Abstract
Purpose
Explore perceived access to, the need for, use of, and satisfaction with telemedicine services for contraceptive counselling and prescription-renewal-only during the COVID-19 pandemic, and the impact of the COVID-19 pandemic period on the choice and use of contraceptives.
Materials and methods
Internet-based e-survey of Swedish women of fertile age, 16–49 years.
Results
In total, 1016 participants completed the survey. Most participants (69.7%) rated their access to contraceptive services ‘as usual’. Among the remaining participants, a higher proportion rated their access as deteriorated (73.4%) compared to improved (26.6%; p < 0.001). In total, 38.0% reported a need for contraceptive counselling, whereof 14.0% had used telemedicine for counselling and reported high satisfaction. Telemedicine for prescription-renewal-only was used by 15.1% of the total population. Two per cent reported use of another contraceptive than their intended, whereof long-acting reversible contraceptives were the most common intended method. The proportion of current contraceptive users was lower than in 2017 (62.4% vs 71.1%, p < 0.001), and current users of long-acting reversible contraception decreased from 30.6% to 19.3% (p < 0.001).
Conclusions
During the COVID-19 pandemic period, most women found their access to contraceptive services unaffected, but more women felt that it had deteriorated than improved. The use of telemedicine was low, and the use of contraception overall fell. Efforts are needed to raise awareness of available services, and TM-provided interventions for maintained quality of care and informed decision-making remain to be evaluated.
The COVID-19 period imposed a change in contraceptive service provision, and efforts are needed to raise awareness of available services, including telemedicine. Access to all contraceptives, including LARCs, is crucial and telemedicine-provided interventions need evaluation.
SHORT CONDENSATION
摘要
目的:探讨在新冠肺炎疫情期间, 对远程医疗避孕咨询和处方更新服务的可及性、需求、使用和满意度, 以及新冠肺炎疫情时期对避孕药具选择和应用的影响。
材料和方法:基于互联网的16-49岁瑞典育龄妇女电子调查。
结果:共有1016名参与者完成了调查。大多数参与者(69.7%)认为她们获得避孕服务的机会“照常”。在其余参与者中, 较高比例的人认为她们获得避孕服务的机会减少(73.4%), 而不是提升(26.6%;p<0.001)。总体而言, 38.0%的人报告需要避孕咨询, 其中14.0%的人采用远程医疗进行咨询, 并报告满意度很高。15.1%的总人口应用仅用于处方更新的远程医疗。2%的人报告应用了超出她们预期的避孕药具, 其中长效可逆避孕药具是最常见的预期方法。目前避孕药具应用者的比例低于2017年(62.4% vs 71.1%, p<0.001), 目前长效可逆避孕药应用者从30.6%下降到19.3%(p<0.001)。
结论:在COVID-19大流行时期, 大多数妇女发现她们获得避孕服务的机会没有受到影响, 但认为情况恶化的女性多于认为情况改善的女性。远程医疗的应用率很低, 避孕措施的应用总体下降。需要努力提高对现有服务的认识, TM为保持护理质量和知情决策提供的干预措施仍有待评估。
短评
COVID-19时期改变了避孕服务的提供, 需要努力提高对现有服务的认识, 包括远程医疗。获得包括LARCs在内的所有避孕药具至关重要, 远程医疗提供的干预措施需要评估。
Introduction
Sexual and Reproductive Health and Rights (SRHR), including contraception, have been defined as ‘fundamental to people’s health and survival, to economic development, and the wellbeing of humanity.’ [Citation1] Unplanned pregnancy results in adverse outcomes such as poor health, lower income, and exposure to social and psychological vulnerability. [Citation2]
In March 2020, the WHO declared the COVID-19 pandemic, leading Sweden to introduce recommendations aimed at reducing social interactions. These recommendations included working from home, reducing public transport usage, and implementing quarantine rules for individuals with COVID-19 symptoms or positive test results. It’s important to note that Sweden did not impose lockdowns; instead, all restrictions were advisory and not legally enforced. Large public events or gatherings were prohibited as permits were not granted, but private events remained unregulated.
