method of contraception, indeed it is the woman herself who tells the doctor that she is sexually active and not wanting to conceive. Some women may want or need help in choosing the most appropriate contraceptive, but the results of the survey demonstrate that most women feel that they are well informed about contraception in general and, indeed, that they already know which method they want to use when they visit their doctor. Moreover, the pharmacists who participated in the survey felt confident in advising women about contraception and would likely feel much more confident when specifically trained in providing a POP. Enhancing their role in providing sexual and reproductive healthcare would be likely to increase their interest in the subject particularly since many female pharmacists are using or have in the past used contraception themselves.
Instructions for use of the progestogen-only pill are extremely simple (take one pill at the same time every day). Incorrect use relates to missing pills and not taking mitigating action (e.g., abstaining from sexual intercourse or using a condom). Missing oral contraceptive pills is common [Citation16] but it is hard to argue that it would occur more commonly because the user had not seen a doctor before she started using taking the pills. Most contraceptive consultations with a doctor last less than 15 minutes and a lot of information about the POP must be given. In a Cochrane review of the effectiveness of interventions to improve OCP adherence neither direct in‐person counselling using either multiple counselling contacts or multiple components during one visit, nor intensive reminders of next dosing, resulted in improved adherence to daily dosing [Citation17].
When asked directly, the vast majority of women said that they would consult a doctor about unwanted side effects even if they had bought the POP over the counter. Training of pharmacists should include informing them of common side effects and when women should be advised to see a doctor. The commonest side effect of the POP is unscheduled vaginal bleeding [Citation18], a side effect which is obvious to women taking the pill and inconvenient rather than harmful.
Pharmacists in Italy and Spain in this survey were concerned about possible misuse of the POP. It is hard to imagine what form deliberate misuse might take and what would be the resulting harm since the POP is extremely safe [Citation18], and progestogens are not abortifacient [Citation19,Citation20]. Moreover, pharmacists felt that with additional training they could provide information to women sufficient to help them use the POP safely and effectively.
It has been suggested anecdotally that OTC OCs would lead to a reduction in the number of women attending for other sexual and reproductive health (SRH) care such as routine cervical screening. However, most survey respondents would continue to attend their doctor for other sexual and reproductive (SRH) problems and for routine screening. In any case women who rely on condom or periodic abstinence are not a captive population for routine screening, but systems are in place for encouraging these women to make use of SRH services. Among both the pharmacists and the consumers the idea that attending a doctor was a ‘good thing’ to do is prevalent. Although the trend in many countries is towards involving pharmacists in managing routine medical care [Citation21] the message seems to be slow in getting through.
Strengths and weaknesses of the study
All surveys have limitations. While we tried to render the sample representative of each country by age and region, the respondent pool for an internet survey can never be truly representative as it is self-selected with a bias towards people who are interested in the topic and excludes people without internet access or who have problems with literacy. Participants generally find it hard to engage in answering a very long questionnaire and questions asked towards the end of the survey may be answered with less thought. Closed-ended questions inevitably restrict the respondents in the expression of their views. Nevertheless, we sought the views of a large number of both consumers and pharmacists and the survey was done by an experienced and well-respected market research organisation.
Relevance and policy implications
The findings of this study suggest that making the POP available without the need to consult a doctor would be welcomed by both potential users and the pharmacists who would provide the method. The responses to many of the questions should provide reassurance to stakeholders, including regulatory agencies, that such a move would be unlikely to result in negative consequences, but would rather be positive both for individual women and for public health.
Unanswered questions and further research
To our knowledge this is the first study to explore views on the potential availability of a POP over the counter in Europe. There has been a multitude of studies on availability of emergency contraception OTC, including studies in Germany and Italy [Citation22,Citation23] however, discussion of EC-OTC is complicated by frequently raised issues of morality which, one hopes, would not be the case with OC. The only way to be certain of how people will behave when a medicine is reclassified to over-the-counter status is to reclassify it. The progestogen-only pill has recently been reclassified in the UK [Citation6] offering an opportunity for good quality research to determine whether and to what extent the POP can be used safely and effectively without input from a doctor.
Conclusions
Most women in Europe are familiar with oral contraception… Taking the pill is not difficult and the POP is a very safe method with very few absolute contraindications and no need for ongoing medical supervision [Citation14,Citation18]. The results of this survey suggest women would welcome improved access to an effective oral contraceptive pill and that pharmacists would be in favour of being able to provide it.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- United Nations, Department of Economic and Social Affairs, Population Division. 2019. Contraceptive Use by Method 2019: Data Booklet (ST/ESA/SER.A/435); [cited 2022 Mar 27]. Available from: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2019_contraceptiveusebymethod_databooklet.pdf.