After the WHO pandemic declaration, publications followed that addressed the risk of disruption of SRH services, including contraception, forecasting a potential surge in unmet need for contraception and unwanted pregnancies. [Citation3] According to the WHO, family planning was one of the most frequently disrupted essential health service. [Citation4] To limit the risk of spreading the disease, healthcare systems were motivated to rapidly adapt and shift from in-person meetings to online services, generally referred to as telemedicine (TM) [Citation5,Citation6]. In Sweden, contraceptive services, including counselling and prescription, are free of charge and mainly provided by trained registered nurse-midwives at youth clinics and maternal health clinics. There are no official statistics on the national coverage of TM at youth clinics. According to unpublished statistics retrieved from the Swedish pregnancy registry, during the COVID-19 pandemic years 2020 and 2021, TM via video calls for contraceptive services at maternal health clinics were available in 15 out of 21 (71.4%) Swedish health care regions. Among regions providing TM, some had full coverage of TM (all clinics), while others had limited coverage (few clinics). In total, during 2020 TM vas provided by 173/573 (30.2%) maternal health clinics. During 2021, the corresponding figure was 144/522 (27.6%). In a Swedish survey study among patients seeking abortion, 4% (23/517) reported that the COVID-19 pandemic had affected their access to contraception. [Citation7]
Although TM has the potential to expand access to hormonal contraceptives, which do not need an in-person physical exam, increased access during the COVID-19 pandemic period was not perceived by all. [Citation8] Also, the uptake of long-acting reversible contraception (LARC) requires physical visits for placement, and a drop in the use of LARC was feared and subsequently a fact. [Citation9] In the UK, this drop in LARC provision was also seen among abortion patients when telemedicine for early medical abortion at home was introduced, where less than half of those requesting a LARC received one [Citation10]
In June 2021, we performed a nationwide e-survey with the primary objective to explore current use and attitudes towards contraceptive use in Sweden. [Citation11] In this publication we present the secondary objectives of the e-survey to explore the access to contraceptive counselling and prescription renewal, use of telemedicine for contraceptive services, and the impact of the COVID-19 pandemic period on choice and use of contraceptive methods. In addition, we compare the use of different contraceptives to our previous nationwide random-sample telephone-surveys conducted in 2013 and 2017. [Citation12,Citation13]
Reporting follows the CHERRIES checklist for internet e-surveys. [Citation14]
Material and methods
A web-based e-survey carried out by Kantar SIFO, specialised in global market surveys, among panellists in the SIFO-panel which include approximately 100,000 individuals recruited through nationally representative surveys on a random sample (i.e., no self-admission; S1, Supplementary information about the SIFO-panel). The sample size was based on the experiences from our previous surveys, [Citation12,Citation13] and the assumption that appoximately 1000 participants would be sufficient to carry out the proposed subgroup analyses. In the target population, women of fertile age, the sample frame was set at women aged 16 to 49 years and matching individuals received an invitation to the e-survey and a unique access link via email. The study information included the objectives of the e-survey, the estimated completion time of 15 min, voluntariness in participation and answering questions, the possibility to quit taking the e-survey at any time, and that the researchers would only receive coded and anonymised data. After this information, women consented to participate by continuing the e-survey. After reaching the target sample size of 1000 participants, the e-survey closed. The full description of the methodology has been previously published. [Citation11]
The e-survey’s structure and questions were modified from our previous surveys. [Citation12,Citation13] For this paper, we included supplementary questions related to the COVID-19 pandemic period. These questions aimed to explore the participants’ need for contraceptive counseling, access to different forms of contraceptive services, use of and reasons for choosing TM services for contraceptive counseling or prescription renewal only, and their satisfaction with contraceptive counseling through TM, rated on a scale from ‘very good’ to ‘very bad.’ Furthermore, participants were asked about the COVID-19 pandemic’s impact on choice and use of contraceptive methods. The collected data refer to the period occurring 12 months prior to completing the e-survey, covering June 2020 to June 2021 to reflect the COVID-19 pandemic period.
Statistical analysis
No power calculation to estimate the sample size needed to detect any potential differences during the COVID-19 pandemic period was undertaken. Descriptive statistics were used to display frequencies. Participants reporting affected access to contraceptive counselling and prescription were dichotomised (much easier/somewhat easier = improved; much more difficult/somewhat more difficult = deteriorated) and analysed by a non-parametric Chi-square test. Group differences and the comparison of use of contraception in the current 2021 population vs. the 2017 population were analysed by Chi-square and Fisher’s exact tests with two-sided p-values less than 0.05 as the significance level. Data were analysed with SPSS Statistics version 28 (IBM, Armonk, NY, USA).
Ethical approval
This study was designed so that no personal data was collected, and without any intentions to handle personal data information. Since all data was de-identified immediately upon entry, neither the data base at Kantar Sifo nor the data base that was sent to the commissioner of the report included any personal data (such as name or personal identifier number). Thus, tracing to a specific individual was not possible and this e-survey required no ethical approval according to Swedish ethics review act. A general statement that ethical review is not required for studies in which no personal data will be collected is openly available on the Swedish Ethical Review Authority’s website, hence no official letter explaining the waiver of the ethical appraisal was needed. Informed consent for participation was by continuing the e-survey after the initial information.
Results
On June 9th 2021, the invitation was sent to 9341 panellists, whereof 1084 started the e-survey. By June 18th, 1016 participants had completed the e-survey, whereafter it closed. The Prisma flow chart and tables of demographic characteristics have been previously published [Citation11], but can be seen in the supplementary material S2 and S3. The distributions of the main contraceptive method used during the last 12 months among current contraceptive users (n = 634) are presented in .
Table 1. Distribution of different contraceptives among current users by the method used during the last 12 months prior to the e-survey.
Access to contraceptive counselling and prescription renewal
Among the participants, 630/1016 (62.0%) stated that they did not need contraceptive counselling or prescription renewal during the COVID-19 pandemic period, with the highest proportion among women aged 40+ (79.4%) followed by 30–39 (67.8%). Among the remaining 386 (38.0%) participants who reported a need for contraceptive services, access to counselling or prescription renewal during the pandemic period was rated ‘as usual’ by 69.7% (n = 269), ‘somewhat more difficult’ by 17.1% (n = 66), ‘somewhat easier’ by 3.9% (n = 15), and ‘much easier’ by 3.6% (n = 14) or ‘much more difficult’ by 3.6% (n = 14). Eight participants (0.8%) preferred not to answer. When the rated access was dichotomised, a higher proportion rated their access as deteriorated (73.4%, 80/109) compared to improved (26.6%, 29/109; p < 0.001). Results were independent of sociodemographic characteristics.
Use of telemedicine for contraceptive services during the pandemic
Among the participants who reported a need for contraceptive counselling (n = 386), 84.2% (n = 325) were currently using contraception, 5.7% (n = 22) had stopped their method the last 12 months, and 10.1% (n = 39) were non-users. The need and use of TM for contraceptive services in different age groups are presented in . Contraceptive counselling through TM services was received by 14.0% (54/386), with a proportion of 49/347 (14.1%) among participants with current use or cessation within the last 12 months, and 5/39 (12.8%) among non-users. Most women (44/54, 81.5%) rated TM counselling as very good or rather good, whereas 14.8% (n = 8) had no opinion. A total of two women found the counselling ‘very bad’. The experience was independent of age (p = 0.29).
Table 2. Need for contraceptive counselling and use of TM for contraceptive services, by age group.
TM services for prescription-renewal-only (i.e., without preceding contraceptive counselling), were used by 15.2% (154/1016) of all participants. The corresponding proportion was 20.7% (143/691) among participants with current use of contraception or cessation in the last 12 months. Prescription-renewal-only via TM differed between age groups, with the highest proportion among participants aged 16–20 years (). Among those who had received contraceptive counselling via TM, 50.0% (27/54) reported also having used TM for prescription-renewal-only. All reasons for choosing TM for contraceptive services are presented in .
Table 3. Reason for choosing telemedicine for contraceptive services, by contraceptive counselling and prescription-renewal-only.