- ESHRE Capri Workshop Group. Why after 50 years of effective contraception do we still have unintended pregnancy? A European perspective. Hum Reprod. 2018;33:777–783.
- Editorial. OCs OTC? Lancet. 1993;342:565–566.
- Grossman D, Grindlay K, Li R, et al. Interest in over-the-counter access to oral contraceptives among women in the United States. Contraception. 2013;88(4):544–552.
- American College of Obstetricians and Gynecologists. Over-the-counter access to hormonal contraception. Committee Opinion No 788. October 2019; [cited 2022 Mar 30]. Available from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/10/over-the-counter-access-to-hormonal-contraception.
- Glasier A. Oral contraception over the counter at last: a momentous occasion. BMJ Sex Reprod Health. 2022;48(1):1–2.
- Lindh I, Skjeldestad FE, Gemzell-Danielsson K, et al. Contraceptive use in the Nordic countries. Acta Obstet Gynecol Scand. 2017;96(1):19–28.
- Kurvits K, Laius O, Uusküla M, et al. Trends in the use of hormonal contraception in Estonia 2005–2019 and the risk of arterial and venous thromboembolism: a population-based study. Eur J Contracept Reprod Health Care. 2021;26(5):413–420.
- IQVIA Midas 2021. data on file.
- Rice CF, Killick SR, Dieben T, et al. A comparison of the inhibition of ovulation achieved by desogestrel 75 micrograms and levonorgestrel 30 micrograms daily. Hum Reprod. 1999;14(4):982–985.
- Korver T, Klipping C, Heger-Mahn D, et al. Maintenance of ovulation inhibition with the 75-microg desogestrel-only contraceptive pill (Cerazette) after scheduled 12-h delays in tablet intake. Contraception. 2005;71(1):8–13.
- Scott A, Glasier AF. Are routine breast and pelvic examinations necessary for women starting combined oral contraception? Hum Reprod Update. 2004;10(5):449–52452.
- Westhoff CL, Jones HE, Guiahi M. Do new guidelines and technology make the routine pelvic examination obsolete? J Womens Health. 2011;20(1):5–10.
- World Health Organization. Selected practice recommendations for contraceptive use. 2008. update. Geneva, Switzerland: World Health Organization; 2008. Available from: http://whqlibdoc.who.int/hq/2008/WHO_RHR_08.17_eng.pdf.
- Qaseem A, Humphrey LL, Harris R, et al. Clinical guidelines committee of the American college of physicians screening pelvic examination in adult women: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2014;161(1):67–72.
- Hou MY, Hurwitz S, Kavanagh E, et al. Using daily text-message reminders to improve adherence with oral contraceptives. A randomized controlled trial. Obstet Gynecol. 2010;116(3):633–640. Erratum inObstet Gynecol 2010;116:1224.
- Mack N, Crawford TJ, Guise JM, et al. Strategies to improve adherence and continuation of shorter‐term hormonal methods of contraception. Cochrane Database Syst Rev. 2019;4(4):CD004317.
- Faculty of Sexual & Reproductive Healthcare Clinical guidance, Progestogen-only Pills (March 2015, Amended April 2019), Available from https://www.fsrh.org/standards-and-guidance/documents/cec-ceu-guidance-pop-mar-2015/.
- Lalitkumar PG, Lalitkumar S, Meng CX, et al. Mifepristone, but not levonorgestrel, inhibits human blastocyst attachment to an in vitro endometrial threedimensional cell culture model. Hum Reprod. 2007;22(11):3031–3037.
- Lalitkumar PG, Berger C, Gemzell-Danielsson K. Emergency contraception. Best Pract Res Clin Endocrinol Metab. 2013;27(1):91–101.
- Christopher J. The changing role of the pharmacist in the 21st century. The Pharmaceutical Journal, PJ. 2018;300:7909.
- Meier S, Giannone A, Umberger A, et al. Messaging and access strategies for improving emergency contraceptive knowledge and uptake among italians. Eur J Contracept Reprod Health Care. 2022;27(2):166–172.
- von Rosen FT, von Rosen AJ, Müller-Riemenschneider F, et al. Awareness and knowledge regarding emergency contraception in Berlin adolescents. Eur J Contracept Reprod Health Care. 2017;22(1):45–52.