Impact of the COVID-19 pandemic on choice and use of contraceptive methods
In total, 59.1% (600/1016) of all participants stated that their contraceptive use was not affected by the pandemic, while 5.5% (56/1016) changed their method but stated it was not due to the COVID-19 pandemic. However, 2.0% (20/1016) stated that the pandemic had made them choose another contraceptive method than their intended one, whereof 17/691 (2.5%) among those reporting current use or cessation during the last 12 months. The most common characteristics of those women were: age groups 21–29 years (n = 7) and 30–39 (n = 9); university (n = 12) or high school (n = 5) level of education; married or co-habiting with children (n = 11) or living at home with their parents (n = 4); yearly household income ranging from 30 000–70 000€ (n = 10) and 70 000€ or more (n = 4) white collar (n = 9) or blue-collar (n = 5) workers (other results not shown due to few cases in each category). Among the 20 participants using another method due to pandemic, the most common intended methods were LARC (35.0%, 7/20), followed by SARC (30.0%, 6/20), and other methods (results not shown due to few cases for each method). Among those with an intended LARC use, one participant did use another type of LARC, and one relied on male sterilisation, while the rest used pills (n = 4) or coitus interruptus (n = 1).
Change in use of contraceptives
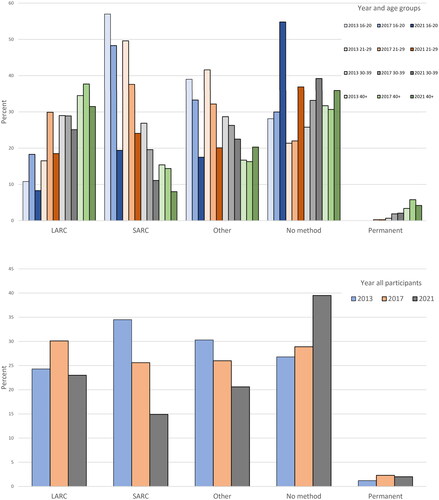
The use of contraceptives from 2013 to 2021 – grouped as LARC, SARC, Other, Permanent and No method – is presented in . The change in use from 2013 to 2017 has been previously published. [Citation13] The proportion of women reporting current use of any contraceptive method in the current population (634/1016, 62.4%) was lower than in 2017 (717/1008, 71.1%; p < 0.001). Whereas the overall decrease of SARCs did not differ significantly from 2017 (258/1008, 25.6%) to 2021 (225/1016, 22.1%; p = 0.069), overall use of LARC decreased from 311/1008 (30.6%) to 196/1016 (19.3%, p < 0.001), which represents a decrease of 36.9%.
Figure 1. Percentage of women using different contraceptive methods, by year and age group and by year among all participants.
LARC: long-acting reversible contraception; SARC: short-acting reversible contraception.
Other methods include; male condom, male condom combined with other, withdrawal, diaphragm, and emergency contraceptive pills.
In the 2013 and 2017 surveys, women could state all methods used during the last 12 months prior to completing the survey. In the current e-survey 2021, women could only state their mainly used method, hence, the overall percentage for 2013 and 2017 may exceed 100%.
Discussion
Findings and interpretation
In this nationwide e-survey on the use and access to contraception during the COVID-pandemic period, 38.0% of the participants needed contraceptive counselling or prescription renewal during the pandemic, whereof 14% had used TM for contraceptive counselling. In total, 15.2% had used TM for prescription-renewal-only. Although most participants stated their access to contraceptive services as unaffected, significantly more participants stated that their access had deteriorated compared to improved. A decrease in the overall current use of contraception was seen compared to our previous survey conducted in 2017. [Citation13] The use of SARC had not decreased, however, significantly fewer participants were using LARC.
In June 2018, TM for SRH services in contraceptive counselling and provision was introduced by public healthcare providers in the Stockholm region, the most populous region in Sweden. According to unofficial statistics retrieved from the public healthcare (accessible upon request to the authors), the mean number of online video consultations provided per month increased fivefold; from 335 in 2018 to 1757 in 2019. During the pandemic, the number of consultations remained high at 1558 in 2020 and increased to 2232 in 2021 (private healthcare providers not included). As reported by health professionals, the increase in online consultations was partly driven by a fear among both patients and healthcare professionals to meet in person. In our study population, the use of TM was highest in the younger age groups, reflecting the figures in the statistics, showing the highest use of TM among women aged 17–19 years (youth centre TM, patients aged 14–24) and 23–29 years (maternal health care TM, no lower age limit).
Although our results show that the COVID-19 pandemic period had some negative effects on access to contraceptive services in Sweden, the use of TM and high satisfaction with such services might have limited negative outcomes. The high proportion of women with unmet need for contraception in Sweden, estimated at 17.2% as previously published,[Citation11] could thus have been even higher without an already existing infrastructure for contraceptive counselling and prescription renewal via TM.
According to the official statistics on abortions conducted in Sweden, retrieved from the National Board of Health and Welfare, the total number of abortions decreased by 10.1% from 2017 to 2021, with the largest drop among the youngest women aged 15–24 years. A higher prescription rate and use of LARC in this age group have been stated as possible explanations. [Citation15] The abortion rates declined in 2021, most likely due to national COVID-19 recommendations on reduced social interactions during the pandemic. The effects of the decreased use of LARC in our study population on long-term abortion statistics are yet to be explored.
Results in the context of what is known
To limit the risk of spreading the SARS-CoV-2 virus, healthcare systems rapidly adapted, introducing or further developing already existing remote online services, generally called telemedicine (TM). TM has been used for several years across the healthcare spectrum,[Citation16] and is an important means to address inequity in access to healthcare in rural and remote areas. [Citation17] In our recent publication, we could show an overall decrease in the use of all methods and the unmet need for contraception rose from 15.2% in 2017 to 17.2% in 2021. [Citation11] In our previous surveys, participants could indicate all methods they had used in the 12 months preceding the survey, while in this survey they could only indicate their mainly used method. Although the results of the comparison need to be interpreted with caution, the proportion of LARC users from 2017 to 2021 fell drastically (-36.9%). [Citation11,Citation13] This drop is partly reflected in the figures from the Swedish register on dispensed pharmaceuticals, which showed a 6.3% decrease in the number of patients/1000 citizens aged 15–49 years who dispensed hormonal IUDs and implants from 2017 to 2021. [Citation18] Similar to our results, a French register study on dispensed contraceptives reported the largest drop in dispensation for LARC methods; 9.5% for the hormonal IUD, 8.6% for the Copper-IUD, and 16.4% for the implant, respectively. [Citation9] In another register-based study on contraceptive prescription during the 2020 lockdown in the UK, which took place from April to June 2020, prescriptions of implants were reduced by 75%, and of IUDs by 79%. [Citation19] In Brazil, however, another pattern in sales figures of LARC was seen. The number of sold implants and levonorgestrel-IUDs initially fell, but later rose simultaneously as the number of reported COVID-19 related deaths increased indicating a change in reproductive plans among couples with access to the private sector where most of the implants and levonorgestrel IUDs are provided. [Citation20] In Senegal, a similar trend in method mix shifting was seen, where more acceptors of LARCs were reported during the pandemic period compared to the prepandemic period. [Citation21] These register- and sales figure based studies show a change in prescribed, dispensed, sold, and provided contraceptives but do not necessarily reflect actual use. To monitor changes in actual use, surveys such as ours may provide a more accurate description. Worries about the potential risk of a global surge in unmet need as an effect of the COVID-19 pandemic[Citation3] is thus supported by our results, indicating that the rapid transition from in-person meetings to TM could not compensate for other factors such as restrictions and a high proportion of healthcare workers staying home due to symptoms of COVID-19.
A mere 2.0% of our participants used another contraceptive than their intended as a result of the COVID-19 pandemic period, and most of those women had intended to use LARC. As a comparison, an e-survey from the US showed that 21.6% of respondents would use another method if it were not for COVID-19. [Citation22] In our study, we saw that the use of another method was most common among well-educated, married, and employed women with higher incomes, whereas in the US, job- and income loss, and food insecurity were associated with the use of another method. [Citation22] The difference could be explained by the Swedish subsidy system, where all contraceptives are free up to 21 years of age and subsidised up to 25 years (annual cost of approximately 10€ for SARCs and 10€ total cost for LARC), whereas in the US access to contraceptives and out-of-pocket costs are highly dependent on health insurance coverage or qualification for government programs with costs up to 50$ per month for the pill, 300$ for the implant, and 1300$ for the IUD for those without insurance coverage (2021 figures). [Citation23]
Fortunately, in 2020 the 52 mg levonorgestrel hormonal IUD, which is the most used hormonal IUD in Sweden, received approval for extended use for up to 6 years for pregnancy prevention, and later up to 8 years. The extended duration of use will be clearly visible as a drop in the number of prescriptions and items dispensed but cannot fully explain the sharp decline in actual use over time. Besides what has already been discussed (national recommendations on limited social interactions, fear of physical meetings, and low use of TM services), other possible reasons for the decline in LARC use during the COVID-pandemic period could be that women during contraceptive counselling were not informed about LARC to the same extent as before or were motivated to choose another or to remain with their current method. However, the reasons need to be further explored.
Clinical implications
The low proportion of participants using TM despite a reported need for contraceptive services indicate a need for increased efforts to spread the information on available services to all women of fertile age to ensure access to contraception. In 2014, the Swedish Medical Products Agency included LARC as an option for first-time users including nulliparous women, [Citation24] which has since led to increasing use of LARC. This trend has now reversed, possibly explained by the restrictions in the context of the pandemic and changes in service provision shifting from in-person to online consultations. The negative trend in the dispensation and use of LARC needs to be addressed, and policymakers deciding over healthcare systems, need to offer both TM and in-person consultations and LARC provision also in the post-pandemic era.
Although studies show that TM improves access to health care, has positive effects on therapeutic outcomes and increased efficiency in health care services, there is a lack of knowledge and understanding of the long-term effects and costs related to TM [Citation16]. We argue that the cost-effectiveness of TM for contraceptive counseling is complex. Any model for cost calculation needs to take all potential effects of TM into account, including the uptake of different contraceptives, the risk of inconsistent use, contraceptive failure, and the subsequent occurrence of unplanned and unwanted pregnancies. Although the intention with the introduction of TM is increased accessibility with maintained quality of care, TM also means a lost opportunity to screen for sexually transmitted infection and intimate partner violence as privacy can never be guaranteed.
Research implications
Although TM for contraceptive services was not used by a high proportion in our sample, satisfaction with TM was high among users and merits further development and implementation. Implementation research is needed to evaluate how we can integrate TM into our healthcare system. Our research group have ongoing trials on TM for abortion services, based on findings that medical abortion can be safely performed and self-managed in the home of the patient. [Citation25,Citation26] There is a knowledge gap on the effects of TM on the uptake and continued use of all contraceptives, especially LARC since these methods still require placement by a skilled inserter at a physical clinic. We have previously shown that structured contraceptive counselling increases the use of LARC and could provide a means for identification of the need for LARC. [Citation27] In an era when TM is gaining momentum, there is an opportunity to adjust and evaluate in-clinic interventions that have proven to be effective in increasing the uptake of LARC [Citation27–29], for use in TM, while maintaining access to in-person provision and high use of LARCs.
Strengths and limitations
The strengths and limitations of the survey study method have been previously discussed. [Citation11] Briefly, the strengths of the e-survey are the large sample size of 1016 participants, the short data collection time (9–18th June 2021), and the low discontinuation rate, showing that the content of the survey was relevant to the invited participants. However, being an e-survey introduces selection bias, as the participants were recruited from an already existing panel of invited individuals who had previously participated in telephone surveys, showing their high interest in contributing to surveys. For this paper, a critical limitation is the difference in methodology from our previous telephone-based surveys, with vast differences in sociodemographic characteristics resulting in a less representative sample compared to the general population. In addition, participants in the previous surveys could state all methods used the last 12 months prior to taking the survey, while in the current survey they could only state their mainly used method. Hence, the analyses of differences in contraceptive use over the years must be interpreted with caution.
Conclusions
During the COVID-19 pandemic period, most women found their access to contraceptive services unaffected, however, more women found their access deteriorated rather than improved. The use of TM for contraceptive services was surprisingly low and efforts to raise awareness about TM in the fertile population are needed. Both TM and in-person encounters are still needed to meet patients’ needs, especially to make LARC provision readily available. TM-provided interventions to ensure comprehensive counselling with maintained quality, informed decision-making, and high patient acceptability in the long term remain to be evaluated.
Author contributions
The study was initiated by HKK and KGD. HKK, KGD and NE participated in the design of the survey. The analysis of the results was performed by NE and HKK. NE, KGD and HKK have participated in manuscript writing.
Supporting information titles
S1. Supporting information about the SIFO-panel.
S2. Supporting information, Flow Chart of the participants.
S3. Supporting information, Table of Demographic characteristics of participants by age group.
Supplemental Material
Download MS Word (16.4 KB)Supplemental Material
Download MS Word (25.7 KB)Supplemental Material
Download PDF (2.8 MB)Disclosure statement
Niklas Envall, Helena Kopp Kallner, and Kristina Gemzell Danielsson have received honorariums for giving lectures for Bayer. HKK and KGD have participated in the national and international medical advisory boards for Bayer. KGD is a member of the standing international Women’s Health Academy supported by Bayer. HKK and KGD have participated in trials sponsored by Bayer as principal investigators. The survey was fully sponsored with an unrestricted grant from Bayer Sweden AB, but the entity had no influence on the content of the survey nor in the writing of the manuscript. The authors received no personal compensation for conducting the study or manuscript writing. Outside the submitted work HKK and KGD receive honorariums for lectures on women’s health, contraception and fibroid care from Actavis, Gedeon Richter Exeltis, Nordic Pharma, Natural Cycles, Mithra, Teva, Merck, Ferring, Consilient Health, Norgine, and KGD also from Campus Pharma, Vifor, Daisy and Obseva/Theramex. HKK provides expert opinion for Evolan, Gedeon Richter, Exeltis, Merck, Teva, TV4 och Natural Cycles and is an investigator in trials sponsored by MSD, Mithra, Ethicon, Azanta and Gedeon Richter. HKK and KGD teach courses sponsored by Merck and MSD/Organon and Gedeon Richter.
Data availability statement
The data-set is available upon request to the authors.
Additional information
Funding
References
- Starrs AM, Ezeh AC, Barker G, et al. Accelerate progress-sexual and reproductive health and rights for all: report of the Guttmacher-Lancet commission. Lancet. 2018;391(10140):2642–2692. doi: 10.1016/S0140-6736(18)30293-9.
- Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32(1):152–174. doi: 10.1093/epirev/mxq012.
- Kumar N. COVID 19 era: a beginning of upsurge in unwanted pregnancies, unmet need for contraception and other women related issues. Eur J Contracept Reprod Health Care. 2020;25(4):323–325. doi: 10.1080/13625187.2020.1777398.
- World Health Organisation. Pulse survey on continuity of essential health services during the COVID-19 pandemic. Interim report. 2020.
- Keller L, Dawson R. Family planning providers show creativity and resilience in response to the COVID-19 pandemic. Guttmacher Institute, 2020. Available from: https://www.guttmacher.org/article/2020/06/family-planning-providers-show-creativity-and-resilience-response-covid-19-pandemic.
- International Federation of Gynecology and Obstetrics (FIGO). COVID-19 contraception and family planning 2020. Available from: https://www.figo.org/sites/default/files/2020-05/COVID%20contraception.pdf.
- Niemeyer Hultstrand J, Törnroos E, Gemzell-Danielsson K, et al. Induced abortion and access to contraception in Sweden during the COVID-19 pandemic. BMJ Sex Reprod Health. 2022;48(4):311–312. doi: 10.1136/bmjsrh-2022-201464.
- Yarger J, Hopkins K, Elmes S, et al. Perceived access to contraception via telemedicine Among young adults: inequities by food and housing insecurity. J Gen Intern Med. 2023; Feb38(2):302–308. doi: 10.1007/s11606-022-07669-0.
- Roland N, Drouin J, Desplas D, et al. Impact of Coronavirus disease 2019 (COVID-19) on contraception use in 2020 and up until the end of April 2021 in France. Contraception. 2022;108:50–55. doi: 10.1016/j.contraception.2021.12.002.
- Dixon A, Reynolds-Wright JJ, Cameron ST. Uptake of long-acting reversible contraception after telemedicine delivered abortion during covid-19. Eur J Contracept Reprod Health Care. 2022;27(4):284–288. doi: 10.1080/13625187.2022.2085680.
- Envall N, Wallström T, Gemzell Danielsson K, et al. Use of contraception and attitudes towards contraceptive use in Swedish women: an internet-based nationwide survey. Eur J Contracept Reprod Health Care. 2022;27:(5):409–417.
- Kopp Kallner H, Thunell L, Brynhildsen J, et al. Use of contraception and attitudes towards contraceptive use in Swedish Women – a nationwide survey. PLoS One. 2015;10(5):e0125990. doi: 10.1371/journal.pone.0125990.
- Hellstrom A, Gemzell Danielsson K, Kopp Kallner H. Trends in use and attitudes towards contraception in Sweden: results of a nationwide survey. Eur J Contracept Reprod Health Care. 2019;24(2):154–160. doi: 10.1080/13625187.2019.1581163.
- Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34.
- The National Board of Health and Welfare. Abortion statistics in Sweden 2021. 2022.
- Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79(11):736–771. doi: 10.1016/j.ijmedinf.2010.08.006.
- Bradford NK, Caffery LJ, Smith AC. Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. Rural Remote Health. 2016;16(4):4268.
- The National Board of Health and Welfare. Statistics on pharmaceuticals 2023; [cited 2023 23 March]. Available from: https://sdb.socialstyrelsen.se/if_lak/val.aspx.
- Walker SH. Effect of the COVID-19 pandemic on contraceptive prescribing in general practice: a retrospective analysis of English prescribing data between 2019 and 2020. Contracept Reprod Med. 2022;7(1):3. doi: 10.1186/s40834-022-00169-w.
- Charles CM, Munezero A, Bahamondes LG, et al. Comparison of contraceptive sales before and during the COVID-19 pandemic in Brazil. Eur J Contracept Reprod Health Care. 2022;27(2):115–120. doi: 10.1080/13625187.2022.2027364.
- Fuseini K, Jarvis L, Ankomah A, et al. Did COVID-19 impact contraceptive uptake? Evidence from Senegal. Stud Fam Plann. 2022;53(2):301–314. doi: 10.1111/sifp.12195.
- Diamond-Smith N, Logan R, Marshall C, et al. COVID-19's impact on contraception experiences: exacerbation of structural inequities in women’s health. Contraception. 2021;104(6):600–605. doi: 10.1016/j.contraception.2021.08.011.
- Alyssa Corso. How Much Does Birth Control Cost Without Insurance in 2021?, 2022. Available from: https://www.talktomira.com/post/how-much-is-birth-control-without-insurance.
- Swedish Medical Products Agency. Antikonception – behandlingsrekommendation. Information från läkemedelsverket. 2014;25(2):14–28.
- Schmidt-Hansen M, Pandey A, Lohr PA, et al. Expulsion at home for early medical abortion: a systematic review with meta-analyses. Acta Obstet Gynecol Scand. 2021;100(4):727–735. doi: 10.1111/aogs.14025.
- Conti J, Cahill EP. Self-managed abortion. Curr Opin Obstet Gynecol. 2019;31(6):435–440. doi: 10.1097/GCO.0000000000000585.
- Emtell Iwarsson K, Envall N, Bizjak I, et al. Increasing uptake of long-acting reversible contraception with structured contraceptive counselling: cluster randomised controlled trial (the LOWE trial). BJOG. 2021;128(9):1546–1554. doi: 10.1111/1471-0528.16754.
- Secura GM, Allsworth JE, Madden T, et al. The contraceptive CHOICE project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;/203(2):115.e1–115.e7. doi: 10.1016/j.ajog.2010.04.017.
- Taft A, Watson CJ, McCarthy E, et al. Sustainable and effective methods to increase long‐acting reversible contraception uptake from the ACCORd general practice trial. Aust N Z J Public Health. 2022;46(4):540–544. doi: 10.1111/1753-6405.13242.
